Back to Journals » Patient Preference and Adherence » Volume 19
Antecedents of Patient Loyalty: Exploring Mediating and Moderating Paradigms in Public Hospitals
Authors Hussain A, Kanwel S , Khan S , Alonazi WB , Malik A, Khan AA
Received 9 September 2024
Accepted for publication 11 February 2025
Published 1 March 2025 Volume 2025:19 Pages 527—542
DOI https://doi.org/10.2147/PPA.S492710
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Abid Hussain,1 Shahida Kanwel,2 Sania Khan,3 Wadi B Alonazi,4 Azam Malik,3 Ali Ahmed Khan5
1School of Nursing, Shandong Xiehe University, Jinan, 250109, People’s Republic of China; 2School of Management, Jiangsu University, Zhenjiang, Jiangsu, 212013, People’s Republic of China; 3Department of Human Resource Management, College of Business Administration, Prince Sattam Bin Abdulaziz University, Al Kharj, 11942, Saudi Arabia; 4Health Administration Department, College of Business Administration, King Saud University, Riyadh, 11587, Saudi Arabia; 5Department of Management Information Systems, College of Business Administration, Prince Sattam Bin Abdulaziz University, Hotat Bani Tamim, Al Kharj, 11942, Saudi Arabia
Correspondence: Sania Khan, Email [email protected]
Purpose: Countries around the world acknowledge the vital role of effective healthcare services in fostering economic, social, and human development. Consequently, many are striving to enhance their medical facilities. This study specifically examines public hospitals in Pakistan and aims to create a framework for evaluating patient loyalty.
Methods: Responses from 650 patients were collected using a random sampling technique. The gathered data were analyzed using the Statistical Program for Social Sciences (SPSS) and Analysis of Moment Structures (AMOS).
Results: The analysis revealed significant relationships among administrative procedures, service effectiveness, patient satisfaction, and loyalty. Additionally, the study identified patient satisfaction and administrative procedures as mediators between service effectiveness and patient loyalty. It also investigated the moderating roles of participative leadership and brand image in shaping administrative procedures, patient satisfaction, and patient loyalty.
Conclusion: These findings offer valuable insights for healthcare authorities in formulating strategies to improve service delivery in public hospitals. Addressing existing deficiencies and enhancing healthcare systems is essential to fostering patient loyalty in these environments.
Keywords: patient loyalty, PL, services effectiveness, SE, administrative procedures, AP, patient satisfaction, PS, participative leader, PAL, brand image, BI
Introduction
Healthcare costs have skyrocketed due to providers’ attempts to satisfy patients’ demands for disease diagnosis, effective treatment, and more comprehensive medical services. In Pakistan, economic growth has slowed down in the past few decades due to various factors, such as a lack of foreign investment, limited water and financial resources, widespread poverty, ineffective policy implementation, and the use of inappropriate metrics that impact the measurement of quality and productivity.1 In response to these challenges, the Malcolm Baldrige National Quality Award Healthcare Criteria (MBNQA) was established in 1987. This criterion has prompted medical institutions to prioritize patient care, engage with stakeholders, empower their organizations, foster green innovation, promote continuous learning, and establish a clear direction for improvement. The National Productivity Organization (NPO) introduced the “Prime Minister Quality Award” (PMQA) in 2020. This initiative involved approximately seventy countries and utilized the MBNQA standards to develop the PMQA methodology. This award aimed to promote the implementation of quality standards that would result in enhanced productivity and customer satisfaction. The primary focus areas include reducing hospital costs, embracing new technologies, advancing diagnostic and treatment methods, and delineating the responsibilities of doctors and hospitals within limited resources.2 To ensure patient satisfaction, hospitals, and outpatient clinics have adopted a market-focused approach to effective quality assurance.3,4
Ali and Anwar5 argued that companies should focus on establishing measurement strategies for patient satisfaction to provide efficient and successful medical care. The effectiveness of medical services is concerned with the health outcomes and technical aspects of treatment, while green administrative procedures (GAP) pertain to the non-technical aspects of various back-office activities. Both medical efficacy and GAP contribute to essential elements such as necessary medical treatments, compassionate behavior, and patient satisfaction, fostering patient loyalty.6 Schaefer7 argues that quality-minded leadership is crucial for organizational success and patient satisfaction. Additionally, academics have recognized the importance of effective leadership in the healthcare system as a vital factor in improving patient happiness.8 An effective leadership style is an external component crucial for achieving organizational performance and goals, as outlined in the MBNQA structural criteria.9
Fry, Latham10 utilized spiritual leadership to enhance the effectiveness of the hospital. Many healthcare organizations have used the MBNQA standards to improve the quality and efficiency of patient-centered care. Participatory leadership significantly impacts patient satisfaction and has been shown to improve clinical and administrative quality. Previous studies have demonstrated that several quality frameworks for medical services, such as doctor and nurse services, doctor-patient communication (R), and pharmacy service satisfaction, have improved hospital performance.11 In the health sector, the most effective way to assess service quality is by considering various components, including brand image (BI), privacy and safety (P&S), communication, customer friendliness (CF), physical environment (PE), and responsiveness and service effectiveness (SE) with the support of green administrations. Previous literature has examined patient loyalty concerning patient satisfaction, administrative procedures, patient experiences, discharge information,12 ward environment Astarini and Fachrodji,13 patient satisfaction, and hospital staff’s impact on patient satisfaction. The author’s sources have found few studies exploring the relationship between service effectiveness and patient loyalty, considering administrative procedures and patient satisfaction as mediators, participative leadership, and brand image as moderators within a single framework.
This conceptual framework examines the relationship between several variables: service effectiveness, administrative procedures, patient satisfaction, and loyalty. The findings suggest that service effectiveness, administrative procedures, and patient satisfaction positively impact patient loyalty. This study adds to the existing literature by analyzing the relationship between administrative procedures and patient satisfaction, as well as administrative procedures and patient loyalty. Additionally, the study investigates the role of patient satisfaction and administrative procedures as mediators in the relationship between service effectiveness and patient loyalty. Furthermore, brand image moderates the relationship between patient satisfaction and patient loyalty, while participative leadership influences the relationship between administrative procedures and patient loyalty.
Theoretical Background and Hypotheses Development
Management Theory (MT)
In healthcare, the application of management theory involves designing and delivering administrative efforts to effectively deliver health standards to patients. The purpose of this initiative is to adapt and improve healthcare within an organization to increase the likelihood of achieving desired outcomes and enhancing patient satisfaction levels.14 Patient satisfaction can be achieved through timely treatment delivery under proper management supervision.15 The sustainability of a hospital depends on effective team management and the provision of high-quality care, which collectively contribute to the best patient experience.16 A study has underscored the significance of applying management theory to enhance service effectiveness in the healthcare sector.17 These theories are instrumental in developing monthly and yearly plans as well as guiding resource allocation. Inadequate hospital management can result in missed deadlines, disease progression, increased inpatient mortality, higher costs, and the waste of human and financial resources. Therefore, hospital management should prioritize patients’ needs and offer services at reasonable prices while ensuring high-quality, safe diagnostic, therapeutic, and rehabilitative services. Consequently, scholars have adapted management theory to create a framework for measuring the effectiveness of service sectors.18 This application of management theory supports a logical study model aimed at enhancing hospital efficacy and patient satisfaction.
Services Effectiveness and Patient Loyalty
Hospital services provide a good patient experience and excellent clinical quality. Prior studies indicated the healthcare services of hospitals that could be successful in building patient loyalty among the public by providing better facilities for patient satisfaction.19 Afifi and Amini20 considered hospital staff effectiveness to be a worthy asset for developing patient loyalty. SE comprises “monitoring and improving the outcomes of patients and service users, which also involves professionalism and updated knowledge to perform well”. A deeply held commitment to rebuy or patronize a preferred product/service consistently in the future, thereby causing repetitive same-brand or same-brand-set purchasing, despite situational influences and marketing efforts having the potential to cause switching behavior, is known as loyalty. In addition, loyalty encompasses psychological, social, and emotional well-being, which may influence patients thinking about services.21 Knox22 described that loyalty is directly connected to services and facilities, improving patient satisfaction. Juhana, Manik23 suggested healthcare services as patient satisfaction, Chaabouni and Abednnadher24 image of loyalty with hospitals determined through pharmacy services. Vimla and Taneja25 indicated that customer satisfaction is significantly related to customer loyalty. Cham, Cheng26 explored loyalty as an endogenous element fueled by satisfaction and effectiveness. The study revealed that effectiveness helps to enhance patients’ loyalty in accepting and executing hospital management. Thus, we hypothesized SE has a positive relation with PL.
Service effectiveness refers to the ability of a service to meet predefined objectives or standards, such as addressing patient needs or providing timely care.27 Patient loyalty, on the other hand, is the long-term commitment of patients to a healthcare provider, often influenced by trust, satisfaction, and emotional connection rather than just service outcomes.28 While effectiveness is performance-based, loyalty encompasses emotional and relational aspects. Patient loyalty, as an outcome, differs from service effectiveness because it reflects the patient’s long-term emotional attachment and willingness to continue using the service, rather than just an immediate response to the service quality. Service effectiveness focuses on measurable achievements, such as timely and accurate treatment, while patient loyalty represents a broader, more subjective result influenced by trust, satisfaction, and overall experience beyond functional performance. Therefore, we hypothesize the following hypothesis:
H1: SE relates positively toward PL
Services Effectiveness, Patient Satisfaction, and Administrative Procedure
A growing population means more demand for healthcare for patient satisfaction with the effectiveness of the services to remain sustainable in healthcare sectors.29 SE was given to the patients by healthcare, which led to patient satisfaction and green loyalty.30 The term “privacy” means patients’ rights to safeguard medical records against unauthorized disclosure. Meanwhile, security protects information against unauthorized access, explicitly mentioning integrity and availability.31 The term “physical environment” describes the external factors and settings that affect human health. Proper planning and advanced hospital infrastructure should ensure patients’ health and safety, as well as a friendly physical environment with ventilation, clean drinking water, accessible restrooms, lights, good sitting places, and stairwells.32
The ability to convey true care about the patient’s condition is essential to effective communication between healthcare providers and patients. Patient safety is compromised when healthcare providers are unable to communicate necessary information to one another in a timely,31 which creates misunderstandings as well as wrong interpretations. A study indicated that communication significantly impacts patient satisfaction and loyalty. While scholars defined communication as a key element of hospital service effectiveness.33 Medical responsiveness designed health facilities because they are very familiar with patients’ universally legitimate expectations.34
Amporfro, Boah35 conducted a study examining the impact of friendly and caring staff behavior on patient satisfaction and loyalty, ultimately contributing to the hospital’s reputation. Our study explored the relationship between service effectiveness, privacy and safety, physical environment, communication, responsiveness, and customer-friendliness. Previous research has shown that service effectiveness, administrative procedures, and patient satisfaction are interconnected and crucial for success. Based on this, we hypothesized that service effectiveness is linked to administrative procedures and patient satisfaction. The results of our study confirmed that service effectiveness plays a significant role in improving administrative procedures and enhancing patients’ satisfaction with hospital management. Therefore, we can conclude that service effectiveness is positively associated with administrative procedures and patient satisfaction.
Hospital administrative procedures are standardized policies and processes designed to streamline operations, ensure compliance with healthcare regulations, and support effective governance within the hospital setting. These procedures encompass areas such as patient admissions, resource management, staff coordination, and operational efficiency, aiming to enhance service delivery and accountability.36,37
H2: SE positively relates to the PS H3: SE refers positively to the AP
Patient Satisfaction, Administrative Procedure, and Patient Loyalty
Patient satisfaction is crucial for building patient loyalty. When patient satisfaction is high, patient loyalty also increases. In the healthcare industry, customer feedback is vital in improving internal systems, directly impacting customer satisfaction.38 Ng and Luk39 argue that better patient care is the first step towards enhancing hospital efficiency and improving healthcare, resulting in greater satisfaction and loyalty. Dunsch, Evans40 explain that patients from different regions, languages, and backgrounds expect positive behavior right from the start when they visit a hospital. Providing a secure, well-communicated, and protected medical setting makes predicting patient satisfaction and loyalty possible. Patient satisfaction is directly linked to patient loyalty.41 Increasing patient loyalty can have a significant clinical impact by ensuring service continuity, reducing patient attrition, promoting adherence to treatment plans, and influencing overall medical conditions.42
Administrative procedures in hospital services encompass the organized techniques and workflows that manage various aspects of operations, including patient admission, billing, planning, record control, and compliance with relevant laws. Effective administrative procedures enhance operational efficiency, improve the patient experience, and contribute to the overall quality of care.43 Curry and Sinclair44 stated that improving administrative procedures, which are essential to hospital service quality, can help alleviate inconveniences for patients. Casado Diaz and Más Ruíz45 further elaborated that delays in hospital service delivery can lead to resentment, prompting patients to misbehave towards staff. Furthermore, effective administrative procedures foster a positive image among satisfied patients who appreciate the medical services they receive.
Vimla and Taneja25 indicated that customer satisfaction is significantly related to customer loyalty. Juhana, Manik23 defined loyalty as an endogenous factor driven by satisfaction, suggesting that it can be enhanced through a combination of elements. Additionally, Aliman and Mohamad46 discovered that patient satisfaction has a direct impact on hospital administrative services, healthcare quality, and patient loyalty. Woodside, Frey47 examined how patient satisfaction mediates the relationship between hospital services such as administrative, medical staff, and technical support and patients’ decisions to revisit or remain loyal to the hospital. Thus, the literature indicates that a hospital’s success relies on the quality of its services, patient satisfaction, and effective administrative procedures. The findings revealed that both satisfaction and procedural efficiency contribute to enhancing patient loyalty toward hospital management. Therefore, we hypothesize that patient satisfaction and administrative procedures are positively related to patient loyalty.
H4: PS positively relates to the PL H5: AP refers positively to the PL
Mediating Role of Patient Satisfaction and Administrative Procedure
Kumar, Jacob48 have demonstrated that providing quality services through efficient administrative procedures positively affects both patient satisfaction and the overall image of the hospital. Previous studies have also confirmed the significant role that administrative procedures play in enhancing patient satisfaction and service quality, which, in turn, improves the hospital’s reputation and attracts the general public.49 Aliman and Mohamad46 emphasize that patient satisfaction directly influences the quality of administrative services, healthcare standards, and patient loyalty. Olesen and Bathula50 highlight that patients’ satisfaction with administrative procedures, including medical care standards and patient reports, is a crucial factor in their loyalty and their likelihood of seeking further treatment at the hospital. Furthermore, another study clarifies that the effectiveness of treatment directly impacts patient loyalty.51
Gejea, Abadiga16 establish a connection between the quality of medical care and both patient loyalty and improvement. Ali and Anwar5 explore the role of satisfaction in fostering customer loyalty. Astarini and Fachrodji13 define the intention to return to a healthcare center and to recommend it to others as behavioral intention. Building on these insights, we hypothesize that patient satisfaction and administrative procedures are linked to service effectiveness and patient loyalty. Our study demonstrates that patient satisfaction plays a vital role in enhancing service effectiveness and cultivating patient loyalty toward hospital management. Thus, both patient satisfaction and administrative procedures have a significant impact on service effectiveness and patient loyalty, reinforcing our hypothesis.
H6: PS plays a mediating role in the relationship between SE and PL H7: AP Plays a Mediating Role in the Relationship Between SE and PL
Moderating Role of Participative Leadership and Brand Image
The MBNQA criterion was established in 1987 to set and evaluate standards across various sectors, including health, education, small business, manufacturing, service, and non-profit organizations. Its goal was to promote the improvement of these institutions and was developed with input from 500 experts in administration and quality management.16 Initially, this approach was applied mainly within the industrial and non-profit sectors. However, in 1995, researchers began to explore a new award criterion that specifically targeted quality assurance initiatives in healthcare facilities. This criterion also offered a recognizable organizational framework for MBNQA, linking leadership to key factors such as procedures, people management, development, strategic planning, data analysis, and investigation. These factors were associated with customer and investor satisfaction, as well as overall business success.20
Alipour, Mehdipour31 studied the Baldrige Healthcare framework and discovered that strong leadership is the most crucial external factor for improving financial outcomes. According to Tushar, Moktadir18 brand equity refers to a brand’s ability to either enhance or diminish its value, which is determined by consumer responses to the company’s products or services. Brand Image is a significant topic in the services sector, as it greatly influences consumer perceptions of a business. While the importance of BI in the healthcare sector is just beginning to gain attention, it is essential for healthcare organizations to succeed in today’s highly competitive landscape.
Aaker52 landmark book, “Managing Brand Equity”, was pivotal in helping business leaders understand branding as a key competitive differentiator and strategic asset. In the medical field, harnessing the goodwill linked to a hospital brand can offer a significant advantage over competitors. While there has been extensive research on the effects of hospital services on patient satisfaction and loyalty, there is limited exploration of the relationship between brand image, loyalty, and their mediating role in patient satisfaction and goodwill. This gap in research within the medical sector underscores the need for further investigation. Consequently, this study aims to address the following healthcare-related research questions.
H8: BI moderates and strengthens the relationship between PS and PL H9: PAL moderates and enhances the relationship between AP and PL
Conceptual Model
The authors have developed a conceptual framework, illustrated in Figure 1, to explore the impact of SE on AP, PS and PL. This framework takes into account the influence of AP and PS on SE and PL. Furthermore, it includes the concept of participative leadership as a moderator in the relationship between AP and PL, as well as the role of brand image in moderating the relationship between PS and PL.
 |
Figure 1 Conceptual Framework. |
Research Methods
Construct Operationalization
The proposed conceptual model was assessed using various variable items adapted from previous studies. Participative leadership, brand image, administrative procedures, service effectiveness, patient satisfaction, and loyalty (excluding demographic information) were assessed using a 5-point Likert scale. The measurement of participative leadership was based on three items adapted from the Baldrige Criteria for healthcare.6 The brand image was measured through three items adapted from the study of Cham, Cheng.26 The administrative procedure evaluated by nine items developed by Babakus and Mangold.33 Service effectiveness, specifically treatment quality, was evaluated using seven items developed by Lee.53 Eight items from Tucker and Adams51 studies were adapted to measure patient satisfaction. Lastly, patient loyalty was measured using four items developed by.54
Sampling and Data Collection
The sample size determination methodology used by Saunders, Lewis,55 Krejcie and Morgan56 is widely recognized for its reliability in service studies. This study involved patients from outpatient departments in four public hospitals located in Bahawalpur, Bahawalnagar, Rahimyar Khan, and Lodhran in Punjab. Questionnaires adapted for the study were distributed to patients using a random sampling technique. The survey was conducted over four months, from February to July 2023, during working hours in public hospitals. Originally developed in English, the questionnaire was subsequently translated into Urdu, the native language of Pakistan, to ensure better understanding for those who cannot read or comprehend English. A total of 650 questionnaires were distributed, but only 499 responses were included in the analysis, yielding a response rate of 76%. The remaining responses were excluded due to inconsistencies in the data and missing values.
Analysis Methods
The data were analyzed using Structural Equation Modeling (SEM) with the Social Science Statistical Package (SPSS and AMOS). This analysis provided correlations for reliability and validity, as well as descriptive statistics. We performed Confirmatory Factor Analysis (CFA) and SEM to evaluate our proposed model. In this study, SEM was utilized for hypothesis testing, and the stability of all items was assessed using Cronbach’s alpha.19 A measurement model was constructed to examine the explicit relationships between each factor and its corresponding items. The three-stage approach implemented suggested by Sahito,9 which is well-suited for a measurement model that includes component scores among all items. Formal discriminant validity tests were conducted using CFA, while the causal model was assessed through SEM.
Common Method Bias (CMB)
Measurement biases were assessed using Harman’s single-factor analysis. The results indicate that the typical technique bias problem does not influence the data, as the proportion of variance explained by a single factor is 30.05%, which is below the 50% threshold.8 Therefore, the analysis data can be considered reliable and valid.8 Table 1 presents the study area, and the population included in the research.
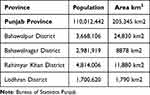 |
Table 1 Study Area and Population |
Results
Demographics
Table 2 presents the demographic details of 499 respondents, 235 were male, and 264 were female. The majority of participants, 418 (83.76%), were married, while 81 (16.24%) were unmarried. In terms of age distribution, 108 participants (21.64%) were aged 20–29, 99 participants (19.84%) were aged 30–39, 103 participants (20.65%) were aged 40–49, and 189 participants (37.87%) were over the age of 50. Regarding education, 107 respondents (21.45%) had no formal education, 179 participants (35.87%) had completed their school education, 139 participants (27.85%) had completed college, and 74 respondents (14.83%) had graduated from university.
 |
Table 2 Demographics Details |
Convergent Validity and Reliability Analysis
Table 3 presents the factor loadings, standard errors, t-statistics, composite reliabilities (CR), and Cronbach’s α values. The accepted criterion for α is 0.70,5 which is the most commonly used method for assessing internal consistency. The α values for participative leadership, brand image, administrative procedures, service effectiveness, patient satisfaction, and patient loyalty are 0.86, 0.81, 0.93, 0.95, 0.82, and 0.84, respectively. The factor loading ranges are as follows: 0.797–0.863 for participative leadership, 0.834–0.851 for brand image, 0.703–0.839 for administrative procedures, 0.755–0.851 for service effectiveness, 0.709–0.874 for patient satisfaction, and 0.776–0.817 for patient loyalty and recommended factor loading criteria is 0.50.27 The CR values should be greater than 0.06, patient loyalty (0.89), patient satisfaction (0.86), service effectiveness (0.87), administrative procedures (0.83), brand image (0.81), and participative leadership (0.85), statistically significant recommended by Asif, Jameel.6
 |
Table 3 Measurement Model |
Discriminant Validity
Table 4 presents the descriptive statistics, including correlations, means, and standard deviations. Participative leadership showed significant correlations with brand image (r = 0.23, p < 0.01), administrative procedures (r = 0.19), service effectiveness (r = 0.29, p < 0.01), patient satisfaction (r = 0.40, p < 0.01), and patient loyalty (r = 0.42, p < 0.01). A significant correlation was also found between brand image and administrative procedures (r = 0.21, p < 0.01). Additionally, administrative procedures had a positive correlation with service effectiveness (r = 0.23, p < 0.01), and service effectiveness significantly correlated with patient satisfaction (r = 0.21, p < 0.01). A strong positive association was observed between service effectiveness and patient loyalty (r = 0.41, p < 0.01), as well as between patient satisfaction and patient loyalty (r = 0.48, p < 0.01). The means and standard deviations for participative leadership (3.29, 0.97), brand image (3.09, 0.91), administrative procedures (3.32, 0.95), service effectiveness (2.97, 1.03), patient satisfaction (2.79, 1.37), and patient loyalty (3.01, 0.42) are also noted. Discriminant validity was assessed using the square root of the average variance extracted (AVE). Table 4 demonstrates satisfactory discriminant validity, as the square root of each construct’s AVE was more significant than the correlations among the latent variable pairs.
 |
Table 4 Descriptive Statistics & Correlations |
Confirmatory Factor Analysis (CFA)
The results of the confirmatory factor analysis (CFA) are presented in Table 5. This table compares our baseline model, a 6-factor model, with several alternative models, including 5-factor, 4-factor, 3-factor, 2-factor, and 1-factor models. In the 5-factor model, we combined the BI and PAL factors into a single variable. The 4-factor model further merged BI, PAL, and AP into one variable. Similarly, in the 3-factor model, we combined PAL, BI, AP, and SE into a single variable. The findings indicate that the 6-factor model is the best fitting, with the following fit indices: χ2 = 842.31, CFI = 0.98, TLI = 0.95, and RMSEA = 0.04. Additionally, all indicators exhibited factor loadings greater than 0.50, suggesting significant loadings. We utilized several fit indices during the CFA analysis, including χ2, χ2/df, CFI, IFI, TLI, and RMSEA. Notably, a χ2/df value below 0.06 is preferred.57 Previous research has established the desired thresholds for model fit indices: CMIN/DF should be ≤ 3, GFI ≥ 0.8, TLI and CFI ≥ 0.9, and RMSEA and SRMR should be ≤ 0.08.58
 |
Table 5 CFA Results |
Hypotheses Testing
The hypotheses were tested using AMOS 25.0 in conjunction with SEM. The H1 demonstrated a significant positive association between service effectiveness and patient loyalty, with values of (β = 0.22; t = 3.666; p < 0.01). The H2 posited a positive and significant connection between service effectiveness and administrative procedures, which was supported by values of (β = 0.27; t = 4.354; p < 0.01). The H3 suggested a positive and significant relationship between service effectiveness and patient satisfaction, with values of (β = 0.32; t = 5.432; p < 0.01) providing strong support for this claim. The H4 indicated a positive and significant relationship between administrative procedures and loyalty, confirmed by values of (β = 0.39; t = 6.842; p < 0.01). Finally, the H5 proposed a positive and significant relationship between patient satisfaction and loyalty, supported by (β = 0.34; t = 5.238; p < 0.01) values. Further, hypothesis testing (H1-H5) values can be seen in Table 6.
 |
Table 6 Results (H1-H5) |
As suggested by Preacher and Hayes59 and Baron and Kenny,60 mediation was examined based on the significance of the indirect effect. Table 7 shows that administrative procedure positively mediates the relationship between service effectiveness and patient loyalty (β = 0.127, p < 0.001). The bootstrap results, at a 95% confidence level, indicate that the confidence intervals do not include zero (Lower Limit of Confidence Interval (LLCI) = 0.289, Upper Limit of Confidence Interval (ULCI) = 0.381. Thus, these findings support hypothesis H6. Additionally, patient satisfaction significantly mediates the relationship between service effectiveness and patient loyalty (β = 0.137, p < 0.001). The bootstrap results for this mediation also reflect a 95% confidence level,61 with confidence intervals that do not contain zero (LLCI = 0.313, ULCI = 0.537), thereby supporting hypothesis H7 as well.
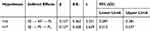 |
Table 7 Bootstrapping Indirect Effects |
Moderation Effects
The moderating effects were evaluated using moderated multiple regression. According to Pattali, Sankar62 If the interaction variable of participative leadership influences the relationship between AP and PL, the statistical significance of this moderating effect can be confirmed. Similarly, if the interaction variable of the brand image affects the association between PS and PL, the statistical significance of this moderating effect can also be established. The moderation hypotheses are significant (see Table 8).
 |
Table 8 Moderation Testing |
Discussion
This research analyzed the association between indices of service effectiveness, administrative procedures, patient satisfaction, patient loyalty, participative decision-making, and brand image in relation to medical service quality. The findings indicate a positive connection between service effectiveness and administrative procedures. Improved executive functions can enhance service levels, as discussed by.59 Additionally, Akanyako63 noted a strong link between administrative actions and performance quality, which is crucial for fostering patient loyalty. Asnawi, Awang49 also found a significant relationship between management processes and services, highlighting that administrative functions serve as the backbone of hospitals in developing patient loyalty. Furthermore, the study demonstrates that service effectiveness is a key factor in improving administrative procedures and enhancing patient loyalty in terms of hospital performance.41
Clinician shortcomings can weaken consumer loyalty, as the timeliness, relevance, and accuracy of communication are more crucial to a patient’s loyalty than how often they communicate.64 The quality of care, responsiveness, and ability to address patients’ broader health needs often serve as benchmarks for measuring healthcare success. When healthcare providers consistently deliver effective services, they foster stronger patient loyalty.65 In healthcare settings, Harriet, Arthur66 emphasize that dimensions of service quality, including service effectiveness, are linked to patient loyalty. Additionally, a systematic review by Kalaja67 indicates a direct correlation between high service achievement and an increased number of patients. Research by Andreano and Pardede68 has shown that the innovation of patient-centered approaches among healthcare organizations enhances patient experience. This improvement, driven by better service delivery, is crucial in fostering patient loyalty in a competitive market.
Afifi and Amini20 explored the relationship between customers and service providers in the service sector. In a related study,49 a significant link between customer satisfaction and loyalty was identified. Additionally, a study emphasized that services convey administrative values positively. In hospitals, administrative procedures and patient satisfaction are closely linked, regardless of whether the setting is public or private.69 It was agreed that the ease and efficiency of administrative processes directly influence patient satisfaction.42 Scholars have indicated in their research that the administrative counter serves as the initial point of contact for concerned visitors.6 Kanwel, Ma27 suggested that an administrative counter could create a more comfortable environment for anxious individuals, ultimately improving patient satisfaction through strong connections and adequate facilities. Enhanced training sharpens managerial responsibilities among staff, equipping them to navigate challenging and demanding situations more effectively, which in turn helps them maintain their mental well-being and fulfill their duties.20 Patient misbehavior often stems from frustration over unreasonable delays. In the context of healthcare in Pakistan, individuals are encountering difficulties with administrative procedures, including online appointments, registration, and test results, which are currently essential.1
Patient loyalty can only be established when patients and their associates feel they are treated effectively and warmly by the hospital and its facilities. It is widely recognized that patient loyalty is one of the most critical success factors in the healthcare service sector, largely due to the highly competitive nature of the industry.3 Effective administrative procedures and high-quality services enhance patient satisfaction, which in turn fosters loyalty. Conversely, if the connection between these elements is weak, service delivery may falter, leading to a decline in both patient satisfaction and loyalty.6 A study found a strong association between patient satisfaction and service quality, which in turn fosters loyalty. Similarly, an analysis of healthcare emphasized that service effectiveness is essential for building patient loyalty. Additionally, a hospital-related study revealed the interconnection between patient satisfaction and loyalty, highlighting the need for improved service quality.23 This research identified a significant correlation between service effectiveness, administrative procedures, and patient loyalty. Currently, the services in Pakistan are not being delivered efficiently, leading to dissatisfaction among patients and their families.8
A significant research area in healthcare management focuses on the relationship between service effectiveness and patient loyalty. Recent studies indicate that this relationship is mediated by patient satisfaction. Research has demonstrated a correlation between service effectiveness defined by quality, efficiency, and timeliness of health services and higher levels of patient satisfaction.70 Satisfied patients are more likely to exhibit loyalty toward healthcare providers, which in turn contributes to patient retention and increased loyalty.71 The findings across various studies consistently highlight the mediating role of patient satisfaction as a crucial factor influencing the relationship between service quality and patient loyalty.72
Similarly, patient perceptions of service effectiveness are affected by administrative procedures, such as appointment scheduling, waiting times, and accessibility of healthcare services.73 These administrative procedures can either enhance or detract from the overall patient experience, thereby influencing their satisfaction and loyalty.74 Empirical evidence suggests that well-organized administrative procedures can moderate the relationship between service effectiveness and patient loyalty, particularly when streamlined operations lead to improved patient experiences and heightened satisfaction.75 Consequently, both patient satisfaction and administrative procedures play vital roles in fostering patient loyalty, as they mediate the impact of service effectiveness on patient engagement with healthcare providers. Administrative performance directly influences the level of patient satisfaction, which is a critical factor that, when increased, also enhances patient loyalty. High levels of patient loyalty contribute to the institution’s success, fostering a positive public image of the hospital and showcasing the professionalism of its staff.6 The study further reveals that PS plays a key role in mediating the relationship between AP and PL. PS is essential for establishing the hospital’s image and business within the healthcare sector.49 Additionally, recent research indicates that brand image moderates the relationship between patient loyalty and patient satisfaction, with a strong brand image amplifying this connection. A positive reputation further boosts patient satisfaction; when healthcare providers possess a favorable brand image, satisfied patients are more likely to exhibit greater brand loyalty.76
The importance of patient satisfaction in improving service quality and hospital staff performance cannot be overlooked. There are statistically significant connections among administrative procedures, effectiveness, patient satisfaction, and patient loyalty, with both service effectiveness and PS mediating the relationship between AP and PL. Although the impact of administrative procedures on service effectiveness is relatively minor, satisfaction with specific healthcare experiences is crucial. The relationship between patient satisfaction and loyalty is vital within the context of hospital services, particularly under the Baldrige healthcare framework. This study reinforces the importance of leadership in enhancing service delivery, satisfaction, and loyalty.
Limitations
This research has several limitations. Firstly, it was conducted in five districts of South Punjab, and the findings are based on specific numerical data; increasing the sample size could provide more comprehensive results. The model used in this study can be scaled up or down and applied to any service industry. Additionally, extending the data collection period could provide a deeper understanding of the industry. Finally, this study can also be relevant to private hospitals within the same districts.
Conclusion & Implication
Conclusion
Pakistan is currently experiencing a political and economic crisis that adversely affects the service delivery of all institutions, particularly in the health sector. This research highlights several key areas that need to be addressed. Firstly, the health sector requires increased funding to implement modern technology effectively. Additionally, hospitals should organize regular training sessions for their staff to enhance their skills. Secondly, the administrative procedures within the health system are cumbersome. Patients are often required to navigate multiple counters separately for admission, medication, and medical test reports, which can involve significant distance and effort. This fragmented system hinders efficiency and patient care. Finally, while the services currently offered are satisfactory to some extent, significant improvements are necessary to meet the needs of the population.
This research identifies the interrelations among service effectiveness, administrative procedures, patient satisfaction, and patient loyalty as key determinants of medical service quality. The findings support the notion that service effectiveness is critical in enhancing administrative procedures and fostering patient loyalty. Effective and efficient services meet patients’ needs, thereby increasing their trust and satisfaction. Furthermore, administrative procedures serve as the operational backbone, with the ease, efficiency, and responsiveness of these processes significantly impacting patient satisfaction and loyalty.
The results indicate that administrative performance is indirectly linked to patient loyalty, with patient satisfaction acting as a mediator in this relationship. Well-structured administrative processes, along with timely, accurate, and patient-centered care, play a crucial role in building loyalty, particularly in competitive healthcare markets. Conversely, patient dissatisfaction arises from inefficiencies in service delivery and administrative activities, which can undermine loyalty and harm the hospital’s public image. This is especially evident in environments plagued by administrative hurdles, such as long wait times for appointments or test results.
Building on these findings, a new conceptual framework is proposed: the Service Quality Loyalty Framework (SQLF). This framework integrates service effectiveness, administrative performance, and patient satisfaction as interrelated drivers of patient loyalty. It emphasizes the following key elements: (1) Administrative excellence: Streamlining processes to minimize patient frustration and maximize satisfaction. (2) Service quality: Ensuring the timely, accurate, and patient-centered delivery of healthcare. (3) Satisfaction-driven loyalty: Positioning patient satisfaction as both a mediator and a primary predictor of loyalty. Healthcare leaders must focus on innovating patient-centered care, strengthening administrative functions, and fostering a culture of compassionate continuous improvement to leverage this framework fully. Future studies will explore the application of this framework in other healthcare settings and assess its impact on patient loyalty and organizational success. Implementing this framework offers hospitals the opportunity to deliver highly competitive service quality and cultivate long-term trust and loyalty among patients.
Implications
Medical and healthcare sector managers are responsible for designing and implementing strategic and operational plans for their hospitals. This study aims to assist governments and hospital administrative bodies in Pakistan. As the patient population continues to grow, there is an increasing demand for medical professionals, such as doctors and nurses. Hospital administration must prioritize critical issues, including staff helpfulness, the speed of responses to inquiries at the front desk, the friendliness of registration staff, and the effectiveness of the complaints system. Consequently, the findings of this study provide valuable and applicable insights into healthcare administration. These insights can help ensure that skilled physicians and nurses deliver high-quality patient care, which may enhance patient satisfaction and foster loyalty. By creating a supportive environment and increasing the number of medical doctors and nurses, hospital administration can reduce patient wait times and ultimately improve overall patient satisfaction.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available by the first author without undue reservation.
Ethics Statement
The present study obtained approval from the Research Ethics Committee of King Saud University, Saudi Arabia. Additionally, this study also got approval from the Ethics Committee of Islamia University, Bahawalpur, Pakistan and complied with the Declaration of Helsinki. Before participation, the subjects were fully informed of the content and purpose of the survey. Informed consent was obtained from all subjects who were involved in the study.
Acknowledgments
This study acknowledges the Youth Innovation Team Development Plan for Universities in Shandong Province (2022KJ339) as well as acknowledges King Saud University, Riyadh, Saudi Arabia(RSP2025R332).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or all these areas; took part in drafting, revising and critically reviewing the article; gave final approval of the version published; have agreed on the journal to which the article has been submitted.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Malik M, Prescott K, Khalid M, et al. Expectations and experiences of women regarding maternal healthcare services in Pakistan: challenges and lessons to be learnt. J Pharm Policy Pract. 2021;14(1):1–9. doi:10.1186/s40545-021-00392-x
2. Miethke-Morais A, Cassenote A, Piva H, et al. COVID-19-related hospital cost-outcome analysis: the impact of clinical and demographic factors. Braz J Infect Dis. 2021;25.
3. Kumar P. Managing service flexibility in healthcare for improved customer experience: a data-driven approach. J Strateg Mark. 2022:1–22.
4. Tan CC, Lam CSP, Matchar DB, et al. Singapore’s health-care system: key features, challenges, and shifts. Lancet. 2021;398(10305):1091–1104. doi:10.1016/S0140-6736(21)00252-X
5. Ali BJ, Anwar G. The effect of marketing culture aspects of healthcare care on marketing creativity. Int J Engl Lit Soc Sci. 2021;6(2):171–182. doi:10.22161/ijels.62.25
6. Asif M, Jameel A, Sahito N, et al. Can leadership enhance patient satisfaction? Assessing the role of administrative and medical quality. Int J Environ Res Public Health. 2019;16(17):3212. doi:10.3390/ijerph16173212
7. Schaefer C. Baldrige 20/20: An Executive’s Guide to the Criteria for Performance Excellence. Quality Press; 2011.
8. Asif M, Jameel A, Hussain A, et al. Linking transformational leadership with nurse-assessed adverse patient outcomes and the quality of care: assessing the role of job satisfaction and structural empowerment. Int J Environ Res Public Health. 2019;16(13):2381. doi:10.3390/ijerph16132381
9. D’Souza SC, Sequeira A. Application of MBNQA for service quality management and performance in healthcare organizations. Int J Eng Sci Technol. 2011;3(7):73–88. doi:10.4314/ijest.v3i7.6S
10. Fry LW, Latham JR, Clinebell SK, et al. Spiritual leadership as a model for performance excellence: a study of Baldrige award recipients. J Manage Spiritual Religion. 2017;14(1):22–47. doi:10.1080/14766086.2016.1202130
11. Um KH, Lau AK. Healthcare service failure: how dissatisfied patients respond to poor service quality. Int J Oper Prod Manage. 2018;38(5):1245–1270. doi:10.1108/IJOPM-11-2016-0669
12. Ayu NF, Pasinringi SA, Sidin AI. The effect of patient experience on patient satisfaction and loyalty at the inpatient room South Sulawesi Provincial Hospitals. J Pharm Negat Results. 2022;13(4):2112–2119.
13. Astarini Y, Fachrodji A. The effect of promotion, quality of service and price on patient loyalty with patient satisfaction as mediation. Int J Soc Manage Stud. 2023;4(2):37–45.
14. Card D, Fenizia A, Silver D. The health impacts of hospital delivery practices. Am Econ J. 2023;15(2):42–81.
15. Alibrandi A, Gitto L, Limosani M, et al. Patient satisfaction and quality of hospital care. Evaluat Prog Plann. 2023;97:102251. doi:10.1016/j.evalprogplan.2023.102251
16. Gejea T, Abadiga M, Hasen T. Maternal satisfaction with delivery services of government hospitals in Ambo town, West Shoa zone, Oromia region, Ethiopia, 2020. Patient Prefer Adherence. 2020;14:1225–1235. doi:10.2147/PPA.S251635
17. Vrontis D, El Chaarani H, El Abiad Z, et al. Managerial innovative capabilities, competitive advantage and performance of healthcare sector during Covid-19 pandemic period. Foresight. 2022;24(3/4):504–526. doi:10.1108/FS-02-2021-0045
18. Tushar SR, Moktadir MA, Kusi-Sarpong S, et al. Driving sustainable healthcare service management in the hospital sector. J Cleaner Prod. 2023;420:138310. doi:10.1016/j.jclepro.2023.138310
19. Aagja JP, Garg R. Measuring perceived service quality for public hospitals (PubHosQual) in the Indian context. Int J Pharm Healthcare Mark. 2010;4(1):60–83. doi:10.1108/17506121011036033
20. Afifi I, Amini A. Factors affect to relationship marketing for creating customer loyalty in hospital services business. ASEAN Mark J. 2021;10(2):2.
21. Khan MT. Customers loyalty: concept & definition (a review). Int J Inf Bus Manage. 2013;5(3):168–191.
22. Knox S. Loyalty-based segmentation and the customer development process. Eur Manage J. 1998;16(6):729–737. doi:10.1016/S0263-2373(98)00049-8
23. Juhana D, Manik E, Febrinella C, Sidharta I. Empirical study on patient satisfaction and patient loyalty on public hospital in Bandung, Indonesia. Int J Appl Bus Econ Res. 2015;13(6):4305–4326.
24. Chaabouni S, Abednnadher C. The relationship between patient satisfaction and service quality: a study of hospitals in Tunisia. Indian J Health Wellbeing. 2014;5(3).
25. Vimla, Taneja U. Brand image to loyalty through perceived service quality and patient satisfaction: a conceptual framework. Health Serv Manage Res. 2021;34(4):250–257. doi:10.1177/0951484820962303
26. Cham TH, Cheng BL, Low MP, Cheok JB. Brand image as the competitive edge for hospitals in medical tourism. Eur Bus Rev. 2020;33(1).
27. Kanwel S, Ma Z, Li M, et al. The influence of hospital services on patient satisfaction in OPDs: evidence from the transition to a digital system in South Punjab, Pakistan. Health Res policy Syst. 2024;22(1):93. doi:10.1186/s12961-024-01178-8
28. Zahra SA, Farida N, Arso SP. Perceived value and trust towards patient loyalty: a literature review. Med Technol Public Health J. 2022;6(1):39–50. doi:10.33086/mtphj.v6i1.3214
29. Bin KJ, Santana Alves PG, Costa R, et al. User experience regarding digital primary health care in Santarém, Amazon: evaluation of patient satisfaction and Doctor’s feedback. JMIR Format Res. 2023;7:e39034. doi:10.2196/39034
30. Aladwan MA, Salleh HS, Anuar MM, Aladwan RM. Patient trust and its impact on patient satisfaction and loyalty. Tuijin Jishu/J Propuls Technol. 2023;44(4):498–506.
31. Alipour J, Mehdipour Y, Karimi A, et al. Security, confidentiality, privacy and patient safety in the hospital information systems from the users’ perspective: a cross-sectional study. Int J Med Inform. 2023;175:105066. doi:10.1016/j.ijmedinf.2023.105066
32. Wong K, McLaughlan R, Collins A, et al. Designing the physical environment for inpatient palliative care: a narrative review. BMJ Support Palliat Care. 2023;13(1):45–51. doi:10.1136/bmjspcare-2021-003087
33. Babakus E, Mangold WG. Adapting the SERVQUAL scale to hospital services: an empirical investigation. Health Serv Res. 1992;26(6):767.
34. Putri S, Nur Afifah T, Ghiffary H, et al. Factors related to patient satisfaction with hospital health care. An-Najat. 2023;1(2):20–28. doi:10.59841/an-najat.v1i2.29
35. Amporfro DA, Boah M, Yingqi S, et al. Patients satisfaction with healthcare delivery in Ghana. BMC Health Serv Res. 2021;21(1):1–13. doi:10.1186/s12913-020-05996-8
36. World Health Organization. World Health Statistics 2016 [OP]: Monitoring Health for the Sustainable Development Goals (Sdgs). World Health Organization; 2016.
37. Kausar M, Siddharth V, Singh AR, et al. Hospital administration control room: an effective concept for managing hospital operation issues: a study in tertiary care public sector hospital. Int J Res Found Hosp Healthc Adm. 2018;6:82–90. doi:10.5005/jp-journals-10035-1097
38. Carr-Hill RA. The measurement of patient satisfaction. J Public Health. 1992;14(3):236–249.
39. Ng JH, Luk BH. Patient satisfaction: concept analysis in the healthcare context. Patient Educ Couns. 2019;102(4):790–796. doi:10.1016/j.pec.2018.11.013
40. Dunsch F, Evans DK, Macis M, et al. Bias in patient satisfaction surveys: a threat to measuring healthcare quality. BMJ Global Health. 2018;3(2):e000694. doi:10.1136/bmjgh-2017-000694
41. Abekah-Nkrumah G, Yaa Antwi M, Braimah SM, et al. Customer relationship management and patient satisfaction and loyalty in selected hospitals in Ghana. Int J Pharm Healthcare Mark. 2021;15(2):251–268. doi:10.1108/IJPHM-09-2019-0064
42. Yubing G, Ye ZH, Xin XI, et al. Exploring the relationship between service quality of private hospitals and patient loyalty from the perspective of health service. Iran J Public Health. 2020;49:1097–1105.
43. Okolo CA, Ijeh S, Olawumi Arowoogun J, et al. Reviewing the impact of health information technology on healthcare management efficiency. Int J Med Res. 2024;4(4):420–440. doi:10.51594/imsrj.v4i4.1000
44. Curry A, Sinclair E. Assessing the quality of physiotherapy services using SERVQUAL. Int J Health Care Qual Assur. 2002;15:197–205. doi:10.1108/09526860210437412
45. Casado Diaz AB, Más Ruíz FJ. The consumer’s reaction to delays in service. Int J Serv Ind Manage. 2002;13(2):118–140. doi:10.1108/09564230210425331
46. Aliman NK, Mohamad WN. Perceptions of service quality and behavioral intentions: a mediation effect of patient satisfaction in the private health care in Malaysia. Int J Mark Stud. 2013;5(4):15. doi:10.5539/ijms.v5n4p15
47. Woodside AG, Frey LL, Daly RT. Linking service quality, customer satisfaction, and behavior. Mark Health Serv. 1989;9(4):5.
48. Kumar NP, Jacob A, Thota S. Impact of healthcare marketing and branding on hospital services. Int J Res Found Hosp Healthc Adm. 2014;2(1):19–24. doi:10.5005/jp-journals-10035-1010
49. Asnawi A, Awang Z, Afthanorhan A, et al. The influence of hospital image and service quality on patients’ satisfaction and loyalty. Manage Sci Lett. 2019;9(6):911–920. doi:10.5267/j.msl.2019.2.011
50. Olesen K, Bathula H. A meta-analysis of the determinants of patient satisfaction and loyalty. Health Mark Q. 2022;39(2):191–210. doi:10.1080/07359683.2022.2050000
51. Tucker JL, Adams SR. Incorporating patients’ assessments of satisfaction and quality: an integrative model of patients’ evaluations of their care. Manag Serv Qual. 2001;11:272–287. doi:10.1108/EUM0000000005611
52. Aaker DA. Managing Brand Equity. Simon and Schuster; 2009.
53. Lee D. HEALTHQUAL: a multi-item scale for assessing healthcare service quality. Serv Bus. 2017;11:491–516. doi:10.1007/s11628-016-0317-2
54. Meesala A, Paul J. Service quality, consumer satisfaction and loyalty in hospitals: thinking for the future. J Retailing Consum Serv. 2018;40:261–269. doi:10.1016/j.jretconser.2016.10.011
55. Saunders M, Lewis P, Thornhill A. Research Methods for Business Students. Pearson education; 2009.
56. Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas. 1970;30(3):607–610. doi:10.1177/001316447003000308
57. Manzoor F, Wei L, Sahito N. The role of SMEs in rural development: access of SMEs to finance as a mediator. PLoS One. 2021;16(3):e0247598. doi:10.1371/journal.pone.0247598
58. Khan A, Bibi S, Ardito L, et al. Revisiting the dynamics of tourism, economic growth, and environmental pollutants in the emerging economies—sustainable tourism policy implications. Sustainability. 2020;12(6):2533. doi:10.3390/su12062533
59. Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi:10.3758/BRM.40.3.879
60. Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173. doi:10.1037/0022-3514.51.6.1173
61. Hussain A, Zhiqiang M, Li M, et al. The mediating effects of perceived usefulness and perceived ease of use on nurses’ intentions to adopt advanced technology. BMC Nurs. 2025;24(1):33. doi:10.1186/s12912-024-02648-8
62. Pattali S, Sankar JP, Al Qahtani H, et al. Effect of leadership styles on turnover intention among staff nurses in private hospitals: the moderating effect of perceived organizational support. BMC Health Serv Res. 2024;24(1):199. doi:10.1186/s12913-024-10674-0
63. Akanyako J. Does patient satisfaction and trust matter in the relationship between service quality and patient loyalty in the health sector? Afr J Empir Res. 2024;5(2):662–675. doi:10.51867/ajernet.5.2.59
64. Dayan M, Al Kuwaiti IA, Husain Z, et al. Factors influencing patient loyalty to outpatient medical services: an empirical analysis of the UAE’s government healthcare system. Int J Qual Reliab Manage. 2022;39(1):176–203. doi:10.1108/IJQRM-11-2020-0373
65. Chen L-H, Chen CH, Loverio JP, et al. Examining soft and hard attributes of health care service quality and their impacts on patient satisfaction and loyalty. Qual Manage Healthcare. 2024;33(3):176–191.
66. Harriet N, Arthur N, Komunda MB, et al. Service quality, customer loyalty and customer retention among private health care services in Mbarara City. Open J Social Sci. 2024;12(01):101–126. doi:10.4236/jss.2024.121008
67. Kalaja R. Determinants of patient satisfaction with health care: a literature review. Eur J Natl Sci Med. 2023;6(1):43–54. doi:10.2478/ejnsm-2023-0005
68. Andreano PR, Pardede R. Service quality and patient trust on patient loyalty mediated by patient satisfaction on inpatients. Interdiscip Soc Stud. 2023;2(12):2684–2692. doi:10.55324/iss.v2i12.595
69. Omaghomi TT, Akomolafe O, Onwumere C, et al. Patient experience and satisfaction in healthcare: a focus on managerial approaches-a review. Int J Med Res. 2024;4(2):194–209. doi:10.51594/imsrj.v4i2.812
70. Akbolat M, Sezer C, Ünal Ö, et al. The mediating role of patient satisfaction in the effect of patient visit experiences on word-of-mouth intention. Health Mark Q. 2021;38(1):12–22. doi:10.1080/07359683.2021.1947080
71. Fatima T, Malik SA, Shabbir A. Hospital healthcare service quality, patient satisfaction and loyalty: an investigation in context of private healthcare systems. Int J Qual Reliab Manage. 2018;35(6):1195–1214. doi:10.1108/IJQRM-02-2017-0031
72. AlOmari F, Hamid ABA. Strategies to improve patient loyalty and medication adherence in Syrian healthcare setting: the mediating role of patient satisfaction. PLoS One. 2022;17(11):e0272057. doi:10.1371/journal.pone.0272057
73. Nguyen NX, Tran K, Nguyen TA. Impact of service quality on in-patients’ satisfaction, perceived value, and customer loyalty: a mixed-methods study from a developing country. Patient Prefer Adherence. 2021;15:2523–2538. doi:10.2147/PPA.S333586
74. Zhang M, Du X, Jia G, et al. Comparative study on the satisfaction of healthcare service providers with the synergistic development of rural healthcare Systems in China: medical Alliance counties vs. non-medical Alliance counties. Int J Integr Care. 2024;24(2):26. doi:10.5334/ijic.7677
75. Htoo KZ. Marketing Mix on Patient Satisfaction and Loyalty at ma Har Myaing Hospital (Kyaw Zin Htoo, 2023). MERAL Portal; 2023.
76. Toreh C, Wuisan DSS. The influence of service quality, brand image, and communication on patient satisfaction and loyalty of urology patient at Siloam hospital manado in 2023. JMBI UNSRAT. 2024;11(1):505–522. doi:10.35794/jmbi.v11i1.53784
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

