Back to Journals » Clinical Ophthalmology » Volume 19
Clinical Outcomes of an Enhanced and Conventional Monofocal IOL in Patients with Early and Intermediate Dry Age-Related Macular Degeneration
Authors Venter JA , Berry CW, Hannan NC, Raju D, Kiss HJ, Belovari M , Hannan SJ , Cooper DR, Schallhorn JM
Received 12 December 2024
Accepted for publication 4 March 2025
Published 4 April 2025 Volume 2025:19 Pages 1203—1214
DOI https://doi.org/10.2147/OPTH.S511743
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Jan A Venter,1 Colin W Berry,1 Noelle C Hannan,1 Dasi Raju,1 Huba J Kiss,1 Mirna Belovari,1 Stephen J Hannan,1 David R Cooper,1 Julie M Schallhorn2,3
1Optical Express, Glasgow, UK; 2Department of Ophthalmology, University of California, San Francisco, CA, USA; 3F.I. Proctor Foundation, University of California, San Francisco, CA, USA
Correspondence: Jan A Venter, Optical Express, 200 St Vincent St, Glasgow, G2 5SG, UK, Email [email protected]
Purpose: To compare the performance of an enhanced and conventional monofocal IOL in eyes with early and intermediate age-related macular degeneration (AMD).
Methods: This retrospective study compared one-month postoperative outcomes of patients bilaterally implanted with TECNIS Eyhance IOL (ICB00 group) or TECNIS Monofocal IOL (ZCB00 group). All patients underwent cataract surgery with pre-existing early or intermediate dry AMD. Outcome measures were monocular and binocular uncorrected distance (UDVA), intermediate (UIVA) and near (UNVA) visual acuity, monocular corrected distance visual acuity (CDVA), and refractive outcomes. Monocular visual acuities and refractive predictability were calculated for the dominant eye of each patient.
Results: The ICB00 group comprised 143 eyes of 143 patients, while 164 eyes of 164 patients were included in the ZCB00 group. Preoperative characteristics were comparable between the two groups. There was no significant difference in postoperative refractive predictability, with 87.4% and 89.6% of eyes within 0.50 D of emmetropia in the ICB00 and ZCB00 groups, respectively (p=0.54). No difference was found in postoperative UDVA or CDVA between the groups. Both monocular and binocular UIVA were significantly better in the ICB00 group (monocular UIVA: 0.32± 0.19 vs 0.42± 0.22 logMAR, p< 0.001; binocular UIVA: 0.25± 0.18 vs 0.36± 0.17 logMAR, p< 0.001). Postoperative UNVA was also better with the ICB00 IOL (monocular UNVA: 0.58± 0.16 vs 0.69± 0.20 logMAR, p< 0.001; binocular UNVA: 0.50± 0.16 vs 0.63± 0.17 logMAR, p< 0.001).
Conclusion: ICB00 IOL enhanced intermediate and near vision in patients with AMD while achieving the same level of corrected and uncorrected distance visual acuity.
Keywords: enhanced monofocal IOL, age-related macular degeneration, intermediate vision
Introduction
Multifocal IOLs are generally not recommended in patients with pre-existing ocular comorbidities.1,2 Even though they can provide good short-term outcomes in patients with mild comorbidities, the likelihood of the progression of the disease, the combined effect of the loss of contrast sensitivity from the disease and the multifocal IOL design can lead to reduced visual function, higher dissatisfaction rates, or even a possibility of IOL explant.1–3
While monofocal IOLs are the better long-term options in patients with ocular co-pathology, studies have been exploring possibilities of improving visual function and reducing spectacle dependence in this group of patients without jeopardizing the quality of vision.4–11 A new group of monofocal IOLs has emerged in recent years aiming to slightly extend the depth of focus and enhance intermediate vision, defined as “enhanced monofocal” IOLs.12 Of these, the lens with the highest volume of peer-reviewed literature is the TECNIS Eyhance ICB00 IOL (Johnson & Johnson Vision, Inc., Irvine, CA).13,14 This IOL features a refractive surface design that is progressive in power from the periphery to the center of the lens, aiming to slightly extend the depth of focus. In our previous study comparing it to its parent IOL (TECNIS Monofocal ZCB00 IOL, Johnson & Johnson Vision, Inc, Irvine, CA), we found approximately one Snellen line better intermediate and near vision with the ICB00 model, while the distance visual acuity and optical side effects were comparable between the two IOLs.15
Operating on patients with AMD requires special considerations. Care should be taken during the counseling process to explain the long-term effect of AMD on vision, contrast sensitivity, color perception, and central vision.16 Moreover, retinal changes can interfere with biometric measurement, mainly axial length.17 This might result in less predictable outcomes, even though it is usually not an issue in eyes with the early stage of the disease. The chosen intraocular lens should maximize vision in the coming years and provide long-term quality of vision and optical clarity.16 A few smaller studies considered the options of implanting an enhanced monofocal IOL in patients with pre-existing ocular comorbidities with encouraging outcomes.4–11 The aim of the current study was to compare the real-world refractive and visual outcomes of patients implanted with an enhanced and standard monofocal IOL in the presence of dry age-related macular degeneration.
Patients and Methods
This comparative retrospective study comprised patients who underwent cataract surgery with the diagnosis of dry age-related macular degeneration (AMD) with either an enhanced monofocal IOL (ICB00) or a conventional monofocal IOL (ZCB00), both manufactured by Johnson & Johnson Vision, Inc, Irvine, CA). The study was deemed exempt from review by the Institutional Review Board at the University of California, San Francisco, because it used only retrospective, de-identified patient data. All patients provided written informed consent to undergo the cataract procedure and agreed to use their de-identified data for statistical analysis and research purposes. The study adhered to the tenets of the Declaration of Helsinki.
All consecutive patients treated between September 2021 and August 2024 who met the following criteria were extracted from the electronic medical record of Optical Express, Glasgow, United Kingdom: bilateral cataracts requiring IOL surgery with the concurrent diagnosis of an early or intermediate AMD in each eye according to a previously published classification,18 bilateral implantation of either ICB00 or ZCB00 IOL, and attended one-month postoperative visit. Patients with advanced age-related macular degeneration (geographic atrophy or neovascular age-related macular degeneration) were not included in this study.
The patients underwent a preoperative ophthalmic examination, including visual acuity measurement, ocular dominance testing, anterior eye slit-lamp examination, and dilated fundus examination. Diagnostic scans included autorefraction and tonometry (Tonoref II, Nidek Co. Ltd., Gamagory, Japan), corneal tomography (Pentacam, Oculus Optikgeräte GmbH, Wetzlar, Germany), endothelial cell count (SP 2000P specular microscope, Topcon Corp, Tokyo, Japan), biometry (IOLMaster, Carl Zeiss Meditec AG, Jena, Germany), and retinal optical coherence tomography (Cirrus 4000/500 OCT, Carl Zeiss Meditec AG, Jena, Germany). AMD was first noted by an optometrist during the initial consultation (from dilated fundus examination as well as from the findings on the optical coherence tomography), and the diagnosis was later confirmed by the treating ophthalmologist.
Visual acuity measurements included monocular corrected distance visual acuity (CDVA), monocular and binocular uncorrected distance (UDVA), intermediate (UIVA), and near (UNVA) visual acuity. Corrected and uncorrected distance visual acuity was measured at 4 meters with a logarithmic acuity chart. Near visual acuity was measured at 40 cm with an early treatment diabetic retinopathy study (ETDRS) near vision chart normalized for a 40 cm distance. Intermediate visual acuity was tested at 66 cm using the same ETDRS chart as for UNVA, with the visual acuity adjusted for the modified viewing distance. All visual acuities were recorded in Snellen equivalents on the electronic medical record and converted to the logarithm of the minimum angle of resolution (logMAR) for statistical analysis. Patients were advised to attend one day, one week, one month, and three months postoperative visits. The one-month visit had considerably higher attendance rate compared to the three-month visit and was selected for analysis in this study.
Surgical Technique
The surgeries were performed using a standard phacoemulsification technique according to the protocol of each surgeon. The IOLs were implanted through a 2.75 mm clear corneal incision under topical anesthesia (proparacaine hydrochloride 0.5%). Although there were some variations between surgeons, most surgeons placed an incision on the steepest meridian if the corneal astigmatism was ≥0.75 D and used a temporal incision if the corneal astigmatism was ≤0.75 D. The choice of the IOL depended on the surgeon/patient preference. In patients who were considered low risk for intraoperative or postoperative complications, bilateral same-day surgery was performed. In patients at higher risk of complications (eg, mature cataracts), surgeries were typically performed one week apart. The non-dominant eye was treated first unless the dominant eye was worse (for example, had poorer corrected visual acuity, worse cataracts, or more notable macular changes), in which case the surgery started with the dominant eye. The surgical procedures were conducted by 15 experienced ophthalmic surgeons in 21 surgical centers across the United Kingdom and Ireland.
The standard postoperative regimen included 250 mg acetazolamide tablet per oral taken 4–6 hours after discharge, topical broad-spectrum antibiotic drops (levofloxacin 5mg/mL) for 2 weeks (every two hours for the first 24 hours and then four times a day for the remaining 13 days), and topical steroid drops (dexamethasone 0.1%) for four weeks (every two hours for the first 24 hours, four times a day for 13 days and three times a day for further 14 days).
Intraocular Lenses
TECNIS™ Monofocal 1-Piece IOL (ZCB00) and TECNIS Eyhance™ IOL (ICB00) are made of the same hydrophobic acrylic material. Both lenses share the same overall geometry. These include a single-piece design with C-loop haptics, an optic diameter of 6 mm, and an overall diameter of the IOL of 13 mm. The refractive index of both lenses is 1.47 (at 35 °C) with the Abbe number of 55. The ZCB00 IOL has a spherical posterior surface and an anterior aspheric surface that corrects negative spherical aberration of −0.27 μm. The ICB00 is distinguished from the ZCB00 IOL by a modified aspheric anterior surface that creates a continuous power progression designed to improve intermediate vision. More specifically, the ICB00 IOL has a small continuous increase in central lens power, which is intended to slightly extend the depth of focus. Outside the central 1 mm diameter, the power profile of the ICB00 IOL decreases towards the periphery in a manner comparable to the ZCB00 IOL, enabling the same correction of corneal spherical aberration and resulting in comparable distance image quality to the ZCB00 IOL for a 3-mm pupil. Both lenses are available in dioptric powers from +5.0 D to +34.0 D in 0.5 D increments with a manufacturer-recommended A-constant of 119.3.
Statistical Analysis
Preoperative characteristics and postoperative refractive and visual outcomes between patients with bilateral ICB00 IOL (“ICB00” group) and those with bilateral ZCB00 IOL (“ZCB00” group) were compared. Continuous variables were assessed with an independent t-test or Mann–Whitney U-test (depending on the normality assumption), while the percentages were compared using a Chi-square test. Monocular visual acuities and refractive outcomes were analyzed using one eye per patient, the dominant eye (dominant eyes were mostly aimed for emmetropia, while non-dominant eyes were sometimes aimed for mini-monovision), and binocular visual acuities were assessed from binocular performance. One-month postoperative outcomes were used for analysis.
Results
A total of 143 dominant eyes of 143 patients were included in the ICB00 group, while the ZCB00 group consisted of 164 dominant eyes of 164 patients. The mean age of the cohort was 74.5 ± 8.0 years (51 to 94 years) for ICB00 IOL and 76.3 ± 7.6 years (50 to 95 years) for ZCB00 IOL (p = 0.05). Even though the difference in age was on the borderline of statistical significance, clinically, it was negligible and unlikely to have impact on outcomes. There was no difference between the two cohorts in the mean power of the implanted IOL (ICB00: 21.31 ± 3.90 D, range 9.5 to 30.5 D vs ZCB00: 21.64 ± 3.07 D, range 12.5 to 33.0 D; p = 0.79), the axial length (ICB00: 23.59 ± 1.27 mm, range 21.08 to 28.15 mm vs ZCB00: 23.57 ± 1.09 mm, range 20.22 to 27.62 mm; p = 0.43), or the anterior chamber depth (ICB00: 2.96 ± 0.46 mm, range 1.59 to 4.07 mm vs ZCB00: 2.95 ± 0.43 mm, range 1.23 to 4.45 mm; p = 0.79). Likewise, the male-to-female ratio was similar between the ICB00 and ZCB00 group (ICB00: 43.4%/56.6% vs ZCB00: 45.7%/54.3%, p = 0.68). Table 1 summarizes the mean preoperative and one-month postoperative refractive and visual data. Preoperatively, there was no statistically significant difference between the two cohorts in the mean refractive error or corrected visual acuity.
 |
Table 1 Preoperative and One Month Postoperative Refractive and Visual Outcomes |
Refractive Outcomes
Figure 1 depicts the distribution of manifest spherical equivalent (MSE) in the dominant eye in the two groups. The percentage of eyes with MSE within ±0.50 D of emmetropia was 87.4% (125 out of 143 eyes) in the ICB00 group and 89.6% (147/164) in the ZCB00 group (p = 0.54). Moreover, 97.9% (140/143) of eyes in the ICB00 group and 98.8% (162/164) in the ZCB00 group had postoperative MSE within ±1.00 D of emmetropia (p = 0.54).
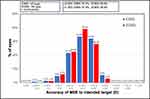 |
Figure 1 Distribution of postoperative manifest spherical equivalent (MSE). Abbreviation: D, diopter. |
Figure 2A and B show the scattergram of attempted vs achieved MSE of the two intraocular lenses. Both groups had very predictable outcomes with almost identical coefficients of determination (R2 for ICB00 0.978 and for ZCB00 0.979).
 |
Figure 2 Attempted vs achieved manifest spherical equivalent. (A) ICB00 IOL, (B) ZCB00 IOL. Abbreviation: D, diopter. |
The mean postoperative monocular manifest spherical equivalent in the dominant eye was very close to emmetropia (0.00 ± 0.44 D, range −1.88 to +1.00 D, in the ICB00 group and −0.02 ± 0.38 D, range −1.25 to +1.00 D, in the ZCB00 group, p = 0.60). The analyses of the non-dominant eye are not presented in this study, but it is important to note that the mean MSE in the non-dominant eye was slightly myopic. This should be considered when interpreting uncorrected bilateral visual acuity outcomes. The mean MSE was more myopic in the ICB00 group (−0.15 ± 0.51 D, range −2.13 to +1.00 D) than in the ZCB00 group (−0.08 ± 0.42 D, range −1.50 to +1.25 D), but the difference did not reach statistical significance (p = 0.61).
Figure 3 shows the distribution of postoperative residual refractive astigmatism. The outcomes were comparable with 58.7% (84/143) of ICB00 eyes and 64.0% (105/164) of ZCB00 eyes having residual astigmatism ≤ 0.50 D (p = 0.34), and 85.3% (122/143) of ICB00 eyes vs 86.6% (142/164) of ZCB00 eyes having residual astigmatism ≤ 1.00 D (p = 0.75). The mean residual astigmatism was −0.61 ± 0.48 D (range −2.00 to 0.00 D) and −0.57 ± 0.47 D (range −2.00 to 0.00 D) in the ICB00 and ZCB00 groups, respectively (p = 0.44).
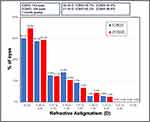 |
Figure 3 Distribution of postoperative refractive astigmatism. Abbreviation: D, diopter. |
Uncorrected Visual Acuity
Figure 4A and B depict monocular and binocular uncorrected distance visual acuity. There was no statistically significant difference in the mean logMAR UDVA in the dominant eye between the two cohorts [ICB00: 0.08 ± 0.12 logMAR (≈20/25+1), range −0.18 to 0.52 logMAR vs ZCB00: 0.09 ± 0.14 logMAR (≈20/25+0.5), range −0.18 to 0.6 logMAR; p = 0.68] or in the mean binocular UDVA [ICB00: 0.02 ± 0.10 logMAR (≈20/20−1), range −0.18 to 0.4 logMAR vs ZCB00: 0.03 ± 0.11 logMAR (≈20/20−1.5), range −0.18 to 0.52 logMAR; p = 0.78]. The percentage of eyes achieving monocular UDVA 20/25 or better was 77.6% (111/143) for ICB00 and 75.0% (123/164) for ZCB00, p = 0.59. Binocular UDVA 20/25 or better was achieved in 91.6% (131/143) and 90.9% (149/164) of patients in the ICB00 and ZCB00 groups, respectively (p = 0.82).
 |
Figure 4 Cumulative monocular (A) and binocular (B) uncorrected distance visual acuity (VA). |
The mean values of both monocular and binocular UIVA were approximately one Snellen line better for the ICB00 IOL [monocular UIVA ICB00: 0.32 ± 0.19 logMAR (≈20/40−1), range −0.12 to 0.98 logMAR vs ZCB00: 0.42 ± 0.22 logMAR (≈20/50−1), range −0.12 to 1.68 logMAR; p < 0.001; binocular UIVA: ICB00: 0.25 ± 0.18 logMAR (≈20/40+2.5), range −0.12 to 0.78 logMAR vs ZCB00: 0.36 ± 0.17 (≈20/50+2), range −0.12 to 0.78 logMAR; p < 0.001]. Cumulative UIVA values are presented in Figure 5A and B. The percentage of dominant eyes achieving 20/40 or better monocular UIVA was 49.7% (71/143) in the ICB00 group vs 28.7% (47/164) in the ZCB00 group (p < 0.001). The same percentages for binocular UIVA were 69.2% (99/143) vs 40.2% (66/164) for the ICB00 and ZCB00 IOL (p < 0.001), respectively.
 |
Figure 5 Cumulative monocular (A) and binocular (B) uncorrected intermediate visual acuity (VA). |
Corresponding with the UIVA, the mean UNVA was also approximately one Snellen line better for the ICB00 IOL (Figure 6A and B). The mean monocular UNVA in the ICB00 group was 0.58 ± 0.16 logMAR (≈20/80+1, range 0.2 to 1.1 logMAR), while it was 0.69 ± 0.20 logMAR (≈20/100+0.5 range 0.2 to 1.9 logMAR) in the ZCB00 group (p < 0.001). For the binocular UNVA, the mean values were 0.50 ± 0.16 logMAR (≈20/60, range 0.18 to 0.9 logMAR) for ICB00 vs 0.63 ± 0.17 logMAR (≈20/80−1.5, range 0.2 to 1.3 logMAR) for ZCB00 (p < 0.001). The proportion of the dominant eyes achieving monocular UNVA 20/50 or better was 20.3% (29/143) in the ICB00 group and only 5.5% (9/164) in the ZCB00 group (p < 0.001). Binocularly, 43.4% (62/143) of patients in the ICB00 group and only 14.6% (24/164) of patients in the ZCB00 group achieved UNVA 20/50 or better (p < 0.001).
 |
Figure 6 Cumulative monocular (A) and binocular (B) uncorrected near visual acuity (VA). |
Corrected Distance Visual Acuity
Both groups had similar postoperative monocular corrected distance visual acuity [ICB00: 0.02 ± 0.09 logMAR (≈20/20−2), range −0.18 to 0.4 logMAR vs ZCB00: 0.02 ± 0.09 logMAR (≈20/20−2), range-0.18 to 0.22 logMAR; p = 0.92]. The cumulative postoperative CDVA is depicted in Figure 7. The percentages are representative of the early to intermediate stage of AMD, with most of the patients achieving driving standard CDVA.
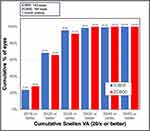 |
Figure 7 Cumulative postoperative monocular corrected distance visual acuity (VA). |
Discussion
The prevalence of age-related macular degeneration increases with advancing age.19 For instance, in European countries, approximately 3.5% of those aged 55–59 are affected by early AMD, increasing to 17.6% in the ≥85 years population, while the corresponding percentages for late AMD for the two age categories are 0.1% and 9.8%, respectively.20 Due to the aging population and the expected rise in the number of cataract surgeries,21 surgeons will often face the decision about the intraocular implant choice in the presence of ocular comorbidity. Dry AMD mainly affects central vision but also manifests as an increased visual blurriness, distortion of straight lines and text, or faded color vision.22 The symptoms in the early stage of the disease are subtle or absent,22 while corrected visual acuity is often unaffected, as evidenced in our cohort, with over 60% of patients having postoperative monocular CDVA 20/20 or better in each group. Because dry AMD progression is typically gradual, it might take several years for symptoms to worsen. Thus, the best compromise for these patients might be to use an IOL that will improve overall visual function in the upcoming years (oftentimes, it might take decades for early AMD to progress) but will not compromise the quality of vision if the vision deteriorates.
There is overwhelming evidence in the literature that Eyhance IOL provides superior intermediate visual acuity compared to a conventional monofocal IOL in a typical population of cataract patients,13,14 while delivering similar contrast sensitivity and visual phenomena incidence.23–31 In our previous study comparing the ICB00 and ZCB00 IOLs in a large population of patients,15 we found, on average, one Snellen line better UIVA in eyes with ICB00 IOL than those with ZCB00 IOLs, yet no difference was found in the distance vision or patient-reported outcomes.
In the current study, a similar difference of approximately one Snellen line was observed in both UIVA and UNVA between the two lenses, although the mean logMAR values were lower than what we had previously reported for the same IOL in eyes without comorbidity.15 For example, the mean monocular UIVA of Eyhance patients in our large population study was 0.23 ± 0.18 logMAR,15 while in the current study, it was approximately one Snellen line worse (0.32 ± 0.19 logMAR). This finding corresponds with the difference in postoperative CDVA (monocular CDVA in Eyhance eyes was −0.05 ± 0.07 logMAR in our previous study,15 compared to 0.02 ± 0.09 logMAR in the current study) and could be attributed to the presence of the disease and age difference between the two cohorts. The mean age of the Eyhance IOL cohort in our previous study was 60.07 ± 8.37 years,15 while it is 74.5 ± 8.0 years in the current study. Yet, even with the comorbidity present, a clear benefit of improved UIVA was seen in Eyhance patients in our AMD cohort. At the same time, the distance vision was comparable between the two lens models. Furthermore, both lenses exhibited very comparable refractive outcomes, which would be expected for two IOLs made of the same material with similar geometric properties.
Several smaller studies compared the performance of Eyhance IOL to a standard monofocal lens in eyes with varying ocular comorbidities.4–11 In a retrospective study, Hwang et al4 evaluated 17 eyes with ICB00 and 18 eyes with a traditional monofocal IOL (AAB00 monofocal IOL of the same manufacturer) in patients with various retinal diseases. ICB00 patients were found to have more than two Snellen lines better UIVA at 70 cm (0.17 ± 0.14 logMAR vs 0.41 ± 0.22 logMAR, p = 0.006), while there was no statistically significant difference in postoperative CDVA. Overall, their study patients had worse postoperative CDVA compared to our cohort (only approximately 20% of eyes had postoperative CDVA 20/20 or better), due to the worse disease severity. The study reported better postoperative UIVA compared to our outcomes, but the mean postoperative manifest spherical equivalent was more myopic (−0.46 ± 0.45 D in the Eyhance group compared to our MSE of 0.00 ± 0.44 D). Another study from the same clinical practice also reported approximately two Snellen lines difference in postoperative UIVA between 33 ICB00 eyes and 40 ZCB00 eyes undergoing cataract surgery in the presence of retinal disease.5 Furthermore, no difference in contrast sensitivity was observed between the two groups. In regression analysis comprising demographics and preoperative clinical variables, preoperative CDVA was the only significant predictor of the level of postoperative UIVA.5
Four studies evaluated the performance of Eyhance IOL compared to conventional TECNIS IOL in eyes undergoing cataract surgery with combined vitrectomy for epiretinal membrane.6–9 All of them concluded that Eyhance provided superior intermediate vision. The mean difference between postoperative UIVA of the Eyhance and conventional monofocal IOL was between 0.1 and 0.25 logMAR (one to two and half Snellen lines), depending on the study population, residual MSE, methodology of obtaining outcomes, or other study parameters. The postoperative defocus curve was more favorable in the Eyhance group,6,9 while both lenses exhibited similar postoperative contrast sensitivity.6–9
Another study that includes ICB00 vs ZCB00 comparison in patients with ocular co-morbidity is a study by Choi et al.10 The analysis was performed on a sample of 89 eyes of 89 patients who underwent combined cataract surgery and pars plana vitrectomy for an idiopathic macular hole. The patients had much poorer preoperative and postoperative CDVA compared to our cohort (postoperative CDVA was 0.35 ± 0.30 logMAR in the ICB00 group vs 0.39 ± 0.35 logMAR in the ZCB00 group, p = 0.68). Despite the poorer overall vision reported in this particular study, the patients still benefited from a better intermediate vision in the Eyhance group (mean UIVA: 0.58 ± 0.31 logMAR for ICB00 vs 0.71 ± 0.29 logMAR for ZCB00, p = 0.01). In regression analysis, postoperative UIVA outcomes were affected by preoperative CDVA and the size of the macular hole. The study did not find any difference in postoperative contrast sensitivity between the two lenses.
Noteworthy to discuss is a retrospective study by Mencucci et al11 comparing DIB00 (the preloaded Eyhance IOL) vs ZCB00 IOL in 48 eyes with combined cataract surgery and Descemet membrane endothelial keratoplasty for Fuchs endothelial corneal dystrophy. Unlike the other papers, this is the only report that presents corneal co-morbidity rather than fundus pathology. In agreement with all other studies, the authors did not find any difference in postoperative UDVA or CDVA between the two groups. Furthermore, no difference between the two lenses was found in other objective quality of vision measurements, such as contrast sensitivity, higher order aberrations, modular transfer function, objective scatter index, and Strehl ratio, indicating that Eyhance delivered a similar quality of vision compared to a standard monofocal IOL in this group of patients. On the other hand, UIVA outcomes agree with most other studies demonstrating one Snellen line difference in postoperative UIVA (DIB00: 0.30 ± 0.10 logMAR vs ZCB00: 0.40 ± 0.10 logMAR; p = 0.016), which translated into a significant difference in the percentage of patients requiring intermediate distance correction in daily activities (23% in DIB00 vs 87% in ZCB00 group).
Our results should be viewed in the context of some study limitations. We provide real-world refractive and visual acuity outcomes obtained from retrospective reviews of electronic medical records. Some important objective metrics of quality of vision, mainly contrast sensitivity, were not presented in our study. These are particularly important in patients with ocular comorbidity as the loss of quality of vision might often be a better indication of the disease progression than the actual Snellen visual acuity. However, the currently available studies have already established that Eyhance does not compromise contrast sensitivity in patients with comorbidities compared to a conventional monofocal IOL.5–11 Subjective patient outcomes would also be valuable, but unfortunately, we were not able to obtain them due to the low postoperative questionnaire completion rate in this particular cohort of patients. Further prospective studies are required to assess the subjective outcomes. Visual phenomena induction would be of particular interest in this group of patients.
Conclusion
Despite the outlined limitations, our study reports a relatively large sample of patients with early to intermediate AMD and summarises their refractive and visual outcomes. It provides evidence that the implantation of Eyhance IOL results in better postoperative intermediate vision without the compromise in distance vision, even in patients with pre-existing comorbidity. The progression of dry AMD is usually gradual. With the advances in modern medicine, the decline in vision can often be slowed down, preserving the visual function for an extended period of time. Hence, AMD patients in need of cataract surgery might benefit from an IOL that could improve visual function and reduce spectacle dependence without long-term compromise to the quality of vision.
Disclosure
Julie Schallhorn received personal fees from Carl Zeiss Meditec, Allergan, Forsight V6, Elios, Jellisee, Long Bridge, Vanda, ViaLase, Zeiss and has a financial interest in Journey 1, Neurotrigger, and Novus Vision. The remaining authors are employees of Optical Express, Glasgow, United Kingdom.
References
1. Braga-Mele R, Chang D, Dewey S, et al. Multifocal intraocular lenses: relative indications and contraindications for implantation. J Cataract Refract Surg. 2014;40(2):313–322. doi:10.1016/j.jcrs.2013.12.011
2. Yeu E, Cuozzo S. Matching the patient to the intraocular lens: preoperative considerations to optimize surgical outcomes. Ophthalmology. 2021;128(11):e132–e141. doi:10.1016/j.ophtha.2020.08.025
3. Kamiya K, Hayashi K, Shimizu K, et al. Multifocal intraocular lens explantation: a case series of 50 eyes. Am J Ophthalmol. 2014;158(2):215–220e1. doi:10.1016/j.ajo.2014.04.010
4. Hwang HS, Lee H, Park JH, Chae JB, Kim DY. Cataract surgery with new monofocal intraocular lens enhanced for intermediate vision and standard monofocal intraocular lens for retinal disorder. Int Ophthalmol. 2024;44(1):104. doi:10.1007/s10792-024-03047-3
5. Park MJ, Lee HS, Chang IB, Hong IH. Improved intermediate visual function with new monofocal intraocular lens in combined cataract and vitrectomy surgery for retinal disease. Korean J Ophthalmol. 2023;37(5):401–408. doi:10.3341/kjo.2023.0056
6. Giansanti F, Dragotto F, Nicolosi C, et al. Enhancing intermediate vision in patients affected by epiretinal membrane treated by phaco-vitrectomy. J Clin Med. 2023;12(15):5016. doi:10.3390/jcm12155016
7. Choi SH, Cho IH, Jeon GS, Chang IB, Ma DJ, Hong IH. Comparative evaluation of visual outcomes in combined cataract and vitrectomy for idiopathic epiretinal membrane with an advanced or conventional intraocular lens. Ophthalmic Res. 2024;67(1):221–231. doi:10.1159/000538316
8. Jukic T, Bajraktari G, Vukojevic N, et al. Clinical outcomes of a new monofocal intraocular lens in patients undergoing phacovitrectomy for idiopathic epiretinal membrane. Ophthalmologica. 2024;247(4):251–260. doi:10.1159/000540362
9. Jeong S, Son S, Sagong M. Efficacy of enhanced monofocal intraocular lens in combined phacovitrectomy for patients with photoreceptor-preserving epiretinal membrane. Sci Rep. 2024;14(1):24377. doi:10.1038/s41598-024-75008-w
10. Choi SH, Lee HS, Chang IB, et al. Evaluation of a new monofocal intraocular lens in patients undergoing cataract and vitrectomy surgery for idiopathic macular hole. Curr Eye Res. 2023;48(10):904–910. doi:10.1080/02713683.2023.2229542
11. Mencucci R, Romualdi G, De Vitto C, Cennamo M. Enhanced monofocal intraocular lenses in Fuchs’ endothelial dystrophy patients: results from triple descemet membrane endothelial keratoplasty procedure. Life. 2024;14(2):243. doi:10.3390/life14020243
12. Fernandez J, Rocha-de-lossada C, Zamorano-Martin F, Rodriguez-calvo-de-mora M, Rodriguez-Vallejo M. Positioning of enhanced monofocal intraocular lenses between conventional monofocal and extended depth of focus lenses: a scoping review. BMC Ophthalmol. 2023;23(1):101. doi:10.1186/s12886-023-02844-1
13. Wan KH, Ack A, Kua WN, et al. Enhanced monofocal versus conventional monofocal intraocular lens in cataract surgery: a meta-analysis. J Refract Surg. 2022;38(8):538–546. doi:10.3928/1081597X-20220707-01
14. Redruello-Guerrero P, Rivera-Izquierdo M, Jimenez-Gutierrez C, Lainez-Ramos-Bossini AJ, Yela R, Lopez-Marin I. Improvement of intermediate vision with new monofocal intraocular lenses: a systematic review and meta-analysis. Eur J Ophthalmol. 2023;33(3):1308–1319. doi:10.1177/11206721221127075
15. Dell SJ, Hannan SJ, Venter JA, et al. Comparative analysis of clinical and patient-reported outcomes of a new enhanced monofocal IOL and a conventional monofocal IOL. Clin Ophthalmol. 2024;18:1157–1169. doi:10.2147/OPTH.S456332
16. Mehta H. Management of cataract in patients with age-related macular degeneration. J Clin Med. 2021;10(12):2538. doi:10.3390/jcm10122538
17. Fabrykowski MC. Retinal considerations crucial for accurate biometry. Optometry Times J. 2022;14(2). https://www.optometrytimes.com/view/retinal-considerations-crucial-for-accurate-biometry.
18. Coleman HR, Chan CC, Ferris FL, Chew EY. Age-related macular degeneration. Lancet. 2008;372(9652):1835–1845. doi:10.1016/S0140-6736(08)61759-6
19. Thomas CJ, Mirza RG, Gill MK. Age-related macular degeneration. Med Clin North Am. 2021;105(3):473–491. doi:10.1016/j.mcna.2021.01.003
20. Colijn JM, Buitendijk GHS, Prokofyeva E, et al. Prevalence of age-related macular degeneration in Europe: the past and the future. Ophthalmology. 2017;124(12):1753–1763. doi:10.1016/j.ophtha.2017.05.035
21. Chen X, Xu J, Chen X, Yao K. Cataract: advances in surgery and whether surgery remains the only treatment in future. Adv Ophthalmol Pract Res. 2021;1(1):100008. doi:10.1016/j.aopr.2021.100008
22. Schultz NM, Bhardwaj S, Barclay C, Gaspar L, Schwartz J. Global burden of dry age-related macular degeneration: a targeted literature review. Clin Ther. 2021;43(10):1792–1818. doi:10.1016/j.clinthera.2021.08.011
23. Huh J, Eom Y, Yang SK, Choi Y, Kim HM, Song JS. A comparison of clinical outcomes and optical performance between monofocal and new monofocal with enhanced intermediate function intraocular lenses: a case-control study. BMC Ophthalmol. 2021;21(1):365. doi:10.1186/s12886-021-02124-w
24. Steinmuller LN, Greve D, Rua Amaro D, Bertelmann E, von Sonnleithner C. Analysis of higher-order aberrations in relation to the clinical outcome of an enhanced monofocal IOL. Eur J Ophthalmol. 2022;11206721221134171. doi:10.1177/11206721221134171
25. Auffarth GU, Gerl M, Tsai L, et al. Clinical evaluation of a new monofocal IOL with enhanced intermediate function in patients with cataract. J Cataract Refract Surg. 2021;47(2):184–191. doi:10.1097/j.jcrs.0000000000000399
26. Choi WK, Han HJ, Son HS, Khoramnia R, Auffarth GU, Choi CY. Clinical outcomes of bilateral implantation of new generation monofocal IOL enhanced for intermediate distance and conventional monofocal IOL in a Korean population. BMC Ophthalmol. 2023;23(1):157. doi:10.1186/s12886-023-02897-2
27. Corbelli E, Iuliano L, Bandello F, Fasce F. Comparative analysis of visual outcome with 3 intraocular lenses: monofocal, enhanced monofocal, and extended depth of focus. J Cataract Refract Surg. 2022;48(1):67–74. doi:10.1097/j.jcrs.0000000000000706
28. Lopes D, Loureiro T, Carreira R, et al. Comparative evaluation of visual outcomes after bilateral implantation of an advanced or conventional monofocal intraocular lens. Eur J Ophthalmol. 2022;32(1):229–234. doi:10.1177/1120672121995343
29. Donoso R, Torres A, Klagges J, et al. Enhanced vs conventional monofocal intraocular lens clinical results in patients with cataract: randomized clinical trial. J Cataract Refract Surg. 2023;49(8):818–825. doi:10.1097/j.jcrs.0000000000001224
30. Mencucci R, Cennamo M, Venturi D, Vignapiano R, Favuzza E. Visual outcome, optical quality, and patient satisfaction with a new monofocal IOL, enhanced for intermediate vision: preliminary results. J Cataract Refract Surg. 2020;46(3):378–387. doi:10.1097/j.jcrs.0000000000000061
31. Kang KH, Song MY, Kim KY, Hwang KY, Kwon YA, Koh K. Visual performance and optical quality after implantation of a new generation monofocal intraocular lens. Korean J Ophthalmol. 2021;35(2):112–119. doi:10.3341/kjo.2020.1115
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

