Back to Journals » Clinical Ophthalmology » Volume 18
A 14-Year Retrospective Clinical Analysis of Ocular Manifestations of Syphilis in a Portuguese Tertiary Center
Authors Faria Pereira A , Gama e Castro A, Teixeira-Martins R , Coelho-Costa I, Torres-Costa S , Silva M, Pedrosa AC, Araújo J, Figueira L, Oliveira-Ferreira C
Received 7 September 2024
Accepted for publication 15 October 2024
Published 29 October 2024 Volume 2024:18 Pages 3053—3069
DOI https://doi.org/10.2147/OPTH.S494585
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ana Faria Pereira,1 Ana Gama e Castro,1 Rita Teixeira-Martins,1 Inês Coelho-Costa,1 Sónia Torres-Costa,1 Marta Silva,1 Ana Catarina Pedrosa,1 Joana Araújo,1 Luís Figueira,1– 3 Cláudia Oliveira-Ferreira1,4
1Department of Ophthalmology, Unidade Local de Saúde de São João, Porto, Portugal; 2Unit of Pharmacology and Therapeutics, Department of Biomedicine, Faculty of Medicine, University of Porto, Porto, Portugal; 3MedInUP - Center for Drug Discovery and Innovative Medicines, Faculty of Medicine, University of Porto, Porto, Portugal; 4Department of Surgery and Physiology, Faculty of Medicine, University of Porto, Porto, Portugal
Correspondence: Ana Faria Pereira, Department of Ophthalmology, Unidade Local de Saúde de São João, Avenida Prof. Hernâni Monteiro, Porto, 4202 – 451, Portugal, Email [email protected]
Purpose: Syphilis is a re-emerging infectious disease with various systemic manifestations, including ocular involvement, which can lead to significant morbidity if untreated. This study aims to analyze the ocular manifestations of syphilis in patients treated at a Portuguese tertiary center over a 14-year period.
Patients and Methods: A retrospective review of patients diagnosed with syphilis who presented with ocular symptoms from 2010 to 2023 was conducted. Data collected included demographic information, clinical presentation, ophthalmologic findings, serologic test results, treatment regimens and outcomes.
Results: A total of 47 patients with ocular syphilis were identified. The mean age of the cohort was 45, with a male predominance of 78.7%. The most common ocular manifestations included uveitis (mostly posterior and panuveitis), optic neuritis, acute syphilitic posterior placoid chorioretinitis and vitritis. Best corrected visual acuity (BCVA) at presentation was highly variable, ranging from hand movements to no impairment of visual acuity. At the end of the follow-up period, the majority of the study eyes achieved a BCVA between 0 and 0.1 (p< 0,000). Acute syphilitic posterior placoid chorioretinitis was associated with poorer visual outcomes after treatment, indicating its presence is a poor prognosis factor. HIV status, the presence of vitritis, vasculitis and papillitis at presentation, a positive syphilis serology in cerebrospinal fluid and treatment regimen did not appear to have a significant impact on the final BCVA.
Conclusion: Ocular syphilis, though rare, remains a significant cause of visual morbidity. Early recognition and prompt treatment are crucial for preventing permanent vision loss. Regular screening and increased awareness among clinicians are essential to manage this potentially sight-threatening condition effectively. Further research is needed to optimize treatment protocols and improve patient outcomes.
Keywords: syphilis, uveitis, optic neuritis, retinal vasculitis, retrospective study, penicillin
Introduction
Syphilis, a chronic bacterial infection caused by the spirochete Treponema pallidum, has been a significant public health challenge for centuries. Described as early as the 15th century, syphilis is often termed “the great imitator” due to its capacity to mimic a wide array of other diseases. This chameleon-like nature extends to its ocular manifestations, which can present variably across different stages of the disease. Despite significant advances in diagnostic and therapeutic approaches, ocular syphilis remains a pertinent issue, particularly with its resurgence in the context of the Human Immunodeficiency Virus (HIV) pandemic.1,2
The incidence of syphilis has fluctuated over the decades, with significant public health campaigns in the mid-20th century leading to a dramatic decline. However, recent years have witnessed a concerning resurgence globally. According to the World Health Organization (WHO), millions of new cases are reported annually, with a notable increase in high-income countries among men who have sex with men (MSM) and individuals co-infected with HIV.3,4 Ocular syphilis, while less common than other manifestations, represents a critical subset due to the potential for severe visual impairment and blindness if left untreated.5
Ocular syphilis can manifest at any stage of the disease, from primary to tertiary syphilis, and may present as an isolated symptom or in conjunction with systemic signs. Early syphilitic eye disease typically involves anterior segment inflammation, such as interstitial keratitis. Secondary syphilis may present with uveitis, retinitis, and vitritis. Tertiary syphilis can lead to more severe complications, including optic atrophy and gummatous involvement of ocular structures. The diversity in presentation necessitates a high index of suspicion, especially in endemic areas or high-risk populations.6
The diagnosis of ocular syphilis is complex, often requiring a multifaceted approach. Serological testing remains the cornerstone, with both non-treponemal (eg, RPR, VDRL) and treponemal-specific tests (eg, FTA-ABS, TP-PA) employed to confirm infection. However, the sensitivity and specificity of these tests can vary, particularly in different stages of the disease or in the context of co-infections such as HIV. Polymerase chain reaction (PCR) and direct visualization of the spirochete in ocular fluids can provide definitive diagnosis but are not universally available.1,6
The treatment of ocular syphilis typically involves intravenous penicillin, which remains the gold standard due to its efficacy in eradicating T. pallidum. However, treatment regimens may need to be tailored based on disease stage, severity of ocular involvement, and the presence of concomitant infections.6 Corticosteroids are often adjunctively used to mitigate inflammatory damage, although their use requires careful monitoring to avoid exacerbating the infection.2 Early diagnosis and prompt initiation of therapy are crucial to prevent irreversible visual impairment.6
The purpose of this retrospective review is to analyze the ocular manifestations of syphilis in patients treated at a Portuguese tertiary center over a 14-year period. By conducting a comprehensive review of these cases, this study aims to elucidate the spectrum of ocular presentations, the diagnostic challenges encountered, and the therapeutic outcomes achieved. Through this detailed examination, we aim to enhance understanding of the disease’s impact on ocular health.
Materials and Methods
A retrospective study of serologic documented cases of ocular syphilis from January 2010 to December 2023 and respective medical records was made at the Ophthalmology Uveitis and Ocular Inflammation Department of Unidade Local de Saúde de São João. This study protocol was conducted according to the Helsinki Declaration and was approved by the Ethics Committee of Unidade Local de Saúde de São João. Patient’s informed consent was waived by the Ethics Committee in view of the retrospective nature of the study. Patients’ names, addresses, and other confidential information were not collected nor shared throughout the study.
Data including demographic features, duration of follow-up, presentation complaint, as well as systemic and ocular comorbidities were collected. In cases of HIV co-infection, CD4 count was recorded. Additional data recorded included best corrected visual acuity (BCVA) at presentation and at the end of follow-up, type of ocular manifestation and characterization, lumbar puncture, prescribed antibiotic and oral corticosteroid therapy and the occurrence of Jarisch Herxheimer reaction were recorded.
Visual acuity was measured by the distance Snellen chart and converted from decimal to the logarithm of the minimum angle of resolution (logMAR) equivalents for statistical analysis. To facilitate analysis, light perception, hand movement, and finger counting were recorded as 2.6, 2.1 and 1.7 logMAR, respectively.
Statistical analysis was performed using IBM Statistical Package for the Social Sciences (SPSS) Statistics version 24 (SPSS inc., Chicago IL., USA). Quantitative variables were expressed as mean ± standard-deviation (SD). The Shapiro–Wilk test was used to assess the normal distribution of numerical data. Normally distributed data were analyzed using parametric tests, whereas non-normally distributed data were assessed using non-parametric tests. A p value less than 0.05 was considered statistically significant. Frequencies along with percentages for qualitative variables were used to describe the data.
Results
Epidemiology
A total of 47 patients and 65 eyes were identified during the study period. The mean age was 45.0 ± 13.9 years (range 24 to 82 years) and thirty-seven patients (78,7%) were men. 10 patients (21,3%) had positive serology for HIV. The main epidemiologic features as well as systemic and ocular comorbidities are presented in Table 1.
 |
Table 1 Epidemiologic Features and Systemic and Ocular Comorbidities |
Ophthalmological Symptoms and Clinical Signs
The most common ocular presenting symptom was visual impairment, followed by pain.
In our study, the most frequent presentations were posterior uveitis and panuveitis. The initial characteristics of the uveitic involvement include a majority of bilateral involvement (61,7%) and a majority of posterior segment involvement (acute syphilitic posterior placoid chorioretinitis, optic disc edema and papillitis, vitritis and vasculitis) (Table 2).
 |
Table 2 Characteristics of Ocular Involvement |
We did not observe any cases of conjunctivitis, macular hole or congenital syphilis and no Argyll-Robertson pupil was detected in our cohort.
Anterior Uveitis
In 6 patients (9 eyes) the presentation of ocular syphilis was in exclusive form of acute anterior uveitis. Anterior uveitis included granulomatous and non-granulomatous forms, hypertensive and non-hypertensive forms and presented with posterior synechiae in one case and “spillover” anterior vitritis in other case, as presented in Table 3.
 |
Table 3 Characteristics of Ocular Involvement in Anterior Uveitis |
Panuveitis and Posterior Uveitis
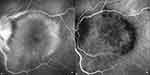
The most common manifestations in patients with posterior and panuveitis included acute syphilitic posterior placoid chorioretinitis (ASPPC) (Figures 1 and 2), optic disc edema, and vitritis; however, the spectrum of posterior involvement exhibited considerable variability, as we can see in Tables 4–6.
 |
Table 4 Characteristics of Posterior Involvement in Posterior Uveitis Patients |
 |
Table 5 Characteristics of Posterior Involvement in Posterior Uveitis Patients |
 |
Table 6 Characteristics of Posterior Involvement in Panuveitis Patients |
An ANOVA was conducted to compare initial visual acuity, final visual acuity, and the difference between visual acuities among different clinical presentation groups, revealing no significant differences. Additionally, the presence of vitritis, vasculitis, or papillitis does not appear to impact initial, final, or differential visual acuity, as seen in Table 7.
 |
Table 7 Best Corrected Visual Acuity at Presentation, End of Follow-Up, and Differential Change in Patients with and without Vitritis, Vasculitis and Papillitis |
To analyze the impact of ASPPC on visual outcomes, we compared the BCVA at presentation, at the end of the follow-up period, and the change in BCVA between eyes with posterior syphilitic involvement (ie, posterior uveitis or panuveitis) with and without ASPPC (Table 8). Remarkably, we observed a clear difference between the compared parameters, with ASPPC being associated with worse visual acuity both at presentation and at the end of treatment, highlighting its role as a poor prognostic factor. However, a statistically significant difference was found only when comparing the post-treatment BCVA.
 |
Table 8 Best Corrected Visual Acuity at Presentation, End of Follow-Up, and Differential Change in Patients with Posterior Involvement with and without ASPPC |
Visual Acuity
In our study, the best corrected visual acuity (BCVA) at presentation was highly variable, ranging from hand movements to no impairment of visual acuity, as seen in Figure 3. At the end of the follow-up period, the majority of the study eyes achieved a BCVA between 0 and 0.1 logMAR, as seen in Figure 4. However, two eyes retained visual acuities of 1.0 and 1.7 logMAR, both attributable to pre-existing amblyopia.
 |
Figure 3 Graphic Representation of Distribution of Patients’ Best Corrected Visual Acuities (BCVA, logMAR) at Presentation. |
 |
Figure 4 Graphic Representation of Distribution of Patients’ Best Corrected Visual Acuities (BCVA, logMAR) at the End of the Follow-up Period. |
Syphilis and HIV
We identified 10 patients with HIV in our study (21,3%), one of whom was diagnosed with HIV during the course of a sexually transmitted diseases screening at the time of syphilis diagnosis. These cases predominantly presented with posterior segment involvement with 5 cases of posterior uveitis, 4 cases of panuveitis and 1 case of intermediate uveitis. Vitritis was present in 9 out of 10 cases, while ASPPC was present in 5 cases.
The HIV status demonstrated no significant impact on both initial and final visual acuity, as well as on the differential between final and initial visual acuity, as confirmed by the t-test analysis, seen in Table 9. Additionally, a linear regression analysis revealed that CD4 count does not appear to be significantly related to final visual acuity (p=0,167).
 |
Table 9 Best Corrected Visual Acuity at Presentation, End of Follow-Up, and Differential Change in Patients with Positive and Negative HIV Serologies |
Serologic Diagnosis
All but one patient tested positive on serology, with both VDRL and TPPA. In the exceptional case in which the serology was negative, diagnosis relied on the identification of Treponema pallidum in vitreous sample using real time PCR. The serum VDRL titers ranged from 1:1 to 1:512 dilutions.
Lumbar puncture was performed in 22 patients (46,8%), revealing positive syphilis serology in cerebrospinal fluid investigations for 13 cases (59,1%).
An analysis based on seropositivity was also conducted. Specifically, VDRL was positive in the cerebrospinal fluid of 40% (4 out of 10) of HIV-positive patients compared to 24.3% (9 out of 37) of non-HIV patients. Due to the limited number of patients, statistical analysis was not feasible.
The involvement of the central nervous system (CNS) by syphilis does not appear to impact the presentation of ocular disease, as observed in the distribution of different clinical presentations in patients with positive and negative or non-performed syphilis serology in cerebrospinal fluid in Figure 5.
Regarding the impact of positive syphilis serology in cerebrospinal fluid in BCVA at baseline and at the end of the follow-up period, there appears to be a trend towards poorer initial visual acuity in cases with evidence of CNS involvement, although this difference is not statistically significant. However, final BCVA does not differ between the groups, as indicated by a higher differential between final and initial BCVA (Table 10).
 |
Table 10 Best Corrected Visual Acuity at Presentation, End of Follow-Up, and Differential Change in Patients with Positive and Negative or Non-Performed Lumbar Puncture |
Therapeutic Management
Intravenous aqueous crystalline penicillin G, or benzylpenicillin, was the most frequently prescribed systemic syphilis therapy, administered to 35 cases (74,5%), in a 14-day regimen in 31 cases (66,0%), 17-day regimen in 1 case (2,1%) and 21-day regimen in 2 cases (4,3%), all administered as 4 million units intravenously every four hours. One of the patients was transferred to another hospital before the end of the treatment, lacking further information on the duration of treatment. Of these 35 cases, 5 were also given intra-muscular Penicillin G benzathine at a dose of 2.4 million units at the end of the benzylpenicillin course. 8 cases (17,0%) were prescribed intra-muscular Penicillin G benzathine at a dose of 2.4 million units per week, for 3 weeks, and 4 (8,5%) were treated with intravenous ceftriaxone at 2 g/day for 2 weeks. Oral corticosteroids were prescribed to 9 (19,1%) of our patients, always initially under antibiotic cover for more than 48 hours, with an anti-inflammatory objective in cases of dense vitreous haze, significant macular or papillary edema to limit functional sequelae.
In addition to syphilis-specific therapies, topical glucocorticoids, cycloplegics and IOP-lowering medications were also frequently prescribed.
As seen in Table 11, the mean BCVA at baseline was 0.79 and notably, it significantly improved to a mean of 0.21, demonstrating the effectiveness of treatment.
 |
Table 11 Mean Changes in Best Corrected Visual Acuity Between Presentation and at the End of the Follow-Up Period, After Treatment |
The treatment regimen did not appear to have a significant impact on final visual acuity, as there were no significant differences observed between the four treatment groups.
There also appears to be no significant difference in final BCVA between patients who received corticosteroids and those who did not (Table 12). Conversely, final visual acuity seems slightly lower in the corticosteroid-treated group, although this difference did not reach statistical significance.
 |
Table 12 Best Corrected Visual Acuity at End of Follow-Up and Differential Change in Patients with or Without Oral Corticosteroid Treatment |
Jarisch-Herxheimer Reaction
One of the patients in the study, who presented with bilateral posterior uveitis, including ASPPC, vitritis, and exudative retinal detachment, experienced a Jarisch-Herxheimer reaction. This reaction was characterized by headache, fever, and a generalized maculopapular rash, which started 24 hours after the first dose of benzylpenicillin and was alleviated with paracetamol. The reaction resolved completely within 48 hours. Notably, the patient had an initial serum VDRL titer of 1:256 dilutions upon admission.
Evolution of Ocular Syphilis Cases Over Time
Over the past fourteen years, the incidence of ocular syphilis at our ophthalmological center has shown a notable trend of increase and fluctuation, reflecting broader epidemiological patterns of syphilis infection, especially in the 2022–2023 biennium as shown in Figure 6, with 10 cases diagnosed.
 |
Figure 6 Graphic Representation of Distribution of Ocular Syphilis Cases over the 14-year Study Period. |
Discussion
A global resurgence of syphilis has recently been reported, and Portugal, like many other European countries, is no exception. According to the Portuguese National Health Institute (Instituto Nacional de Saúde Doutor Ricardo Jorge), data indicates an increase in the incidence of syphilis, with a significant growth in the number of cases since the early 2000s.7 This increase is attributed to various factors, including risky sexual behaviors, such as decreased use of condoms and an increase in multiple sexual partners.4
According to the 2022 report from the Portuguese General Directorate of Health (Direção-Geral da Saúde), the number of notified syphilis cases has shown an upward trend, especially in large metropolitan areas like Lisbon and Porto. Syphilis predominantly affects men, with a high proportion of cases among men who have sex with men (MSM). In 2021, the notification rate was approximately 11 cases per 100,000 inhabitants.7
Congenital syphilis, which occurs when the infection is transmitted from an infected mother to her child during pregnancy, continues to be a public health concern.8 Notification of this condition is mandatory in Portugal, and preventive measures include systematic screening of all pregnant women for syphilis, usually conducted in the first and third trimesters of pregnancy.9
Ocular syphilis is uncommon, with recent studies indicating that approximately 0.5–1.5% of patients with syphilis exhibit ocular manifestations.10 Ocular involvement can occur at any stage of syphilis, with acute ocular inflammation typically arising during the early stages, namely primary, secondary and early latent syphilis. More chronic inflammatory processes are associated with late-stage syphilis. Ocular syphilis presenting as the initial manifestation of the infection has also been documented.10,11
Any part of the eye can be affected by syphilis, including the eyelid, orbit, conjunctiva, sclera, cornea, uvea, retina, retinal vasculature, optic nerve, pupillomotor pathways and cranial nerves involved in extraocular movements. A wide range of ocular signs were encountered in this series, including scleritis, keratouveitis, anterior uveitis, intermediate uveitis, panuveitis, acute syphilitic posterior placoid chorioretinitis, retinitis, necrotising retinitis, cystoid macular edema, exsudative retinal detachment, branch arterial occlusion and optic neuritis. The most common manifestation of ocular syphilis is uveitis, although syphilitic uveitis accounts for less than 1–2% of all uveitis cases.2,8,10,12
In recent years, there have been increasing reports emphasising the prevalence of non-granulomatous syphilitic anterior uveitis.13,14 This trend was observed in the study cohort with mutton-fat, or granulomatous, keratic precipitates found in only two eyes.
The most common presenting ocular symptom in our study was visual impairment, affecting 53 (81,5%) eyes, consistent with other reports.8,15 The initial ophthalmological clinical presentation was very heterogeneous in our study, and, in contrast to our findings of a predominance of posterior and panuveitis (76,9%), the literature frequently documents anterior uveitis as the most prevalent ocular presentation.14 This disparity can be attributed to the fact that routine cases of anterior uveitis are commonly managed by general ophthalmologists and typically do not necessitate an etiological investigation, particularly in initial episodes, while more complex posterior manifestations, which pose greater risk of complications, are often referred to specialized tertiary care centers.
It is also noteworthy that papillitis is not commonly described in literature as a typical feature, yet our study found a higher incidence of papillitis at around 48%, which aligns with findings reported by other authors.8,16
The near-pathognomonic “butterfly-wing” appearance of posterior placoid chorioretinitis is predominantly observed in immunocompromised individuals and was observed in almost half of our sample. This condition carries the risk of underlying chorioretinal atrophy and consequent visual loss. The presentation appears to be directly related to the patient’s immune status and does not seem to be influenced by adjuvant corticosteroid treatment.17,18 Remarkably, we observed a clear difference between visual acuity after treatment in patients with ASPPC when compared to patients with other forms of posterior involvement, highlighting its role as a poor prognostic factor.
Given the frequent co-infection of HIV-syphilis and the often-associated ocular involvement, it should be systematically sought.19 In our study, 21.3% of patients also had HIV co-infection. The association between HIV status and ocular segment involvement has been analyzed in previous case series with a suggestion that HIV positive patients tend to present with predominantly posterior segment involvement, that goes along with our findings.16,20 It is possible that posterior segment involvement in ocular syphilis is not solely associated with positive HIV status but may also be influenced by the degree of immunosuppression. Our study did not identify significant differences between seropositive and seronegative patients regarding visual acuity recovery or cerebrospinal fluid involvement, likely due to the moderate sample size. The literature presents divergent perspectives on this matter: some indicate seropositivity as a potential prognostic factor for poorer outcomes, while others attribute this variation to consistent patient monitoring and early intervention before symptom manifestation.8 The presentation of ocular syphilis heralded diagnosis of HIV in one patient of our cohort.
Darkfield microscopy and PCR tests, which directly identify Treponema pallidum from lesion exudate or tissue, or in the aqueous humor, are definitive for early syphilis diagnosis. Despite this, serological testing remains the primary method for most diagnoses. A presumptive diagnosis involves using two types of serological tests: nontreponemal and treponemal tests.6,10 Nontreponemal tests, such as the VDRL and RPR tests, detect antibodies against cardiolipin, a membrane phospholipid.2,18 These tests are quick, straightforward, and cost-effective but lack specificity for syphilis, leading to potential false positives and negatives. They are valuable for assessing disease activity, and serial testing is useful for monitoring the response to antibiotic therapy.21 Post-treatment, titres usually decrease and may become non-reactive or remain very low. Treponemal tests, including FTA-ABS and TP-PA, detect syphilis-specific antibodies that remain positive for life. While these tests are effective for confirming a diagnosis, they are not suitable for assessing treatment response.6
Ocular syphilis often occurs alongside central nervous system syphilis, commonly referred to as neurosyphilis. Traditionally, ocular syphilis was classified as a subtype of neurosyphilis.1 However, contemporary research indicates that ocular syphilis is a separate condition from neurosyphilis. It appears that the central nervous system invasion by Treponema pallidum is not necessarily required for the onset of ocular syphilis.22 Regarding cerebrospinal fluid (CSF) examination in the context of syphilitic uveitis, there is significant variation in clinical practice. Some authors advocate for universal CSF analysis in cases of syphilitic uveitis, while others argue against its routine use. According to Ghanem et al, a CSF examination is not necessary to diagnose ocular or optic syphilis in patients with reactive serologic tests.6 They highlight that despite positive serologic tests, up to 30% of patients with ocular syphilis and up to 90% with optic syphilis may have a normal CSF examination.6,19,23
In our study, albeit limited by a small sample size, positive syphilis serology in CSF did not significantly impact baseline or final best-corrected visual acuity (BCVA) in patients with syphilitic uveitis. Similarly, it did not influence the clinical presentation of the disease. While cases with evidence of CNS involvement showed a tendency towards poorer initial BCVA, this difference did not reach statistical significance. Moreover, there was no significant difference in final BCVA between groups, suggesting that undergoing a lumbar puncture did not provide prognostically significant information regarding visual outcomes.
Thus, the decision to perform CSF examination in cases of syphilitic uveitis should be guided by clinical judgment and individual patient factors.19
Regarding treatment, penicillin is highly effective for all stages of syphilis and is the drug of choice.24 Resistance to penicillin has not been observed in Treponema pallidum.25 According to 2010 recommendations, the treatment for ocular syphilis should be identical to that for neurosyphilis, which relies on intravenous penicillin G at 18 to 24 million IU per day (depending on weight) administered as 3–4 million units intravenously every four hours or via continuous infusion for 10 to 14 days. The alternative in case of compliance difficulties is intramuscular benzathine penicillin at 2.4 million IU per week for 3 weeks. The treatment is the same for HIV patients.6,8
For individuals with a documented penicillin allergy, desensitization followed by treatment with penicillin is recommended.2,6 The limited data available on alternative antibiotic agents suggests they should only be considered when treatment with penicillin is not possible or is absolutely contraindicated. In nonpregnant adults with penicillin allergy in whom desensitization is not possible, intramuscular ceftriaxone at 2 g per day for 10 to 14 days is an alternative. Ceftriaxone penetrates the CNS well and has been shown to have efficacy similar to that of penicillin in all stages of syphilis, although the data are restricted to observational studies.26,27
Appropriate systemic syphilis therapy has been demonstrated to positively impact upon visual outcome, as we proved in our cohort, with BCVA found to significantly improve for involved eyes after appropriate treatment and is often taken as an indication of a correct diagnosis.4,28
Topical and periocular corticosteroids play a crucial role in the treatment of ocular inflammation associated with syphilis, effectively managing syphilitic interstitial keratitis and anterior uveitis. Despite concerns about using systemic steroids in infectious uveitis, both oral and intravenous corticosteroids are appropriate adjunct treatments for posterior uveitis, scleritis, and optic neuritis, as extensively documented in uveitis management literature.2,17,29 In our study, oral corticosteroids were prescribed to almost 1/5 of patients, always initiated under antibiotic coverage for more than 48 hours. This approach aims to reduce dense vitreous haze, significant macular or papillary edema, and limit functional sequelae. Interestingly, there was no significant difference in final BCVA between patients who received corticosteroids and those who did not. This finding may be influenced by the initial use of corticosteroids in more severe cases with poorer visual prognosis from the outset. Conversely, the final visual acuity appeared slightly lower in the corticosteroid-treated group, potentially reflecting the initial severity of cases, although this difference did not achieve statistical significance.
The Jarisch-Herxheimer reaction is a hypersensitivity response triggered by the release of treponemal antigens during the rapid destruction of spirochetes, resulting in flu-like symptoms and exacerbation of lesions such as uveitis, macular edema, or papillary edema. This reaction can typically be managed with supportive measures and antipyretic treatment, and it usually occurs within the first 24 hours. Pretreatment with corticosteroids has not been shown to provide any advantage.8,10 In our cohort, we observed one case that rapidly resolved with supportive care to manage symptoms.
It is crucial to distinguish between the Jarisch-Herxheimer reaction and a penicillin allergy to ensure the continuity of appropriate treatment.10
While our study encompasses a relatively large number of patients compared to similar research, its sample size remains limited for drawing definitive conclusions. To address this limitation and achieve more robust findings, a multicenter approach involving a larger and more diverse patient cohort would be necessary. Additionally, OCT data could offer valuable insights into the visual outcomes of these patients, particularly in cases of syphilitic APSC.30 Future studies incorporating OCT findings would allow for a more comprehensive analysis of visual outcomes in this population.
Conclusion
In conclusion, ocular syphilis, though rare, remains a significant cause of visual morbidity. Diagnosing syphilis-related ocular manifestations poses challenges due to its varied clinical presentations. Clinicians must maintain a high suspicion for ocular syphilis in HIV-positive patients presenting with uveitis. Early diagnosis, supported by detailed clinical history and specific ocular findings is crucial for preventing permanent vision loss despite occasional negative serological tests.
Research into vaccines for syphilis is ongoing but lacks a viable candidate in the near term. Recent studies suggest potential for biomedical prevention using doxycycline: a daily dose reduced syphilis, gonorrhea, and chlamydia infections by 73% in HIV-infected men. While routine use of doxycycline is not recommended yet, it may become a key preventive strategy.
Strategies to combat syphilis should include awareness and health education campaigns, promotion of condom use, and screening and treatment programs for STIs (Sexually Transmitted Infections) in health centers and hospitals.
Data Sharing Statement
Statement Access to any supplemental information is available from the corresponding author upon reasonable request.
Statements of Ethics
The study was approved by the Institutional Ethics Committee of Unidade Local de Saúde de São João, Porto, Portugal. The protocol conformed with the canons of the Declaration of Helsinki for research involving human participants, as well as the European Union’s General Data Protection Regulation. Informed consent was waived by the Ethics Committee in view of the retrospective nature of the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Dutta Majumder P, Chen EJ, Shah J, et al. Ocular syphilis: an update. Ocul Immunol Inflamm. 2019;27(1):
2. Aldave AJ, King JA, E.T. C
3. Northey LC, Skalicky SE, Gurbaxani A, et al. Syphilitic uveitis and optic neuritis in Sydney. Australia Br J Ophthalmol. 2015;99(9):
4. Tran TH, Cassoux N, Bodaghi B, et al. Syphilitic uveitis in patients infected with human immunodeficiency virus. Graefes Arch Clin Exp Ophthalmol. 2005;243(9):863–869. doi:10.1007/s00417-005-1137-6
5. Buscho SE, Ishihara R, Gupta PK, et al. Secondary syphilis presenting as bilateral simultaneous papillitis in an immunocompetent individual. Cureus. 2022;14(8):e28465. doi:10.7759/cureus.28465
6. Ghanem KG, Ram S, Rice PA. The modern epidemic of syphilis. N Engl J Med. 2020;382(9):845–854. doi:10.1056/NEJMra1901593
7. Estatística IND. Estatísticas da Saúde: 2018. INE. 2018.
8. Carbonniere C, Couret C, Guillouzouic A, et al. [Ocular syphilis: a retrospective study of 27 cases in Nantes University Hospital (France) from 2000 to 2013]. Rev Med Interne. 2015;36(11):722–727. doi:10.1016/j.revmed.2015.07.008
9. Plotzker RE, Murphy RD, Stoltey JE. Congenital syphilis prevention: strategies, evidence, and future directions. Sex Transm Dis. 2018;45(9S Suppl 1):
10. Tsan GL, Claiborne RT. Ocular syphilis. Clin Exp Optom. 2021;104(7):
11. Davis JL. Ocular syphilis. Curr Opin Ophthalmol. 2014;25(6):
12. Koksaldi S, Nazlı A, Kaya M, et al. Never forget ocular syphilis: a case series from a single tertiary centre. Int J STD AIDS. 2023;34(11):
13. Eandi CM, Neri P, Adelman RA, et al. Acute syphilitic posterior placoid chorioretinitis: report of a case series and comprehensive review of the literature. Retina. 2012;32(9):
14. Anshu A, Cheng CL, Chee SP. Syphilitic uveitis: an Asian perspective. Br J Ophthalmol. 2008;92(5):
15. Zhu J, Jiang Y, Shi Y, et al. Clinical manifestations and treatment outcomes of syphilitic uveitis in HIV-negative patients in China: a retrospective case study. Medicine. 2017;96(43):
16. Kayabasi M, Köksaldı S, Saatci AO, et al. Presentation of ocular syphilis with bilateral optic neuropathy. Neuroophthalmology. 2023;47(5–6):
17. Zamani M, Garfinkel RA. Corticosteroid-induced modulation of acute syphilitic posterior placoid chorioretinitis. Am J Ophthalmol. 2003;135(6):
18. Brito P, Penas S, Carneiro Â, et al. Spectral-domain optical coherence tomography features of acute syphilitic posterior placoid chorioretinitis: the role of autoimmune response in pathogenesis. Case Rep Ophthalmol. 2011;2(1):
19. Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR–03):
20. Li SY, Birnbaum AD, Tessler HH, et al. Posterior syphilitic uveitis: clinical characteristics, co-infection with HIV, response to treatment. Jpn J Ophthalmol. 2011;55(5):
21. Romanowski B, Sutherland R, Fick GH, et al. Serologic response to treatment of infectious syphilis. Ann Intern Med. 1991;114(12):
22. Reid GA, Halmagyi GM, Whyte C, et al. Ocular vs neurosyphilis. are they the same? A guide to investigation and management. Eye. 2024;38(12):
23. Harding AS, Ghanem KG. The performance of cerebrospinal fluid treponemal-specific antibody tests in neurosyphilis: a systematic review. Sex Transm Dis. 2012;39(4):
24. Idsoe O, Guthe T, Willcox RR. Penicillin in the treatment of syphilis. The experience of three decades. Bull World Health Organ. 1972;47:
25. Chen XS, Yin Y-P, Wei W-H, et al. High prevalence of azithromycin resistance to Treponema pallidum in geographically different areas in China. Clin Microbiol Infect. 2013;19(10):975–979. doi:10.1111/1469-0691.12098
26. Liang Z, Chen Y-P, Yang C-S, et al. Meta-analysis of ceftriaxone compared with penicillin for the treatment of syphilis. Int J Antimicrob Agents. 2016;47(1):6–11. doi:10.1016/j.ijantimicag.2015.10.020
27. Cao Y, Su X, Wang Q, et al. A multicenter study evaluating ceftriaxone and benzathine penicillin G as treatment agents for early syphilis in Jiangsu. China Clin Infect Dis. 2017;65(10):
28. Gass JD, Braunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology. 1990;97(10):
29. Solebo AL, Westcott M. Corticosteroids in ocular syphilis. Ophthalmology. 2007;114(8):
30. Mirzania D, Zacks DN, Zhou Y, et al. Clinical characteristics and visual outcomes of acute syphilitic posterior placoid chorioretinopathy. Ophthalmol Retina. 2023;7(12):
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Systemic Immunomodulatory Therapy in Uveitis Related to Behçet’s Disease: A 10-year Profile
Almeida M, Ferreira AM, Araújo JR, Figueira L
Clinical Ophthalmology 2025, 19:2133-2141
Published Date: 5 July 2025