Back to Journals » Risk Management and Healthcare Policy » Volume 18
A Randomized Controlled Study on the Application of LEARNS Health Education Combined with Intelligent Follow-up Management in Secondary Prevention of Ischemic Stroke and Its Impact on Patient Compliance and Neurological Function
Authors Chu R, Zhen X, Wang L, Zhang M, Shang M , Wang C, Liu J
Received 9 January 2025
Accepted for publication 2 July 2025
Published 10 July 2025 Volume 2025:18 Pages 2377—2386
DOI https://doi.org/10.2147/RMHP.S516608
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Kyriakos Souliotis
Rui Chu,1 Xue Zhen,2 Lei Wang,2 Min Zhang,3 Min Shang,4 Chao Wang,5 Jia Liu6
1The Third Ward of Medical Oncology Department, the First Affiliated Hospital of Qiqihar Medical College, Qiqihar, People’s Republic of China; 2Neurointerventional Ward, Department of Rehabilitation Medicine, the First Affiliated Hospital of Qiqihar Medical College, Qiqihar, People’s Republic of China; 3Department of Nursing, the First Affiliated Hospital of Qiqihar Medical College, Qiqihar, People’s Republic of China; 4Second Ward, Department of Neurology, the First Affiliated Hospital of Qiqihar Medical College, Qiqihar, People’s Republic of China; 5Qiqihar Medical College, Qiqihar, People’s Republic of China; 6Academic Affairs Department, The First Affiliated Hospital of Qiqihar Medical College, Qiqihar, People’s Republic of China
Correspondence: Jia Liu, Email [email protected]
Objective: This randomized controlled study aimed to evaluate the effectiveness of LEARNS health education combined with intelligent follow-up management in the secondary prevention of ischemic stroke (IS), focusing on patient compliance and neurological function outcomes. The LEARNS model is a structured patient education framework encompassing Listen, Establish, Adopt, Reinforce, Name, and Strengthen, aiming to support individualized and interactive patient learning.
Methods: A total of 120 first-episode IS patients admitted to the Neurology Department of our hospital from April to June 2024 were enrolled and randomly assigned to either a control group (n = 60), receiving conventional health education plus intelligent follow-up, or an observation group (n = 60), receiving LEARNS health education combined with intelligent follow-up management. Patient outcomes were assessed using the General Medication Adherence Scale (GMAS), secondary prevention control measures (including blood glucose, blood pressure, lipid control, smoking/alcohol cessation, obesity control, and exercise adherence), the Barthel Index (BI) for neurological function, and ischemic stroke recurrence. Evaluations were conducted at discharge and at all follow-up time points within six months post-discharge.
Results: Compared to the control group, the observation group showed significantly higher medication adherence rates, better control in all secondary prevention measures, and higher neurological function recovery rates at all follow-up time points (P < 0.05). Additionally, the 6-month recurrence rate was significantly lower in the observation group (1.67%) than in the control group (13.33%) (P < 0.05).
Conclusion: LEARNS health education combined with intelligent follow-up management effectively enhances patient compliance, improves secondary prevention outcomes, supports neurological recovery, and reduces recurrence risk in patients with ischemic stroke.
Keywords: LEARNS model, health education, intelligent follow-up, ischemic stroke, secondary prevention, medication adherence, neurological recovery
Introduction
Ischemic stroke (IS), an acute cerebrovascular event resulting from the obstruction of cerebral blood flow, remains one of the primary global causes of death and long-term disability.1 In China, recent epidemiological studies2 reveal that stroke has emerged as the leading health burden, with IS comprising over 70% of all stroke cases. Although substantial progress has been made in acute-phase treatments, IS patients are still highly susceptible to recurrent strokes, sustained neurological deficits, and compromised quality of life after discharge—posing significant burdens on both families and society. Consequently, preventing IS recurrence through effective secondary prevention has become a major priority in clinical and public health contexts.
Secondary prevention includes a range of strategies: blood pressure, glucose, and lipid control; smoking cessation and alcohol moderation; adherence to healthy dietary and exercise habits; strict medication compliance; and engagement in neurorehabilitation programs.3 Despite their proven effectiveness, these measures are often inadequately implemented in real-world settings. Many patients experience poor adherence and unhealthy lifestyle behaviors due to a lack of disease-specific education and structured guidance post-discharge.4 Factors such as fragmented follow-up systems, insufficient patient education, and weak self-management capabilities significantly undermine secondary prevention efforts.5 Therefore, the development of structured, integrated, and patient-centered intervention models is essential to bridge this gap and enhance long-term outcomes for IS patients.
The LEARNS health education model—comprising Listen, Establish, Adopt, Reinforce, Name, and Strengthen—is a patient-centered framework rooted in social constructivist theory. It emphasizes interaction, individualized learning, and empowerment, aiming to promote health literacy, self-efficacy, and disease-specific knowledge. Recent studies have demonstrated the model’s clinical utility: Zhang et al6 reported that LEARNS-based perioperative education significantly improved disease understanding and compliance in patients with laryngeal tumors; Zhao et al7 summarized high-level evidence supporting LEARNS-based rehabilitation guidance for post-stroke motor dysfunction; and Martin et al8 validated learner-centered strategies—aligned with the LEARNS principles—for enhancing communication and patient engagement in chronic disease management.
Meanwhile, intelligent follow-up management systems, enabled by mobile health (mHealth) technologies and data analytics, offer tools for personalized care planning, remote monitoring, and behavioral reinforcement.9–11 These systems can help overcome traditional limitations in continuity of care and improve patient engagement. While both LEARNS education and intelligent follow-up have shown individual promise, their synergistic application in IS secondary prevention remains underexplored.
Therefore, this study investigates whether the combined use of LEARNS health education and intelligent follow-up management yields superior outcomes in medication adherence, neurological function, and recurrence prevention compared to conventional management. We hypothesize that IS patients receiving this integrated intervention will demonstrate significantly improved adherence, clinical indicators, neurological recovery, and reduced recurrence. A randomized controlled trial involving 120 first-episode IS patients is conducted to provide evidence-based guidance for long-term secondary prevention practices in stroke care.
Materials and Methods
Study Design
This was a single-center, prospective, randomized controlled trial (RCT) conducted to evaluate the effect of LEARNS health education combined with intelligent follow-up management on secondary prevention outcomes in patients with IS.
Participants and Inclusion Criteria
A total of 120 patients who were first-time inpatients at the Neurology Department of our hospital between April and June 2024, and diagnosed with IS, were recruited. Inclusion criteria were as follows: (1) Met the diagnostic criteria of the Guidelines for the Diagnosis and Treatment of Acute Ischemic Stroke in China (2022);12 (2) Completed a 6-month follow-up with complete and valid clinical data; (3) Aged between 18 and 80 years; (4) Possessed basic communication ability (verbal or assisted), sufficient to complete the intervention and follow-up assessments; (5) Provided informed consent and voluntarily agreed to participate in the study. Exclusion criteria were as follows: (1) Diagnosed with severe cognitive impairment, as assessed by a Mini-Mental State Examination (MMSE)13 score < 18; (2) Severe comorbidities such as congenital heart disease or uncontrolled hypertension; (3) Severe visual or auditory impairment that could not be corrected or compensated for and would hinder participation in education or follow-up activities; (4) Substance or alcohol dependence; (5) Active malignant tumors; (6) Autoimmune diseases; (7) Pregnancy or lactation.
Sample Size Calculation
The sample size was estimated using G*Power 3.1.9.7 software. Assuming a medium effect size (Cohen’s d = 0.5), an α level of 0.05, and a power (1–β) of 0.80 for a two-tailed test, the minimum sample size required per group was calculated as 51. Considering a potential 15% dropout rate, we enrolled 60 participants in each group (total 120).
Randomization and Blinding
Randomization was conducted using a computer-generated random number sequence created by an independent statistician. Participants were randomly assigned in a 1:1 ratio into either the control group (n = 60) or the observation group (n = 60) using block randomization with a block size of 4 to ensure group balance throughout the enrollment period.
Although stratified randomization based on baseline stroke severity (eg, NIHSS score) was considered, it was not implemented due to the relatively small sample size and the similar distribution of baseline characteristics in the study population.
To ensure allocation concealment, group assignments were placed in sequentially numbered, sealed, opaque envelopes, which were prepared and opened by a third-party research coordinator who was not involved in the intervention delivery or outcome evaluation.
Due to the nature of the health education intervention, neither participants nor the healthcare providers could be blinded to the treatment allocation. However, outcome assessors and data analysts were blinded to group assignments to minimize observer bias and analysis bias.
Ethical Considerations
This study was reviewed and approved by the Medical Ethics Committee of The First Affiliated Hospital of Qiqihar Medical College (Approval No. 2024–005-01). All patients and their families were fully informed of the study objectives, procedures, potential risks, and benefits. Written informed consent was obtained from all participants. The study complied with the principles of the Declaration of Helsinki (as revised in 2013).
Methods
Secondary prevention strategies were implemented in accordance with the Chinese Guidelines for Secondary Prevention of Cerebrovascular Diseases.14 Data were collected via electronic medical records and semi-structured interviews, including demographics, neurological recovery, blood pressure, blood glucose and lipid levels, and health behavior metrics. Personalized patient health records were established.
Control group (routine health education + intelligent follow-up): Patients received standard hospital-based health education on disease knowledge, medication use, lifestyle modification, and warning signs, delivered through brochures and in-person nurse counseling during hospitalization. After discharge, intelligent follow-up was conducted using the “3+1” model, which included regular reminders and check-ins via WeChat, SMS, intelligent voice system, and monthly manual phone calls. The frequency and interaction time were matched with those of the observation group to control for attention bias.
Observation group (LEARNS health education + intelligent follow-up): In addition to the above, patients received the LEARNS-based intervention. The intervention consisted of six modules: (1) Listen: Upon admission, semi-structured interviews explored patients’ individualized needs, preferences for health education formats, and expectations. (2) Establish: After consent, personal recovery plans were created collaboratively with patients and caregivers, emphasizing patient-provider partnership. (3) Adopt: The hospital information center maintained the intelligent follow-up system. Educational materials (videos, audio, text, infographics) were pushed at scheduled intervals post-discharge. Patients were required to complete at least 80% of the assigned educational content, and system logs were used to track engagement and adherence. (4) Reinforce: Encouragement messages and peer support via WeChat groups were offered weekly. Family members were also invited to participate, reinforcing knowledge and behavioral change. (5) Name: Patient responses to follow-up questionnaires were automatically categorized. Based on the feedback, staff adjusted education strategies and follow-up intensity. (6) Strengthen: Key areas of misunderstanding or noncompliance were addressed through individualized coaching and reinforced during follow-up contacts.
To reduce the “contact effect”, both groups received an equal number of interactions, similar communication formats, and contact duration over the 6-month intervention period.
Observation Indicators and Evaluation Criteria
(1) Medication Adherence: At discharge (T0), and at 1 month (T1), 3 months (T2), and 6 months (T3) post-discharge, patients’ medication adherence was assessed using the General Medication Adherence Scale (GMAS).15 The GMAS is a validated tool that comprehensively evaluates medication-taking behaviors, beliefs, and barriers, and has demonstrated good reliability and construct validity in chronic disease populations, including stroke patients. Scores were categorized into high (29–33), moderate (17–28), and low (0–16) adherence. The medication adherence rate was calculated as: Medication adherence rate = (number of patients with high adherence + number with moderate adherence) / total number of patients × 100%.
(2) Secondary Prevention Control: At T0, T1, T2, and T3, the following indicators were assessed: ① Blood glucose: Fasting 4.4–6.1 mmol/L, 2-hour postprandial 6.1–11.1 mmol/L, HbA1c <7%. ② Blood pressure: SBP <140 mmHg, DBP <90 mmHg. ③ Blood lipids: TC <5.2 mmol/L, LDL-C <3.12 mmol/L. ④ Smoking and alcohol: Non-smoking and alcohol <25 g/day. ⑤ Obesity control: Overweight/obese patients aimed to reduce weight by 10%; others maintained a normal BMI. ⑥ Exercise: Aerobic activity 3–4 times/week, about 40 minutes/session.
(3) Neurological Recovery: Neurological function was assessed using the Barthel Index (BI)16 at T0, T1, T2, and T3. The BI is a widely used and validated scale that assesses the performance of activities of daily living (ADL) and reflects the degree of functional independence. It is recommended in stroke rehabilitation guidelines due to its sensitivity to changes in functional status over time. Patients scoring at Level 1 or Level 2 were considered to have good neurological recovery.
(4) IS Recurrence: During the 6-month follow-up, medical staff monitored recurrence of ischemic stroke through clinical reexamination and patient/family reporting.
Data Completeness: No participants were lost to follow-up, and all outcome data were complete; therefore, no imputation or special handling for missing data was required.
Statistical Analysis
GraphPad Prism 8 was used for charting, and SPSS 22.0 software for data analysis.
Categorical data: Expressed as percentages (%) and analyzed using the χ²-test. Continuous data: Expressed as ( ), with independent sample t-tests for comparisons between groups. A p-value <0.05 was considered statistically significant.
), with independent sample t-tests for comparisons between groups. A p-value <0.05 was considered statistically significant.
Results
Comparison of Baseline Information
The baseline information, including gender, age, body mass index (BMI), comorbidities, neurological function, and education level, was compared between the two groups (P > 0.05), indicating comparability. See Tables 1 and 2.
 |
Table 1 Barthel Index (BI) Evaluation Standards |
 |
Comparison of Medication Adherence
In the control group, the numbers of patients adhering to medication at T0, T1, T2, and T3 were 48 (80.00%), 45 (75.00%), 42 (70.00%), and 40 (66.67%), respectively. In the observation group, the numbers were 56 (93.33%), 54 (90.00%), 53 (88.33%), and 51 (85.00%), respectively. The medication adherence rates at T0, T1, T2, and T3 in the observation group were significantly higher than those in the control group (P < 0.05). See Figure 1.
 |
Figure 1 Comparison of Medication Adherence [n (%)]. Note: Comparison between groups at the same time points, *P < 0.05. |
Comparison of Secondary Prevention Control
The rates of glucose control, blood pressure control, lipid control, smoking cessation/alcohol restriction, obesity control, and exercise compliance at T0, T1, T2, and T3 in the observation group were significantly higher than those in the control group (P < 0.05). See Table 3.
 |
Table 3 Comparison of Secondary Prevention Control [n (%)] |
Comparison of Neurological Function Recovery
In the control group, the numbers of patients with good neurological recovery at T0, T1, T2, and T3 were 32 (53.33%), 35 (58.33%), 37 (61.67%), and 38 (63.33%), respectively. In the observation group, the numbers were 43 (71.67%), 47 (78.33%), 50 (83.33%), and 51 (85.00%), respectively. The rates of good neurological recovery at T0, T1, T2, and T3 in the observation group were significantly higher than those in the control group (P < 0.05). See Figure 2.
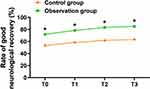 |
Figure 2 Comparison of Neurological Function Recovery [n (%)]. Note: Comparison between groups at the same time points, *P < 0.05. |
Comparison of Recurrence Rates
Among the 60 patients in the control group, 8 experienced recurrence; in the observation group, only 1 experienced recurrence. The 6-month recurrence rate in the observation group (1.67%) was significantly lower than that in the control group (13.33%) (P < 0.05). See Figure 3.
 |
Figure 3 Comparison of Recurrence Rates [n (%)]. Note: Comparison between groups at the same time points, *P < 0.05. |
Discussion
IS, as a prevalent neurological disease, is characterized by a high disability and recurrence rate, making secondary prevention a critical aspect of long-term management.17 However, in clinical practice, secondary prevention management of patients faces numerous challenges, including poor medication adherence, inadequate control of risk factors, and insufficient patient awareness of disease management. These issues not only limit the effectiveness of secondary prevention but also significantly increase the risk of recurrence and disability.18,19 Therefore, exploring more efficient and comprehensive intervention strategies has become a crucial task to enhance the effectiveness of secondary prevention for IS. The combination of LEARNS health education and intelligent follow-up management provides an innovative intervention pathway. LEARNS health education is patient-centered and aims to enhance patients’ awareness of disease and self-management ability through targeted health education and behavioral change support.20 Intelligent follow-up management, leveraging real-time and intelligent features of information technology, provides personalized feedback support for patients.21 The combination of these approaches not only addresses the limitations of single interventions but also forms a multidimensional, comprehensive management model, offering robust theoretical support for improving the effectiveness of secondary prevention in patients.
Studies22 have shown that medication adherence is a key factor influencing the long-term management outcomes of IS patients. This study revealed that patients receiving the combined intervention of LEARNS health education and intelligent follow-up management (observation group) demonstrated significantly higher medication adherence rates across all four time points compared to the control group (P < 0.05). This result highlights the effectiveness of the combined intervention in improving patients’ medication behaviors through innovative measures. Firstly, LEARNS health education adopts personalized strategies in medication education by engaging in-depth communication with patients to identify their concerns and doubts about pharmacological treatment, thereby developing tailored educational content. This educational approach emphasizes two-way interaction, enhancing patients’ understanding of the necessity of medication and reducing the likelihood of treatment discontinuation due to misunderstandings.23 Secondly, intelligent follow-up management uses technological tools to push medication reminders and monitor patients’ medication behaviors through data feedback, enabling timely corrections and fostering regular medication habits. Finally, the intervention also emphasizes family involvement, further consolidating patients’ medication adherence through family support. Regarding improvements in secondary prevention control, this study demonstrated that the observation group showed significantly better control rates in blood glucose, blood pressure, blood lipids, smoking cessation, alcohol limitation, obesity control, and physical activity compared to the control group (P < 0.05). These findings underscore the unique advantages of the combined intervention model in risk factor management. LEARNS health education systematically educates patients on the potential impact of various risk factors on stroke recurrence. For instance, in blood glucose control, the educational content emphasizes the importance of monitoring glucose levels and provides specific dietary and pharmacological adjustment plans. Similarly, for blood lipid and blood pressure management, the approach illustrates the risks of hyperlipidemia and hypertension through examples and offers practical intervention suggestions. Moreover, the combined intervention focuses on guiding healthy behaviors, such as creating exercise plans tailored to patients’ conditions and highlighting the positive effects of smoking cessation and alcohol limitation on health.
The scheduled monitoring function of intelligent follow-up management provides assurance for the control of risk factors, enabling healthcare professionals to promptly adjust intervention strategies based on the data, thereby achieving individualized management. This closed-loop health management model effectively enhances patients’ control over risk factors, laying a foundation for reducing recurrence risks.
Neurological function recovery is an essential metric for evaluating rehabilitation outcomes in IS patients.24 The study demonstrated that the Barthel Index scores for neurological recovery in the observation group were significantly higher than those in the control group (P < 0.05), indicating that the combined intervention significantly promotes functional recovery, consistent with previous research.25,26 This effect is attributed to several factors. LEARNS health education provides scientific guidance to help patients better complete rehabilitation training. Additionally, psychological support, as part of the education, helps patients build confidence in rehabilitation and mitigates the adverse effects of anxiety and depression on recovery processes.27 Intelligent follow-up systems support rehabilitation training by sending reminders, recording patients’ training progress, and adjusting training content based on feedback data, ensuring the scientific validity and feasibility of rehabilitation plans. Previous studies28 have shown that dynamic management models improve patients’ training adherence and promote sustained improvements in functional recovery, corroborating the findings of this study. Stroke recurrence is a critical issue affecting patient prognosis. This study found that the recurrence rate within six months in the observation group was 1.67%, significantly lower than the control group’s 13.33% (P < 0.05). This result demonstrates that the combined intervention model effectively reduces the risk of stroke recurrence. Effective control of risk factors is fundamental to reducing recurrence rates.29,30 The integration of LEARNS health education and intelligent follow-up management significantly improved patients’ indicators such as blood pressure, blood glucose, and blood lipids. Moreover, the long-term adherence to healthy behaviors (eg, smoking cessation, alcohol limitation, physical activity) further reduced recurrence risk. Mechanistically, LEARNS health education enhances patients’ comprehensive understanding of the disease and its management, increasing their willingness to actively participate in health management. Intelligent follow-up, through dynamic monitoring and data analysis, provides real-time decision-making support for patients and healthcare providers, ensuring timely adjustments to interventions. This bidirectional mechanism effectively lowers recurrence risks.
The results of this study offer new insights into secondary prevention management models for IS patients. The combined intervention of LEARNS health education and intelligent follow-up management significantly improved medication adherence, enhanced risk factor control, promoted functional recovery, and reduced recurrence rates, providing robust support for optimizing post-stroke care. The intervention’s comprehensive and individualized characteristics make it highly suitable for clinical use. However, this study has some limitations. First, the relatively small sample size and single-center design may limit the generalizability of the findings. Furthermore, while this study evaluated outcomes over a 6-month follow-up period, it is worth noting that the behavioral foundation established through the LEARNS-based intervention may exert a more enduring impact. The LEARNS model fosters long-term behavior change by promoting patient engagement, empowering individuals with disease-related knowledge, and reinforcing goal-oriented self-management strategies. These changes are not merely temporary improvements but may be internalized into patients’ daily routines, leading to sustained medication adherence, regular monitoring, and healthier lifestyles. The intelligent follow-up component further enhances this process by providing continuous feedback and adaptive support, helping patients maintain behavioral momentum and prevent relapse. Therefore, the integrated approach is not only effective in the short term but also has the potential to support long-term secondary prevention. Future studies with extended observation periods are needed to verify these long-term effects.
Conclusion
The combined LEARNS health education and intelligent follow-up management model demonstrates significant benefits in the secondary prevention of ischemic stroke. It offers an innovative, feasible, and patient-centered strategy for improving post-stroke recovery, medication adherence, and recurrence control. This approach shows promise not only for hospital-based management but also for integration into community and home-based care settings. In future research, this model may be adapted and tested in the management of other chronic diseases, potentially broadening its scope and impact in chronic care.
Acknowledgments
An unauthorized version of the Chinese MMSE was used by the study team without permission, however this has now been rectified with PAR. The MMSE is a copyrighted instrument and may not be used or reproduced in whole or in part, in any form or language, or by any means without written permission of PAR (www.parinc.com).
Funding
Qiqihar Science and Technology Bureau Joint guidance project, Item number:LSFGG-2024074.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zhou H, Wang SW, Shi JC, et al. [Effect of diurnal temperature range on the number of elderly inpatients with ischemic stroke in Hunan Province]. Zhonghua Yu Fang Yi Xue Za Zhi. 2023;57(4):528–534.
2. Zhang GB, Huang HW, Guo W. [Prevention and treatment of stroke in Chinese and African young adults]. Zhonghua Yu Fang Yi Xue Za Zhi. 2022;56(8):1142–1149. doi:10.3760/cma.j.cn112150-20220104-00008
3. Luo Y, Li YR. [Application prospects of blood biomarkers in secondary prevention of ischemic stroke]. Zhonghua Yu Fang Yi Xue Za Zhi. 2022;56(8):1062–1068. doi:10.3760/cma.j.cn112150-20220321-00270
4. Wang X, Li Y, Li J, et al. [Medication compliance for secondary prevention and long-term outcome among patients with acute coronary syndrome after percutaneous coronary intervention in different regions]. Zhonghua Xin Xue Guan Bing Za Zhi. 2021;49(2):143–149. doi:10.3760/cma.j.cn112148-20200528-00442
5. Shirokov EA. [Modern strategies for the management of patients who have suffered ischemic stroke or transient ischemic attack]. Zh Nevrol Psikhiatr Im S S Korsakova. 2023;123(12. Vyp. 2):61–67. doi:10.17116/jnevro202312312261
6. Zhang B, Sun Q, Hu S, et al. LEARNS model as perioperative education strategy for patients with laryngeal tumors. Evid Based Complement Alternat Med. 2022;2022:3360966. doi:10.1155/2022/3360966
7. Zhao H, Zhou L, Hu L, et al. Summary of best evidence for rehabilitation management of patients with motor dysfunction after stroke. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2024;49(4):497–507. doi:10.11817/j.issn.1672-7347.2024.240006
8. Martin A, Weller I, Amsalem D, et al. Co-constructive patient simulation: a learner-centered method to enhance communication and reflection skills. Simul Healthc. 2021;16(6):e129–e135. doi:10.1097/SIH.0000000000000528
9. Tsimane TA, Downing C. A model to facilitate transformative learning in nursing education. Int J Nurs Sci. 2020;7(3):269–276. doi:10.1016/j.ijnss.2020.04.006
10. Huang C, Zhou Y, Fang Y, et al. [Research progress of comprehensive follow-up management strategy on the natural history of simultaneous, persistent multiple pulmonary ground-glass nodules]. Zhongguo Fei Ai Za Zhi. 2024;27(9):691–696. doi:10.3779/j.issn.1009-3419.2024.106.25
11. Yadav SK, Jha CK, Mishra SK, et al. Smartphone-Based Application for Tele-follow-up of Patients with Endocrine Disorders in Context of a LMIC: a Compliance, Satisfaction, Clinical Safety and Outcome Assessment. World J Surg. 2020;44(2):612–616. doi:10.1007/s00268-019-05212-7
12. Mead GE, Sposato LA, Sampaio Silva G, et al. A systematic review and synthesis of global stroke guidelines on behalf of the World Stroke Organization. Int J Stroke. 2023;18(5):499–531. doi:10.1177/17474930231156753
13. Peng YZ, Shuai D, Zhou CM, Yuan J, Zha Y. [Association between extracellular water/body cell mass ratio and cognitive impairment in patients on maintenance hemodialysis]. Zhonghua Yi Xue Za Zhi. 2023;103(32):2522–2528. Chinese. doi:10.3760/cma.j.cn112137-20230403-00531
14. Fan Y, Yu J, Chen H, et al. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of cerebral venous sinus thrombosis. Stroke Vasc Neurol. 2020;5(2):152–158. doi:10.1136/svn-2020-000358
15. Sendekie AK, Netere AK, Kasahun AE, Belachew EA. Medication adherence and its impact on glycemic control in type 2 diabetes mellitus patients with comorbidity: a multicenter cross-sectional study in Northwest Ethiopia. PLoS One. 2022;17(9):e0274971. doi:10.1371/journal.pone.0274971
16. Hu SJ, Fu SS, Zhu LL, et al. [Therapeutic effect of intravenous thrombolysis with tenecteplase on patients with post awakening branch atheromatous disease]. Zhonghua Yi Xue Za Zhi. 2024;104(23):2173–2178. doi:10.3760/cma.j.cn112137-20231110-01054
17. Zhou J, Fu Y-B, Song Y-Q, et al. Progress of researches on mechanisms of acupuncture for secondary prevention of ischemic stroke. Zhen Ci Yan Jiu. 2024;49(6):625–633. doi:10.13702/j.1000-0607.20230142
18. Pyshkina LI, Tyazhelnikov AA, Kabanov AA, et al. [Risk factors and adherence to treatment of patients with cerebrovascular diseases]. Zh Nevrol Psikhiatr Im S S Korsakova. 2023;123(8. Vyp. 2):84–89. doi:10.17116/jnevro202312308284
19. Kulesh AA, Yanishevskiy SN, Demin DA, et al. [Optimization of secondary prevention in patients with high-risk atherothrombotic ischemic stroke or transient ischemic attacks]. Zh Nevrol Psikhiatr Im S S Korsakova. 2023;123(6):36–43. doi:10.17116/jnevro202312306136
20. Stanley MJ, Hall K. A paradigm shift for the nursing education model: a scoping review. J Nurs Educ. 2024;63(3):141–147. doi:10.3928/01484834-20240108-08
21. Rabin A, Chechik O, Maman E, et al. Adherence of patients to methods of self-reduction of shoulder dislocation taught via smartphones: a medium-term follow-up survey. Wilderness Environ Med. 2024;35(3):266–270. doi:10.1177/10806032241249453
22. Iglseder B, Mutzenbach JS. [Prevention of ischemic stroke in old age]. Z Gerontol Geriatr. 2024;57(5):402–410. doi:10.1007/s00391-024-02336-x
23. Duevel JA, Elkenkamp S, Gensorowsky D, et al. A case management intervention in stroke care: evaluation of a quasi-experimental study. Z Evid Fortbild Qual Gesundhwes. 2024;187:69–78. doi:10.1016/j.zefq.2024.03.008
24. Xia Y, Liu H, Zhu R. Risk factors for stroke recurrence in young patients with first-ever ischemic stroke: a meta-analysis. World J Clin Cases. 2023;11(26):6122–6131. doi:10.12998/wjcc.v11.i26.6122
25. Fruhwirth V, Enzinger C, Weiss E, et al. [Use of smartphone apps in secondary stroke prevention]. Wien Med Wochenschr. 2020;170(1–2):41–54. doi:10.1007/s10354-019-00707-3
26. Elfghi M, Jordan F, Dunne D, et al. The effect of lifestyle and risk factor modification on occlusive peripheral arterial disease outcomes: standard healthcare vs structured programme-for a randomised controlled trial protocol. Trials. 2021;22(1):138. doi:10.1186/s13063-021-05087-x
27. Kontou E, Kettlewell J, Condon L, et al. A scoping review of psychoeducational interventions for people after transient ischemic attack and minor stroke. Top Stroke Rehabil. 2021;28(5):390–400. doi:10.1080/10749357.2020.1818473
28. Meuzelaar RR, den Hartog FPJ, Verleisdonk EJMM, et al. Feasibility of a smartphone application for inguinal hernia care: a prospective pilot study. Updates Surg. 2023;75(4):1001–1009. doi:10.1007/s13304-023-01455-1
29. Fukuoka Y, Hosomi N, Hyakuta T, et al. Effects of a disease management program for preventing recurrent ischemic stroke. Stroke. 2019;50(3):705–712. doi:10.1161/STROKEAHA.118.020888
30. Dalli LL, Andrew NE, Kim J, et al. Understanding of medications and associations with adherence, unmet needs, and perceived control of risk factors at two years post-stroke. Res Social Adm Pharm. 2022;18(9):3542–3549. doi:10.1016/j.sapharm.2022.01.007
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Impact of Evidence-Based Nursing Interventions on Recovery in Traumatic Brain Injury Patients Undergoing Hematoma Evacuation
Qi A, Li P
Journal of Multidisciplinary Healthcare 2025, 18:973-981
Published Date: 19 February 2025
Follow-Up in Primary Care After Ischemic Stroke – Insights From the Nor-COAST Study

Sande IS, Helgheim KL, Saltvedt I, Røsstad TG, Spigset O, Ellekjær H, Gynnild MN
International Journal of General Medicine 2025, 18:2141-2150
Published Date: 15 April 2025
Long-Term Benefits of N-Butylphthalide in Preventing Ischemic Stroke Recurrence: A 12-Month Prospective Study
Liu W, Shao Y, Liu J, Hao J, Lu Y, Yang L, Wang J, Ning X
Therapeutics and Clinical Risk Management 2025, 21:781-792
Published Date: 27 May 2025


