Back to Journals » Journal of Inflammation Research » Volume 17
Association of the Systemic Inflammation Response Index with Functional Outcome in Acute Large Vessel Occlusion Stroke Patients Receiving Mechanical Thrombectomy
Authors Wu W , Zhang YP, Qu XG, Zhang ZH
Received 24 September 2024
Accepted for publication 6 December 2024
Published 14 December 2024 Volume 2024:17 Pages 11057—11072
DOI https://doi.org/10.2147/JIR.S497754
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tara Strutt
Wen Wu,1,2 Yu-Pei Zhang,1,2 Xing-Guang Qu,1,2 Zhao-Hui Zhang1,2
1Departments of Critical Care Medicine, Yichang Central People’s Hospital, Yichang, Hubei, 443003, People’s Republic of China; 2The First College of Clinical Medical Science, China Three Gorges University, Yichang, Hubei, 443003, People’s Republic of China
Correspondence: Zhao-Hui Zhang, Department of Critical Care Medicine, Yichang Central People’s Hospital, Yichang, Hubei, 443003, People’s Republic of China, Tel/Fax +86 0717 6481546, Email [email protected]
Purpose: The systemic inflammation response index (SIRI) has recently emerged as a novel inflammatory and prognostic marker across various diseases. However, there is limited research examining the relationship between SIRI and 90-day functional outcome in patients with acute large vessel occlusion stroke (ALVOS) undergoing mechanical thrombectomy (MT). This study aimed to investigate the potential of SIRI as an innovative, inflammation-based predictor of 90-day functional outcome.
Methods: This retrospective cohort study consecutively recruited 604 Chinese patients with diagnosed ALVOS who underwent MT at the First College of Clinical Medical Science of China Three Gorges University between July 2017 and April 2023. Comprehensive data, including baseline demographic and clinical characteristics, were systematically extracted from electronic medical records. Poor functional outcome at 90 days was defined as modified Rankin Scale (mRS) score ≥ 3. We employed logistic regression models, curve fitting, sensitivity analyses, subgroup analyses, and receiver operating characteristic (ROC) curves to validate the association between SIRI and poor outcome, as well as to assess the predictive efficacy.
Results: Final analysis included 604 ALVOS subjects of whom 54.3% experienced poor functional outcome at 90 days. In the multivariate analysis, after adjusting for potential confounders, SIRI remained significantly associated with an elevated risk of poor outcomes (OR 1.18, 95% CI 1.08– 1.28, P < 0.001). Nonlinear curve fitting revealed a reverse J-shaped association between SIRI and poor outcomes, with inflection points at 4.5. Subgroup analyses showed no significant interactions (all P for interaction > 0.05), However, atrial fibrillation demonstrated a significant interaction (all P for interaction = 0.001).
Conclusion: SIRI shows promise as a novel prognostic marker for 90-day functional outcome in patients with ALVOS undergoing MT. The identified nonlinear relationship and inflection point may provide valuable insights for risk stratification and clinical decision-making in this specific patient population.
Keywords: systemic inflammation response index (SIRI), acute large vessel occlusion stroke (ALVOS), functional outcome, mechanical thrombectomy (MT)
Introduction
Ischemic stroke, accounting for approximately 70% of all stroke cases, remains a leading cause of disability and mortality worldwide.1 The standard treatment for acute ischemic stroke (AIS) patients with large vessel occlusion (LVO) has evolved to include endovascular thrombectomy (EVT), often preceded by intravenous thrombolysis (IVT) with recombinant tissue plasminogen activator (rt-PA).1,2 Despite advancements in treatment modalities, studies indicate that nearly half of these patients experience futile recanalization, a frequent occurrence following mechanical thrombectomy (MT).3–6
Futile recanalization is defined as poor functional independence (modified Rankin scale score of >2 at 3 months) or treatment failure despite successful angiographic recanalization after endovascular intervention.3,7 The etiology of this phenomenon is multifactorial, potentially involving blood-brain barrier dysfunction, capillary damage, impaired cerebral autoregulation, inadequate collateral circulation, and the development of secondary brain injuries such as cerebral edema, subacute re-occlusion, infarct expansion, and hemorrhagic transformation.4,8 However, the precise mechanisms underlying these complications remain incompletely elucidated.
Accumulating evidence suggests that immune and inflammatory responses play pivotal roles in stroke pathobiology. Inflammatory signaling is involved throughout the ischemic cascade, from early damaging events triggered by arterial occlusion to late regenerative processes underlying post-ischemic remodeling and tissue repair.5 The immune system contributes to ischemia-induced brain damage, while the damaged brain, in turn, exerts an immunosuppressive effect that promotes potentially fatal infections, thereby threatening post-stroke survival.6
Recent investigations have identified novel biomarkers for predicting stroke severity and poor prognosis in both ischemic and hemorrhagic stroke, including the neutrophil-to-lymphocyte ratio (NLR)9,10 and the monocyte-to-lymphocyte ratio (MLR).11,12 The systemic inflammatory response index (SIRI), which incorporates both NLR and MLR using neutrophil, monocyte, and lymphocyte counts, has emerged as a readily available and cost-effective measure of inflammatory status and immune pathway activity. While SIRI has been extensively studied as a prognostic indicator in oncology, evidence regarding its relationship with functional outcome in stroke patients is limited. Recent studies have explored SIRI in various stroke subtypes, including aneurysmal subarachnoid hemorrhage,13,14 intracerebral hemorrhage,15 and ischemic stroke16,17 with recanalization therapy.18
However, the prognostic value of SIRI in acute large vessel occlusion stroke (ALVOS) patients undergoing successful mechanical thrombectomy remains understudied, particularly in Chinese populations. We hypothesized that SIRI could serve as a reliable predictor of functional outcome in these patients. This study aimed to investigate the association between admission SIRI and functional outcome in Chinese ALVOS patients following successful MT recanalization.
Materials and Methods
Study Design
In this observational, retrospective study, we recruited stroke patients consecutively treated with mechanical thrombectomy at the Comprehensive Stroke Center (CSC) in Yichang Central People’s Hospital, between July 2017 and April 2023. The study protocol was reviewed and approved by the Hospital of Medicine Ethics Committee (ethical approval number: 2023–129-01) and conducted in accordance with the Declaration of Helsinki.
Inclusion and Exclusion Criteria
This retrospective analysis utilized data from a prospectively maintained database at our CSC, encompassing patients admitted between July 2017 and April 2023. We included consecutive patients who presented with acute neurological deficits and were diagnosed with acute ischemic stroke (AIS) using a “one-stop-shop” multimodal CT examination within 24 hours of symptom onset.
The inclusion criteria were as follows: (1) Acute intracranial large vessel occlusion (ALVO) confirmed by computed tomographic angiography (CTA), magnetic resonance angiography (MRA), or digital subtraction angiography within 24 hours of symptom onset; (2) Treatment with acute recanalization therapy, either EVT alone or in combination with IVT; (3) Achievement of complete or near-complete recanalization following reperfusion therapy.
Exclusion criteria: (1) without obvious LVO at baseline CTA; (2) Severe hepatic or renal disease; (3) Active malignancy, hematologic disorders, or immunosuppressed status; (4) Presence of infectious disease at admission; (5) Incomplete admission laboratory data; (6) Pre-stroke modified Rankin scale (mRS) score ≥ 2 and (7) Loss to follow-up at 90 days post-intervention. Figure 1 illustrates the patient selection process and study flow diagram.
EVT consisted of mechanical thrombectomy with aspiration catheters alone, stent-retrievers alone, or both, depending on occlusion type/location and neuro-interventionist’s choice. Revascularization was assessed by applying the modified thrombolysis in cerebral infarction (mTICI) classification.19 Successful recanalization was defined as grade 2b, 2c, or 3 of reperfusion. According to the 2018/2019 American Guidelines for Early Management of AIS,20 patients were treated using IVT or/and MT or stent implantation, while patients with thrombolysis contraindication or unsuitable for EVT were treated using general supportive treatment.
Baseline Characteristics and Data Collection
We extracted baseline demographic, clinical characteristics and pre-admission treatments, from our prospectively maintained stroke registry database. The following data were collected: (1) Demographics (age and sex); (2) Medical history of current stroke risk factors (smoking status, hypertension, diabetes mellitus, hyperlipidemia, atrial fibrillation, coronary artery disease; (3) Clinical and Imaging Parameters (Time from last known well (TFLKW) to CT examination, baseline the National Institutes of Health Stroke Scale (NIHSS) score on admission,21 Pre-stroke modified Rankin Scale (mRS) score and Alberta Stroke Program Early CT Score (ASPECTS) to determine the extent of initial core infarct on pre-therapeutic CT.22 (4) Laboratory Parameters (hemoglobin, white blood cell count, neutrophil count, monocyte count, platelet count, lymphocyte count, serum creatinine and blood pressure). All blood samples were collected upon arrival at neurocritical care unit after thrombectomy. Laboratory tests were performed using standardized methods in our hospital’s central laboratory. The inflammatory indices were calculated as follows: NLR = neutrophil count / Absolute lymphocyte count; MLR = monocyte count / lymphocyte count; PLR = platelet count / lymphocyte count; Systemic Immune Inflammation Index (SII) = NLR × platelet count; System Inflammation Response Index (SIRI) = (Neutrophil count × Monocyte count) / Lymphocyte count.
Outcome Parameters
The primary outcome was neurological functional status at 90 days post-intervention, assessed using the modified Rankin Scale (mRS). Functional independence was evaluated through either telemedicine consultation or in-person assessment at our CSC. All assessments were conducted by trained neurologists who were blinded to the patients’ SIRI values and other clinical data not essential for mRS scoring. Outcomes were categorized as follows: Poor functional outcome: mRS score ≥ 3; good functional outcome: mRS score 0–2.
The secondary outcome was the occurrence of early neurological deterioration (END),23,24 within the first week of admission. END was defined as any new neurologic symptoms/signs or neurologic worsening meeting one or more of the following criteria: (1) an increase of ≥2 points in total NIHSS score, (2) an increase of ≥1 point in the motor NIHSS score, and/or (3) an increase of ≥1 point in the consciousness score.25,26
Statistical Analysis
The continuous variables were presented as mean ± standard deviation (SD) for normally distributed data or median with interquartile range (IQR) for non-normally distributed data. Categorical variables were summarized as frequencies and percentages. Shapiro–Wilk and Kolmogorov–Smirnov tests were used to assess normality of continuous variables. Levene’s test was employed to evaluate variance homogeneity. The Chi-square test (categorical variables), the one-way ANOVA (normal distributed variables), or the Kruskal–Wallis H-test (skewed distributed variables) was used to test the differences between SIRI groups. The relationship between SIRI and poor functional outcome was examined using univariate and multivariable logistic regression analyses. Results are reported as odds ratios (OR) with 95% confidence intervals (CI).
Four progressive models were employed: Non-adjusted Model, without adjust any variables. Model 1 was adjusted for age, sex; Model 2 was adjusted for model 1 plus smoking status, hypertension, diabetes mellitus, coronary artery disease, hyperlipemia, atrial fibrillation, temperature, systolic BP and diastolic BP on admission; Model 3 was adjusted for variables in model 2 as well as time from last known well to reperfusion, baseline NIHSS score, ASPECTS, AIS location, Stroke subtypes, TOAST classification, CRP, albumin and recanalization therapy.
In addition, Smooth curve fitting, adjusted for Model 3 covariates, was used to visualize the relationship between SIRI and poor outcome. A two-piecewise binary logistic regression model further explored observed nonlinearity.
Furthermore, to identify modifications and interactions, we used a stratified linear regression model and likelihood ratio test (LRT) in subgroups of age (<65 and ≥65 years), sex (female and male), diabetes, atrial fibrillation, acute ischemic stroke location (anterior and posterior circulation), stroke subtypes (non−cardioembolic and cardioembolic), recanalization therapy (MT alone and MT combined with IVT), CRP (<5 mg/L and ≥5 mg/L), and NIHSS (<16 score and ≥16 score). Multiple imputation was used to handle missing data.27
All the analyses were performed with the statistical software packages R (http://www.R-project.org, The R Foundation) and Free Statistics software versions 1.9. A two-tailed test was performed and P < 0.05 was considered statistically significant.
Results
Baseline Clinical Characteristics
A total of 604 patients with MT for ALVOS achieved successful recanalization were enrolled in this study. Among them, 328 patients (54.3%) experienced poor functional outcome, defined as mRS ≥ 3 at 3 months. Baseline characteristics based on functional outcome are summarized in Table 1. There were no statistically significant differences between the good and poor outcome groups regarding in age, sex, current smoking status, history of hypertension, diabetes mellitus, atrial fibrillation, admission temperature, systolic BP, diastolic BP, CRP, albumin, ASPECTS, AIS location, stroke subtypes, time from last known well to reperfusion, or white blood cells (all P > 0.05). Conversely, significant differences were observed between the groups in terms of coronary artery disease, hyperlipemia, baseline NIHSS, location of intracranial vessel occlusion, recanalization therapy, lymphocytes, neutrophils, monocytes, NLR, MLR, PLR, SII, as well as SIRI (P < 0.05). Baseline demographic characteristics and clinical data of the included patients according to SIRI tertiles are presented in Table 2. Patients in the highest SIRI tertile (T3) exhibited higher baseline NIHSS, elevated white blood cells, neutrophils, and monocytes, increased NLR, PLR, SII, and a greater prevalence of early neurological deterioration (END) and posterior circulation stroke compared to lower tertiles. Conversely, they had lower lymphocyte counts, ASPECTS scores, and a lower proportion of combined intravenous thrombolysis and mechanical thrombectomy (IVT + MT) for recanalization therapy. No significant differences were found among SIRI tertiles for age, sex, current smoking status, history of hypertension, diabetes mellitus, history of stroke, coronary artery disease, hyperlipemia, atrial fibrillation, admission temperature, systolic BP, diastolic BP, CRP, albumin, and time from last known well to reperfusion (all P > 0.05).
 |
Table 1 Baseline Characteristics and Comparison of Clinical Variables Stratified by Functional Outcome |
 |
Table 2 Baseline Characteristics and Comparison of Clinical Variables Stratified by the SIRI Tertile |
Univariate and Multivariate Logistic Regression Analyses of SIRI and Poor Functional Outcome
According to univariate analysis, baseline NIHSS score, monocytes, END, history of coronary artery disease, diabetes mellitus, hyperlipemia, lymphocytes, non-cardioembolic stroke, and elevated SIRI were correlated with poor outcome (P < 0.1; details in Table S1).
We constructed multivariate logistic regression analysis with models to evaluate the independent effects of SIRI on the presence of 90-day poor functional outcome (Table 3). When SIRI was evaluated as a continuous variable, in the full variables adjusted model (model 3), the adjusted OR was 1.18 (95% CI: 1.08–1.28) for 90-day poor outcome. When SIRI was analyzed as tertiles, also in model 3, the adjusted OR for 90-day poor functional outcome in T2 and T3 were 2.35 (95% CI: 1.49–3.70, P < 0.001) and 2.58 (95% CI: 1.59–4.2, P < 0.001), respectively, with T1 as reference. Moreover, it was statistically significant in all models (P for trend < 0.001), indicating that the risk of 90-day poor outcome increased stepwise across SIRI tertiles.
 |
Table 3 Multivariate Logistic Regression Analyses of SIRI on the Risk of Poor Outcome |
The Nonlinear Relationship Between SIRI and Poor Functional Outcome
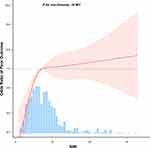
Figure 2 demonstrates a reverse J-shaped curve (P for non-linearity < 0.01) in restricted cubic spline model.
In the threshold analysis, the data were fitted to a piecewise multiple logistic regression model with two different slopes (Table 4). There was dose-responsive relationship between increasing SIRI levels and elevated adjusted odds ratios for 90-day poor outcomes in patients with SIRI < 4.5. While, there was no association between SIRI and 90-day poor outcome when SIRI was ≥ 4.5. This means that the risk of poor outcomes no longer elevates with increasing SIRI.
 |
Table 4 Threshold Effect Analyses of SIRI on the Risk of Poor Outcome Using Two-Piecewise Regression Models |
ROC Curves for Comparison of Biomarkers to Predict Poor Outcome
From Figure 3, we compared the predictive value of various inflammation-related indicators for poor outcome in patients with ALVOS. Among these, the area under the ROC curve (AUC) for the SIRI was 68.20% (95% CI: 63.91–72.49%), which was higher than NLR, MLR, PLR, and SII, but lower than the NIHSS score. The details were seen in Table S2.
Subgroup Analysis
Subgroup analyses explored possible associations of the SIRI (treated as a continuous variable) with 90-day poor outcome among different stratification variables (Figure 4).
The associations between the SIRI (treated as a continuous variable) with 90-day unfavorable outcome were similar among the following subgroups: age (<65 years vs ≥65 years), sex, diabetes mellitus, atrial fibrillation, hyperlipemia, AIS location (anterior vs posterior circulation), time from last known well to reperfusion (≤6h vs >6h), stroke subtypes (Cardioembolic vs Non-cardioembolic), NIHSS (<16 vs ≥16), CRP (<5 mg/L vs ≥5 mg/L) and recanalization therapy (MT alone vs MT with IVT) (all P interaction > 0.05). Noticeably, the SIRI interacted significantly with atrial fibrillation (OR 1.43, 95% CI 1.18–1.74 for subjects without atrial fibrillation vs OR 1.11, 95% CI 1.01–1.21 for subjects with atrial fibrillation, P interaction = 0.001).
Discussion
In this study, we examined 604 patients with acute large vessel occlusion stroke (ALVOS) who underwent mechanical thrombectomy in China to investigate the association between the SIRI and poor functional outcome at 90 days post-intervention. Our findings indicate that SIRI is an independent risk factor for poor 90-day functional outcome in MT patients, exhibiting a dose-response relationship with adverse outcomes. Furthermore, our analysis revealed that SIRI outperformed other inflammatory and clinical markers, including SII, NLR, MLR, PLR, and WBC in predicting functional outcome. Consequently, SIRI emerges as a viable non-invasive predictive tool for assessing the risk of unfavorable 90-day functional outcome in the Chinese population undergoing endovascular thrombectomy for ALVOS.
While various pathophysiological mechanisms contribute to post-stroke injury at the site of cerebral ischemia, mounting evidence indicates that inflammatory responses are closely associated with injury repair, regeneration, systemic inflammation, immunosuppression, and patient functional prognosis.6,28,29 Inflammation contributes to progress of acute ischemia stroke, and leukocytes, with different leukocyte subsets playing distinct roles in the inflammatory reaction.9–11,30 Neutrophils activate inflammatory reaction and induce brain damage by releasing inflammatory mediators and induce damage to the blood-brain barrier,31 whereas monocytes Contribute to inflammatory and prothrombotic pathways by interacting with platelets and endothelial cells. They also differentiate into brain-resident macrophages as part of the initial inflammatory cascade.11,12,32 In contrast, lymphocytes have a downregulation effect on inflammation.9,10,12,33 Various subsets of lymphocytes and specific T-cell lymphocytes secrete anti-inflammatory factors, regulate the activation of glial cells, and reduce the body’s immune response to cerebral ischemia. In addition, lymphocytes play an important role in anti-inflammatory response functions and confer endothelial protection.34
The systemic inflammation response index (SIRI) was described as a novel inflammatory marker by Qi et al.35 SIRI, which combines neutrophil, monocyte, and lymphocyte count, has been established as a prognostic indicator in patients with malignancies.35–37 Given the complex interplay of immune-inflammatory processes in stroke, utilizing indices or ratios that incorporate multiple cellular lines may provide a more reliable reflection of the balance between innate and adaptive immunity, compared to single blood parameters alone. It offers a comprehensive evaluation of inflammation, immunity, hemostasis, and thrombosis. Our study showed that SIRI has the ability to effectively predict 90-day functional outcome with an AUC of 0.682 (0.639–0.725), and the optimal cut-off point of SIRI for predicting 90-day functional outcome was 3.31, with a sensitivity of 69.51% and a specificity of 62.68%. Moreover, SIRI showed superior prognostic predictivity compared to NLR, LMR, PLR, and SII.
These findings suggest that SIRI could be a valuable addition to existing clinical predictors such as age, baseline stroke severity, and success of brain reperfusion in patients undergoing mechanical thrombectomy for acute large vessel occlusion stroke.38,39 Recent studies have confirmed that SIRI is linked to poor functional outcomes, post-stroke pneumonia, and the incidence of sICH in patients undergoing thrombectomy.40–44
Our study consistently demonstrated that patients with poor prognoses had higher neutrophil and monocyte counts and lower lymphocyte counts than those with favorable prognoses.16,17,42
In addition, our study found a non-linear relationship between SIRI and 90-day functional outcome. Moreover, subgroup analysis revealed that the predictive value of SIRI for unfavorable functional outcome was prominent in patients with atrial fibrillation (OR 1.69, 95% CI: 1.41–2.03) compared to those without atrial fibrillation (OR 1.14, 95% CI: 1.06–1.24), indicating that this atrial fibrillation subgroup may be more vulnerable to poor functional outcome. It is possible to believe that atrial fibrillation could increase the risk of acute heart failure, pulmonary infections, and recurrent thromboembolic events, potentially worsening overall outcomes. Notably, patients admitted to our hospital showed low compliance with standard anticoagulation therapy before admission, which is essential for long-term outcomes and reducing stroke mortality.45
While the exact biological mechanisms underlying the association between the SIRI and adverse functional outcome are not fully elucidated, several rational pathways have been proposed based on current evidence. Following cerebral infarction, the activating of microglia, macrophages, and mast cells leads to the release of pro-inflammatory cytokines. This inflammatory cascade triggers the sympathetic nervous system and the hypothalamic-pituitary-adrenal (HPA) axis, resulting in increased secretion of stress hormones, which ultimately contribute to neutrophil leucocytosis and lymphopenia.46 Lymphocytes depletion may compromise pathogen resistance and heighten susceptibility to infections, which are common complications after cerebral infarction can adversely affect the clinical trajectory.47 Moreover, specific regulatory lymphocyte subpopulations are essential for maintaining immune homeostasis and offer neuroprotective effects by modulating the immune response. These cells counteract pro-inflammatory mediator production, regulate microglial activation, suppress autoreactive cellular responses, and promote neurogenesis and tissue repair processes within the ischemic region.48,49
In summary, our analysis indicates that the SIRI provides a comprehensive evaluation of an individual’s inflammatory and immune status and holds promise as a prognostic biomarker for functional outcome in patients with ALVOS undergoing mechanical thrombectomy. Furthermore, incorporating the SIRI into routine clinical practice may enhance risk stratification and improve predictions related to clinical outcomes.
However, our study also had several limitations. Frist of all, the retrospective nature of this investigation precludes the establishment of definitive causal relationships. Although we employed multivariate adjustments and subgroup analyses to mitigate confounding factors, the potential influence of residual confounders on clinical outcomes cannot be entirely excluded. Secondly, this study exclusively analyzed baseline SIRI values. Future research should evaluate the dynamic changes in SIRI over time to better understand its predictive power and potential fluctuations during the clinical course. Consequently, further studies with larger sample sizes and prospective designs are essential to validate these findings.
Conclusion
This study revealed that SIRI, an affordable and readily available biomarker, exhibits an independent association with an elevated risk of poor functional outcome in a cohort of Chinese patients due to ALVOS with endovascular reperfusion. However, the intricate mechanisms underlying inflammation in AIS remain incompletely elucidated, necessitating further exploration of the complex interplay between inflammatory markers and clinical outcomes.
Data Sharing Statement
Data is available from the corresponding author on reasonable request.
Ethical Statement
The current retrospective study was approved by the Ethics Committee of the First College of Clinical Medical Science of China Three Gorges University (ethical approval number: 2023-129-01), which waived consent from study participants as it was not required due to the retrospective nature of the study. All patient data was anonymized during processing. This study was performed following the Declaration of Helsinki.
Acknowledgments
We extend our gratitude to Dr. Liu Jie from the People’s Liberation Army of China General Hospital, Beijing, China, for their invaluable assistance in the revision of this manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
All authors have declared that they have no conflicts of interest in this work.
References
1. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723–1731. doi:10.1016/S0140-6736(16)00163-X
2. Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3). doi:10.1161/STR.0000000000000158
3. Hussein HM, Georgiadis AL, Vazquez G, et al. Occurrence and predictors of futile recanalization following endovascular treatment among patients with acute ischemic stroke: a multicenter study. Am J Neuroradiol. 2010;31(3):454–458. doi:10.3174/ajnr.A2006
4. Shi K, Tian D-C, Li Z-G, et al. Global brain inflammation in stroke. Lancet Neurol. 2019;18(11):1058–1066. doi:10.1016/S1474-4422(19)30078-X
5. Macrez R, Ali C, Toutirais O, et al. Stroke and the immune system: from pathophysiology to new therapeutic strategies. Lancet Neurol. 2011;10(5):471–480. doi:10.1016/S1474-4422(11)70066-7
6. Lattanzi S, Di Napoli M, Ricci S, Divani AA. Matrix metalloproteinases in acute intracerebral hemorrhage. Neurotherapeutics. 2020;17(2):484–496. doi:10.1007/s13311-020-00839-0
7. Shahid AH, Abbasi M, Larco JLA, et al. Risk factors of futile recanalization following endovascular treatment in patients with large‐vessel occlusion: systematic review and meta‐analysis. SVIN. 2022;2(6):e000257. doi:10.1161/SVIN.121.000257
8. Mizuma A, You JS, Yenari MA. Targeting reperfusion injury in the age of mechanical thrombectomy. Stroke. 2018;49(7):1796–1802. doi:10.1161/STROKEAHA.117.017286
9. Gong P, Liu Y, Gong Y, et al. The association of neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, and lymphocyte to monocyte ratio with post-thrombolysis early neurological outcomes in patients with acute ischemic stroke. J Neuroinflammation. 2021;18(1):51. doi:10.1186/s12974-021-02090-6
10. Brooks SD, Spears C, Cummings C, et al. Admission neutrophil–lymphocyte ratio predicts 90 day outcome after endovascular stroke therapy. J NeuroIntervent Surg. 2014;6(8):578–583. doi:10.1136/neurintsurg-2013-010780
11. Juega J, Palacio-Garcia C, Rodriguez M, et al. Monocyte-to-lymphocyte ratio in clot analysis as a marker of cardioembolic stroke etiology. Transl Stroke Res. 2022;13(6):949–958. doi:10.1007/s12975-021-00946-w
12. Lux D, Alakbarzade V, Bridge L, et al. The association of neutrophil-lymphocyte ratio and lymphocyte-monocyte ratio with 3-month clinical outcome after mechanical thrombectomy following stroke. J Neuroinflammation. 2020;17(1):60. doi:10.1186/s12974-020-01739-y
13. Feghali J, Kim J, Gami A, et al. Monocyte-based inflammatory indices predict outcomes following aneurysmal subarachnoid hemorrhage. Neurosurg Rev. 2021;44(6):3499–3507. doi:10.1007/s10143-021-01525-1
14. Yun S, Yi HJ, Lee DH, Sung JH. Systemic inflammation response index and systemic immune-inflammation index for predicting the prognosis of patients with aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2021;30(8):105861. doi:10.1016/j.jstrokecerebrovasdis.2021.105861
15. Yu T, Liu H, Liu Y, Jiang J. Inflammatory response biomarkers nomogram for predicting pneumonia in patients with spontaneous intracerebral hemorrhage. Front Neurol. 2023;13:1084616. doi:10.3389/fneur.2022.1084616
16. Zhang Y, Xing Z, Zhou K, Jiang S. The predictive role of Systemic Inflammation Response Index (SIRI) in the prognosis of stroke patients. CIA. 2021;16:1997–2007. doi:10.2147/CIA.S339221
17. Dang H, Mao W, Wang S, et al. Systemic inflammation response index as a prognostic predictor in patients with acute ischemic stroke: a propensity score matching analysis. Front Neurol. 2023;13:1049241. doi:10.3389/fneur.2022.1049241
18. Chen Y-F, Qi S, Yu Z-J, et al. Systemic inflammation response index predicts clinical outcomes in patients with Acute Ischemic Stroke (AIS) after the treatment of intravenous thrombolysis. The Neurologist. 2023;28(6):355–361. doi:10.1097/NRL.0000000000000492
19. Dargazanli C, Fahed R, Blanc R, et al. Modified thrombolysis in cerebral infarction 2C/Thrombolysis in cerebral infarction 3 reperfusion should be the aim of mechanical thrombectomy: insights from the ASTER trial (contact aspiration versus stent retriever for successful revascularization). Stroke. 2018;49(5):1189–1196. doi:10.1161/STROKEAHA.118.020700
20. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344–418.
21. Wityk RJ, Pessin MS, Kaplan RF, Caplan LR. Serial assessment of acute stroke using the NIH stroke scale. Stroke. 1994;25(2):362–365. doi:10.1161/01.STR.25.2.362
22. Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. Lancet. 2000;355(9216):1670–1674. doi:10.1016/S0140-6736(00)02237-6
23. Seners P, Turc G, Oppenheim C, Baron J-C. Incidence, causes and predictors of neurological deterioration occurring within 24 h following acute ischaemic stroke: a systematic review with pathophysiological implications. J Neurol Neurosurg Psychiatry. 2015;86(1):87–94. doi:10.1136/jnnp-2014-308327
24. Ji X, Tian L, Yao S, et al. A systematic review of body fluids biomarkers associated with early neurological deterioration following acute ischemic stroke. Front Aging Neurosci. 2022;14:918473. doi:10.3389/fnagi.2022.918473
25. Park TH, Lee J-K, Park M-S, et al. Neurologic deterioration in patients with acute ischemic stroke or transient ischemic attack. Neurology. 2020;95(16). doi:10.1212/WNL.0000000000010603
26. Weimar C. Neurologic worsening during the acute phase of ischemic stroke. Arch Neurol. 2005;62(3):393. doi:10.1001/archneur.62.3.393
27. Zhang Z. Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann Translat Med. 2016;4.
28. Anrather J, Iadecola C. Inflammation and stroke: an overview. Neurotherapeutics. 2016;13(4):661–670. doi:10.1007/s13311-016-0483-x
29. Saand AR, Yu F, Chen J, Chou SH-Y. Systemic inflammation in hemorrhagic strokes – a novel neurological sign and therapeutic target? J Cereb Blood Flow Metab. 2019;39(6):959–988. doi:10.1177/0271678X19841443
30. Świtońska M, Piekuś-Słomka N, Słomka A, et al. Neutrophil-to-lymphocyte ratio and symptomatic hemorrhagic transformation in ischemic stroke patients undergoing revascularization. Brain Sci. 2020;10(11):771. doi:10.3390/brainsci10110771
31. Herz J, Sabellek P, Lane TE, et al. Role of neutrophils in exacerbation of brain injury after focal cerebral ischemia in hyperlipidemic mice. Stroke. 2015;46(10):2916–2925. doi:10.1161/STROKEAHA.115.010620
32. Ren H, Liu X, Wang L, Gao Y. Lymphocyte-to-monocyte ratio: a novel predictor of the prognosis of acute ischemic stroke. J Stroke Cerebrovasc Dis. 2017;26(11):2595–2602. doi:10.1016/j.jstrokecerebrovasdis.2017.06.019
33. Yang Y, Sun G, Diao S, Yang L, Dong W. Diagnostic performances of neutrophil to lymphocyte ratio and lymphocyte to monocyte ratio in acute ischemic stroke caused by cervicocranial arterial dissection. Clin Lab Analysis. 2020;34(12):e23515. doi:10.1002/jcla.23515
34. Si Y, Liu J, Shan W, et al. Association of lymphocyte-to-monocyte ratio with total coronary plaque burden in patients with coronary artery disease. Coronary Artery Dis. 2020;31(7):650–655. doi:10.1097/MCA.0000000000000857
35. Qi Q, Zhuang L, Shen Y, et al. A novel systemic inflammation response index (SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy. Cancer. 2016;122(14):2158–2167. doi:10.1002/cncr.30057
36. Topkan E, Kucuk A, Ozdemir Y, et al. Systemic inflammation response index predicts survival outcomes in glioblastoma multiforme patients treated with standard stupp protocol. J Immunol Res. 2020;2020:1–10. doi:10.1155/2020/8628540
37. Wei L, Xie H, Yan P. Prognostic value of the systemic inflammation response index in human malignancy: a meta-analysis. Medicine. 2020;99(50):e23486. doi:10.1097/MD.0000000000023486
38. Van Horn N, Kniep H, Leischner H, et al. Predictors of poor clinical outcome despite complete reperfusion in acute ischemic stroke patients. J NeuroIntervent Surg. 2021;13(1):14–18. doi:10.1136/neurintsurg-2020-015889
39. Semerano A, Laredo C, Zhao Y, et al. Leukocytes, collateral circulation, and reperfusion in ischemic stroke patients treated with mechanical thrombectomy. Stroke. 2019;50(12):3456–3464. doi:10.1161/STROKEAHA.119.026743
40. Cong Y, Xia X, Liao J, et al. Association of systemic inflammatory response index and neutrophil-to-lymphocyte ratio on unfavorable functional outcomes in acute ischemic stroke patients after endovascular therapy. World Neurosurg. 2024;190:e1071–e1080. doi:10.1016/j.wneu.2024.08.065
41. Yi HJ, Sung JH, Lee DH, et al. Systemic inflammation response index and systemic immune-inflammation index are associated with clinical outcomes in patients treated with mechanical thrombectomy for large artery occlusion. World Neurosurg. 2021;153:e282–e289. doi:10.1016/j.wneu.2021.06.113
42. Lattanzi S, Norata D, Divani AA, et al. Systemic inflammatory response index and futile recanalization in patients with ischemic stroke undergoing endovascular treatment. Brain Sci. 2021;11(9):1164. doi:10.3390/brainsci11091164
43. Cao W, Song Y, Bai X, et al. Systemic-inflammatory indices and clinical outcomes in patients with anterior circulation acute ischemic stroke undergoing successful endovascular thrombectomy. Heliyon. 2024;10(10):e31122. doi:10.1016/j.heliyon.2024.e31122
44. Zheng F, Gao W, Xiao Y, et al. Systemic inflammatory response index as a predictor of stroke-associated pneumonia in patients with acute ischemic stroke treated by thrombectomy: a retrospective study. BMC Neurol. 2024;24(1):287. doi:10.1186/s12883-024-03783-0
45. Halcox JPJ, Wareham K, Cardew A, et al. Assessment of remote heart rhythm sampling using the alivecor heart monitor to screen for atrial fibrillation: the REHEARSE-AF study. Circulation. 2017;136(19):1784–1794. doi:10.1161/CIRCULATIONAHA.117.030583
46. Schulze J, Vogelgesang A, Dressel A. Catecholamines, steroids and immune alterations in ischemic stroke and other acute diseases. Aging Dis. 2014;5(5):327–339. doi:10.14336/AD.2014.0500327
47. Vogelgesang A, Grunwald U, Langner S, et al. Analysis of lymphocyte subsets in patients with stroke and their influence on infection after stroke. Stroke. 2008;39(1):237–241. doi:10.1161/STROKEAHA.107.493635
48. Brait VH, Arumugam TV, Drummond GR, Sobey CG. Importance of T lymphocytes in brain injury, immunodeficiency, and recovery after cerebral ischemia. J Cereb Blood Flow Metab. 2012;32(4):598–611. doi:10.1038/jcbfm.2012.6
49. Li P, Mao L, Liu X, et al. Essential role of program death 1-Ligand 1 in regulatory T-Cell–afforded protection against blood–brain barrier damage after stroke. Stroke. 2014;45(3):857–864. doi:10.1161/STROKEAHA.113.004100
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.