Back to Journals » Clinical Interventions in Aging » Volume 20
Association Between Frailty and Albuminuria in the Community-Dwelling Geriatric Population
Authors Lin CH, Chou CY , Li TC, Liu CS, Lin WY, Li CI, Yang CW, Lin CC
Received 18 February 2025
Accepted for publication 7 June 2025
Published 27 June 2025 Volume 2025:20 Pages 903—909
DOI https://doi.org/10.2147/CIA.S518738
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Chih-Hsueh Lin,1– 3 Che-Yi Chou,4– 6 Tsai-Chung Li,7 Chiu-Shong Liu,1,2 Wen-Yuan Lin,1,2 Chia-Ing Li,8 Chuan-Wei Yang,8 Cheng-Chieh Lin1,2,9
1School of Medicine, College of Medicine, China Medical University, Taichung, Taiwan, Republic of China; 2Department of Family Medicine, China Medical University Hospital, Taichung, Taiwan, Republic of China; 3Division of Geriatric Medicine, China Medical University Hospital, Taichung, Taiwan, Republic of China; 4Division of Nephrology, Asia University Hospital, Taichung, Taiwan, Republic of China; 5Department of Post-Baccalaureate Veterinary Medicine, Asia University, Taichung, Taiwan, Republic of China; 6Division of Nephrology, China Medical University Hospital, Taichung, Taiwan, Republic of China; 7Department of Public Health, College of Public Health, China Medical University, Taichung, Taiwan, Republic of China; 8Department of Medical Research, China Medical University Hospital, Taichung, Taiwan, Republic of China; 9Department of Healthcare Administration, College of Medical and Health Sciences, Asia University, Taichung, Taiwan, Republic of China
Correspondence: Cheng-Chieh Lin, China Medical University, No. 100, Sec. 1, Jingmao Road, Beitun Dist, Taichung City, 406040, Taiwan, Republic of China, Tel +886-4-22053366 ext 1013, Fax +886-4-22060248, Email [email protected]
Aim: Elderly with frailty are more at risk of cardiovascular disease and all-cause mortality than the general population. Albuminuria is a risk factor for atherosclerosis, a major cause of frailty. We investigated the association between frailty and albuminuria in community-dwelling elderly.
Methods: This was a cross-sectional study for analyzing 1347 participants aged at least 65 years in the north district of Taichung, Taiwan. We defined the frailty phenotype as at least three characteristics: weight loss, exhaustion, weakness, slow walking speed, and decreased physical activity. We collected random urine and measured all participants’ albumin/creatinine ratio (ACR). We analyzed the association between frailty and ACR using logistic regression with adjustments for confoundings.
Results: The average age of 1347 participants was 76 ± 7 years, and 649 (48.2%) were male. Two hundred and forty-two (18.7) participants were robust, 853 (63.3%) participants were pre-frail, and 242 (18%) were frail. One thousand sixty-four (79%) participants had an ACR < 30 mg/g; the highest ACR was 2825 mg/g. The odds ratio of ACR was 1.12 (95% confidence interval 1.05– 1.25, p = 0.001) with adjustments for age, body mass index, estimated glomerular filtration rate, diabetes, liver function, and cholesterol.
Conclusion: Frailty is associated with urinary albuminuria in community-dwelling elderly, and this association is independent of traditional and non-traditional cardiovascular risk factors.
Keywords: frailty, albuminuria, elderly, community, albumin
Background
Frailty is a prevalent geriatric syndrome that involves a decline of multiple systemic functions and is associated with increased all-cause mortality in the elderly.1 Frailty affects 11% of community-dwelling residents in Taiwan2 and 10.2% to 13.9% among inhospital patients.3 Fifty percent of patients with heart failure4 and twenty percent with diabetes had frailty.5–8 The prevalence of frailty is expected to rise with the aging population.9 Since frailty is associated with chronic disease, frailty has significant implications in clinical practice and public health.
Albuminuria is a marker of atherosclerosis10 and is associated with increased all-cause mortality in patients with chronic diseases.11 Atherosclerosis is linked to frailty, cognitive decline, neurodegenerative diseases, and malnutrition.12 The association between albuminuria and frailty was investigated in older patients.13 Low-grade albuminuria (less than 30 mg/g) is associated with frailty among community-dwelling middle-aged and older people.14 The urinary albumin creatinine ratio is linked to an increased incidence of frailty using a frailty index of at least 2.5 in a longitudinal follow-up for 5.3 years.15 We explore the association between urinary albumin creatinine ratio and frailty in community-dwelling elders. In this cross-sectional study, we defined frailty using a 5-item FRAIL score.16
Methods
We conducted a population-based cross-sectional study in the North District of Taichung city residents between 2009 and 2011.17 The age and sex distributions of the residents in the North District were similar to those in Taiwan. The five items of frailty include shrinking, weakness, poor endurance and energy, slowness, and low physical activity. Shrinking is an unintentional weight loss of more than 4.5 kg in one year. Weakness is the grip strength in the lowest quintile at baseline, measured by a handgrip dynamometer (TTM-110D, TTM, Tokyo, Japan) based on gender and body mass index (BMI) subgroups. Poor endurance and energy were measured using self-reports of exhaustion by two questions from the Center for Epidemiological Studies-Depression scale. Slowness was measured as the slowest quintile of the population in terms of subgroups of sex and height based on the 15 feet walking time. Low physical activity level was measured by energy expenditure using frequency, duration, and types of leisure activities reported by the participants. Participants with none of those mentioned above components were considered robust, whereas those with one or two were pre-fail, and those with more than two were frail.
Self-reported hypertension (HTN), diabetes mellitus (DM), and congestive heart failure (CHF) were recorded at enrollment. Hemoglobin (Hb), alanine transaminase (ALT), blood urea nitrogen (BUN), serum creatinine, uric acid, serum albumin, high-sensitivity c-reactive protein (hCRP), cholesterol, triglyceride, high-density lipoprotein (HDL), low-density lipoprotein (LDL), and urinary albumin creatinine ratio (ACR) were measured at the enrollment. The estimated glomerular filtration rate (eGFR) was calculated using the CKD-EPI formula.18
Statistical Analysis
We reported demographic data as the mean ± standard deviation in normally distributed or median (interquartile range) in not normally distributed continuous variables or percent frequency in categorical variables. We used Kolmogorov–Smirnov test to assess the distribution of continuous variables. The t-test or Mann–Whitney U-test were used for continuous variables according to their distribution. The Chi-square test was used for categorical variables. Because the distribution of ACR and hCRP are right-skewed, we used log-transformed ACR and hCRP in logistic regression.19 We used univariate and multivariate logistic regression to analyze the association between frailty and all parameters. The odds ratio (OR) was calculated, and a p less than 0.05 was considered significant. All data were analyzed using a standard statistical package (R version 4.1.2 Vienna, Austria) with tableone, rms, and finalfit packages.
Results
We enrolled 1347 participants in this study, and 649 (63.3%) were male. The average age was 74 ± 7 years old. Two hundred and fifty-two (18.7%) participants were robust, 835 (63.3%) participants were pre-frail, and 242 (18%) participants were frail (Table 1). Frail participants were older and had a lower BMI. Frail participants were more likely to have DM, HTN, and CHF. In the laboratory data, frail participants had lower ALT, eGFR, serum albumin, cholesterol, higher ACR, and hCRP.
 |
Table 1 Characteristics of All Participants |
ACR (log-transformed) was associated with frail (Table 2) in univariate (p < 0.001) and multivariable logistic regression (p = 0.006). The likelihood of being frail was increased with advancing age (p < 0.001 and < 0.001) and diabetes (p = 0.001 and 0.003) in univariable and multivariable regression. Males (p = 0.002 and < 0.001) and higher BMI (p = 0.010 and 0.038) were associated with a lower likelihood of being frail. An increased ALT (p < 0.001 and p = 0.029) and cholesterol (p = 0.033 and p = 0.001) were associated with less likelihood of frail in univariable and multivariable regression. An increased hCRP was associated increased chance of being frail. Factors related to frail in both univariable and multiple variable regression were selected in the model (Table 3). ACR (OR 1.12, 95% CI 1.05–1.25), hCRP (OR 1.36, 95% CI 1.19–1.54), age (OR 1.10, 95% CI 1.08–1.12), male (OR 0.53, 95% CI 0.38–0.72), BMI (OR 0.95, 95% CI 0.90–0.99), diabetes (OR 1.81, 95% CI 1.22–2.65), and ALT (OR 0.98, 95% CI 0.97–1.00) were independently associated with frail.
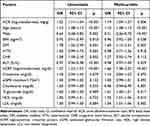 |
Table 2 The Odds Ratio of Pre-Frailty or Frailty in Univariable and Multivariable Logistic Regression |
 |
Table 3 Odd Ratio of Frail in Multivariable Logistic Regression |
We showed the OR of frail according to ACR in Figure 1. The OR and 95% CI of the OR were increased with the increased urinary ACR in multivariable logistic regression with adjustments for age, gender, BMI, diabetes, eGFR, hCRP and ALT. A histogram of urinary ACR (black bars) showed this distribution of ACR after log transformation.
We presented the OR and 95% CI of frail in subgroups (Figure 2) as a forest plot. The likelihood of frail was not different in participants with an ACR < 30 mg/g, 30–300 mg/g, and ≥300mg/g. Participants older than 90 had the highest likelihood of being frail, followed by participants aged between 80 and 89 and between 70 and 79 years. The possibility of being frail was higher in underweight participants (BMI < 18). Diabetic participants were likelier to be frail, and the OR of frail was 1.81 (95% CI 1.23–2.65, p = 0.002). Participants with CKD stage 1 were more likely to be frail than participants with no CKD (OR 2.74, 95% CI 1.05–7.07). The participants with an hCRP 1–3 mg/dl were more at risk of frail, and the OR of frail was 3.00 (95% CI 1.42–6.10, p = 0.003).
Discussions
This cross-sectional population-based study showed a linear correlation between frail and urinary ACR. The association is independent of traditional atherosclerosis risk factors such as DM, HTN, CHF, dyslipidemia and non-traditional atherosclerosis risks factors such as eGFR, and hCRP. The association of CHF and CKD is also supported by a recent study in geriatric CHF patients.20 Five-item frailty score, a more comprehensive range of ACR, and community-dwelling elders are the significant characteristics that distinguish this study from the previous studies.2,13–15 The increased likelihood of frail in CKD stage 1 participants supported the association of frail and ACR because an ACR > 30 mg/g is one of the CKD definitions21 in participants with an eGFR > 60 mL/min/1.73m2. The previous studies focused on the association between mildly increased albuminuria and frailty.22–25 The majority of our population with urine protein had an ACR between, 30–300 and >300 mg/g. Our findings supported an association of frailty and moderately/severely increased ACR in a community-based elder.
A lower eGFR is associated with frailty,26,27 and mobility disability.28 In this study, participants with an eGFR 30–59, 30–89, and ≥90 had a lower risk of being frail. This may provide an important clinical application that access for frailty should be considered among chronic kidney disease (CKD) patients with an eGFR < 30 (CKD stage 4). hCRP was originally a serum marker for bacterial infection and is widely used in the differential diagnosis of fever of unknown origin. Emerging research suggests that hCRP is also a marker for inflammation and atherosclerosis29 and is linked to multiple clinical outcomes such as mortality and sarcopenia.30,31 We also found a higher risk of frail in participants with an hCRP > 3 mg/dl compared to those with an hCRP < 1 mg/dl. The increased CRP in participants may support the association between inflammation/atherosclerosis and increased urine ACR. Most participants had an hCRP < 1 mg/dl because the study was conducted in the community.
There are some limitations of this study. First, we cannot determine the cause-and-effect relationship between ACR and frailty because of the cross-sectional study design. Second, chronic disease prevalence was low because the self-reported disease was used in this study. About 1.7% of the participants reported having CKD, but 21% were diagnosed with CKD, according to the eGFR and ACR readings. Third, while ORs from logistic regression facilitated multivariable adjustment, they must be interpreted carefully in this cross-sectional setting. Specifically, the OR can numerically overestimate the strength of an association compared to the prevalence ratio when the outcome (frailty) is common, as it may be in this geriatric population. Therefore, our reported ORs reflect the odds of prevalent frailty and should not be interpreted as direct estimates of relative risk.
Conclusions
Urinary albumin creatinine ratio is associated with frail in community-dwelling elderly. The association is an independent traditional atherosclerosis risk factor such as diabetes and hypertension.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Ethics Approval and Consent to Participate
The present study was approved by the institutional review board of China Medical University Hospital (DMR-97-IRB-055). Participants or their legal guardians have given their written informed consent to participate in the study before taking part. The study was conducted in accordance with the 2004 revision of the Declaration of Helsinki.
Acknowledgments
This paper has been uploaded to ResearchSquare as a preprint: https://www.researchsquare.com/article/rs-3142053/v1.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National Health Research Institutes of Taiwan (NHRI-EX98-9838PI) and China Medical University Hospital (DMR-113-056). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors have no conflicts of interest to declare in this work.
References
1. Steinmeyer Z, Piau A, Thomazeau J, et al. Mortality in hospitalised older patients: the WHALES short-term predictive score. BMJ Support Palliat Care. 2021. doi:10.1136/bmjspcare-2021-003258
2. Chang CI, Chan D-C, Kuo K-N, et al. Prevalence and correlates of geriatric frailty in a northern Taiwan community. J Formos Med Assoc. 2011;110(4):247–257. doi:10.1016/S0929-6646(11)60037-5
3. Soong J, Poots AJ, Scott S, et al. Quantifying the prevalence of frailty in English hospitals. BMJ Open. 2015;5(10):e008456. doi:10.1136/bmjopen-2015-008456
4. Denfeld QE, Winters-Stone K, Mudd JO, et al. The prevalence of frailty in heart failure: a systematic review and meta-analysis. Int J Cardiol. 2017;236:283–289. doi:10.1016/j.ijcard.2017.01.153
5. Kong LN, Lyu Q, Yao H-Y, et al. The prevalence of frailty among community-dwelling older adults with diabetes: a meta-analysis. Int J Nurs Stud. 2021;119:103952. doi:10.1016/j.ijnurstu.2021.103952
6. Diez-Villanueva P, Arizá-Solé A, Vidán MT, et al. Recommendations of the Geriatric Cardiology Section of the Spanish Society of Cardiology for the Assessment of Frailty in Elderly Patients With Heart Disease. Rev Esp Cardiol. 2019;72(1):63–71. doi:10.1016/j.rec.2018.06.035
7. Kennard AL, Rainsford S, Glasgow NJ, et al. Use of frailty assessment instruments in nephrology populations: a scoping review. BMC Geriatr. 2023;23(1):449. doi:10.1186/s12877-023-04101-y
8. Ruilope LM, Ortiz A, Lucia A, et al. Prevention of cardiorenal damage: importance of albuminuria. Eur Heart J. 2023;44(13):1112–1123. doi:10.1093/eurheartj/ehac683
9. Hoogendijk EO, Afilalo J, Ensrud KE, et al. Frailty: implications for clinical practice and public health. Lancet. 2019;394(10206):1365–1375. doi:10.1016/S0140-6736(19)31786-6
10. Kimura T, et al. High-normal albuminuria is associated with subclinical atherosclerosis in male population with estimated glomerular filtration rate >/=60 mL/min/1.73 m2: a cross-sectional study. PLoS One. 2019;14(8):e0218290. doi:10.1371/journal.pone.0218290
11. Chang DR, Yeh H-C, Ting I-W, et al. The ratio and difference of urine protein-to-creatinine ratio and albumin-to-creatinine ratio facilitate risk prediction of all-cause mortality. Sci Rep. 2021;11(1):7851. doi:10.1038/s41598-021-86541-3
12. Gomez-Gomez ME, Zapico SC. Frailty, Cognitive Decline, Neurodegenerative Diseases and Nutrition Interventions. Int J Mol Sci. 2019;20(11):2842. doi:10.3390/ijms20112842
13. Yang X, Jiang Y, Li J, et al. Association between Frailty and Albuminuria among Older Chinese Inpatients. J Nutr Health Aging. 2021;25(2):197–200. doi:10.1007/s12603-020-1481-6
14. Chang CC, Hsu C-Y, Chang T-Y, et al. Association between low-grade albuminuria and frailty among community-dwelling middle-aged and older people: a cross-sectional analysis from I-Lan Longitudinal Aging Study. Sci Rep. 2016;6:39434. doi:10.1038/srep39434
15. Liu M, He P, Zhou C, et al. Association of urinary albumin: creatinine ratio with incident frailty in older populations. Clin Kidney J. 2022;15(6):1093–1099. doi:10.1093/ckj/sfac002
16. Pilotto A, Custodero C, Maggi S, et al. A multidimensional approach to frailty in older people. Ageing Res Rev. 2020;60:101047. doi:10.1016/j.arr.2020.101047
17. Lin CH, Chou C-Y, Liu C-S, et al. Association between frailty and subclinical peripheral vascular disease in a community-dwelling geriatric population: Taichung Community Health Study for Elders. Geriatr Gerontol Int. 2015;15(3):261–267. doi:10.1111/ggi.12265
18. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi:10.7326/0003-4819-150-9-200905050-00006
19. West RM. Best practice in statistics: the use of log transformation. Ann Clin Biochem. 2022;59(3):162–165. doi:10.1177/00045632211050531
20. Diez-Villanueva P, Jiménez-Méndez C, Pérez-Rivera Á, et al. Different impact of chronic kidney disease in older patients with heart failure according to frailty. Eur J Intern Med. 2025;132:90–96. doi:10.1016/j.ejim.2024.12.001
21. Inker LA, Astor BC, Fox CH, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63(5):713–735. doi:10.1053/j.ajkd.2014.01.416
22. Forman JP, Fisher NDL, Schopick EL, et al. Higher levels of albuminuria within the normal range predict incident hypertension. J Am Soc Nephrol. 2008;19(10):1983–1988. doi:10.1681/ASN.2008010038
23. Zoccali C, Mallamaci F. Albuminuria in the normal range: the lower is not the better. J Am Coll Cardiol. 2013;61(15):1634–1636. doi:10.1016/j.jacc.2013.01.049
24. Ren F, Li M, Xu H, et al. Urine albumin-to-creatinine ratio within the normal range and risk of hypertension in the general population: a meta-analysis. J Clin Hypertens (Greenwich). 2021;23(7):1284–1290. doi:10.1111/jch.14263
25. Kang M, Kwon S, Lee J, et al. Albuminuria within the Normal Range Can Predict All-Cause Mortality and Cardiovascular Mortality. Kidney360. 2022;3(1):74–82. doi:10.34067/KID.0003912021
26. Ballew SH, Chen Y, Daya NR, et al. Frailty, Kidney Function, and Polypharmacy: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Kidney Dis. 2017;69(2):228–236. doi:10.1053/j.ajkd.2016.08.034
27. Guerville F, de Souto Barreto P, Taton B, et al. Estimated Glomerular Filtration Rate Decline and Incident Frailty in Older Adults. Clin J Am Soc Nephrol. 2019;14(11):1597–1604. doi:10.2215/CJN.03750319
28. Liu CK, Lyass A, Massaro JM, et al. Chronic kidney disease defined by cystatin C predicts mobility disability and changes in gait speed: the Framingham Offspring Study. J Gerontol a Biol Sci Med Sci. 2014;69(3):301–307. doi:10.1093/gerona/glt096
29. Kim JY, Park JT, Kim HW, et al. Inflammation Alters Relationship Between High-Density Lipoprotein Cholesterol and Cardiovascular Risk in Patients With Chronic Kidney Disease: results From KNOW-CKD. J Am Heart Assoc. 2021;10(16):e021731. doi:10.1161/JAHA.120.021731
30. Shokri-Mashhadi N, Moradi S, Heidari Z, et al. Association of circulating C-reactive protein and high-sensitivity C-reactive protein with components of sarcopenia: a systematic review and meta-analysis of observational studies. Exp Gerontol. 2021;150:111330. doi:10.1016/j.exger.2021.111330
31. Li Y, Zhong X, Cheng G, et al. Hs-CRP and all-cause, cardiovascular, and cancer mortality risk: a meta-analysis. Atherosclerosis. 2017;259:75–82. doi:10.1016/j.atherosclerosis.2017.02.003
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



