Back to Journals » Clinical Ophthalmology » Volume 18
36-Month Outcomes of Standalone Kahook Dual Blade Goniotomy Compared with Ab-Interno Closed Conjunctiva Xen Gel Stent Implantation
Authors Boopathiraj N , Wagner IV , Lentz PC, Draper C, Krambeer C, Abubaker YS , Ang BCH, Miller DD , Dorairaj S
Received 11 April 2024
Accepted for publication 6 September 2024
Published 16 September 2024 Volume 2024:18 Pages 2593—2603
DOI https://doi.org/10.2147/OPTH.S473303
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Nithya Boopathiraj,1 Isabella V Wagner,1 Paul Connor Lentz,2 Christian Draper,3 Chelsey Krambeer,1 Yazan S Abubaker,1 Bryan Chin Hou Ang,1,4,5 Darby D Miller,1 Syril Dorairaj1
1Department of Ophthalmology, Mayo Clinic, Jacksonville, FL, USA; 2Department of Ophthalmology, Mayo Clinic Alix School of Medicine, Jacksonville, FL, USA; 3Department of Ophthalmology, Eye Consultants, Spokane, WA, USA; 4Department of Ophthalmology, Tan Tock Seng Hospital, National Healthcare Group Eye Institute, Singapore; 5Department of Ophthalmology, Woodlands Health, National Healthcare Group Eye Institute, Singapore
Correspondence: Syril Dorairaj, Department of Ophthalmology, Mayo Clinic, 4500 San Pablo Road, Jacksonville, FL, 32224, USA, Tel +1-904-953-2377, Fax +1-904-953-7040, Email [email protected]
Purpose: To compare the safety and effectiveness of standalone Kahook Dual Blade (KDB) excisional goniotomy to standalone ab-interno Xen gel stent implantation in eyes with moderate-to-severe open-angle glaucoma (OAG).
Methods: A single-center, retrospective study including eyes with moderate-to-severe OAG undergoing standalone KDB goniotomy or Xen gel stent implantation was conducted. Intraocular pressure (IOP), the number of antiglaucoma medications taken daily, and best-corrected visual acuity (BCVA) were recorded at baseline and for up to 36-months. Primary outcomes assessed included changes from baseline in IOP and the number of antiglaucoma medications taken. Intergroup comparisons were conducted using independent-samples Student’s t-tests. The incidence of intraoperative and postoperative adverse events and the need for glaucoma surgical re-interventions were also recorded.
Results: Eyes receiving standalone KDB (n=26) or Xen gel stent (n=45) surgery were analyzed. The baseline mean IOP and number of antiglaucoma medications in both groups were as follows: KDB: 23.2 ± 6.0 mmHg, 2.2 ± 1.4 medications; Xen: 22.7 ± 8.8 mmHg, 3.0 ± 1.0 medications. At 36 months, IOP was reduced to 16.6 ± 5.4 mmHg in KDB eyes (n=23, − 23.5%; p=0.0004) and 15.3 ± 5.6 mmHg in Xen gel stent eyes (n=15, − 22.1%; p=0.006), while number of antiglaucoma medications was reduced to 1.1 ± 0.7 (− 30.8%; p=0.0005) and 2.2 ± 1.4 (− 25.6%; p=0.01), respectively. Three eyes (11.5%) in the KDB group and 19 eyes (42.2%) in the Xen gel stent group required additional surgery before month 36 due to refractory high IOP.
Conclusion: Both KDB goniotomy and Xen gel stent implantation significantly lowered the IOP and antiglaucoma medication burden in patients with moderate-to-severe OAG. While the Xen gel stent is frequently used to treat moderate-to-severe OAG patients with uncontrolled IOP, standalone KDB goniotomy may be equally effective as a long-term intervention, reducing the need for subsequent glaucoma surgery.
Keywords: kahook dual blade, micro-invasive glaucoma surgery, open angle glaucoma, xen gel stent
Introduction
Glaucoma is the leading cause of irreversible blindness in developed and developing countries.1,2 As the projected increase in disease prevalence is expected to reach 111.8 million individuals worldwide by 2040,1 the need for effective glaucoma treatment options is being explored. Elevated intraocular pressure (IOP) is the most common finding in open-angle glaucoma (OAG), and is considered the only modifiable risk factor for disease progression.3–5 Traditional IOP-lowering glaucoma treatments have evolved from antiglaucoma medications, lasers, and invasive bleb-based procedures (eg, trabeculectomy and drainage device implantation) to minimally invasive glaucoma surgery (MIGS). MIGS has revolutionized glaucoma management by offering a significant reduction in IOP with minimal tissue trauma and reduced procedural risks.6,7 When compared to traditional incisional procedures, MIGSs provide faster postoperative recovery, improved patient satisfaction, and shorter operation times, though they may slightly compromise on IOP-reducing efficacy.6,7 By targeting the aqueous outflow through the Schlemm’s canal, subconjunctival space, or suprachoroidal space,8 MIGS lower IOP by altering aqueous humor dynamics and can be performed with or without cataract surgery.
The Kahook Dual Blade (KDB; New World Medical, Rancho Cucamonga, CA) is a novel goniotomy blade created to produce a more complete removal of trabecular meshwork (TM) tissue through an ab interno approach under gonioscopic visualization. It is a single-use, disposable instrument that manually excises a strip of TM tissue using two parallel blades, leaving a direct opening for the aqueous humor to pass from the anterior chamber into the Schlemm’s canal. The footplate of the KDB rests on the outer wall of Schlemm’s canal and provides a controlled excision, thereby preventing deeper penetration or trauma that may induce scarring. KDB restores the normal aqueous outflow by removing tissue from the site of outflow obstruction in the OAG and TM and avoids complications associated with bleb formation. Thus, the procedure results in minimal tissue damage, quicker recovery times, and less fibrosis over time, leading to effective long-term outcomes.9,10 KDB goniotomy has been shown to be effective in the treatment of OAG as a standalone therapy or when combined with phacoemulsification. Studies have reported an IOP reduction of 24–36% and an antiglaucoma medication reduction of 26–40% for up to 12 months after standalone KDB.11,12
The Xen gel stent (Allergan Inc., CA, USA) is an implant that directs aqueous flow from the anterior chamber into the subconjunctival space through a scleral channel. The device consists of a small hydrophilic tube made of porcine collagen-derived gelatin cross-linked with glutaraldehyde. A gel stent can be molded when soft and hydrated. It is noninflammatory and causes a minimal fibrotic response in the extraocular tissue. Initially, three distinct designs were developed: Xen 140, Xen 63, and Xen 45, each measuring 6.0 mm in length but varying in their lumen diameters of 140 μm, 63 μm, and 45 μm, respectively. Currently, the Xen 45 is the only version commercially available. Implantation of the Xen gel stent is commonly conducted via an ab interno approach, which does not necessitate dissection of the conjunctiva. It can be implanted through a clear corneal incision providing subconjunctival filtration, thus avoiding conjunctival incisions and related complications such as bleb leak or hypotony. Alternatively, an ab-externo approach may be employed, which can involve surgical dissection of the conjunctiva. In this technique, the conjunctiva is displaced anteriorly, and a needle is inserted through the scleral tissue roughly 2.5 mm from the limbus, entering the anterior chamber where the stent is subsequently deployed. In procedures requiring conjunctival dissection, the stent is positioned 2.5 mm from the limbus. After placement of the implant, the conjunctiva and Tenon’s layer are closed with sutures. This procedure has demonstrated significant IOP reduction as a standalone procedure or when combined with phacoemulsification in various studies.13–16
These two procedures – excisional goniotomy with the KDB and Xen gel stent implantation –act through different IOP-reducing mechanisms. KDB goniotomy removes a strip of the TM to improve the flow of aqueous humor, while the Xen gel stent is placed under the conjunctiva to establish a permanent drainage channel that directs aqueous egress from the anterior chamber to the subconjunctival space. To our knowledge, there is only one study in the literature comparing the outcomes of standalone KDB goniotomy to Xen gel stent implantation over a 24-month follow-up period. Therefore, additional studies are needed to directly compare the clinical outcomes of both procedures over long-term follow-up. This study aimed to fulfill this unmet need by evaluating the 36-month safety and efficacy outcomes of KDB goniotomy and Xen gel stent implantation when performed as standalone procedures for the treatment of moderate-to-severe OAG.
Methods
This was a retrospective, nonrandomized analysis of the data of patients diagnosed with moderate to severe OAG who underwent elective standalone KDB excisional goniotomy or Xen gel stent implantation at the Mayo Clinic in Jacksonville, Florida, United States from January 2015 to December 2020. No protected health information, as defined by the Health Information Portability and Accounting Act, was collected, and all procedures were conducted in accordance with the ethical standards of institutional and/or national research committees. The study protocol was approved by the Institutional Review Board (IRB) of the Mayo Clinic (IRB: 18–000006) and was conducted in accordance with the tenets of the Declaration of Helsinki. Informed consent was waived by the Mayo Clinic IRB as the study was retrospective in nature and all information was de-identified. Patients aged > 18 years who were diagnosed with OAG (including pseudoexfoliative and pigmentary glaucoma) were included. Data collection included a complete review of the patient’s ophthalmic history, including previous surgeries, number of antiglaucoma medications taken, Goldmann applanation IOP, Snellen best-corrected visual acuity (BCVA), gonioscopy findings, non-dilated and dilated slit-lamp biomicroscopy examination of the anterior and posterior segments, and standard automatic perimetry using a Humphrey Field Analyzer (Carl Zeiss Meditec Inc., Dublin, CA, USA). Baseline IOP was calculated at the last follow-up visit prior to surgery. Glaucoma severity was classified according to the current International Classification of Diseases, Tenth Revision classification system. The indications for surgery in all cases were moderate-to-severe OAG with suboptimal IOP control despite maximally tolerated medications or confirmed disease progression, as recorded by Humphreys field analysis. Patients with previous laser or surgical treatment for glaucoma were included. The exclusion criteria consisted of patients aged less than 18 years with corneal opacities not permitting an adequate view for surgery and associated retinal or optic nerve disease.
All the surgeries were performed by a single surgeon (S.D). Both surgeries were performed under topical anesthesia with monitored care, and the eye was prepared with betadine (povidone-iodine) and draped. During KDB surgery, a 2.2 mm clearcut keratome was used to enter the anterior chamber with a shelf-like incision. Viscoelasticity was used to inflate the anterior chamber and a gonioscopic contact lens was placed over the cornea to visualize the angle. The KDB device was advanced into the anterior chamber, and approximately 120° of TM tissue was excised circumferentially. Miochol was used to constrict pupils. During the Xen gel stent implantation surgery, a 2.75 mm clearcut keratome was used to enter the anterior chamber with a shelf-like incision. Viscoelasticity was used to fully inflate the anterior chamber and a gonioscopic contact lens was placed over the cornea to visualize the angle. Under the ab interno approach, the Xen gel stent implant was placed in the superonasal region, confirming that it entered the anterior part of the TM, exiting 3 mm from the limbus, with the bevel facing the 12’ clock hour in the sclera. The remaining viscoelastic material was irrigated from the anterior chamber and the wounds were sealed. With a 30-gauge needle 0.2 mg/mL of mitomycin C mixed with preservative-free lidocaine was injected in the superior nasal quadrant and mitomycin C was massaged to form a diffuse elevated bleb. Topical antibiotics and steroid drops were administered postoperatively for both procedures.
The postoperative data collected included BCVA, IOP, slit-lamp examination, and review of antiglaucoma medications and surgical complications on day 1, week 1, and months 1, 3, 6, 12, 24, and 36. The primary outcomes were changes in IOP from baseline and number of antiglaucoma medications at 36 months. Surgical success was defined as >20% IOP reduction from baseline to 36 months on the same or fewer antiglaucoma medications. Failure was defined as the need for an additional glaucoma procedure to control IOP. The secondary outcome measures were the incidence of complications (intraoperative and postoperative) and reoperations related to both procedures. Patient data were censored after failure. An IOP spike was defined as an IOP elevation of ≥10 mmHg from baseline or an IOP of ≥30 mmHg. Needling was referred to the in-office revision of bleb using 5-Fluorouracil, and “bleb revision” referred to surgical revision of scarring, wound leak, or use of Mitomycin-C for a failing bleb. Additional glaucoma surgeries were defined as any procedure performed, including open bleb revision, Xen gel stent replacement, or any other drainage procedure to control the IOP. In-office needling was not considered a complication or additional procedure.
Statistical Analysis
All data were de-identified and analyzed using BlueSky Statistics v10.3.1-Pro (BlueSky Statistics LLC, Chicago, IL, USA). Baseline characteristics and study outcomes were compared using independent-samples Student’s t-tests for continuous variables, and Pearson’s chi-squared test and Fisher’s exact test, as needed, for categorical variables. An independent-samples Student’s t-test was used for the evaluation of IOP and the number of antiglaucoma medications from baseline for up to 36 months between the KDB and Xen gel stent groups. All tests within this analysis were 2-sided, and a p-value of ≤ 0.05, was considered statistically significant. Kaplan-Meier analysis was used to compare the probability of failure, and Log rank test was used for statistical comparisons.
Results
Seventy-one eyes of 55 patients, including 26 eyes of 17 patients who underwent standalone KDB goniotomy and 45 eyes of 38 patients who underwent standalone Xen gel stent implantation, were included in the analysis. Eleven patients in the Xen gel stent group (24.4%) did not have 36-month data due to death (n=1) or loss to follow-up (n=10).
Baseline clinical and demographic characteristics of the participants are shown in Table 1. No significant differences were observed in the baseline characteristics (such as age, sex, or ethnicity) between the KDB and Xen groups. The KDB group had a larger number of eyes with pigmentary glaucoma (n=7, 26.9%) than the Xen gel stent group (n=1, 2.2%). The eyes that underwent KDB goniotomy were all pseudophakic (n=26; 100%) compared with the eyes in the Xen gel stent group (n=41; 91.1%). The severity of glaucoma was comparable between the groups (p=0.33). In both groups, 46.7% and 34.6% of the eyes in the Xen and KDB groups, respectively, had undergone previous glaucoma surgery and/or laser procedure (p=0.11).
 |
Table 1 Baseline Demographics and Preoperative Characteristics |
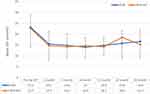
Figure 1 and Table 2 show the mean IOP reduction between the groups at each time point. Mean baseline values for IOP were comparable between both groups (KDB: 23.2 ± 6.0 mmHg; Xen gel stent group: 22.7 ± 8.8 mmHg; p= 0.31). At 36 months, the mean IOP was 16.6 ± 5.4 mmHg after KDB goniotomy (n=23, −23.5%; p=0.0004) and 15.3 ± 5.6 mmHg after Xen gel stent implantation (n=15, −22.1%; p=0.006). The IOP reduction was comparable between both groups at 36 months (p=0.18). Statistically significant reductions in IOP occurred at each time point after surgery in both groups (p<0.001), and there were no significant differences between the groups at any time point.
 |
Table 2 IOP and Medication Outcomes at Baseline and All Time Points |
At 36 months, surgical success was achieved in 53.8% of the KDB eyes. Of these, 3 eyes (29.4%) did not require antiglaucoma medications. Three eyes (11.5%) were considered failures because they required additional glaucoma surgery to control IOP. These eyes underwent a subsequent glaucoma procedure at a mean of 21 months (range: 3–36 months) after goniotomy. In the Xen gel stent group, surgical success was achieved in 31.1% of the eyes, and of these, only 1 eye was medication-free. Nineteen eyes (42.2%) required additional surgery to control the IOP. Most of the surgical failures occurred within the first 12 months. Eyes that did not require secondary surgical reintervention during the first postoperative year were more likely to maintain long-term IOP stability. Figure 2 shows the Kaplan-Meier analysis of the cumulative probability of failure for KDB goniotomy and Xen gel stent implants. A significant difference was observed between the groups (Log rank test, p= 0.008).
 |
Figure 2 Kaplan-Meier cumulative probability of failure for Kahook Dual Blade goniotomy and Xen gel stent implant. There was significant difference between both groups (log-rank p= 0.008). |
Figure 3 and Table 2 depict the mean reductions in the antiglaucoma medication burden between both groups at all time points. The mean preoperative medication use was comparable between the groups (p=0.36). The number of antiglaucoma medications taken in the KDB group at baseline and 36 months were 2.2 ± 1.4 and 1.1± 0.7, respectively (−30.8%; p=0.0005). Within the Xen gel stent group, the number of antiglaucoma medications taken were 3.0 ± 1.0 and 2.2 ± 1.4, respectively (−25.6%; p=0.01). Statistically significant reductions in the need for antiglaucoma medications occurred at all time points in both groups (p<0.001), and there was a significant difference in antiglaucoma medications reduction in the KDB group compared with the Xen gel stent group at 24 months (p<0.02) and 36 months (p<0.002).
The complications and surgical reinterventions are presented in Tables 3 and 4. No sight-threatening complications were observed in either of the groups. Additionally, the BCVA and HVF remained stable across all eyes throughout the follow-up period. Hypotony, hyphema, and IOP spikes were the most common adverse events in both the groups. The hyphotony and hyphema were mostly self-limiting. An IOP spike was observed in 11.5% (n=3) and 4.4% (n=2) of KDB and Xen eyes, respectively. The addition of AGMs was required to control IOP spikes in all five eyes. The observed complications did not differ significantly between the groups (p=0.49). Needling, although not considered a complication or additional surgery, was performed in 10 of the 45 eyes (22.2%) in the Xen gel stent group. Among these, 3 eyes underwent needling once, 6 eyes underwent needling twice, and 3 eyes underwent >3 needling sessions. The first needling session was performed during the first six postoperative months. Within 36 months, additional glaucoma surgery was performed in 22 eyes, with 3 eyes in the KDB group (11.6%) and 19 eyes in the Xen gel group (42.2%).
 |
Table 3 Incidence of Postoperative Complications Following Standalone KDB Goniotomy versus Xen Gel Stent Implantation |
 |
Table 4 Incidence of Secondary Surgical Reinterventions Following KDB Goniotomy versus Xen Gel Stent Implantation |
Discussion
In recent years, MIGSs have gained popularity as effective options for reducing IOP in patients with OAG. This retrospective study compared the effectiveness of standalone KDB excisional goniotomy and ab-interno Xen gel stent implantation in reducing the IOP and antiglaucoma medication burden. Both procedures significantly reduced the IOP and number of antiglaucoma medications from baseline, for up to 36 months postoperatively. Mean IOP and number of antiglaucoma medications in the KDB group were reduced by 23.5% and 30.8% at 36 months, respectively, comparable to two prior studies on KDB excisional goniotomy that reported mean IOP reductions by 24–31% and mean antiglaucoma medication reductions by 26–37% under a shorter-term follow-up (6–12 months).11,17 This reduction in IOP is also comparable to similar procedures such as incisional goniotomy with the Trabectome (NeoMedix Corp., Tustin, CA, USA)18–20 and Gonioscopy-assisted transluminal trabeculotomy (GATT).21–24 There are only a few studies have demonstrated the efficacy of KDB goniotomy in patients with refractory glaucoma. Our study showed comparable results to those of Salinas et al17 who reported a significant reductions in IOP (24%) and antiglaucoma medication burden (36%) at 6 months post-KDB goniotomy in severe and refractory glaucoma patients.
The present study also demonstrates the IOP-lowering potential of standalone Xen gel stent implantation, with a mean IOP reduction of 22.1% at 36 months, consistent with most published Xen studies.13,14,25 Few studies have evaluated the efficacy of the XEN implant in patients who have undergone previous glaucoma laser and/or surgical procedures26–28 but Lewczuk et al29 demonstrated that surgical success rates after Xen gel stent implantation in eyes with a history of previous glaucoma surgeries did not differ from those in surgically naïve eyes. Previous studies on Xen gel stent implantation have shown the need for postoperative revisions due to fibrosis.25 After 36 months of follow-up, some Xen eyes in our study also required postoperative bleb revisions (n=2; 4.4%), and nearly half of the eyes (n=19; 42.2%) required another surgical procedure to control IOP. This reintervention rate is comparable to previous reports by Laroche et al30 who reported that 40% of Black and Afro-Latino patients required secondary glaucoma surgery following Xen gel stent implantation at 12 months, and Gillmann et al31 who reported a reoperation rate of 26.1% in Caucasian patients following Xen gel stent implantation with or without concomitant phacoemulsification at 36 months.31 Our study also reports the same observed trend that the majority of surgical failures occurred during the first few postoperative months. Eyes that did not require any additional procedures to control IOP during the first few months were more likely to maintain a stable long-term IOP. Hence, identifying preoperative risk factors may help to achieve optimal surgical outcomes.
Within the PubMed-indexed literature, only one report comparing retrospective outcomes between KDB and Xen gel stent surgery was found but with a shorter follow-up period and lower retention rate. Duong et al32 evaluated the 24-month outcomes of both procedures and concluded that comparable IOP and antiglaucoma reductions, as well as safety profiles, were observed in both groups. In contrast, our study demonstrated a significantly favorable safety profile with KDB goniotomy over a longer follow-up period, although the IOP and antiglaucoma medication reductions were comparable between the groups. By lowering topical medication use, the KDB may also tackle problems related to non-adherence, ocular surface toxicity, and health care costs. Although the demographic and baseline ocular characteristics were similar between both groups, permitting reasonable analysis, future prospective studies with long-term data are needed to more conclusively assess and compare the surgical outcomes between both procedures.
The advantages of this study include its long-term follow-up and the evaluation of data related to standalone MIGS. Despite growing evidence that standalone MIGS lowers IOP and antiglaucoma medication dependence, few studies have evaluated the effects of standalone MIGS without the influence of cataract surgery.33 Limitations of this study include its retrospective design and incomplete follow-up. Additionally, the Kaplan-Meier analysis did not account for differences in the types of glaucoma.
Overall, this study demonstrated that both Xen gel stent implantation and KDB goniotomy are effective options for reducing IOP and antiglaucoma medication use in uncontrolled moderate-to-severe OAG as a standalone procedure. Although the percentage of IOP reduction achieved at 36 months was similar between the groups, Xen gel stent-treated eyes required more medications and had a higher rate of reintervention than KDB goniotomy-treated eyes. Thus, lowering the antiglaucoma medication burden and the reduced need for postoperative reintervention makes KDB goniotomy a potentially favorable long-term option in patients with moderate-to-severe OAG compared with Xen gel stent implants.
Conclusion
In summary, both standalone procedure can effectively reduce IOP and antiglaucoma medication use for up to 36 months in eyes with moderate-to-severe OAG. In most eyes, KDB goniotomy was shown to be non-inferior to Xen gel stent implantation, and the need for secondary glaucoma surgery was delayed or prevented for at least 36 months. Although Xen gel stent implantation is a highly effective method to control IOP, patients should be advised regarding the procedure’s loss of efficacy over time, potential risk of failure, possible need for bleb revisions, and probability of repeat surgery.
Data Sharing Statement
The authors’ institutions did not permit any data sharing. Any query should be directed toward corresponding author (S.D.).
Acknowledgments
We would like to thank Ms. Joyce Baker for her many contributions to the Department of Ophthalmology, Mayo Clinic, Florida.
Author Contributions
All listed authors made a significant contribution to this work in multiple areas including conception, study design, execution, data acquisition, analysis, interpretation, drafting, and/or critical review. All authors gave final approval of the version to be published, agreed on the journal of submission, and agreed to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040 -. Ophthalmology. 2014;121(11):2081–2090. doi:10.1016/j.ophtha.2014.05.013
2. Zhang N, Wang J, Li Y, Jiang B. Prevalence of primary open angle glaucoma in the last 20 years: a meta-analysis and systematic review. Sci Rep. 2021;11(1):13762. doi:10.1038/s41598-021-92971-w
3. Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression - Results from the early manifest glaucoma trial. Arch Ophthalmol-Chic. 2002;120(10):1268–1279. doi:10.1001/archopht.120.10.1268
4. Lichter PR, Musch DC, Gillespie BW, et al. Collaborative initial glaucoma treatment study comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001;108(11):1943–1953. doi:10.1016/S0161-6420(01)00873-9
5. Van Veldhuisen PC, Ederer F, Gaasterland DE, et al. The advanced glaucoma intervention study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130(4):429–440.
6. Richter GM, Coleman AL. Minimally invasive glaucoma surgery: current status and future prospects. Clin Ophthalmol. 2016;10:189–206. doi:10.2147/OPTH.S80490
7. Gurnani B, Tripathy K. Minimally Invasive Glaucoma Surgery. StatPearls. 2023.
8. Pillunat LE, Erb C, Junemann AG, Kimmich F. Micro-invasive glaucoma surgery (MIGS): a review of surgical procedures using stents. Clin Ophthalmol. 2017;11:1583–1600. doi:10.2147/OPTH.S135316
9. Tanito M, Matsuo M. Ab-interno trabeculotomy-related glaucoma surgeries. Taiwan J Ophthalmol. 2019;9(2):67–71. doi:10.4103/tjo.tjo_38_19
10. Seibold LK, Soohoo JR, Ammar DA, Kahook MY. Preclinical investigation of ab interno trabeculectomy using a novel dual-blade device. Am J Ophthalmol. 2013;155(3):524–529e2. doi:10.1016/j.ajo.2012.09.023
11. Sieck EG, Epstein RS, Kennedy JB, et al. Outcomes of kahook dual blade goniotomy with and without phacoemulsification cataract extraction. Ophthalmol Glaucoma. 2018;1(1):75–81. doi:10.1016/j.ogla.2018.06.006
12. ElMallah MK, Berdahl JP, Williamson BK, et al. Twelve-month outcomes of stand-alone excisional goniotomy in mild to severe glaucoma. Clin Ophthalmol. 2020;14:1891–1897. doi:10.2147/OPTH.S256423
13. Karimi A, Lindfield D, Turnbull A, et al. A multi-centre interventional case series of 259 ab-interno Xen gel implants for glaucoma, with and without combined cataract surgery. Eye. 2019;33(3):469–477. doi:10.1038/s41433-018-0243-8
14. Schlenker MB, Gulamhusein H, Conrad-Hengerer I, et al. Efficacy, safety, and risk factors for failure of standalone Ab interno gelatin microstent implantation versus standalone trabeculectomy. Ophthalmology. 2017;124(11):1579–1588. doi:10.1016/j.ophtha.2017.05.004
15. Parra MTM, López JAS, Grau NSL, Ceausescu AM, Santonja JJP. XEN implant device versus trabeculectomy, either alone or in combination with phacoemulsification, in open-angle glaucoma patients. Graef Arch Clin Exp. 2019;257(8):1741–1750. doi:10.1007/s00417-019-04341-y
16. Ibanez-Munoz A, Soto-Biforcos VS, Rodriguez-Vicente L, et al. XEN implant in primary and secondary open-angle glaucoma: a 12-month retrospective study. Eur J Ophthalmol. 2020;30(5):1034–1041. doi:10.1177/1120672119845226
17. Salinas L, Chaudhary A, Berdahl JP, et al. Goniotomy using the kahook dual blade in severe and refractory glaucoma: 6-month outcomes. J Glaucoma. 2018;27(10):849–855. doi:10.1097/IJG.0000000000001019
18. Mizoguchi T, Nishigaki S, Sato T, Wakiyama H, Ogino N. Clinical results of Trabectome surgery for open-angle glaucoma. Clin Ophthalmol. 2015;9:1889–1894. doi:10.2147/OPTH.S83958
19. Kaplowitz K, Bussel II, Honkanen R, Schuman JS, Loewen NA. Review and meta-analysis of ab-interno trabeculectomy outcomes. Br J Ophthalmol. 2016;100(5):594–600. doi:10.1136/bjophthalmol-2015-307131
20. Maeda M, Watanabe M, Ichikawa K. Evaluation of trabectome in open-angle glaucoma. J Glaucoma. 2013;22(3):205–208. doi:10.1097/IJG.0b013e3182311b92
21. Grover DS, Godfrey DG, Smith O, Feuer WJ, Montes de Oca I, Fellman RL. Gonioscopy-assisted transluminal trabeculotomy, ab interno trabeculotomy: technique report and preliminary results. Ophthalmology. 2014;121(4):855–861. doi:10.1016/j.ophtha.2013.11.001
22. Grover DS, Godfrey DG, Smith O, Shi W, Feuer WJ, Fellman RL. Outcomes of Gonioscopy-assisted Transluminal Trabeculotomy (GATT) in eyes with prior incisional glaucoma surgery. J Glaucoma. 2017;26(1):41–45. doi:10.1097/IJG.0000000000000564
23. Rahmatnejad K, Pruzan NL, Amanullah S, et al. Surgical outcomes of Gonioscopy-assisted Transluminal Trabeculotomy (GATT) in patients with open-angle glaucoma. J Glaucoma. 2017;26(12):1137–1143. doi:10.1097/IJG.0000000000000802
24. Olgun A, Aktas Z, Ucgul AY. XEN gel implant versus gonioscopy-assisted transluminal trabeculotomy for the treatment of open-angle glaucoma. Int Ophthalmol. 2020;40(5):1085–1093. doi:10.1007/s10792-019-01271-w
25. Galal A, Bilgic A, Eltanamly R, Osman A. XEN glaucoma implant with mitomycin C 1-year follow-up: result and complications. J Ophthalmol. 2017;2017:5457246. doi:10.1155/2017/5457246
26. Hengerer FH, Kohnen T, Mueller M, Conrad-Hengerer I. Ab interno gel implant for the treatment of glaucoma patients with or without prior glaucoma surgery: 1-year results. J Glaucoma. 2017;26(12):1130–1136. doi:10.1097/Ijg.0000000000000803
27. Grover DS, Flynn WJ, Bashford KP, et al. Performance and safety of a new Ab interno gelatin stent in refractory glaucoma at 12 months REPLY. Am J Ophthalmol. 2018;188:186–187. doi:10.1016/j.ajo.2018.01.032
28. Lenzhofer M, Kersten-Gomez I, Sheybani A, et al. Four-year results of a minimally invasive transscleral glaucoma gel stent implantation in a prospective multi-centre study. Clin Exp Ophthalmol. 2019;47(5):581–587. doi:10.1111/ceo.13463
29. Lewczuk K, Konopinska J, Jablonska J, et al. XEN glaucoma implant for the management of glaucoma in naive patients versus patients with previous glaucoma surgery. J Clin Med. 2021;10(19):4417. doi:10.3390/jcm10194417
30. Laroche D, Nkrumah G, Ng C. Real-world retrospective consecutive study of Ab interno XEN 45 gel stent implant with mitomycin C in black and afro-latino patients with glaucoma: 40% required secondary glaucoma surgery at 1 year. Middle East Afr J Ophthalmol. 2019;26(4):229–234. doi:10.4103/meajo.MEAJO_126_19
31. Gillmann K, Bravetti GE, Rao HL, Mermoud A, Mansouri K. Combined and stand-alone XEN 45 gel stent implantation: 3-year outcomes and success predictors. Acta Ophthalmologica. 2021;99(4):E531–E539. doi:10.1111/aos.14605
32. Duong RT, Pittner AC, Roa TM, Dirghangi AJ, Netland PA. Stand-alone Xen gel microstent implantation compared with kahook dual blade goniotomy. J Glaucoma. 2022;31(11):898–902. doi:10.1097/IJG.0000000000002120
33. Armstrong JJ, Wasiuta T, Kiatos E, Malvankar-Mehta M, Hutnik CML. The effects of phacoemulsification on intraocular pressure and topical medication use in patients with glaucoma: a systematic review and meta-analysis of 3-year data. J Glaucoma. 2017;26(6):511–522. doi:10.1097/IJG.0000000000000643
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.