Back to Journals » Patient Preference and Adherence » Volume 19
Are HIV Treatment Clients Offered a Choice of Differentiated Service Delivery Models? Evidence from Malawi, South Africa, and Zambia
Authors Mokhele I , Ntjikelane V , Scott NA , Kaiser JL , Morgan AJ, Huber A, Mokgethi NO , Tchereni TH, Phiri W, Kamanga A, Haimbe PM, Lumano-Mulenga P, Nyirenda RK, Pascoe SJS, Rosen S
Received 7 November 2024
Accepted for publication 10 May 2025
Published 25 June 2025 Volume 2025:19 Pages 1825—1841
DOI https://doi.org/10.2147/PPA.S494679
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Idah Mokhele,1 Vinolia Ntjikelane,1 Nancy A Scott,2 Jeanette L Kaiser,2 Allison Juntunen Morgan,2 Amy Huber,1 Nomcebo Oratile Mokgethi,1 Timothy Henry Tchereni,3 Wyness Phiri,3 Aniset Kamanga,4 Prudence Michelo Haimbe,4 Priscilla Lumano-Mulenga,5 Rose Kolola Nyirenda,6 Sophie JS Pascoe,1 Sydney Rosen1,2
1Health Economics and Epidemiology Research Office, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa; 2Boston University School of Public Health, Boston, MA, USA; 3Clinton Health Access Initiative, Lilongwe, Malawi; 4Clinton Health Access Initiative, Lusaka, Zambia; 5Ministry of Health, Lusaka, Zambia; 6Ministry of Health, Lilongwe, Malawi
Correspondence: Idah Mokhele, Health Economics and Epidemiology Research Office, Building C, First Floor, Sunnyside Office Park, 32 Princess of Wales Terrace, Parktown, Johannesburg, 2193, South Africa, Tel +27 10 001 7930, Email [email protected]
Purpose: Differentiated service delivery (DSD) models for antiretroviral therapy (ART) for HIV aim to increase patient-centeredness, a concept that incorporates patient choice of service delivery options. We explored choice in DSD model enrollment at 42 public sector clinics in Malawi, South Africa, and Zambia.
Methods: From 09/2022-05/2023, we surveyed people receiving HIV treatment to ask if they had a choice about DSD model enrollment and healthcare providers about their practices in offering choice. We estimated risk differences for ART clients’ self-reported offer of choice and report risk differences. We thematically analyzed open-ended questions and report key themes.
Results: We enrolled 1049 people receiving HIV treatment (Malawi 409, South Africa 362, Zambia 278) and 404 providers (Malawi 110, South Africa 175, Zambia 119). The proportion of study participants indicating that they had been offered a choice ranged from 4% in Malawi to 17% in Zambia to 47% in South Africa. Over 90% of people receiving HIV treatment in all three countries reported that they were happy to be enrolled in their current DSD model. Participants from urban (ARD 0.94 [0.90– 0.99]) and medium-volume facilities (2000– 4000 ART clients, 0.91 [0.84– 0.98]) were slightly less likely to be offered DSD enrollment. Participants in community-based models 1.21 [1.12– 1.30] and those satisfied with their current model 1.06 [1.01– 1.13] were more likely to be offered a choice. Among providers, 64% in Malawi, 80% in South Africa, and 59% in Zambia said they offered clients the choice to enroll in DSD or remain in conventional care.
Conclusion: As of 2023, relatively few people receiving HIV treatment in Malawi, South Africa, and Zambia reported being offered a choice about enrolling in a DSD model, despite most providers reporting offering such a choice. The value of patient choice in improving clinical outcomes and satisfaction should be explored further.
Plain-Language Summary: Differentiated service delivery (DSD) models for antiretroviral therapy (ART) enhance patient-centeredness by offering choices in service delivery options. We explored choice in DSD model enrollment at 42 public sector clinics in Malawi, South Africa, and Zambia. From 09/2022-05/2023, we interviewed people receiving HIV treatment and healthcare providers, asking participants whether they had a choice about DSD model enrollment and whether providers offered this choice to their patients. We analyzed the data to identify differences in how people receiving HIV treatment reported being offered a choice. 1049 people receiving HIV treatment participated: 409 from Malawi, 362 from South Africa, and 278 from Zambia, alongside 404 providers (110 in Malawi, 175 in South Africa, and 119 in Zambia). 4% in Malawi, 17% in Zambia, and 47% in South Africa reported being offered a choice to enroll in a DSD model. Few actively sought to join a DSD mode (Malawi 10%, South Africa 19%, and Zambia 13%)—but many consented to enroll even when not explicitly offered (Malawi 66%, South Africa 80%, Zambia 59%). Over 90% were happy with their current DSD model. Among providers, 64% in Malawi, 80% in South Africa, and 59% in Zambia reported offering patients the choice to enrol in a DSD model or remain in conventional care. Most people receiving HIV treatment in our study did not report being offered a choice to join a DSD model despite providers claiming they offered one. Further research is needed to understand how offering choices could improve health outcomes and satisfaction with care.
Keywords: antiretroviral therapy, differentiated service delivery, client choice, client-centered
Introduction
Differentiated service delivery (DSD) models for HIV treatment aim to increase the extent to which service delivery is client-centered, a term broadly defined as care that is holistic and responsive to individual needs.1–3 An important element is shared decision-making between providers and clients that empowers clients and can improve outcomes.4 DSD adjusts service delivery to meet the needs of treatment clients in terms of the location, frequency, and other characteristics of interactions with the healthcare system.5 For DSD for HIV treatment, healthcare systems are expected to offer treatment clients information about different options and a choice of available service delivery models so that individual clients can select the model that best meets their needs.6
Many sub-Saharan African countries have actively implemented differentiated service delivery for HIV treatment since 2016, when World Health Organization guidelines first recommended this approach.3 Research conducted in sub-Saharan Africa has demonstrated the benefits of DSD models for patients, providers and the health system. Among patients, improved access to care, higher patient satisfaction, lower costs of accessing care, and better clinical outcomes have been reported.7–9 Health providers report experiencing improved job satisfaction and workload and improved health system efficiency through decreased clinic congestion and better resource utilization.10–12 The years since then have seen countries experiment with, adopt, scale up, and retire various models of service delivery as they have gained experience with differentiation and the benefits and costs of specific DSD models. While DSD implementation continues to evolve, many countries are gradually converging on the widespread use of a few models for “established” or stable ART clients who have been on treatment for at least 6 months and are virally suppressed. These include multi-month dispensing of ART that reduces the frequency of clinic visits; facility-based fast-track models that allow clients to refill prescriptions without waiting in regular clinic queues; community-based medication pickup points; and, to a lesser extent, group or club models and home medication delivery. In most countries, clients may also opt to remain in conventional (undifferentiated) care, which generally requires4–6 full clinic visits and medication refills per year.
Each of these models offers established ART clients a different set of service delivery characteristics, benefits, and costs and should thus be preferred by different groups of clients, depending on their own circumstances and constraints.13 While national guidelines in many countries specify a range of DSD models to be made available,14–17 the extent to which clients are offered a choice of models, or of any differentiated model versus remaining in conventional care, is unclear. As part of a survey of the benefits and costs of DSD models for ART, we asked ART clients enrolled in DSD models in Malawi, South Africa, and Zambia whether they had been offered an opportunity to choose their model of care and explored which characteristics of clients and facilities were associated with being offered a choice. In addition, we asked providers whether they offer clients a choice between models and, if not, their reasons for not providing this choice.
Materials and Methods
Study Sites
The AMBIT Project’s SENTINEL 2.0 survey was the second round of a repeated, cross-sectional, interviewer-administered survey delivered to a sample of ART clients and healthcare workers at 12 public sector clinics in Malawi, 18 in South Africa, and 12 in Zambia during the period from September 2022 to May 2023. The study design has previously been published,18 and study sites are briefly described in Supplementary Table 1.
The study sites reported offering varying combinations of models of care, depending on national guidelines, facility size and resources, and, in the case of Malawi and Zambia, the presence of a nongovernmental partner organization that contributed equipment, staff, and other resources for specific models of care. For clients meeting criteria to be considered established on ART, medication dispensing intervals ranged from 2–6 months per pickup. Facility-based, six-month dispensing of medications was rapidly expanding in Malawi and Zambia at the time of the survey, and facilities in each country also offered community medication pickup points and various population-specific models such as teen/youth clubs and mother-infant pair clinics. South Africa offers three “less intensive” models for ART clients established on treatment, namely facility-based medication pickup points, external (out-of-facility) medication pickup points, and adherence clubs. (In South Africa, these options are known as Differentiated Models of Care (DMOC) and, as less intensive models, classified under Repeat Prescription Collection strategies (RPCs)). Although adherence club models and patient-led group models of care were originally popular, at the time of study enrolment, club and group models had been scaled back significantly because of COVID-19, and we did not encounter these models at most of the study sites. Supplementary Table 2 describes the lists of commonly offered models of care found in each country when the survey was administered.
For the current analysis the models of care were combined into three categories, based on a commonly used taxonomy of DSD models.5
- Facility-based individual models: These included facility medication pickup points, fast-track services, 6-month multi-month dispensing (MMD), and high-intensity models for ART clients who were not yet established on ART.
- Facility-based group models: This category comprised adherence clubs and family models, which were structured to support group-based care within the facility setting.
- Community-based group or individual models: These were either individual and group-based models implemented in the community. They encompassed community-based pickup points and home-delivery options for individuals. The group-based models, implemented within community settings, included patient or provider-led adherence or outreach groups.
Study Populations and Enrollment
We enrolled two discrete populations into SENTINEL 2.0. The first study population comprised adult ART clients; defined as ≥16 years in Malawi and≥18 years in other locations. To be eligible for inclusion in the study, ART clients were required to have 6 or more months’ experience on ART during which they received conventional, facility-based care. At this point, all participants had sufficient time on ART to qualify for DSD enrollment if they met other criteria for being designated as “established on ART”. They also needed to have received at least one medication refill in their current care model and be attending the clinic for routine HIV care. Clients who were not enrolled in a DSD model, those who had not received at least one medication refill in their current DSD model, or those attending the clinic for reasons unrelated to routine HIV care were excluded from the study. At each study site, up to 10 clients per active model of care were enrolled. Although clients remaining in conventional care (not enrolled in any DSD model) were also recruited for SENTINEL 2.0, they were not asked questions about DSD model choice and were not included in the analysis reported here. Providers identified potentially eligible patients through health records and referred them for study. Clients were enrolled in the survey sequentially as they arrived at the facilities for routine HIV-related care. Following written informed consent, they were administered a questionnaire by a study research assistant.
The second study population consisted of up to 10 healthcare providers at each facility. This group included three main categories:
- Healthcare Professionals: This includes nurses, doctors, and clinicians who are involved in patient care and clinical decision-making.
- Lay Health Workers: This category includes lay counsellors, peer educators/ navigators, and community health workers who provide essential support and education to patients.
- Support and Administrative Staff: This group includes data clerks, data capturers, and other administrative personnel who support the operational aspects of healthcare delivery.
Eligible providers had been working at the facility for a minimum of six months and self-reported being involved in implementing DSD models. Potential respondents were referred to the study team by the facility manager and were asked for written informed consent. They were then interviewed by a research assistant using a structured questionnaire. Further details on enrollment procedures for both study populations have previously been published.18
Survey Questions Regarding Choice of DSD Model
Survey instruments for both populations were designed by the study team and included quantitative and open-ended questions aimed at understanding clients’ experiences and providers’ perspectives. Clients were asked if they were offered a choice of model enrollment; if they had asked to be enrolled in their current model; if they provided consent for DSD model enrollment (written or verbal); if they were happy to be enrolled in their current model; and whether they would prefer a different model. Providers were asked two questions concerning the offer of choice to clients. The first question inquired whether providers offered established clients the option to enrol in a DSD model or not; if they chose not, they would remain in conventional (non-DSD) care. The second question asked whether they provided established clients with a choice among the available DSD models at the facility and, if not, their reasons for not offering this choice.
The survey also collected information on factors that could affect the offer of choice of DSD model enrollment among ART clients, including patient-related factors such as age and sex and duration of time the client had been on ART medication. Facility characteristics such as location (urban or rural) and size were also recorded. Facility size was based on the total number of patients on ART during the study enrolment period and was classified into three categories: facilities with 1000–2000 clients remaining on ART, facilities with 2000–4000 clients, 4000–6000 and facilities with more than 6000 clients. The exact language of the questions used in each survey is included in Supplementary files 1 and 2.
Data Analysis
We first describe participant characteristics for each population using proportions, frequencies, means with standard deviations, and medians with interquartile ranges (IQR), as appropriate. For the client survey, we report the proportions of respondents indicating that they were or were not offered a choice and the characteristics of clients, healthcare facilities, and DSD models that are associated with being offered a choice. We estimated the risk differences (RD) for self-reported offer of DSD model choice among study participants using a Poisson distribution with an identity link function. We adjusted for duration on ART, country, age, sex, facility size, and clinic locality and report adjusted risk differences (ARD) and 95% confidence intervals (CI).
For the provider survey, we describe provider characteristics using proportions, frequencies, means with standard deviations, and medians with interquartile ranges (IQR), as appropriate. We report the proportion of providers who reported offering ART clients a choice in DSD model participation. Open-ended questions from the provider survey were used to develop the codebook a priori. The codebook was refined after a reading of responses. All questions were then coded using Excel and analyzed thematically. Results were compared across countries and by respondent type, then triangulated with quantitative findings. Emerging themes were summarized and are presented with illustrative quotes which were lightly edited for clarity when needed.
Ethics
The study protocol was reviewed and approved by the Human Research Ethics Committee of the University of Witwatersrand in South Africa (protocol M210241), the Boston University Institutional Review Board (IRB) (protocol H-41402), the National Health Science Research Committee (NHSRC) in Malawi (protocol 21/03/2672), and ERES Converge Institutional Review Board in Zambia (protocol 2021-Mar-012). All participants provided written informed consent.
Results
ART Client Study Population
A total of 409, 362, and 278 ART clients were enrolled in Malawi, South Africa, and Zambia, respectively. Demographic and socioeconomic characteristics of participants and the DSD models in which they were enrolled are presented in Table 1. Consistent with overall ART uptake in sub-Saharan Africa, roughly two-thirds of participants were female. Unemployment was high in South Africa; informal employment was the most common occupation in Malawi and Zambia. Most participants had already been on ART for more than 5 years at the time of the survey.
 |
Table 1 Characteristics of ART Client Study Population (n=1049) |
ART Clients’ Self-Report of Offers of Choice in Model Participation
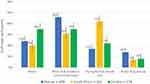
Figure 1 illustrates the share of participants in each country who indicated that they had asked to be enrolled in their current model of care, provided consent for DSD model enrollment (written or verbal), were given a choice about participating in their current model, and were happy to be enrolled in it. The proportion of participants indicating that they had been offered a choice ranged from 4% in Malawi to 17% in Zambia to 47% in South Africa. Fewer than 14% in each country (Malawi 10%, South Africa 19%, Zambia 13%) indicated they had actively asked to enroll in a DSD model.
Figure 1 Continued.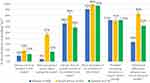
Despite participants’ self-reported lack of choice between DSD models, over two-thirds (Malawi 66%, South Africa 80%, Zambia 59%) indicated they consented to DSD model enrollment (in any model) rather than remaining in conventional care. Among the participants who reported providing consent for DSD model enrolment (723/1049), 22% gave written consent, and 78% gave verbal consent. In Malawi, South Africa, and Zambia, only 1%, 38%, and 4% provided written consent, respectively.
In all three countries, around 70% of individuals reported receiving counselling, education, or support before enrolling in their current model, and 60% said they understood the differences between their current and prior models of care. Overall, 38% discussed their choice of DSD model with their provider at their initial enrollment, and a quarter did so during their most recent clinical visit or drug pickup, though again with variation by country (Figure 1b). Despite the relative lack of choice offered, large majorities, in excess of 90% in all three countries, reported that they were happy to be enrolled in their current DSD model.
When asked if they were aware of other DSD models currently implemented in their facility and if they preferred any other model to their current model, all participants from South Africa and Zambia and 82% of those from Malawi said they were aware of other models (Table 2). Among those aware of other DSD models, a third said they would have preferred to be in a different model (48% in Malawi, 38% in South Africa, and 19% in Zambia).
 |
Table 2 Awareness of and Preferred DSD Model Among ART Client Study Population (n=1049) |
Qualitatively, among the few patients in Zambia (n=46) and Malawi (n=15) who responded to the open-ended question about having been given a choice, they primarily described it being a single option (ie they were offered one of the models) by the provider, with the choice to opt into that model or remain in conventional care. They primarily reported selecting the option that was more convenient, closer to home, or would save time and transport money. Illustrative quotes are included below:
[I] was asked if I would prefer the healthcare providers to deliver medication at my home or not. – Zambia, female patient, age 50-64
They [the providers] asked for those that were willing to join the community adherence groups. – Zambia, male patient, age 35-49
It was the choice to either remain in standard of care or switch to 6MMD. – Zambia, female patient, age 35-49
[I was given the choice] to either join adolescent group or not but was told of the benefits that come with joining it. – Zambia, female patient, age 20-24
To choose if I can be in 6MMD or not. – Malawi, Male Patient, Age 25-34
[I was given the choice] whether to join teen club or to be in standard of care. – Malawi, male patient, age 15-19
Choice of whether to accept getting medications from outreach or at the facility. – Malawi, female patient, age 50-64
Conversely, in South Africa (n=171), patients qualitatively described a much more varied experience. Many stated that providers explained the DSD model options to them as well as the benefits of different models and gave them an option for choosing either to remain on conventional care or opt for a facility or external medication pickup point. Most patients described choosing specifically where they would pick up their medication to make it most convenient for them. Patients also widely discussed choosing their DSD model because it would save them time due to shorter waits and queues and quicker service, which made their experience more convenient and easier. They connected the convenience with the locations of the pickup points (pharmacies, grocery stores, or the clinic), liking that the pickup points were close to either their homes or work, where they could easily walk to and did not require them to miss work. Multiple noted the convenience of someone else being able to pick up medications for them if needed. Illustrative quotes are included below:
They [the providers] gave me more options to choose from as to where to collect my medication in a convenient place for me. – South Africa, female patient, age 35-49
They [the providers] informed me and asked me nicely if it’s okay with me if they send me to collect medication at Clicks.* They also mentioned the benefits of collecting medication at the External pickup point. – South Africa, female patient, age 35-49 (*A commercial pharmacy chain in South Africa.)
I was given different external pickup points within the community, and I choose the one where I’m taking medication now. – South Africa, male patient, age 35-49
They [the providers] asked if I prefer to collect at clinic or go to the external pickup point so they did educate me also I was given a choice to choose my preferred method for ART collection they never forced or decided on my behalf. – South Africa, female patient, age 35-49
They [the providers] explained the available DSD models which they offer at this facility and that I can choose the one which will be convenient for me. – South Africa, female patient, age 25-34
Associations Between Being Offered a Choice and Client, Facility, and Model Characteristics
Neither age nor sex was associated with the probability of being offered a choice of models of care (Table 3). As mentioned above, choice was much more common in South Africa than in either Zambia or Malawi. Participants enrolled in urban facilities (ARD 0.94 [95% CI: 0.90–0.99]) and in sites with 2000–4000 ART clients were slightly less likely to be offered DSD model enrollment (2000–4000 ART clients vs <2000 ART clients, 0.91 [0.84–0.98]). Clients at high-volume sites, in contrast, were more likely to have requested DSD enrollment (4000–6000 ART clients vs 1000–2000 ART clients, 1.08 [1.00–1.16]), (>6000 ART clients vs 1000–2000 ART clients, 1.12, [1.04–1.22]). Compared to clients in facility-based individual care models, clients enrolled in community-based models were somewhat more likely to have been offered a choice (1.21, [1.12–1.30]) and more likely to have asked for DSD model enrollment (1.15, [1.08–1.22]). Finally, those reporting that they were happy with their current model of care were likely to have been offered a choice (1.06, [1.01–1.13]).
 |
Table 3 Crude and Adjusted Risk Differences for ART Clients’ Experiences of DSD Model Choice (n=1049) |
Health Provider Study Population
Characteristics of the 404 providers enrolled in the study are presented in Table 4. Consistent with the overall healthcare provider workforce, a majority were female. Most had been in their current positions for five years or more. Nurses at any level were most commonly enrolled in the study, particularly in South Africa, where they provide a large share of HIV care. In Malawi and Zambia, roughly half of the providers enrolled in the study were employees of partner organizations, rather than the Ministry of Health. In South Africa, the provincial departments of health employ most public-sector healthcare workers, including those enrolled in the study.
 |
Table 4 Characteristics of Health Providers Study Population (n=404) |
Health Provider Self-Report of Offering Choice to ART Clients
The majority of providers in all three countries stated that they do offer clients the option to choose between remaining in conventional care or enrolling in a differentiated model (Figure 2). Approximately 35% of providers in Zambia reported not offering this choice routinely, however, and a smaller proportion of providers said that they do not offer this choice occasionally, implying that they use personal judgment as to whether to make the offer to any individual client. Most providers also stated that they give clients an option among available DSD models, with this practice being most common in South Africa.
 |
Figure 2 Health provider self-report of offer of choice in DSD model participation to ART clients, by country (n=404). |
The majority (70%) of providers reported providing information about DSD models to all clients, regardless of the individual client’s DSD eligibility status (Figure 3). In all three countries, most of the information provided to patients about DSD models focused on eligibility criteria for enrolment, the frequency of visits, and the potential benefits of DSD models (Table 5).
 |
Table 5 Information Provided to Patients on Available DSD Models (n=404) |
 |
Figure 3 Clients to whom information about DSD models is conveyed, provider self-report (n=394). |
Providers in Malawi, South Africa, and Zambia reported that clients are informed about DSD models through multiple mechanisms (Table 6). Health education talks occurring in the common areas of the clinic throughout the day were the most widely described mechanism to convey information about DSD models, benefits, and eligibility criteria. Providers frequently noted that these talks are reinforced during one-on-one consultations or counseling sessions between providers and clients which provides clients the opportunity to ask further questions. Additionally, a few providers specifically discussed sharing information through brochures given to clients or posters in common areas of the clinic. Emerging themes were not substantively different between countries.
 |
Table 6 Information About DSD Models Offered at the Facility, as Reported by Providers (n=282)* |
When qualitatively explaining criteria for guiding clients on DSD model choices, providers in all three countries who responded (n=113, of whom 78% were from Malawi) discussed the official eligibility criteria for enrollment in DSD to first determine whether clients were eligible. Providers described offering choice to patients who were stable on treatment for at least six months and reported that the client’s home location was taken into account. For example, one provider in Zambia discussed that a group of patients who live close to each other might be enrolled in community adherence groups, while patients who live very far from the facility are recommended home delivery with 6MMD. Providers also discussed other criteria they might consider, such as age (teenagers often have separate DSD models), gender (if there are male-only models), comorbidities (which might affect the frequency or timing of clinic visits), and patients’ availability due to work or other obligations (to determine if it coincides with model requirements). As a crosscutting theme, providers discussed what they considered to be the right fit for the clients both within their ART treatment path and within their larger lives. Patient convenience and ability to benefit were key considerations (Table 7).
 |
Table 7 Providers’ Report of Criteria They Use for Guiding Patients on DSD Model Choice (n=110)* |
Providers were asked to generate ideas to improve DSD and client choice; emerging themes and illustrative quotes are presented in Table 8. Providers in all countries widely recommended providing clients with more information on the benefits and guidelines for DSD models to ensure they can make an informed choice. Providers discussed relaying this information to clients through multiple sources, including during counseling sessions, during general health education talks, through posters, on TV screens in the waiting areas, and in leaflets. A few providers noted the importance of this information being relayed in the primary language the patient spoke (eg Bemba in Zambia). Additionally, numerous providers described the importance of making this information available throughout the early treatment period, not only after the client becomes stable and eligible for enrollment in the DSD models. They speculated that early enrollment in DSD models could be motivating for good adherence if clients are informed of the benefits and eligibility requirements early in their treatment journey. Providers also recommended providing additional adherence support to clients so they can more quickly be eligible for DSD, including increased adherence counseling, outreach (SMS (text message), phone calls, or home visits if needed) after missed appointments, and interactions with peer educators.
 |
Table 8 Key Provider Suggestions for Facilitating Patient Choice of DSD Models (n=370)* |
During the conversation in which the client needs to choose their DSD mode, providers discussed the importance of offering complete information to the patients, including the benefits and drawbacks of each model. Many providers described either advising the patient on which model might be best suited for their needs or helping them to determine this, such as by identifying which external pickup point is closest to their home. Many also stated that it is just the client’s place to choose, and it was not clear from their responses whether those providers offered additional decision-making support.
Some providers suggested various forms of expanded DSD enrolment, with more patients on DSD models, more DSD models available, or more medication pickup location options.
A small number of providers suggested additional and continuous capacity building and education for the providers so they can better explain the model options to clients and assist in this decision-making support role.
Discussion
This mixed-methods study explored patient and provider perspectives on one element of client-centeredness of HIV treatment, the opportunity to choose a model of care. As of early 2023, 4% of HIV treatment clients enrolled in differentiated service delivery models in Malawi, 17% in Zambia, and 47% in South Africa reported being offered a choice of model prior to enrolment. Only a few in any of the focus countries said that they had asked to be enrolled in any DSD model, rather than remaining in conventional care, and over a third said that they would have preferred to be in a different model. On the other hand, roughly two-thirds reported consenting to DSD enrollment, and nearly all—between 91 and 99%—said that they were happy to be enrolled in their current model. Quantitative and qualitative data from providers (Figure 2 and Table 8) suggest that they strongly endorse the principles of client-centered care and even recommend that DSD models and choice be introduced earlier in a patient’s treatment journey as a strategy to improve adherence. In contrast to clients’ perceptions of their experience, most providers in all three countries reported they did usually offer clients the choice either to enroll in a DSD model or to remain in conventional care to clients.
Our survey suggests a disconnect between what providers believe they are offering, in terms of both the opportunity for choice and the greater value of their own judgement, and what clients are experiencing with regard to choice.2,8,19 Qualitatively, most participants said that they were given only one option, to enroll in a specific model or remain in conventional care. Client-centered care is a fundamental tenant, if not the raison d’etre, of the differentiated service delivery approach.5 Choice is considered a core element of patient empowerment and, thus, of client-centered care, which in turn has been shown to improve patient adherence and outcomes,20–23 including for HIV.21,24 To the extent that the importance of choice pertains to our study setting, DSD can only achieve its goals if patients have the opportunity to make their own decisions, where options are available. In our analysis (Table 3), we found that having been offered a choice was the factor most consistently associated with self-reported happiness to be in the client’s DSD model.
At the same time, the findings reported here suggest that being offered choice is not essential to overall, self-reported patient satisfaction with care received. Patients may find that the services they receive meet or exceed their expectations regardless of having had a choice, or they may be unaware of alternative options, leading to satisfaction by default rather than by preference.8,25,26 It is possible that clients simply prefer any DSD model to conventional care and/or that they had no expectation of being empowered to participate in decisions. Alternatively, some clients may prefer an “opt-out” approach to DSD models, in which they are enrolled in a model of the provider’s choice unless they actively express a different preference, in order to simplify clients’ lives, mitigate the burden or anxiety associated with having to make a choice, or reassure the clients of the expertise of the provider.19
In Malawi and Zambia, many facility-based DSD models limit enrollment based on individual characteristics such as gender (eg male adherence clinic), age (teen/youth clubs), current life stage such as being pregnant/post-partum (mother-infant pairs or family model clinic), or clinical condition (not being established on ART for a high viral load clinic). These requirements constrain the choices available to some clients, such that for some individuals at some study sites, only one DSD option would have been both available and suitable These limitations may have led healthcare providers to recommend only one specific model and may explain why study participants reported having less choice in these countries, a speculation supported by our qualitative results. Where more than one alternative was available, though, and clients were still assigned to a model based on their characteristics without being given a genuine opportunity to choose, then enrollment may not have truly reflected a personal preference.20,21,23,27 Providers in Malawi and Zambia may thus have an opportunity to improve outcomes by offering sufficient information about all models a client is eligible for (including remaining in conventional care) rather than solely the specific model that matches that individual’s characteristics. Actively involving the client in the decision-making process may also improve treatment outcomes,28,29 for example, by imbuing a sense of responsibility for self-management of care.30
An important finding of this study is that providers’ explanations of how they determine which DSD model(s) to recommend diverge from guidelines to some extent and clearly involve individual judgment (Table 6). The patient’s location, for example, was frequently cited as a reason for recommending one model over another, implying that distant patients may be offered community-based models like home delivery more frequently than those who live nearby. Location is not a criterion mentioned in DSD guidelines. More important, both distant and nearby patients may have other considerations that take priority for them as individuals, such as fear of disclosure to neighbors due to home delivery or a community adherence group. The provision of full information about all available models, without undue pressure to select the model recommended by the provider, may help offset this concern.
Our study had several limitations. With regard to patient results, response and recall biases, where participants may inaccurately report or remember details about the choices offered, are likely, as many participants were describing experiences that occurred several years in the past. Additionally, the lack of data on how long participants had been enrolled in a DSD model limits our ability to assess whether recall of being offered a choice was influenced by time in the model. Respondents may have had different interpretations of what constitutes a meaningful choice, and the influence of healthcare providers in presenting options could skew perceptions. Our study only included patients enrolled in DSD models; those who remained in conventional care at the time of the survey were excluded, even though many of them may have chosen the conventional care model. As a result, the study may not accurately reflect how choices are offered or perceived by patients who prefer or are recommended to remain in conventional care.
On the provider side, respondents may have overstated how often or effectively they offer choices to their ART clients. Recall bias could affect the accuracy of their recollections of client interactions, and variability in how they interpret the concept of offering a choice could lead to inconsistent responses. Social desirability bias may also cause providers to report practices that align with expected norms rather than their actual behaviors. Finally, the cross-sectional nature of the study also limits its ability to capture changes in provider practice or client experience over time and could also affect the reliability and generalizability of the findings.
Conclusion
One of the main goals of DSD—in fact, its primary goal--is to increase the client-centeredness of HIV treatment, which in turn entails offering clients the opportunity to choose among existing options for service delivery models. However, few clients in Malawi, South Africa, and Zambia reported being offered a choice, despite most providers having reported almost always offering DSD information and choice. Further examination of what clients and providers consider to constitute “choice” and improving healthcare provider communication with patients could improve client-centeredness. Future research should also explore the value of choice in improving both clinical and non-clinical outcomes, facilities’ capacity to offer choice and whether there is a quantity/quality tradeoff in having multiple options, whether choices evolve over clients’ lifetimes, and how to make the choice process dynamic over time.
Abbreviations
DSD, Differentiated service delivery; ART, antiretroviral therapy; HIV, human immunodeficiency virus; DMOC, Differentiated Models of Care; RPC, Repeat Prescription Collection Strategies; COVID-19, coronavirus disease 2019; MMD, multi-month dispensing; IQR, interquartile ranges; RD, risk differences; ARD, adjusted risk differences; CI, confidence intervals; CHW, Community Health Workers; SMS, short message service.
Data Sharing Statement
All data used in this study were collected by the study team following written informed consent. Data will be made available within one year after the closure of the study by the supervising ethics committees. At that time, data will be posted in a public data repository.
Ethics Approval and Consent to Participate
Ethical approval to conduct this study was granted by University of Witwatersrand (Medical) Human Research Ethics Committee in South Africa (Protocol M210241), the National Health Science Research Committee (NHSRC) in Malawi (protocol 21/03/2672), ERES Converge Institutional Review Board in Zambia (Protocol 2021-Mar-012), and by the Boston University Medical Campus Institutional Review Board in the United States (Protocol H-41402). All approvals were granted in accordance with the ethical principles of the Helsinki Declaration. Data collectors were trained in research ethics, the overarching study, and the specific survey instrument. Written informed consent was obtained from each participant before the survey commenced, including consent for the publication of anonymized responses and direct quotes.
Acknowledgments
We would like to express our gratitude to the staff at the study sites for their participation in the research. Additionally, we extend our thanks to the Malawi Ministry of Health, the South Africa National Department of Health, and the Zambia Ministry of Health for approving our research. We are especially thankful for the support provided by the Differentiated Service Delivery Technical Working Group in each country. We would also like to acknowledge the other members of the AMBIT SENTINEL study team for their contributions to the project at large: Frehiwot Birhanu, Nyasha Mutanda, Linda Sande, Nkgomeleng Lekodeba, Nkosinathi Ncgobo, Aniset Kamanga, and Taurai Makwalu.
Funding
Funding for the study was provided by the Bill & Melinda Gates Foundation through INV-037138 to the Wits Health Consortium. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Disclosure
The authors report no competing interests. PLM and RN are employees of the Ministry or Department of Health in their respective countries and thus have some supervisory authority over the study sites. This paper has been uploaded to MedRxiv as a preprint: https://www.medrxiv.org/content/10.1101/2024.12.09.24317166v1#:~:text=Over%2090%25%20of%20clients%20in,or%20remain%20in%20conventional%20care
References
1. Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press; 2001.
2. Johnsson A, Wagman P, Boman Å, Pennbrant S. What are they talking about? Content of the communication exchanges between nurses, patients and relatives in a department of medicine for older people—An ethnographic study. J Clin Nurs. 2018;27(7–8):e1651–e1659. doi:10.1111/JOCN.14315
3. World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. 2016. Available from: https://apps.who.int/iris/bitstream/handle/10665/208825/97892?sequence=1.
4. Dolan H, Li M, Trevena L. Interventions to improve participation in health-care decisions in non-Western countries: a systematic review and narrative synthesis. Health Expectations. 2019;22(5):894–906. doi:10.1111/hex.12933
5. Duncombe C, Rosenblum S, Hellmann N, et al. Reframing HIV care: putting people at the centre of antiretroviral delivery. Trop Med Int Health. 2015;20(4):430–447. doi:10.1111/tmi.12460
6. Ehrenkranz P, Grimsrud A, Rabkin M. Differentiated service delivery: navigating the path to scale. Curr Opin HIV AIDS. 2019;14(1):60–65. doi:10.1097/COH.0000000000000509
7. Kuchukhidze S, Long L, Rosen S, et al. Patient costs and satisfaction associated with differentiated models of service delivery for HIV treatment in sub-Saharan Africa. AIDS 2020. 2020. PEE1624.
8. Mokhele I, Huber A, Rosen S, et al. Satisfaction with service delivery among HIV treatment clients enrolled in differentiated and conventional models of care in South Africa: a baseline survey. J Int AIDS Soc. 2024;27(3):26233. doi:10.1002/jia2.26233/full
9. Jo Y, Jamieson L, Phiri B, et al. Attrition from HIV treatment after enrollment in a differentiated service delivery model: a cohort analysis of routine care in Zambia. PLoS One. 2023;18(3):e0280748. doi:10.1371/journal.pone.0280748
10. Ntjikelane V, Phiri B, Kaiser JL, et al. Effect of differentiated service delivery models for HIV treatment on healthcare providers’ job satisfaction and workloads in sub-Saharan Africa: a mixed methods study from Malawi, Zambia, and South Africa. Human Resources for Health. 2025;23(1):1–2. doi:10.1186/s12960-025-00993-6
11. Prust ML, Banda CK, Callahan K, et al. Patient and health worker experiences of differentiated models of care for stable HIV patients in Malawi: a qualitative study. PLoS One. 2018;13(7):e0196498. doi:10.1371/journal.pone.0196498
12. Phiri K, McBride K, Siwale Z, et al. Provider experiences with three- and six-month antiretroviral therapy dispensing for stable clients in Zambia. AIDS Care - Psychological and Socio-Medical Aspects of AIDS/HIV. 2020;33(4):541–547. doi:10.1080/09540121.2020.1755010
13. IAS – the International AIDS Society. Differentiated service delivery (DSD). 2022. Available from: https://www.differentiatedservicedelivery.org/models/treatment/.
14. Huber A, Pascoe S, Nichols B, et al. Differentiated service delivery models for HIV treatment in Malawi, South Africa, and Zambia: a landscape analysis. Glob Health Sci Pract. 2021;9(2):296–307.
15. National Department of Health. Differentiated models of care standard operating procedures: minimum differentiated models of care package to support linkage to care, adherence and retention in care. adherence guidelines for HIV, TB and NCDs 2023.
16. Ministry of Health and Population. Malawi integrated guidelines and standard operating procedures for providing HIV services: 2022 clinical management of HIV in children and adults. 2022.
17. Ministry of Health. Zambia differentiated service delivery framework. 2018. Available from: https://www.moh.gov.zm/wp-content/uploads/filebase/Zambia-Consolidated-Guidelines-for-Treatment-and-Prevention-of-HIV-Infection-2020.pdf.
18. Pascoe S, Huber A, Mokhele I, et al. The SENTINEL study of differentiated service delivery models for HIV treatment in Malawi, South Africa, and Zambia: research protocol for a prospective cohort study. BMC Health Serv Res. 2023;23(1):891. doi:10.1186/s12913-023-09813-w
19. Toerien M, Reuber M, Shaw R, Duncan R. Generating the perception of choice: the remarkable malleability of option-listing. Sociol Health Illn. 2018;40(7):1250–1267. doi:10.1111/1467-9566.12766
20. Rutten GEHM, Van Vugt H, De Koning E. Person-centered diabetes care and patient activation in people with type 2 diabetes. BMJ Open Diabetes Res Care. 2020;8(2):e001926. doi:10.1136/BMJDRC-2020-001926
21. Chinyandura C, Jiyane A, Tsalong X, Struthers HE, McIntyre JA, Rees K. Supporting retention in HIV care through a holistic, patient-centred approach: a qualitative evaluation. BMC Psychol. 2022;10(1):1–9. doi:10.1186/S40359-022-00722-X/PEER-REVIEW
22. Glover V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract Res Clin Obstet Gynaecol. 2014;28:25–35. doi:10.1016/j.bpobgyn.2013.08.017
23. Yu C, Xian Y, Jing T, et al. More patient-centered care, better healthcare: the association between patient-centered care and healthcare outcomes in inpatients. Front Public Health. 2023;11:1148277. doi:10.3389/FPUBH.2023.1148277/BIBTEX
24. Long L, Kuchukhidze S, Pascoe S, et al. Retention in care and viral suppression in differentiated service delivery models for HIV treatment delivery in sub-Saharan Africa: a rapid systematic review. J Int AIDS Soc. 2020;23(11):1–14. doi:10.1002/jia2.25640
25. Reidy W, Kambale HN, Hughey AB, et al. Client and healthcare worker experiences with differentiated HIV treatment models in Eswatini. PLoS One. 2022;17(5 May):e0269020. doi:10.1371/journal.pone.0269020
26. Mukumbang FC, Ndlovu S, van Wyk B. Comparing patients’ experiences in three differentiated service delivery models for HIV treatment in South Africa. Qual Health Res. 2022;32(2):238–254. doi:10.1177/10497323211050371
27. Glover A, Holman C, Boise P. Patient-centered respectful maternity care: a factor analysis contextualizing marginalized identities, trust, and informed choice. BMC Pregnancy Childbirth. 2024;24(1):1–13. doi:10.1186/S12884-024-06491-2/TABLES/5
28. Flickinger TE, Saha S, Moore RD, Beach MC. Higher quality communication and relationships are associated with improved patient engagement in HIV care. J Acquir Immune Defic Syndr. 2013;63(3):362–366. doi:10.1097/QAI.0B013E318295B86A
29. Okoli C, Brough G, Allan B, et al. Shared decision making between patients and healthcare providers and its association with favorable health outcomes among people living with HIV. AIDS Behav. 2021;25(5):1384–1395. doi:10.1007/s10461-020-02973-4
30. Mukumbang FC, Van Belle S, Marchal B, Van Wyk B. Towards developing an initial programme theory: programme designers and managers assumptions on the antiretroviral treatment adherence club programme in primary health care facilities in the metropolitan area of Western Cape Province, South Africa. PLoS One. 2016;11(8):e0161790. doi:10.1371/JOURNAL.PONE.0161790
 © 2025 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a
Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the
original author and source are credited.
© 2025 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a
Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the
original author and source are credited.