Back to Journals » Clinical Ophthalmology » Volume 18
An Open-Label, Phase III Study to Assess the Efficacy and Safety of Cysteamine Ophthalmic Solution 0.55% in Japanese Cystinosis Patients
Authors Goi N , Iwata F, Sugihara Y, Higa S , Chikama T
Received 24 June 2024
Accepted for publication 1 November 2024
Published 25 November 2024 Volume 2024:18 Pages 3457—3471
DOI https://doi.org/10.2147/OPTH.S479770
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Nobuhiro Goi,1 Fumino Iwata,2 Yoko Sugihara,3 Shingo Higa,1 Taiichiro Chikama4
1Medical Affairs, Viatris Pharmaceuticals Japan G.K., Tokyo, Japan; 2Iwata Eye Clinic, 2-15-21 Nishinakanobu, Shinagawa-ku, Tokyo, 142-0054, Japan; 3Global Clinical Operations, Viatris Pharmaceuticals Japan G.K., Tokyo, Japan; 4Department of Ophthalmology and Visual Science, Graduate School of Biomedical and Health Sciences, Hiroshima University, 1-2-3 Kasumi, Minami-ku, Hiroshima, 734-8551, Japan
Correspondence: Nobuhiro Goi, Viatris Pharmaceuticals Japan G.K., Azabudai Hills Mori JP Tower 1-3-1 Azabudai Minato-ku, Tokyo, 106-0041, Japan, Tel +81-70-2180-4803, Email [email protected]
Purpose: Corneal cystine accumulation results in photophobia and affects patients’ quality of life. We assessed the efficacy and safety of cysteamine 0.55% solution in Japanese cystinosis patients with corneal cystine crystals for 52 weeks.
Patients and Methods: This was a Phase III, open-label, single-arm study conducted in Japan (jRCT2021200029; registered on 07/12/2020). Patients with white blood cell cystine levels > 1 nmol/half-cystine/mg protein or presence of corneal cystine crystal deposits identified by slit-lamp biomicroscopy were included. The primary endpoint was assessed as the in vivo confocal microscopy (IVCM) total score of 7 corneal layers. Visual acuity, photophobia and safety (adverse events [AEs]) endpoints were also evaluated.
Results: Six patients (four males and two females) were included. The mean age (standard deviation [SD]) of the patients was 29.0 (10.30) years, with a mean treatment duration of 13.7 (0.52) months. Although the acquisition of the IVCM total score was limited, an overall downward trend was observed in IVCM scores for each layer of the cornea. A decrease in the average of smoothed intensity was observed in four out of six patients at Week 16. Most patients reported at least 1-step improvement in physician and patient-reported photophobia assessment. Thirty-three AEs were reported in five patients (83.3%). Three patients (50.0%) reported eye and general disorders and administration site conditions. Tingling sensation was the most frequently reported local adverse drug reaction. No serious AEs or deaths were reported.
Conclusion: Cysteamine eye drops were efficacious and well tolerated in the Japanese cystinosis patients with corneal cystine crystals.
Keywords: cystine, clinical trial, corneal crystals, IVCM total score, photophobia, Japan
Introduction
Cystinosis is a rare autosomal recessive lysosomal storage disorder caused by mutations in the cystinosin gene (CTNS) on chromosome 17.1,2 CTNS encodes a membrane transporter protein, cystinosin, which exports lysosomal cystine into the cytoplasm. This protein’s dysfunction results in cystine crystals accumulating throughout the body, leading to multiple organ damage.1,2
The prevalence of CTNS gene mutations has primarily been reported in European and North American populations3–6 and rarely in the Asian and Middle Eastern populations, including Japan, due to the absence of the 57-kb Northern European founder deletion in the CTNS gene.7,8
The worldwide prevalence of cystinosis is estimated to be 1/100,000–200,000 live births.2 A considerably lower incidence of cystinosis was reported in Japan.9 The severe form of cystinosis, which manifests as infantile nephropathic cystinosis, affects 95% of children by 6–12 months of age.7 The less severe forms are juvenile nephropathic cystinosis and ocular non-nephropathic cystinosis, which manifests in late childhood or adolescence and adulthood, respectively.7,10 Adult, ocular non-nephropathic cystinosis is mainly identified by photophobia due to cystine crystals in the cornea.11 Ocular deposition of cystine crystals starts in the anterior segment of the eye (in the cornea and conjunctiva) and gradually progresses towards the posterior segment.12,13 The visual manifestations include photophobia, blepharospasm, corneal ulcer, superficial keratopathy, and band keratopathy.14 When left untreated, ocular cystinosis can lead to vision loss, eventually necessitating keratoplasty.15,16
Over the last 20 years, aminothiol cysteamine has been used to treat cystinosis.17 Cornea being an avascular tissue, oral cysteamine is ineffective in treating corneal symptoms as the corneal tissues do not absorb it.18 The failure of oral cysteamine in treating ocular cystinosis, which was effective in treating nephropathic cystinosis, necessitated the development of topical cysteamine.18–21 Topical cysteamine is effective for lysis of cystine crystals in the cornea and helps reduce corneal crystal density and photophobia.14,21,22 In 2012, the Food and Drug Administration approved a 0.44% cysteamine with 0.01% benzalkonium chloride formulation.18 Similarly, a 0.55% cysteamine hydrochloride (CH) topical formulation was found to have optimal performance when sodium hyaluronate was used as a vehicle.23 In Europe, a viscous formulation of 0.55% CH (equivalent to 0.37% cysteamine), CYSTADROPS®, Recordati Rare Diseases SARL, was approved in 2017,24 and subsequently also approved in the United States in 2020.25 In addition, Cystadrops Ophthalmic Solution, Viatris Pharmaceuticals G.K., was approved in Japan in 2024.26
In vivo confocal microscopy (IVCM) is the gold standard for quantification of cystine crystals in corneal layers.27 Topical cysteamine has improved the IVCM score from baseline to Month 48.28 In a study by Labbé et al, 0.55% CH significantly reduced the IVCM score by 29.9 ± 26.29% (p=0.001) compared to 0.1% CH eye drop, administered 4 times daily.28 Liang et al demonstrated a significant change in the mean scores of IVCM from baseline to Day 90 in the 0.55% CH group (−4.6 ± 3.1) versus the 0.10% CH group (−0.46 ± 3.38; p < 0.0001). Photophobia was also significantly improved in the 0.55% CH group.29 Although oral drugs containing cysteamine tartrate with the lytic action of intracellular cystine crystals in vascularized structures have been approved in Japan for nephrogenic cystinosis,30 it was ineffective in treating cystine crystals accumulated in the cornea. Hence, a 0.55% ophthalmic cysteamine solution developed by Recordati Rare Diseases SARL was tested in a Phase I study in Japanese adult men and was well tolerated (Data on file).
Since cystinosis is a rare disease, no data on the efficacy and safety of CH are available in Japan. Here, we evaluated the efficacy and safety of a 0.55% ophthalmic solution of cysteamine in Japanese patients presenting with corneal cystine crystals.
Materials and Methods
Study Design and Participants
This was a Phase III, open-label, single-arm study (jRCT2021200029; registered on 07/12/2020) conducted between January 2021 to April 2022 across multiple centers in Japan.
The study was conducted based on the principles of the Declaration of Helsinki (revised on October 19, 2013) and the standards specified in Article 14, Article 3, and Article 80 (2) of the Law Concerning Quality, Efficacy, and Safety of Clinical Trial Protocols, Pharmaceuticals, and Medical Devices and Good Clinical Practice (Ministry of Health and Welfare dated March 27, 1997) implemented in compliance with Order No. 28 and its amended ministerial ordinance and other relevant notices.
Patients were informed of the objectives, methods, duration, nature of drug, effects, anticipated adverse reactions, etc of the study, and voluntary written consent to participate in the study was obtained for all patients before study entry. The respective ethics committees of the study centers (All Tohoku Clinical Trial Review and Audit Organization (ACTIVATO), Yokohama City University Medical Center Institutional Review Board, and Japan Community Health Care Organization Chukyo Hospital Institutional Review Board) approved the study.
Patients with cystinosis, demonstrated by either white blood cell cystine levels >1 nmol/half-cystine/mg protein before the initiation of treatment with oral cysteamine or the presence of corneal cystine crystal deposits identified by slit-lamp biomicroscopy at screening were included. For study inclusion, patients also had to meet the following inclusion criteria: patients willing to comply with 4 doses of the investigational product per day for the study, patients for whom the principal investigator or a sub-investigator ascertains that they can adhere to the protocol-defined procedures, and patients or legally accepted representatives (if minor) who were willing to provide informed consent before study initiation.
Excluded patients were ones who received cysteamine ophthalmic solution within 1 year before administration of the investigational product, those with uncontrolled liver, heart, and neurological diseases and complications of malignancy, history of hypersensitivity to cysteamine, benzalkonium chloride, edetate disodium, carmellose sodium, citrate monohydrate, and penicillamine, patients with alcohol or drug dependence or a history of substance abuse, pregnant women or possibly pregnant or breastfeeding, those of childbearing potential without adequate contraception (eg complete abstinence, condoms, diaphragms, intrauterine devices, or oral contraceptives) and those who participated in a clinical or post-marketing study within 4 months before ophthalmic solution administration.
Treatment and Administration
The study product comprised A0003, an ophthalmic solution of 0.55%, containing 3.8 mg of cysteamine in 1 mL dosage form. This was a fixed-dose study in which the cysteamine ophthalmic suspension of 0.55% was administered four times daily (4-hour intervals) as a single drop in both eyes or to either eye per the treatment requirement over 52 weeks.
In the absence of treatments for conditions resulting from the accumulation of cystine in the cornea in Japan, it was considered that active drugs could not be used as a control. Using a placebo was considered ethically unsuitable; thus, the study used a single arm.
Endpoints and Assessments
The primary efficacy endpoint was comprehensive scoring of crystal density of 7 layers of the cornea (superficial epithelium, basal epithelium, Bowman’s membrane, stroma [shallow, middle, and deep layers], endothelium) measured using IVCM global score (IVCM total score). The IVCM total score was measured at baseline (8 weeks before the study initiation), then during the follow-up at 13–16 weeks, and 49–52 weeks after ophthalmic solution administration. Details of IVCM measurements are presented in Supplementary Methods 1.
The secondary endpoints were the assessment of luminous waveform (anterior segment optical coherence tomography [AS-OCT]) of corneal cystine crystals and photophobia severity assessed by the physicians and patients. Additional details are in Supplementary Methods 2 and 3. These endpoints were measured at baseline (8 weeks before the study initiation) and during follow-up after the study initiation at Weeks 4, 16, 28, 40, and 52.
The incidence of adverse events (AEs) and local adverse drug reactions (LADRs) were assessed throughout the study. After ophthalmic solution administration, AEs were reviewed through Weeks 4, 16, 28, 40, and 52. If safety issues, such as the occurrence of AEs, led to treatment discontinuation, the investigator or sub-investigator took appropriate measures and the patient was followed up until symptoms (laboratory values, etc) resolved to almost the status before the start of the study, or at least for one month. The detailed assessment and intensity, and relationship to the treatment is presented in Supplementary Methods 4.
Visual acuity testing (logarithm of the minimum angle of resolution [logMAR] visual acuity), contrast-sensitivity, refractive testing, intraocular pressure testing, corneal geometry analysis (corneal topography), fluorescein staining, and fundus examination (fundus photography) were evaluated from baseline to Weeks 4, 16, 28, 40, and 52. The ophthalmological assessments of visual acuity testing are presented in Supplementary Methods 5.
Blood pressure (seated), pulse rate (seated), body temperature (axilla), 12-lead electrocardiogram (ECG), hematology, serum chemistry, and urinalysis were also evaluated. Pregnancy tests were performed only on females of childbearing potential at Week 52. Details of the tests and the assessment criteria are presented in Supplementary Methods 6.
Statistical Analyses
Previously, in a Phase I/IIa28 and an open-label, Phase III clinical study29 the means and standard deviations (SD) of the differences in IVCM total score on Day 90 in the drug group were 3.19 (1.80) and −4.6 (3.1), respectively. A sample size of 6 and 8 patients was required at one-sided α = 0.025 and 90% power to observe this difference. The number of patients with cystinosis in Japan was estimated to be 14.9 Hence, considering the possibility of discontinuations and drop-offs, the sample size was set as 14 evaluable patients.
The primary efficacy analysis was performed on the full analysis set (FAS: all eligible patients with data available for the efficacy endpoint). The safety analysis was performed on the safety analysis set (SAS: all eligible patients who received the investigational product and for whom safety data was available). The secondary analysis was performed on the per-protocol set (PPS: all patients from the FAS and SAS who complied with all protocol-specified procedures and had no protocol violations).
Summary statistics were provided as mean, SD, median, minimum, and maximum. Descriptive statistics (summary statistics and transition chart of the mean) were performed for IVCM total score, luminance waveform for each eye, left and right by AS-OCT, within 8 weeks before study treatment, 13–16 weeks after treatment, and 49–52 weeks after treatment.
A paired t-test was performed for differences in IVCM total score and average of smoothed intensity (ASI) between 8 weeks before and 13–16 weeks after study initiation. Descriptive statistics (power and graphs) for photophobia assessment by physicians and by patients (scale: 0, 1, 2, 3, 4, 5) for the pre- and post-dose at Weeks 4, 16, 28, 40, and 52 were provided.
The number and percentage of patients with AEs and adverse drug reactions (ADRs) by system organ class (SOC) and by events related to the ophthalmic solution, respectively, were tabulated. Incidence and percentage of serious AEs (SAEs) were analyzed based on the relationship to the ophthalmic solution. Similar tabulations were performed for medically significant events. The number and incidence of LADRs by symptom type (hyperemia, blurred vision, itching, tingling, burning, etc) were also tabulated. Concomitant medications and treatment compliance were tabulated. Summary statistics for the changes from baseline were shown for physiologic (excluding 12-lead ECG), ophthalmologic, and laboratory test (urinalysis is pH only) parameters by time point. The transition from administration initiation is provided for urinalysis (urine protein, urine sugar, occult blood, urobilinogen, bilirubin, ketone body). Summary statistics for physiologic tests, hematological parameters, ophthalmological examinations, and general laboratory values were provided.
A post-hoc analysis was performed to assess the IVCM total score by stratum for the five middle layers of the cornea to generate the crystal density score, since the evaluation of the primary efficacy endpoint was limited due to the small sample size.
All statistical analyses were performed using SAS® version 9.4. Additionally, JMP® version 11.2.1 and OriginPro 2015J Sr2 softwares were used.
Results
Patient Demographics and Characteristics
A total of 6 patients (four males and two females) who met the inclusion criteria were enrolled (Figure 1). The mean age (SD) of patients was 29 (10.30) years (Table 1). The median duration of cystinosis was 23.0 years (range, 8–41 years); five patients had infantile nephropathic cystinosis (83.3%), one had intermediate cystinosis (16.7%) and none had non-nephropathic cystinosis. Four patients had a history of peritoneal dialysis (66.7%), and one (16.7%) underwent hemodialysis. Five patients (83.3%) had undergone renal transplantation at a mean age of 17.8 (2.28) years. All 6 patients used systemic cysteamine; the mean treatment duration with systemic cysteamine was 13.7 (0.52) months (Table 1). Median treatment adherence in the FAS (n=3) was 92.40% (91.0%–99.4%) and in the SAS (n=6) was 95.85% (88.0%–99.4%).
 |
Table 1 Patient Demographics and Baseline Characteristics |
 |
Figure 1 Patient disposition. Abbreviations: GCP, good clinical practice; IVCM, in vivo confocal microscopy; n, number of patients in each category; N, total number of patients. |
Treatment Efficacy
The primary endpoint could not be evaluated because of the inability to obtain the samples as planned. Hence, a post-hoc analysis was performed using the IVCM total score of the 5 middle layers of the cornea. Tables 2 and 3 provide the details of IVCM scores for each corneal layer and the middle 5 corneal layers for 3 patients whose eyes were partially scored. Crystalline densities were scored in all 7 corneal layers, IVCM total score was calculated for only 1 patient (Patient C) at Week 13–16 post-dose, and IVCM total score for the left and right eyes were 4.50 and 5.40, respectively. Due to the sample being limited to one patient, the statistical tests for differences in IVCM total score between 8 weeks before (baseline) and 13–16 weeks (first follow-up) could not be performed.
 |
Table 2 Summary of IVCM Scores for Each Corneal Layer by Patient |
 |
Table 3 IVCM Total Score for the Middle 5 Layers of the Cornea (FAS) |
In another patient (Patient B), IVCM for the left eye was partially scored within 8 weeks before administration of ophthalmic solution and 13–16 weeks after administration. Scores increased in some of the corneal layers in deep stroma. However, a downward trend in IVCM total scores was observed. In Patient C in both eyes, IVCM was partially scored at each evaluation time point (baseline, 13–16 weeks, and 49–52 weeks post-dose). A decrease in scores was observed over time (Figure 2 and Table 2). A similar trend of decreasing scores was also observed in the 5 middle layers of the cornea (Figure 3 and Table 3).
 |
Figure 2 Change in IVCM score for each corneal layer for a) Patient B - Left eye; b) Patient C - Right eye; and c) Patient C - Left eye. Abbreviation: IVCM, in vivo confocal microscopy. |
 |
Figure 3 Change in IVCM total score for the middle 5 layers of the cornea. Abbreviation: IVCM, in vivo confocal microscopy. |
With regards to ASI, one of the secondary endpoints, the mean ASI per patient was 85.7 (10.1) for all patients and 91.7 (11.7) for FAS (n=3) at baseline and decreased to 85.1 (10.4) and 91.2 (10.4) at Week 16, respectively (Supplementary Table 1).
The mean ASI by eye for each patient was 83.6 (8.3), which decreased to 82.7 (9.1) at Week 16 for all eyes (n=10). In the FAS cohort (n=4) it was 89.3 (10.7) at baseline and decreased to 88.4 (10.5) at Week 16. There were no statistically significant differences between the baseline and 16-week post-dose ASI by eye for each patient in the FAS cohort (one-sided t-test, one-sided p=0.3743) (Supplementary Table 2).
With regards to photophobia severity, the other secondary endpoint, the physician-assessed photophobia by eyes (n=10) at Week 16 was compared with the baseline (Supplementary Table 3). A 2-step improvement was observed in 1 patient (1 eye), 1-step improvement was observed in 2 patients (1 eye each), and the condition remained unchanged in 3 patients (5 eyes) and worsened in 1 patient (2 eyes). At Week 52, two patients showed two-step improvement from baseline (one eye in each patient). One patient (1 eye) reported improvement, 4 patients (7 eyes) remained unchanged, and no deterioration in the condition was observed in any patients. For one patient, all photophobia assessments by the physician were “0”. No photophobia was observed under slit light at the maximum light level 1.
Photophobia assessed by the patients (n=10) was evaluated at Week 16 (Supplementary Table 4). Two-step improvement was observed in 1 patient (1 eye), 1-step improvement was observed in 4 patients (7 eyes), the condition remained unchanged in 1 patient (2 eyes), and there were no reports of deterioration. At Week 52, 2-step improvement was observed in 1 patient (1 eye), 1-step improvement was observed in 3 patients (5 eyes), and no change was observed in 2 patients (4 eyes) from baseline. Most patients improved by one step.
In the FAS cohort (n=3 or n=4), eye-by-patient ASI (paired t-test, one-sided p=0.3743) (Supplementary Table 2), and patient-by-patient ASI (paired t-test, one-sided p=0.4445) (Supplementary Table 1) were not statistically significant between baseline and 16 weeks post-dose.
Ocular Safety
A total of 33 AEs were reported by 5 patients (83.3%). Three (50.0%) patients reported eye and general disorders and administration site conditions (Table 4). ADRs were reported by 3 patients (50.0%), all related to the eye (Table 4). Corneal disease, eye irritation, eye pain, and eyelash change were reported by one patient each (16.7%). Tingling sensation was the most frequently reported LADR (Table 5).
 |
Table 4 Adverse Events and Adverse Drug Reactions During the Study (SAS) |
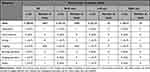 |
Table 5 Frequency of Local Adverse Drug Reactions (SAS) |
In the ophthalmological, laboratory (hematological, biochemical, and urinalysis) and physiological examinations, abnormal changes were observed occasionally and reported as AEs. However, these parameters had no specific trends except for the aggravation of the primary disease (Supplementary Tables 5 to 12).
Discussion
This was the first Phase III study evaluating the efficacy and safety of 0.55% ophthalmic solution of CH in Japanese cystinosis patients. Consistent with previous reports, the number of confirmed cystinosis patients in Japan at the start of the study was 14,9 and considering the rarity of the condition, we could enroll only 6 patients in this study. Overall, we observed a decrease in the IVCM scores from baseline to Week 52. However, a statistical significance could not be established due to the limited sample size and limitations in performing the tests. An improvement in photophobic assessment by both the physician and patients was observed.
The primary endpoint, an IVCM total score (based on evaluating all 7 layers of the cornea), is a highly quantitative and reliable outcome. However, only 3 of 6 patients were partially evaluated using IVCM, and the data obtained were incomplete due to practical limitations. Using IVCM to measure corneal crystal density in 7 distinct corneal layers throughout its depth using a standardized scoring system is a more precise tool but being a technique in which the cornea must remain in contact with the lens, it requires high patient cooperation, thus limiting its use.31 Nevertheless, the IVCM total score was considered an appropriate tool for our study, in line with previous studies.
Considering the difficulty in evaluating efficacy using the IVCM total score, a post-hoc analysis was performed. This analysis used the total score of the 5 middle layers of cornea from the IVCM, the analyses were feasible for 3 eyes in 2 patients, and the results showed that crystal density decreased after 0.55% CH treatment. Additionally, the results by each layer were presented to compensate for the limited data on the primary endpoint. However, it is difficult to compare the amount of change (−2.45 ± 1.88, 3 eyes) with the previously reported value (−4.6 ± 3.1, 22 eyes), in which the IVCM score was based on all 7 layers of the cornea.29
We further considered the analytical validity of the middle 5 layers of the cornea for the IVCM score. In the corneal epithelium, the basal cells divide into wing cells, and the wing cells mature to become superficial cells, and this cycle is around 1 to 2 weeks.32 Therefore, it seems unlikely that cystine crystals continue to accumulate in the uppermost corneal epithelium. Ozdemir et al33 reported the case of a 36-year-old female with cystinosis with crystal accumulation except in the epithelium and the endothelium. In addition, Csorba et al34 reported corneal deposits in 6 patients with cystinosis (4 males and 2 females, 8–36 years old). In 2 patients (3 out of 12 eyes), no crystal accumulation was observed in the epithelium, while all 6 patients (12 out of 12 eyes) reported no crystal accumulation in the endothelium.
A Phase I/IIa28 and an open-label, Phase III clinical study29 supporting regulatory approval in Europe showed cystine crystal accumulation in the middle 5 layers of the cornea accounted for >80% of the total accumulation in the 7 corneal layers. Based on these findings, additional analysis for cystine crystal accumulation evaluation in the intermediate 5 corneal layers was considered appropriate.
Reduction in photophobia was observed due to the reduced crystal density representing a clinical benefit for cystinosis patients in Japan; as demonstrated by Labbé et al and Liang et al.28,29 These studies showed a significant improvement in the IVCM score from baseline to Day 90. Labbé et al28 demonstrated that the improvement in the IVCM score was sustained over 4 years from baseline in the group receiving 0.55% CH compared with 0.1% CH solution. Significant improvement was also observed in the physician- and patient-assessed photophobia scores from baseline to Day 90. In our study, in 4 patients (7 out of 10 eyes), the patient-assessed photophobia score decreased from 2 (before administration) to 1 (16 weeks after administration). The decrease in the frequency of blinking from routinely to occasionally, which is linked to slight discomfort with light, is likely to contribute to an improvement in the patient’s quality of life. Furthermore, this change is of great clinical significance to physicians, as it allows them to make a diagnosis based on detailed observation. Cysteamine improved visual acuity scores and contrast sensitivity, and provided better response to therapy compared with placebo/saline treatment.22,35 In our study, we did not report any vision loss, in line with findings by Iwata et al.36
The report of any AE in our study was 83%. Most were eye-related disorders and administration site conditions (50% each). A tingling sensation (33%) was the most frequently reported local AE, although stinging and burning sensations have been the most reported local AEs in other cysteamine studies.29,36 While two studies reported blurred vision as a common AE,29,37 we did not observe blurred vision due to the ophthalmic solution.
This study provides the long-term efficacy and safety data associated with the 0.55% ophthalmic cysteamine solution in patients with cystinosis, besides assessing the treatment compliance and adherence over 52 weeks. Using standard diagnostic criteria and methods ensures the generalizability of the study results. Despite the study filling the knowledge gap in this rare disease area, the limitations need to be discussed in the context of methodological issues.
Developing orphan medicines for rare/difficult-to-treat conditions presents many challenges. These challenges are faced at several stages such as funding of clinical trials, identifying suitable clinical investigators, and most importantly, recruiting sufficient patients.38 Another critical challenge was to obtain sufficient evidence of efficacy given the low acceptability of IVCM, the primary evaluation method. Additionally, this was an open-label, single-arm study, lacking a control group. However, without a standard of care for this rare condition, we did not use placebo as a control. Thus, the absence of blinding as well as a control group may have led to potential observer bias in the assessment of subjective variables like photophobia severity. Finally, due to the impact of COVID-19, there was limited access to only one IVCM facility, limiting our recruitment efforts. Nevertheless, we developed a protocol to do the best in the given scenario considering inputs from preliminary interviews of the experts.
Conclusion
In conclusion, our study findings suggested that efficacy against corneal cystine accumulation and an acceptable safety profile of 0.55% CH ophthalmic solution, when administered repeatedly, may be applicable to Japanese patients with cystinosis. These findings add to the previous evidence on the efficacy and safety of 0.55% CH ophthalmic solution in cystinosis patients. More studies in diverse patient populations are needed to increase the evidence for treatment of this rare ocular disease.
Abbreviations
AE, adverse event; ADR, adverse drug reaction; AS-OCT, anterior segment optical coherence tomography; ASI, average of smoothed intensity; CH, cysteamine hydrochloride; CTNS, cystinosin; ECG, electrocardiogram; FAS, full analysis set; IVCM, in vivo confocal microscopy; LADR, local adverse drug reaction; NIH, National Institute of Health; PPS, per-protocol set; SAE, serious adverse event; SAS, safety analysis set; SD, standard deviation; SOC, system organ class.
Data Sharing Statement
The data that support the findings of this study are available from Viatris Pharmaceuticals Japan G.K., but restrictions apply to the availability of these data, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Viatris Pharmaceuticals Japan G.K.
Ethics Approval and Informed Consent
The study was conducted based on the principles of the Declaration of Helsinki (revised on October 19, 2013) and the standards specified in Article 14, Article 3, and Article 80 (2) of the Law Concerning Quality, Efficacy, and Safety of Clinical Trial Protocols, Pharmaceuticals, and Medical Devices and Good Clinical Practice (Ministry of Health and Welfare dated March 27, 1997) implemented in compliance with Order No. 28 and its amended ministerial ordinance and other relevant notices. Patients were informed of the objectives, methods, duration, nature of drug, effects, anticipated adverse reactions, etc of the study, and voluntary written consent to participate in the study was obtained for all patients before study entry. The respective ethics committees of the study centers (All Tohoku Clinical Trial Review and Audit Organization (ACTIVATO), Yokohama City University Medical Center Institutional Review Board, and Japan Community Health Care Organization Chukyo Hospital Institutional Review Board) approved the study.
Consent for Publication
The authors confirm this manuscript does not include details of images, videos, or recordings of any study participants. Consent forms were obtained from each participant before initiating the study.
Acknowledgments
Vidula Bhole, Md Najeeb Ashraf, and Lakshmi Hariharan of MedPro Clinical Research provided medical writing and editorial support towards developing the manuscript per the ICMJE criteria. We are deeply grateful to Dr. Shuichi Ito (Department of Pediatrics, Yokohama City University, Yokohama, Japan) for fulfilling his responsibilities as a Coordinating Investigator. We also thank the investigators, Dr. Shunji Yokokura (Department of Ophthalmology, Tohoku University Graduate School of Medicine, Sendai, Japan), Dr. Tatsuya Inoue (Department of Ophthalmology and Micro-Technology, Yokohama City University, Kanagawa, Japan), and Dr. Tatsushi Kaga (Department of Ophthalmology, Japan Community HealthCare Organization, Chukyo Hospital, Nagoya, Japan) and the patients who participated in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Viatris Pharmaceuticals Japan G.K. The funder was involved with the study design, data collection, analysis, interpretation, and writing. Full access to study data is with the corresponding author, who took final responsibility for the decision to submit for publication. Support on medical writing was provided by MedPro Clinical Research and was funded by Viatris Pharmaceuticals Japan G.K.
Disclosure
FI and TC declare having professional service agreement with Mylan EPD G.K. and Viatris Pharmaceuticals Japan G.K. NG, SH and YS declare having received Orphan Drug Development Grants from National Institutes of Biomedical Innovation, Health and Nutrition. NG, SH and YS are full-time employees of Viatris Pharmaceuticals Japan G.K., and SH holds stock of Viatris Inc. The authors report no other conflicts of interest in this work.
References
1. Town M, Jean G, Cherqui S, et al. A novel gene encoding an integral membrane protein is mutated in nephropathic cystinosis. Nat Genet. 1998;18(4):319–324. doi:10.1038/ng0498-319
2. Nesterova G, Gahl WA. Cystinosis: the evolution of a treatable disease. Pediatr Nephrol. 2013;28(1):51–59. doi:10.1007/s00467-012-2242-5
3. Shotelersuk V, Larson D, Anikster Y, et al. CTNS mutations in an American-based population of cystinosis patients. Am J Hum Genet. 1998;63(5):1352–1362. doi:10.1086/302118
4. Levtchenko E, van den Heuvel L, Emma F, Antignac C. Clinical utility gene card for cystinosis. Eur J Hum Genet. 2014;22(5):713. doi:10.1038/ejhg.2013.204
5. Forestier L, Jean G, Attard M, et al. Molecular characterization of CTNS deletions in nephropathic cystinosis: development of a PCR-based detection assay. Am J Hum Genet. 1999;65(2):353–359. doi:10.1086/302509
6. Yarahmadi SG, Sarlaki F, Morovvati S. Cystinosis and two rare mutations in CTNS gene: two case reports. J Med Case Rep. 2022;16(1):181. doi:10.1186/s13256-022-03379-7
7. Elmonem MA, Veys KR, Soliman NA, van Dyck M, van den Heuvel LP, Levtchenko E. Cystinosis: a review. Orphanet J Rare Dis. 2016;11(1):47. doi:10.1186/s13023-016-0426-y
8. Soliman NA, Elmonem MA, van den Heuvel L, et al. Mutational spectrum of the CTNS gene in Egyptian patients with nephropathic cystinosis. JIMD Rep. 2014;14:87–97. doi:10.1007/8904_2013_288
9. Higashi S, Matsunoshita N, Otani M, Tokuhiro E, Nozu K, Ito S. Diagnostic challenge in a patient with nephropathic juvenile cystinosis: a case report. BMC Nephrol. 2017;18(1):300. doi:10.1186/s12882-017-0721-4
10. Gahl WA, Thoene JG, Schneider JA. Cystinosis. N Engl J Med. 2002;347(2):111–121. doi:10.1056/NEJMra020552
11. Nesterova G, Gahl WA. Cystinosis. 2001 Mar 22 [Updated 2017 Dec 7]. In: Adam MP, Mirzaa GM, Pagon RA, et al. editors. GeneReviews® [Internet]. Seattle: University of Washington, Seattle; 1993-2023. Available from https://www.ncbi.nlm.nih.gov/sites/books/NBK1400/.
12. Biswas S, Gaviria M, Malheiro L, Marques JP, Giordano V, Liang H. Latest clinical approaches in the ocular management of cystinosis: a review of current practice and opinion from the Ophthalmology Cystinosis Forum. Ophthalmol Ther. 2018;7(2):307–322. doi:10.1007/s40123-018-0146-6
13. Shams F, Livingstone I, Oladiwura D, Ramaesh K. Treatment of corneal cystine crystal accumulation in patients with cystinosis. Clin Ophthalmol. 2014;8:2077–2084. doi:10.2147/OPTH.S36626
14. Gahl WA, Kuehl EM, Iwata F, Lindblad A, Kaiser-Kupfer MI. Corneal crystals in nephropathic cystinosis: natural history and treatment with cysteamine eyedrops. Mol Genet Metab. 2000;71(1–2):100–120. doi:10.1006/mgme.2000.3062
15. Dufier JL, Dhermy P, Gubler MC, Gagnadoux MF, Broyer M. Ocular changes in long-term evolution of infantile cystinosis. Ophthalmic Paediatr Genet. 1987;8(2):131–137. doi:10.3109/13816818709028529
16. Flockerzi E, Daas L, Schlötzer-Schrehardt U, Zimpfer A, Bohle R, Seitz B. Ocular changes in nephropathic cystinosis: the course of the gold-dust. Int Ophthalmol. 2019;39(6):1413–1418. doi:10.1007/s10792-018-0954-7
17. Gahl WA. Early oral cysteamine therapy for nephropathic cystinosis. Eur J Pediatr. 2003;162 Suppl 1:S38–41. doi:10.1007/s00431-003-1349-x
18. Huynh N, Gahl WA, Bishop RJ. Cysteamine ophthalmic solution 0.44% for the treatment of corneal cystine crystals in cystinosis. Expert Rev Ophthalmol. 2013;8(4):341–345. doi:10.1586/17469899.2013.814885
19. Makuloluwa AK, Shams F. Cysteamine hydrochloride eye drop solution for the treatment of corneal cystine crystal deposits in patients with cystinosis: an evidence-based review. Clin Ophthalmol. 2018;12:227–236. doi:10.2147/OPTH.S133516
20. Tsilou ET, Thompson D, Lindblad AS, et al. A multicentre randomised double masked clinical trial of a new formulation of topical cysteamine for the treatment of corneal cystine crystals in cystinosis. Br J Ophthalmol. 2003;87(1):28–31. doi:10.1136/bjo.87.1.28
21. Kaiser-Kupfer MI, Fujikawa L, Kuwabara T, Jain S, Gahl WA. Removal of corneal crystals by topical cysteamine in nephropathic cystinosis. N Engl J Med. 1987;316(13):775–779. doi:10.1056/NEJM198703263161304
22. Kaiser-Kupfer MI, Gazzo MA, Datiles MB, Caruso RC, Kuehl EM, Gahl WA. A randomized placebo-controlled trial of cysteamine eye drops in nephropathic cystinosis. Arch Ophthalmol. 1990;108(5):689–693. doi:10.1001/archopht.1990.01070070075038
23. McKenzie B, Kay G, Matthews KH, Knott R, Cairns D. Preformulation of cysteamine gels for treatment of the ophthalmic complications in cystinosis. Int J Pharm. 2016;515(1–2):575–582. doi:10.1016/j.ijpharm.2016.10.044
24. European Medicines Agency. Cystadrops. Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/cystadrops#authorisation-details.
25. PR Newswire. U.S. FDA Approves CYSTADROPS® (Cysteamine Ophthalmic Solution) 0.37%, A New Practical Treatment Option for the Ocular Manifestations of Cystinosis. Available from: https://www.prnewswire.com/news-releases/us-fda-approves-cystadrops-cysteamine-ophthalmic-solution-0-37-a-new-practical-treatment-option-for-The-ocular-manifestations-of-cystinosis-301118026.html.
26. Pharmaceuticals and Medical Devices Agency. List of Approved Products. Available from: https://www.pmda.go.jp/english/review-services/reviews/approved-information/drugs/0002.html.
27. Pinxten AM, Hua MT, Simpson J, Hohenfellner K, Levtchenko E, Casteels I. Clinical practice: a proposed standardized ophthalmological assessment for patients with cystinosis. Ophthalmol Ther. 2017;6(1):93–104. doi:10.1007/s40123-017-0089-3
28. Labbé A, Baudouin C, Deschênes G, et al. A new gel formulation of topical cysteamine for the treatment of corneal cystine crystals in cystinosis: the Cystadrops OCT-1 study. Mol Genet Metab. 2014;111(3):314–320. doi:10.1016/j.ymgme.2013.12.298
29. Liang H, Labbe A, Le Mouhaer J, Plisson C, Baudouin C. A new viscous cysteamine eye drops treatment for ophthalmic cystinosis: an open-label randomized comparative phase III pivotal study. Invest Ophthalmol Vis Sci. 2017;58(4):2275–2283. doi:10.1167/iovs.16-21080
30. Pharmaceuticals and Medical Devices Agency. List of Approved Products – FY 2014. Available from: https://www.pmda.go.jp/files/000267885.pdf.
31. Kowalczyk M, Toro MD, Rejdak R, Załuska W, Gagliano C, Sikora P. Ophthalmic evaluation of diagnosed cases of eye cystinosis: a tertiary care center’s experience. Diagnostics. 2020;10(11):911. doi:10.3390/diagnostics10110911
32. Oshika T, editor. Ophthalmology Clinical Qualification 30 “Development, Anatomy and Function of the Eye”.
33. Ozdemir HB, Özmen MC, Aktas Z, Hasanreisoglu M. In vivo confocal microscopy and anterior segment optical coherence tomography follow-up of cysteamine treatment in corneal cystinosis. Indian J Ophthalmol. 2019;67(1):153–155. doi:10.4103/ijo.IJO_736_18
34. Csorba A, Maka E, Maneschg OA, et al. Examination of corneal deposits in nephropathic cystinosis using in vivo confocal microscopy and anterior segment optical coherence tomography: an age-dependent cross-sectional study. BMC Ophthalmol. 2020;20(1):73. doi:10.1186/s12886-020-01336-w
35. Bradbury JA, Danjoux JP, Voller J, Spencer M, Brocklebank T. A randomised placebo-controlled trial of topical cysteamine therapy in patients with nephropathic cystinosis. Eye (Lond). 1991;5(6):755–760. doi:10.1038/eye.1991.139
36. Iwata F, Kuehl EM, Reed GF, McCain LM, Gahl WA, Kaiser-Kupfer MI. A randomized clinical trial of topical cysteamine disulfide (cystamine) versus free thiol (cysteamine) in the treatment of corneal cystine crystals in cystinosis. Mol Genet Metab. 1998;64(4):237–242. doi:10.1006/mgme.1998.2725
37. Liang H, Labbé A, Baudouin C, Plisson C, Giordano V. Long-term follow-up of cystinosis patients treated with 0.55% cysteamine hydrochloride. Br J Ophthalmol. 2021;105(5):608–613. doi:10.1136/bjophthalmol-2020-316450
38. Buckley BM. Clinical trials of orphan medicines. Lancet. 2008;371(9629):2051–2055. doi:10.1016/S0140-6736(08)60876-4
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

