Back to Journals » Clinical Ophthalmology » Volume 19
A Prospective Single-Center Clinical Trial Comparing Short-Term Outcomes of a Novel Non-Cavitating Handheld Lensectomy Device versus Phacoemulsification
Authors Cannon NT , Scruggs K, Pantanelli SM
Received 12 February 2025
Accepted for publication 2 July 2025
Published 14 July 2025 Volume 2025:19 Pages 2281—2288
DOI https://doi.org/10.2147/OPTH.S522334
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Nathan T Cannon, Kathleen Scruggs, Seth M Pantanelli
Department of Ophthalmology, Penn State College of Medicine, Hershey, PA, USA
Correspondence: Seth M Pantanelli, Department of Ophthalmology, Penn State College of Medicine, Hershey, PA, USA, Tel +1 717 5315690, Email [email protected]
Purpose: To compare the short-term outcomes of a non-cavitating lensectomy device (MICOR) to phacoemulsification.
Patients and Methods: This was a two-arm prospective open-label clinical trial. Patients with visually significant cataracts at a single academic center between March and December 2023 were consecutively enrolled to undergo cataract surgery using either MICOR or phacoemulsification for nuclear fragmentation and lens removal. Adverse events (AE), lensectomy time, fluid use, and ultrasound energy use were assessed intraoperatively. Visual acuity, refraction, and AE were assessed on postoperative day one.
Results: A total of 34 eyes of 23 patients were included in the MICOR arm and 50 eyes of 32 patients in the phacoemulsification arm. No difference (p = 0.727) in logMAR best corrected distance visual acuity was observed postoperatively between MICOR (0.14 ± 0.25) and phacoemulsification (0.16 ± 0.33), nor was any difference observed in AE rates [3% versus 8%, respectively (p = 0.644)]. Lens removal time was faster with MICOR [209 vs 255 s (p = 0.003)], including for grade 2 cataracts [203 vs 237 s (p = 0.008)]. Irrigation volume was less for MICOR [33 vs 62 mL (p < 0.001)], including for grade 2 [34 vs 60 mL (p < 0.001)] and 3 cataracts [36 vs 60 mL (p = 0.004)]. Mean cumulative dissipated energy for phacoemulsification was 8.7.
Conclusion: Compared to phacoemulsification, MICOR has similar visual outcomes and adverse event rates while requiring less time, irrigation fluid, and ultrasound energy, suggesting MICOR is a viable alternative to phacoemulsification.
Plain Language Summary: The MICOR nucleus fragmentation and lens removal device is a new non-ultrasound technology used in clear-cornea extracapsular cataract surgery. This study prospectively compares MICOR to the industry standard, phacoemulsification. Compared to phacoemulsification, MICOR results in equivalent short-term visual outcomes at similar adverse event rates. MICOR may be more time efficient, emits less energy, and uses less irrigation fluid compared to phacoemulsification, suggesting it is a viable alternative.
Keywords: phacoemulsification, cataract extraction, biomedical technology
Introduction
Few advances in lens fragmentation and extraction have rivaled the advent of phacoemulsification since it was introduced in 1967 by Charles Kelman. Still, there are several disadvantages to the technology that leave room for improvement. First, the high cost and lack of portability of the console are barriers to access for the developing world.1,2 Second, the requirement that the ultrasound handpiece undergo sterile processing demands additional ancillary support staff and equipment. Third, the use of ultrasound energy in the setting of dense cataracts contributes to an increased incidence of wound burn and pseudophakic bullous keratopathy when compared with manual small incision cataract surgery (MSICS).3,4 This combination of factors leaves room for a more cost-effective, and less traumatic lens extraction technology.
The MICOR (Carl Zeiss Meditec, Jena, Germany) lensectomy system as pictured in Figure 1 is a handheld lens-pen device which performs both endocapsular nuclear fragmentation and lens removal. It maintains the same minimally invasive surgical approach as phacoemulsification through a small 2.4 mm clear-corneal incision. Phacoemulsification employs high-frequency thermogenic ultrasound energy (20–40 kHz) to create cavitation bubbles which, upon collapse, cause focal “trauma” to the lens material, thereby facilitating breakup and subsequent aspiration. On the other hand, MICOR uses low-frequency non-thermogenic mechanical agitation (rapid forward motion with slow recoil) of up to 40 Hz paired with high vacuum (up to 650 mm Hg) to break up and remove lens segments. The blunt oscillating tip is comprised of a mechanical coring apparatus, complemented by a positive displacement pump to generate a peristaltic-like vacuum at the tip. There are separate instrument tips for lens fragmentation, irrigation and aspiration (I/A), and anterior vitrectomy. Rather than requiring a foot pedal, device frequency, amplitude, and flow rate is actuated using a finger throttle on the handpiece.5
To date, there have been two studies reporting on the performance of this non-cavitating device. Ianchulev et al provided an initial retrospective case series of 665 surgeries demonstrating the device’s ability to perform nuclear fragmentation and lens extraction across a range of cataract grades with minimal adverse events (AEs; 0.45% rate of capsular tear).6 Beniz et al confirmed these low AE rates and additionally observed a significant decrease in the time required for the procedure over 61 consecutive cases, reflecting the device’s intuitive integration into the surgery workflow and the potential for surgeons to rapidly overcome the learning curve associated with mastering the technology.7 There have been no prospective clinical trials evaluating the head-to-head performance of MICOR as compared to the industry standard, phacoemulsification. Long term outcomes are important, but may mask real differences between the technologies due to the healing response that occurs over the first month postoperatively. On the other hand, short term outcomes such as corneal edema and incidence of intraocular pressure elevation may more accurately capture direct effects on the eye. As such, the purpose of this study was to compare the short-term clinical outcomes of MICOR and phacoemulsification in subjects undergoing routine cataract surgery.
Methods
This was a prospective, single-center, open-label, double-arm clinical trial. The study was approved by Western IRB (SITE00001269) and adhered to tenets of the Declaration of Helsinki, as well as the Health Insurance Portability and Accountability Act. Patient consent was required for participation in the study. The trial is registered at clinicaltrials.gov (NCT05729477) and aggregated results will be posted there. Deidentified demographics and postoperative outcome measures on individual subjects are available upon written request by contacting the corresponding author for up to 3 years after publication.
Adult subjects undergoing routine clear cornea cataract surgery with IOL implantation between March and December, 2023 at the participating site (Department of Ophthalmology, Penn State College of Medicine, Hershey, PA) were eligible for inclusion. Patients needed to be willing to participate and able to understand and complete informed consent. Subject eyes were excluded from study enrollment if they had any comorbidities which, in the opinion of the investigator, might compromise outcomes, or if they were having concurrent corneal surgery with cataract extraction. Both eyes from the same subject could be enrolled if eligible; otherwise, only the eligible eye was enrolled. The two subject cohorts were enrolled consecutively: first, a cohort undergoing cataract surgery with phacoemulsification (Centurion Vision System, Alcon, Fort Worth, TX; “Phaco” cohort); second, a cohort undergoing cataract surgery using the MICOR 700 device (Carl Zeiss Meditec, Inc, Jena, Germany; “MICOR” cohort). The primary outcome was the mean postoperative best corrected distance visual acuity (BCVA) on postoperative day 1, and the secondary outcome was the AE rate.
Patients first underwent a defined set of preoperative measurements, including BCVA, spherical equivalent (SE), and cataract type and grade, as well as collection of patient demographics. This was followed by cataract surgery in one or both eligible eyes. Intraoperatively, routine clear-cornea cataract surgery was performed for both groups by a single surgeon (SMP) with experience using MICOR. Specifically, the site investigator/surgeon performed approximately 100 cases with MICOR before study initiation. The steps of surgery included: (1) temporal clear corneal incision of 2.4 mm; (2) one side port incision; (3) topical and intracameral anesthesia; (4) viscoelastic; (5) capsulorhexis; (6) hydrodissection; (7) either (a) MICOR to pre-chop and aspirate or (b) phacoemulsification to pre-chop, emulsify, and aspirate the cataractous lens; (8) either (a) MICOR I/A or (b) phacoemulsification associated I/A; (9) IOL implantation; (9) 0.3 mL intracameral moxifloxacin 0.16% (Fagron, Inc, Rotterdam, Netherlands); and wound hydration with balanced salt saline (BSS).
Data collected during surgery included total nucleus removal time [defined as either: (a) MICOR tip in until MICOR I/A out and ready for IOL implantation; or (b) phacoemulsification tip in until phacoemulsification I/A out and ready for IOL implantation], total irrigation fluid volume used, intraoperative AEs, device failures, and any secondary intraoperative procedures (such as the use of a capsular tension ring, Malyugin ring, trypan, miLOOP, or iris hooks) and their indications. Surgeries were followed by postoperative day one appointments, during which BCVA, SE, and postoperative AE were collected, and the surgeon’s standard postoperative care was implemented. Changes in a chronic condition or consistent with natural disease progression were not considered AEs. Reasons patients were unable to complete the study were also tracked.
Data on subjects who completed all required visits were compiled and analyzed for mean values and standard deviations (SD) for each cohort and collectively. Snellen VA was converted to logMAR to facilitate averaging and statistical analyses. Nucleus removal time, BSS use, and phacoemulsification energy used were further stratified by preoperative cataract grade. For each cohort, the proportion of postoperative BCVA of at least 20/40, 20/30, 20/25, and 20/20 were calculated.
Comparisons between cohorts were made using the unpaired two-tailed t-test in Excel v16.89.1 (Microsoft Corporation). For comparisons of AE rates and the proportions of eyes with postoperative BCVA of at least 20/40, 20/30, 20/25, and 20/20, Fisher’s Exact test was performed in GraphPad Prism v10.4.0 (GraphPad Software, LLC).
Results
In total, 84 eyes of 55 subjects were included in the study: 34 eyes of 23 patients in the MICOR cohort; and 50 eyes of 32 subjects in the Phaco cohort. Within the MICOR cohort, 15 (65%) subjects were female, 22 (96%) Caucasian, and 1 (4%) Hispanic, with an average age (mean ± SD) of 67 ± 8 years. For the Phaco cohort, 22 (69%) subjects were female, 31 (97%) Caucasian, and 1 (3%) Asian, with an average age of 70 ± 7 years.
Initially, 48 eyes of 31 patients were enrolled in the MICOR arm. However, 14 eyes of 11 patients did not complete the study, including 3 eyes of 2 patients whose surgeries were rescheduled outside of the study window, 10 eyes of 8 patients who dropped out due to a hold placed on the study by the sponsor, and 1 eye of 1 patient who did not show up to their postoperative appointment. Likewise, 54 eyes of 34 patients were initially enrolled in the Phaco arm, but 4 eyes of 3 patients did not complete the study: one eye of 1 patient was lost to follow up, and 3 eyes of 2 patients cancelled their surgeries.
Preoperative characteristics of the eyes in each cohort are given in Table 1. Most cataracts were nuclear sclerotic [22 (65%) for MICOR; 34 (68%) for Phaco] and grade 2 [23 (68%) for MICOR; 33 (66%) for Phaco]. Preoperative SEs were comparable, with −1.38 ± 2.95 D for MICOR and −2.70 ± 3.29 for Phaco (p = 0.060). Eyes in the Phaco arm had somewhat poorer preoperative BCVAs [logMAR 0.37 ± 0.45 versus 0.21 ± 0.20, respectively (p = 0.027)].
 |
Table 1 Preoperative Characteristics |
An overview of intraoperative and postoperative outcomes is given in Table 2. There were no significant differences in postoperative UCVA (p = 0.980), BCVA (p = 0.727), pinhole VA (p = 0.499), or SE (p = 0.534) between the two cohorts. Even when cohorts were stratified by the proportion of eyes with at least 20/40, 20/30, 20/25, and 20/20 BCVA as shown in Figure 2, there were still no significant differences between groups (p values all ≥ 0.512). Nor was there any difference in overall AE rates (p = 0.644). Intraoperative and postoperative AEs included 1 (3%) MICOR eye with elevated postoperative intraocular pressure (IOP) requiring treatment, compared to 2 (4%) Phaco eyes with elevated IOP requiring treatment. One eye (2%) in the Phaco arm experienced a retained lens fragment requiring washout and another eye (2%) experienced an intraoperative Descemet’s membrane detachment. All AEs resolved by the end of the study without complication.
 |
Table 2 Intraoperative and Postoperative Outcomes |
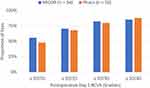 |
Figure 2 Postoperative visual outcomes. No significant differences were observed (p values ≥ 0.512). Abbreviation: BCVA, best corrected distance visual acuity. |
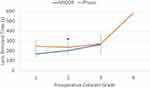
There was no significant relationship between sequential case number and nucleus removal time (R2 = 0.02) in either group. This is important because it suggests that the surgeon had overcome the learning curve with MICOR (he had completed approximately 100 procedures with the device before the study began). However, as shown in Figure 3, mean MICOR lens removal times were 46 seconds (18%) faster than phacoemulsification lens removal times (p = 0.003). When broken down by cataract grade, MICOR was 34 seconds (14%) more efficient at removing grade 2 cataracts compared to phacoemulsification (p = 0.008). MICOR also required 29 mL (47%) less irrigation fluid throughout the surgery (p < 0.001), including 26 mL (43%) less fluid for grade 2 cataracts (p < 0.001) and 25 mL (41%) less for grade 3 cataracts (p = 0.004). On average, sonic and thermal energy emission for phacoemulsification was 8.7 ± 8.9 cumulative dissipated energy units (CDE).
Additional intraoperative complications included iris damage and a wound leak requiring a stitch for one eye in the Phaco arm, as well as transient tissue incarceration within the wound (which resolved without incident) also in the Phaco arm. During one case, the MICOR device became clogged during lens extraction, requiring a replacement of the device. Secondary intraoperative procedures in the MICOR arm included the use of a Malyugin ring due to poor dilation in 2 eyes. In the Phaco arm, there was 1 anterior chamber washout due to a retained lens fragment, 3 eyes required trypan blue, 2 eyes required iris hooks, 2 eyes required miLOOP, and 1 eye required a Malyugin ring due to poor dilation and dense cataracts.
Discussion
As mentioned above, two previous studies have been published on outcomes of cataract surgery with the MICOR lensectomy device.6,7 These studies demonstrated that 1) the device can produce satisfactory vision outcomes and a low rate of complications,6 and 2) that the learning curve with MICOR can be overcome in less than 60 cases.7 On the other hand, the previous studies left an obvious knowledge gap in that they did not provide any direct comparison of the new technology to the standard of care, phacoemulsification. To our knowledge, this is the first study to compare the two technologies.
MICOR is not the first proposed alternative to phacoemulsification for lens fragmentation and extraction. Notably, the Aqualase device (Alcon Laboratories, Forth Worth, TX, USA) facilitated lens fragmentation by delivering micropulses of BSS. However, Aqualase ultimately did not gain traction, perhaps because conversion to phacoemulsification was required for dense (> 2+ NS) cataracts.8 In contrast, no conversion to phacoemulsification was required in the present study, and only a single case of voluntary conversion to phacoemulsification is reported in the literature due to a complication not attributed to lens fragmentation itself.7 MICOR has so far shown to be sufficient for managing dense cataracts up to 4+ NS.6
The choice of vision at day 1 as a primary outcome measure was derived from the belief that any observed differences between groups would be attributable to corneal edema, and that comparing VA at 1 week or 1 month would be less likely to reveal disparities.9 Importantly, we found no differences in post-operative day 1 UCVA, BCVA, or pinhole VA. These results are reassuring and help to earn the trust of surgeons with the new technology.
On the other hand, eyes in the MICOR group experienced significantly faster lens removal times than those in the Phaco group. Speed should never be considered an acceptable measure of success, at the expense of safety. However, assuming similar safety profiles, increased speed is an attractive result for surgeons that are focused on optimizing the patient experience and the reality of decreasing reimbursements from insurance.
Ianchulev et al reported lensectomy times 99 to 134 seconds faster than the times reported herein, for grades 1 and 3 cataracts, respectively. However, Ianchulev et al measured times from MICOR entry to MICOR removal, while the current study additionally included the time for cortex removal with I/A prior to IOL insertion. Second, the Ianchulev study pooled outcomes from twelve ambulatory surgical centers, whereas the present study only included outcomes from a single academic center. Thus, it is plausible that the cataract grades were, on average, softer in the Ianchulev study than in the present one. These differences likely explain the observed disparities in nucleus extraction time.
The present study also found that irrigation volume used in the MICOR group was nearly half that used in the Phaco group. Our findings (33 ± 9 mL) were consistent with those reported by Beniz et al (27 ± 7 mL) and Ianchulev (24 ± 8 mL for grades 2–3). The clinical significance of this finding is unclear. However, if we surmise that the 10–15% decrease in endothelial cell count observed with phacoemulsification is related to the irrigation volumes going through the eye during a case,3,10,11 it is plausible that use of MICOR could translate to lower levels of cell loss. Future work is needed to further scrutinize this hypothesis.
Conclusion
The strengths of this study include its prospective design and use of a surgeon experienced in both lensectomy techniques. On the other hand, the study is not without limitations. First, the small sample size limited power to detect other significant differences (ie, for lens removal time in grade 1 and grade 4 cataracts) between groups. Second, the non-randomized study design could have contributed to meaningful demographic differences between groups. For example, the poorer preoperative BCVAs, higher proportion of grade 3–4 cataracts (30% versus 18%) and higher incidence of secondary procedures in the Phaco group suggests that it included more complex cataracts than the MICOR group. This could have disproportionately worsened outcomes reported for phacoemulsification. Last, the use of a single surgeon and site may be viewed as both a strength and limitation. For one, having a single surgeon complete the procedure with both pieces of equipment, but with otherwise similar nucleus disassembly technique (pre-chop) and OR staff standardized the study and served as its own internal control. On the other hand, it limits generalizability of the results to other surgeons and practice settings.
In summary, MICOR offers a viable alternative to phacoemulsification, with similar immediate postoperative vision and safety outcomes, but perhaps with improved speed. Larger multi-center studies are needed to confirm the results found herein and further elucidate long-term complications and outcomes. For example, a future study incorporating specular microscopy is needed to evaluate whether differences in fluid volume used and heat generated impact endothelial cell loss. Similarly, macular optical coherence tomography (OCT) could be used to evaluate for differences in incidence of macular edema. The new technology also needs to be studied in specific populations, such as in eyes with Fuchs endothelial dystrophy (where cumulative dispersed ultrasound energy matters) or hyper-mature cataracts. There also may be compelling argument for MICOR in the developing world where its portability and sterility may be particularly advantageous when compared with phacoemulsification.
Ethics and Data Availability
This study was approved by Western IRB (SITE00001269) and adhered to tenets of the Declaration of Helsinki, as well as the Health Insurance Portability and Accountability Act. Patient consent was required for participation in the study. The trial is registered at clinicaltrials.gov (NCT05729477) and aggregated results will be posted there. Deidentified demographics and postoperative outcome measures on individual subjects are available upon written request by contacting the corresponding author for up to 3 years after publication.
Funding
This study was funded by Carl Zeiss Meditec, Jena, Germany.
Disclosure
Supported by Carl Zeiss Meditec, Jena, Germany. Nathan Cannon received consulting fees from Carl Zeiss Meditec related to the present work. Seth Pantanelli reports research support and consulting fees from Bausch & Lomb. Seth Pantanelli also reports research support and consulting fees from Carl Zeiss Meditec, both of which are related to the present work. The authors report no other conflicts of interest in this work.
References
1. Tabin G, Chen M, Espandar L. Cataract surgery for the developing world. Curr Opin Ophthalmol. 2008;19(1):55–59. doi:10.1097/ICU.0b013e3282f154bd
2. Khanna R, Pujari S, Sangwan V. Cataract surgery in developing countries. Curr Opin Ophthalmol. 2011;22(1):10–14. doi:10.1097/ICU.0b013e3283414f50
3. Kumar R, Wahi D, Tripathi P. Comparison of changes in endothelial cell count and central corneal thickness after phacoemulsification and small-incision cataract surgery: a prospective observational study at a tertiary care center of eastern Uttar Pradesh. Indian J Ophthalmol. 2022;70(11):3954–3959. doi:10.4103/ijo.IJO_1906_22
4. Sorensen T, Chan CC, Bradley M, Braga-Mele R, Olson RJ. Ultrasound-induced corneal incision contracture survey in the United States and Canada. J Cataract Refract Surg. 2012;38(2):227–233. doi:10.1016/j.jcrs.2011.08.039
5. ZEISS MICOR 700 specifications. Available from: https://www.zeiss.com/meditec/en/products/phaco-vitrectomy-lensfragmentation/zeiss-micor-700.html#accordionItem-756939286.
6. Ianchulev T, Yeu E, Hu EH, et al. First in-human clinical performance of a new non-cavitating handheld lensectomy system in 665 consecutive cataract surgeries. J Cataract Refract Surg. 2024;50(7):693–697. doi:10.1097/j.jcrs.0000000000001446
7. Beniz LAF, Chatzea MS, Zarei-Ghanavati S, Jammal AA, Yoo SH. Finger-Controlled Nonultrasonic Lens Extractor. J Cataract Refract Surg. 2024. doi:10.1097/j.jcrs.0000000000001561
8. Hughes E, Mellington F, Whitefield L. Aqualase for cataract extraction. Eye. 2007;21:191–194. doi:10.1038/sj.eye.6702162
9. Díez-Ajenjo MA, Luque-Cobija MJ, Peris-Martínez C, Ortí-Navarro S, García-Domene MC. Refractive changes and visual quality in patients with corneal edema after cataract surgery. BMC Ophthalmol. 2022;22(1):242. doi:10.1186/s12886-022-02452-5
10. Briceno-Lopez C, Burguera-Giménez N, García-Domene MC, Díez-Ajenjo MA, Peris-Martínez C, Luque MJ. Corneal edema after cataract surgery. J Clin Med. 2023;12(21):6751. doi:10.3390/jcm12216751
11. Sharma N, Singhal D, Nair SP, Sahay P, Sreeshankar SS, Maharana PK. Corneal edema after phacoemulsification. Indian J Ophthalmol. 2017;65(12):1381–1389. doi:10.4103/ijo.IJO_871_17
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.