Back to Journals » Clinical Ophthalmology » Volume 18
A Novel Procedure for Treating Radial Keratotomy (RK) Induced Corneal Irregularity Utilizing Treatment of Epithelial Compensation of Higher-Order Aberrations and Topographic Guided Ablation-The CREATE Protocol
Authors Motwani M
Received 2 May 2024
Accepted for publication 23 September 2024
Published 7 October 2024 Volume 2024:18 Pages 2813—2820
DOI https://doi.org/10.2147/OPTH.S476555
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Manoj Motwani
Cornea Revolution/Motwani LASIK Institute, San Diego, CA, 92121, USA
Correspondence: Manoj Motwani, Cornea Revolution/Motwani LASIK Institute, 8710 Scranton Road, Ste 170, San Diego, CA, 92121, USA, Tel +1 (858) 554-0008, Email [email protected]
Purpose: To present the outcomes of a retrospective study of treatment of radial keratotomy-induced corneal irregularity with topographic guided ablation and a trans-epithelial approach based on epithelial compensation.
Methods: Sixty eyes of 31 patients were treated for radial keratotomy-induced corneal irregularity utilizing a customized trans-epithelial topographic guided ablation photorefractive keratectomy (PRK) for treatment of corneal higher-order aberrations and lower-order astigmatism. Three-month results were analyzed via measurement of vision, refraction, residual higher-order aberrations (HOAs), residual lower-order and higher-order aberrations, as well as for loss or gains of lines of best corrected visual acuity.
Results: Higher-order aberrations (HOA) were reduced by 69%, with an 80% reduction of higher-order aberrations grouped with lower-order aberrations (Grouped). Most (95%) of eyes achieved 20/40 vision or better, 50% of eyes gained 1– 9 lines of best corrected vision, and no eyes had loss of best corrected vision.
Conclusion: Use of the CREATE protocol to treat RK-induced corneal irregularity resulted in a significant decrease in HOA, as well as a significant improvement in corrected distance visual acuity.
Keywords: astigmatism, higher-order aberrations, radial keratotomy, lower-order aberrations, photorefractive keratectomy, corneal irregularity
Introduction
Radial Keratotomy (RK) as a procedure has a problematic history. Although it aided many in correcting their refractive error before excimer laser refractive ablation became available, the hand-created incisions caused significant corneal irregularity in many patients. Combined with a common propensity for significant hyperopic over-correction, RK has left many patients with visual issues such as refractive error, blurry vision, multiple images, poor night vision, and variable vision.1,2 These visual problems can reach debilitating levels. Although treatment has been attempted with various modalities such as scleral/RGP lenses, corneal transplant, and excimer laser refractive ablation,3 the most effective treatment would remove the high levels of corneal irregularity, or higher-order aberrations, (HOA) present in the post-RK cornea. In 2022, we published a study treating RK patients with topographic guided ablation (WaveLight Contoura, WaveLight Laser Technologie AG, Erlangen, Germany) and the San Diego Protocol.4 These results demonstrated improved vision with a 52.5% reduction in HOA. We have also shown in a prior publication that corneal epithelial compensation can mask a significant amount of corneal HOA from being measured by a topographic system.5 It is possible to measure epithelial compensation via optical coherence tomography, but there is no existing technology that combines this epithelial thickness map with the topography generated HOA map to create a full irregularity map for excimer laser treatment. In lieu of this, the author used PTK (Phototherapeutic Keratectomy) to the depth of epithelial compensation provided by a Visionix/Optovue epithelial thickness mapping (ETM) device. This effectively creates an epithelial mask to remove the compensated for stromal irregularity. This customized trans-epithelial PRK approach utilizing topographic guided ablation (WaveLight Contoura) was termed the CREATE Protocol, Corneal Repair Epithelium, and Topography Enhanced. The author has already published the results of this treatment for corneal ectasia/keratoconus.6 Here we report on the normalization of RK-induced corneal irregularity.
Materials and Methods
We retrospectively examined patients who had treatment for RK-induced corneal irregularity with the CREATE Protocol and also had at least 3 months of follow-up results. We were able to analyze data from 60 eyes of 31 patients.
Results were tabulated for pre- and post-operative vision, average K, and manifest cylinder. Pre-op Contoura (topography utilizing the Topolyzer Vario (WaveLight, Erlangen, Germany)) measured astigmatism was also averaged. Pre- and post-operative corrected distance visual acuity (CDVA) was tabulated, as were lines of vision gained or lost.
Measurements of up to 4th order Zernike polynomials to measure higher-order aberrations (HOA) were tabulated, as were what we defined as Grouped. These were HOA plus lower-order sphere and astigmatism, excluding piston and tilt. The first number was measured to demonstrate corneal irregularity reduction, the second to include lower-order aberration reduction.
Visionix/Optovue (Visionix/Optovue, Fremont, CA) Avanti and Solix optical coherence tomography (OCT) devices were utilized to measure epithelial compensation. This was accomplished by measuring the epithelial thickness of the thinnest and thickest areas in the central 5 mm of the cornea and the difference designated the epithelial compensation for HOA.
Epithelial removal was either performed by using the PTK mode on the Nidek EC-5000 or on the WaveLight EX500. For the latter, epithelial removal was performed by programming a WFO (wavefront optimized) myopic treatment to the depth of corneal epithelium removal determined by Optovue OCT mapping or by including the epithelial removal as part of the topographic guided treatment by adding myopic treatment equal to the depth of the epithelium. This was due to the fact that there is currently no PTK mode available on WaveLight lasers in the United States. The OCT epithelium map was analyzed for the thickest and thinnest points in the central 5 mm zone, and epithelial removal by laser was set to the depth of the thickest epithelial measurement. Residual epithelial removal was accomplished to a width of 9 mm via manual removal by cellulose sponge or corneal epithelial scraper as necessary for further hyperopic treatment.
WaveLight Contoura was then used to treat the corneal higher-order aberrations and irregular astigmatism measurable by topography of the anterior cornea.7 Surgical planning utilized the measured astigmatism up to the maximum 3 diopters (D) allowed in the Contoura FDA approval. All Contoura ablations used the Contoura measured astigmatism and axis and were performed with a 6 mm optical zone. In the latter part of this study, patients also had subsequent treatment of hyperopia via WFO to prevent a high amount of post-operative hyperopia. This hyperopic correction was performed with the 6.5 mm optical zone with a 9 mm transition zone. Mitomycin C 0.2mg/cc was applied topically via sponge applicator for 20 seconds after ablation.
Patients would then have a planned treatment at the 4-month mark to eliminate residual refractive error via simple PRK Wavefront Optimized ablation. This was virtually always hyperopia/hyperopic astigmatism.
All procedures were performed on the WaveLight EX500 excimer laser. All procedures were performed by one surgeon (MM) at one center in San Diego, California. All topographies were obtained utilizing the Topolyzer Vario (Alcon Surgical, Fort Worth, TX, USA). All epithelial thickness maps (ETM) were obtained with the Optovue Avanti or Solix devices (9-mm ETM) (Optovue, Fremont, CA, USA).
Post-operative care consisted of fluorometholone 0.1% bid for 4 weeks, ofloxacin 0.3% qid × 1 week, and Prolensa qd as needed for pain during epithelial healing. Bandage contact lenses were removed with healing of the corneal abrasion which was between 3–5 days on average. Some patients were also treated with Tyrvaya nasal spray twice a day to increase tear film in an attempt to speed epithelial healing.
All patients signed written informed consent forms allowing their data to be used in this study and published including sample cases 1–4. This study falls under the exemption of the Health and Human Services (HHS) Policy for the Protection of Human Research Subjects 45 CFR 46.104 (d) for retrospective studies and 46.104 for exempt research, and thus, no Institutional Review Board approval was required. This study also conforms to the Declaration of Helsinki guidelines. No safety-related incidents occurred or were reported to Alcon Inc. or WaveLight concerning patients involved in this study.
Results
Table 1 contains the demographics of the 60 (60) eyes of 31 patients included in this study, 20 men and 11 women. Average patient age was 60 years, range 47–84 years. Dark pupil measurements were less than 6 mm in all eyes.
 |
Table 1 Patient Demographics |
Table 2 contains pre-op and post-op values for the average K, pre-op measured and manifest cylinder, post-op manifest cylinder, and spherical equivalent.
 |
Table 2 Pre-Op and Post-Op Values for Average K, Pre-Op Measured and Manifest Cylinder, Post-Op Manifest Cylinder, and Pre-Op Spherical Equivalence |
Table 3 lists the pre-op and post-op 4th order higher-order aberrations (HOA), and with lower-order astigmatism and sphere (Grouped). The Grouped category does not include tilt or piston. The average HOA were reduced post-op by 69%, and the Grouped values were reduced by 80.2%. This compares favorably with our prior RJ repair study (which did not treat epithelial compensation) that showed an average reduction of 52.5% for HOA and 46.6% for the Grouped values.
 |
Table 3 Zernike Polynomials for 6th Order Higher-Order Aberrations and for Grouped Polynomials |
Statistical testing was performed to determine the validity of the results for HOA reduction, Grouped Reduction, and for all values combined. T testing resulted in statistical significance between the post-op and pre-op HOA values with a p value of 0.0369. Comparing pre-op and post-op Grouped values was not statistically significant with a p value of 0.1178. Comparing all pre-op and post-op values per patient was statistically significant with a p value of 0.0378.
Table 4 presents the best corrected visual acuities pre-op and post-op by Snellen chart measurements, as well as the percentages of eyes in that category. It is notable that 95% of the eyes achieved a best-corrected distance acuity of 20/40 or better post-operatively, while only 80.3% could achieve this pre-operatively.
 |
Table 4 Best-Corrected Visual Acuities Pre-Op and Post-Op by Snellen Chart Measurements |
Table 5 shows the lines of BCVA gained. 50% of the eyes gained between 1 and 7 lines of best corrected vision, while the remaining 50% neither gained nor lost lines of vision. Notably, no eyes lost any lines of BCVA.
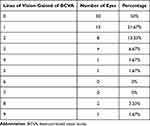 |
Table 5 Gains in Best-Corrected Visual Acuity |
Sample Cases
Case 1: 53-year-old male (Figure 1A–D) and Table 6 (Patient Data).
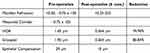 |
Table 6 Case 1 Patient Data |
 |
Figure 1 (A-D) Case 1: 53-year-old male. (A) Pre-op topography, (B) Post-op topography, (C) Pre-op Epithelial map, (D) Post-op Epithelial map. |
Case 2: 56-year-old female (Figure 2A–F) and Table 7 (Patient Data) who had treatment via a Schwind and then with the CREATE Protocol.
 |
Table 7 Case 2 Patient Data |
Discussion
Corneal irregularity is likely present in all radial keratotomy cases as each incision would have to be made at exactly the same depth, the same length, and placed perfectly in conjunction with the other incisions to get a regular central flattening of the cornea. With hand-made incisions, this is nearly impossible. It is notable that patients find that visual problems increase significantly with age. It is likely that the loss of crystalline lens accommodation plays a significant part due to the hyperopia found in many post-RK patients, but there also may be an element of cortical visual compensation that appears to decrease with age. Although some patients had visual phenomena such as multiple images, ghosting, starbursts/halos etc. almost immediately post-RK, many had these symptoms become pronounced with age. Some patients seemed to worsen after cataract surgery, likely from new irregularity induced from cataract incisions, or by the loss of light scattered absorption by the cataract.
The reduction of corneal irregularity via topography guided laser ablation can significantly ameliorate the visual symptoms as well as the significant refractive error post-RK as demonstrated in a previous study.4 Virtually all of these patients have significant epithelial compensation of their corneal stromal irregularity. This compensation is not measurable by either topography or wavefront aberrometry devices. Therefore, treatment with such imaging guided procedures would incompletely treat the actual stromal irregularity, which could then lead to different epithelial compensation further decreasing the accuracy of the outcome. To completely reduce corneal stromal irregularity, a topography map must be combined with an epithelial compensation map to create a final treatment map. A device to create such a treatment map has not been produced to the best of our knowledge, so therefore we treated with PTK utilizing the epithelium compensation as a mask. By treating to the thickest point of epithelium as measured within the center 5 mm of the epithelial thickness map from the Visionix Optovue Solix device with an excimer laser, we take advantage of the fact that corneal epithelium and stroma are ablated at the same rate. This does have the effect of flattening the central cornea as ablation is performed to the point of greatest epithelial compensation of stromal irregularity flattening the central cornea inducing hyperopia. Patients subjectively noted increased quality of vision as HOA were reduced but did not enjoy wearing spectacles with high amounts of hyperopia in the interim 4-month phase in between corneal reconstruction and refractive correction. As our experience with this procedure progressed, we pre-emptively treated hyperopia calculated by adding the manifest hyperopia + C4/C12 compensation (as in the San Diego Protocol + one diopter of hyperopia for approximately 15 microns of epithelial compensation. This smaller residual refractive error was easily corrected for by spectacles as necessary in the interim period. If the patient chose, they could continue to wear the spectacles with visual quality improvement and not receive the second refractive treatment.
Since WaveLight does not have a PTK mode in the United States, the WFO myopic mode was used to treat to the required depth either in a procedure separate from the treatment procedure or by including the myopic PTK treatment as part of the irregularity treatment similar to the Lightstream treatment available outside the US on the WaveLight excimer lasers.
In the current study, the average amount of epithelial compensation was 24 microns. Utilizing the CREATE Protocol in this study reduced the average higher-order aberrations by 69% post-operatively, and when lower-order astigmatism and sphere were additionally factored in, reduced this Grouped category by 80.2%. This is a significant change from the 52.5% and 46.6%, respectively, from the prior RK study that did not treat epithelial compensation. Just as importantly, 50% of the eyes gained between 1 and 9 lines of vision, while no eye lost any lines of vision, and 95% achieved vision of 20/40 or better post-operatively even in this group of older patients.
Sample case 1 pre-op topography demonstrates the highly irregular optical zone seen in many RK patients, with individual incisions creating linear flattening through the central optical zone. Post-op topography has a much more uniform optical zone, which corresponds to a change to the 75% HOA reduction as well as reduction in epithelial compensation from 29 microns to 10 microns. The epithelial compensation map change is striking as well, with a post-operative epithelial map that is far more uniform centrally.
The patient in sample case 2 is unique in that we are able to see the outcome of a Schwind Amaris 1050 (Schwind GmbH, Kleinostheim, Germany) corneal repair treatment. This patient originally consulted with us in 2019 for her irregular cornea from RK. She had a Schwind corneal repair treatment performed and was unsatisfied with the results. She later returned to us in 2022 for treatment. The Schwind system uses wavefront aberrometry imaging to create a corneal map for topography guided ablation. Although Schwind does allow for partial correction of the corneal irregularity (WaveLight Contoura treats all or none of the measured HOA), the corneal map is limited by the lower resolution of the wavefront aberrometry which measures 1600 points as opposed to the 22,000-point Placido topography based Contoura treatment map. Furthermore, although Schwind can perform a trans-epithelial ablation, it does not measure epithelial compensation to customize the treatment.
The Schwind treatment resulted in a 31.6% HOA reduction. Visually, it is evident that the irregular optical zone created by the RK is more regular, but it is still de-centered and of an irregular shape. Correspondingly, the epithelial compensation changed little from 27 microns to 23 microns. Treatment via the CREATE Protocol increased HOA reduction to 69.3%, corresponding with the average reduction we saw in this study. Post-op topography is visually more regular with a widened optical zone. Epithelial compensation also decreased to 11 microns with mostly central, even epithelial thickening.
Although we did not perform formal subjective visual quality testing on our patients, the reduction in HOA correlated anecdotally with a higher quality of vision and decreased visual phenomena. Also, corresponding are 95% of the eyes which had a post-operative BCVA of 20/40 or better, with 50% of eyes gaining 1–9 lines of best corrected vision. More importantly, no patient lost lines of best corrected vision or had serious adverse outcomes. In the future, standardized subjective visual testing could be performed to further confirm and quantitate the subjective visual improvement.
The biggest drawback of this procedure was the high levels of hyperopia due to the flat corneas created after the first phase of laser corneal reconstruction. Patients could see well with correction but disliked the thick hyperopic glasses. By pre-emptively treating hyperopia in conjunction with the initial corneal reconstruction treatment, patients were far more satisfied with fairly low to moderate levels of hyperopic correction. This was easily tolerated over the 4-month period until final refractive correction. This 4-month period was adopted after clinical experience with patients demonstrated incomplete epithelial re-normalization and unstable refractive error at 3 months post-op. Refractive error stabilized by 4 months in most patients. There have been a small number of eyes in our total clinical experience that had late refractive error changes well after 6 months. It was surmised this was due to late epithelial change or other factors such as crystalline lens cataractous change.
Haze was present in some patients when high amounts of hyperopic correction were performed in conjunction with corneal reconstruction. This was treated with steroid drops over 4–6 weeks. It was noted that the MMC sponge would often sit elevated on the center prolate ablation area increasing the probability of peripheral circular haze post-operatively. The occurrence of haze post-operatively was decreased by simply moving the MMC soaked sponge with a forceps in a circular manner through the hyperopic laser treatment area of 9 mm.
This same treatment protocol can be utilized for other forms of irregularity as well. We utilize the same techniques for de-centered or irregular LASIK/PRK ablations, cataract surgery, incision-induced corneal irregularity, other corneal surgery-induced irregularity (pterygium, corneal transplant, etc.), trauma or infection-induced corneal scar and irregularity, as well as keratoconus and corneal ectasia (in conjunction with corneal cross-linking).
The goal of CREATE Protocol is to restore vision by repairing the patient’s own cornea and relegate cornea transplant to only a small minority of extreme cases where it is not possible for the native cornea to be reconstructed. The results from this study, and our prior RK study, create a convincing argument that topography guided ablation and CREATE Protocol as treatment solutions for RK are reliable, safe, and appear effective at significantly decreasing the high levels of HOA seen in eyes with radial keratotomy.
Abbreviations
BCVA, best-corrected visual acuity; D, diopters; ETM, epithelial thickness maps; FDA, Food and Drug Administration; HHS, Health and Human Services; HOAs, higher-order aberrations; MMC, mitomycin C; OD, right eye; OS, left eye; PRK, photorefractive keratectomy; qd, daily; qid, four times daily; RK, radial keratotomy; UCVA, uncorrected visual acuity; US, United States.
Acknowledgments
The author would like to thank Julie Crider, PhD, for editing contributions, and Lourdes Haydaw for her extensive data collection, editing, and analytic contributions.
Disclosure
The author would like to disclose that the author has been granted United States patent no. 10857032 concerning the creation of a more uniform cornea utilizing the topography measured astigmatism, and United States patent no. 10857033 for the treatment of epithelial compensation of corneal irregularity in conjunction with the use of topography guided ablation system. These patents are the basis for the LYRA/San Diego/CREATE Protocols. The LYRA/San Diego/CREATE Protocols can be seen as a competitor to other surgical planning systems, including but not limited to Phoricdes, ZZ, Manifest Refraction with Contoura, Wavefront Optimized, and Alcon Innoveyes. The author also has patents pending for an integrated system for creating a complete treatment map of the Ocular Focusing System.
References
1. Fu L, Patel BC. Radial keratotomy correction. In: StatPearls. Treasure Island; 2021.
2. Colombo-Barboza GN, Colombo-Barboza MN, Colombo-Barboza LR, et al. Vision quality questionnaire assessment in patients after topography-guided photorefractive keratectomy for irregular astigmatism secondary to radial keratotomy. Clin Ophthalmol. 2022;16:3491–3501. doi:10.2147/OPTH.S386009
3. Colombo-Barboza GN, Rodrigues PF, Colombo-Barboza FDP, et al. Radial keratotomy: background and how to manage these patients nowadays. BMC Ophthalmol. 2024;24(1):9. doi:10.1186/s12886-023-03261-0
4. Motwani M. Treatment of corneal irregularity in radial/astigmatic keratotomy patients utilizing waveLight contoura. Clin Ophthalmol. 2022;16:111–126. doi:10.2147/OPTH.S328050
5. Motwani M, Pei R. The use of wavelight contoura to create a uniform cornea: 6-month results with subjective patient surveys. Clin Ophthalmol. 2018;12:1559–1566. doi:10.2147/OPTH.S175661
6. Motwani M. Treatment of keratoconus with wavelight contoura and corneal cross-linking combined. Clin Ophthalmol. 2021;15:2455–2472. doi:10.2147/OPTH.S303559
7. Motwani M. A protocol for topographic-guided corneal repair utilizing the US food and drug administration-approved wavelight contoura. Clin Ophthalmol. 2017;11:573–581. doi:10.2147/OPTH.S127855
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


