Back to Journals » Clinical Ophthalmology » Volume 18
Combined Phacoemulsification and 360-Degree Suture Trabeculotomy Ab Externo in Primary Chronic Angle Closure Glaucoma: A Modified Technique
Authors Elhofi AS, Helaly HA , Eldakhs R
Received 29 May 2024
Accepted for publication 6 September 2024
Published 7 December 2024 Volume 2024:18 Pages 3657—3666
DOI https://doi.org/10.2147/OPTH.S480485
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Abdelhamid Shaker Elhofi, Hany Ahmed Helaly, Rania Eldakhs
Ophthalmology Department, Faculty of Medicine, Alexandria University, Alexandria, Egypt
Correspondence: Hany Ahmed Helaly, Email [email protected]
Purpose: To assess the outcome of combined phacoemulsification and 360-degree suture trabeculotomy ab externo in chronic angle closure glaucoma using a modified technique.
Methods: This is a retrospective clinical study that included 60 eyes of 60 patients who had undergone combined phacoemulsification and 360-degree suture trabeculotomy ab externo for the treatment of primary chronic angle closure glaucoma. The patients were divided into two groups. The first group (ab externo group) and the second group (modified ab externo group). Data were collected from the records and the final follow-up visit including age, sex, intraocular pressure (IOP), number of antiglaucoma medications, presence of complications, corrected distant visual acuity, and need for another intervention. All the included patients completed at least 12 months follow-up.
Results: The ab externo group included 30 patients and the modified ab externo group included 30 patients. The postoperative IOP was reduced in both groups significantly from the preoperative levels. The percent of reduction was around 60% for both groups (59.5% for the ab externo group and 59.3% for the modified ab externo group). There was statistically significant reduction in the mean amount of required topical medications after the intervention for both groups (p = 0.001). Most of the complications were not serious. Around 90% of the cases in both groups had mild degree of grade 1 hyphema.
Conclusion: Both ab externo 360 degree suture trabeculotomy and its modified technique with ab interno pulling of the suture when combined with phacoemulsification are safe and provide adequate decrease in the intraocular pressure. Modified technique of ab interno pulling of the prolene suture might be more gentle procedure with less severe hyphema and lower chance of rupture of trabeculo-Descemet’s membrane.
Keywords: suture trabeculotomy, phaco-trabeculotomy, 360-degree trabeculotomy, ab externo, chronic angle closure glaucoma
Introduction
In angle-closure glaucoma, the outflow of aqueous humor is obstructed leading to an increase in the intraocular pressure (IOP). This obstruction may be primarily resulting from an anatomical predisposition of the eye or secondary to pathophysiologic diseases in the eye. Relative pupillary block with crowding of the angle is the possible mechanism for angle closure glaucoma. The possible explanation for such mechanisms is the increase in lens thickness with age or anterior displacement of the lens due to a posterior force eg choroidal effusion.1–4
Primary angle closure glaucoma (PACG) has different prevalence according to the geographic and racial distribution. Recent studies in Asian countries reported higher prevalence and incidence rates of PACG to those reported in studies of other racial groups.5–7 The presentation of chronic PACG is either asymptomatic or symptoms related to optic nerve damage, but not due to raised IOP. The signs of chronic PACG include glaucomatous disc cupping and/or nerve fiber layer defects, raised IOP, associated visual field defects, and a narrow or closed anterior chamber angle.8,9 Multiple surgical treatments have been suggested for PACG. Those include laser peripheral iridotomy, laser iridoplasty, trabeculectomy, trabeculotomy, gonioplasty, and lens extraction.10–14
The standard trabeculotomy technique used a metal probe or a trabeculotome to perform an opening between Schlemm’s canal and the angle of the anterior chamber for 120 degrees. Various modifications were made for this procedure. Utilizing Nylon suture for 360-degree trabeculotomy was first used in 1962. Later on, the use of prolene suture was described in 1995 and has been used since then.15–17
Ab externo 360-degree trabeculotomy using prolene suture is a well-known procedure with a high success rate. Although being successful in lowering the IOP, variable complications were noted such as hyphema and false passage of the prolene suture in the suprachoroidal space.18–20
Ab interno pulling of the prolene suture in 360-degree trabeculotomy is a newer technique, which is more controllable than the usual Ab externo prolene suture pulling that aims at lowering the rate of the complications eg trabeculo-Descemet’s membrane rupture and hyphema. The current study aimed at assessing the outcome of combined phacoemulsification and 360-degree suture trabeculotomy ab externo in chronic angle closure glaucoma using a modified technique.
Materials and Methods
This is a retrospective comparative interventional clinical study that included 60 eyes of 60 patients who had undergone combined phacoemulsification and 360-degree suture trabeculotomy ab externo for the treatment of primary chronic angle closure glaucoma. The patients were divided into two groups. The first group (ab externo group) had undergone the standard ab externo 360-degree suture trabeculotomy procedure with ab externo pulling of the prolene suture. The second group (modified ab externo group) had undergone a modified ab externo 360-degree suture trabeculotomy procedure in which the pulling of the prolene suture is done through an ab interno approach. Patients were recalled for a final follow-up visit. The patients signed an informed consent in which they agreed to participate in the study. If the patient had undergone bilateral surgery, only one eye was included in the study to avoid duplication of data. This study was approved by the local ethics committee of the Faculty of Medicine of Alexandria University, Alexandria, Egypt. The ethical code was based on the tenets of the Declaration of Helsinki.
Records of the patients were reviewed (from January 2020 to December 2022). Patients were diagnosed as chronic PACG if the following criteria were present: the presence of glaucomatous optic disc changes associated with corresponding glaucomatous visual field defects, and the anterior chamber angle is closed on gonioscopy. Data were collected from the records and the final follow up visit including: age, sex, right or left eye, history of previous laser iridotomy or iridoplasty, IOP, cup: disc ratio, number of antiglaucoma medications, presence of complications, corrected distant visual acuity (CDVA) converted into logMAR, visual field mean defect (dB), need for another intervention eg ab interno revision and the extent of peripheral anterior synechiae if present. All the included patients completed at least 12 months follow-up. Patients were excluded if they had secondary angle closure glaucoma, previous intraocular surgery, and patients with complicated phacoemulsification procedure.
Surgical Procedure
All surgeries were performed by a single surgeon (A.E.) using a reproducible technique. All patients were operated upon under general anesthesia. A corneal bridle suture was taken, and a superior conjunctival flap was created with a fornix base pattern (Figure 1). A superficial rectangular scleral flap of 5 × 5 mm size partial thickness scleral flap was dissected, which was extended up to 1 mm of clear cornea (Figure 2). Then, a deep scleral flap of 4 × 4 mm size was created and extended till reaching scleral spur and advanced till the deroofing the Schlemm’s canal and the creation a trabeculo-Descemet’s window (Figure 3). This was followed by phacoemulsification and IOL implantation in the bag. The inner wall of Schlemm’s canal was then exposed, and viscoelastic material was injected into the canal. A 5/0 prolene suture with a blunted tip, using a cautery, was inserted into the Schlemm’s canal and threaded circumferentially until the other end came from the opposite side.
 |
Figure 1 A corneal bridle suture was taken and a superior conjunctival flap was created with a fornix base pattern. |
 |
Figure 2 A superficial rectangular scleral flap of 5×5 mm size partial thickness scleral flap, which was extended up to 1 mm of clear cornea. |
 |
Figure 3 Deep scleral flap 4×4 mm was created and extended till reaching scleral spur and advanced till deroofing the Schlemm’s canal and create a trabeculo-Descemet’s window. |
In the first group, both ends of the suture were grasped and pulled until it was seen in the anterior chamber (Figure 4). Then, the prolene suture was pulled out, and the second scleral flap was cut anteriorly. The first scleral flap was sutured using two sutures, and the conjunctiva was closed with a 10/0 Nylon suture to prevent leakage of aqueous humor. This was followed by injection of subconjunctival 5 Fluorouracil. In the second group, a trabeculotome was used from the nasal end of Schlemm’s canal to perform 120 trabeculotomy (Figure 5). A small limbal incision at the temporal side was created, and the anterior chamber was filled with viscoelastic. Prolene suture was then gently pulled from the inside of the anterior chamber (ab interno) by an end gripping forceps while holding still the other end of the suture ab externo. This was followed by pulling the prolene suture out and continuing the same steps as the first group. Gonio lens was used to identify the temporal end of the prolene suture.
 |
Figure 4 Both ends of the suture were grasped and pulled until it was seen in the anterior chamber. |
 |
Figure 5 A trabeculotome was used from the nasal end of Schlemm’s canal to perform 120 trabeculotomy. |
Ab interno revision was done, when needed, in operation room under topical anesthesia and a spatula was inserted into the anterior chamber through a side port toward the trabeculo-Descemet’s window and open it by the blunt tip of the spatula seeing it under the conjunctiva then subconjunctival injection of 0.50 mL of 5-fluorouracil around the bleb was done.
The postoperative follow-up visits data were recorded at 1 month, 3 months, 6 months, 9 months, and 12 months. The primary outcome was the intraocular pressure. Other outcome parameters were the number of antiglaucoma medications, complications rates, best corrected visual acuity, and cumulative success rates (Kaplan–Meier survival analysis). Surgical success was defined as an IOP between 6 and 15 mmHg. When no antiglaucoma medication was needed, it was considered a complete success. When antiglaucoma medication(s) was/were needed, it was considered a qualified success. Surgical failure was defined as IOP > 15 mmHg despite maximum tolerated antiglaucoma medications or the need for additional glaucoma surgery. Fluctuations of the IOP during the first postoperative 4 weeks were not determinants of surgical success as the short-term changes would not affect the long-term success rates.
The assessment of safety measures included intra- and postoperative complication rates, BCVA at 12 months postoperative. The possible postoperative complications to look for included hyphema, shallow anterior chamber and wound leaks, IOP spikes of >30 mmHg within the first month, hypotony with an IOP <5 mmHg, infection, and vision loss.
Data analysis was performed using the Social Sciences SPSS Statistics for Windows (version 26.0; SPSS Inc., Chicago, IL, USA). Quantitative data were described using the range, mean, and standard deviation. Normality of the data was evaluated using the Kolmogorov–Smirnov test. ANOVA test was used to compare different means. Paired t test for paired samples was used to compare the means of the same group. Kaplan Meier survival analysis was used to show cumulative success rates over time. Chi square test was also used. Differences were considered statistically significant when the associated p value was less than 0.05.
Results
The study included 60 eyes of 60 patients that were divided into 2 groups according to the method of intervention. The ab externo group included 30 patients and the modified ab externo group included 30 patients. Thirty-four patients (56.7%) were females and 26 patients (43.3%) were males. Table 1 shows the demographic data of the 2 groups. There was no statistically significant difference between the 2 groups regarding the age, sex and laterality. Table 2 shows the preoperative data of the 2 groups including IOP levels, number of antiglaucoma medications, CDVA, mean deviation of the visual field, cup: disc ratio, previous laser iridotomy or iridoplasty, and extent of peripheral anterior synechiae (PAS). There was no statistically significant difference between the 2 groups (p > 0.05).
 |
Table 1 Demographic Data of the Included Patients |
 |
Table 2 The Preoperative Data of the Included Patients |
The postoperative IOP was reduced in both groups significantly from the preoperative levels. The percent of reduction was around 60% for both groups (59.5% for the ab externo group and 59.3% for the modified ab externo group). In the ab externo group, the IOP was reduced from 28.40 + 6.80 mmHg preoperatively to 11.51 + 3.99 at 12 months postoperative (p < 0.05). In the modified ab externo group, the IOP was reduced from 28.80 + 6.40 mmHg preoperatively to 11.73 + 4.09 at 12 months postoperative (p < 0.05). There was statistically significant difference between all the postoperative IOP measurements in comparison to the preoperative level for both groups (p < 0.05). There was no statistically significant difference between the 2 groups regarding the IOP measurements at different postoperative periods (p > 0.05). There was statistically significant difference between the IOP measurements at 1 and 3 months for both groups. There was statistically significant difference between the IOP measurements at 6 and 9 months for both groups. Table 3 shows the different preoperative IOP measurements at the preoperative and the postoperative periods.
 |
Table 3 The Preoperative and Postoperative Intraocular Pressure Values Among the Study Group |
Table 4 shows the mean preoperative and postoperative values for topical antiglaucoma medications required among the study group. There was statistically significant reduction in the mean amount of required topical medications after the intervention for both groups (p = 0.001). There was no statistically significant difference between the different follow-up periods among the same group (p > 0.05). There was no statistically significant difference between the 2 groups along the different follow up postoperative periods (p > 0.05).
 |
Table 4 The Mean Preoperative and Postoperative Values for Topical Antiglaucoma Medications Required Among the Study Group |
There was no statistically significant difference between the preoperative and the postoperative CDVA in the 2 groups along the different postoperative period. Also, there was no statistically difference between the 2 groups along the postoperative follow-up period. Table 5 shows the mean best corrected visual acuity among the study group. Table 6 shows the visual field defect mean deviation among the study group. There was no statistically significant change in the mean deviation postoperatively from the preoperative levels. There was no statistically significant change along the different periods of postoperative follow-up among the same group and between the 2 groups (p < 0.05).
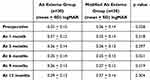 |
Table 5 The Mean Best Corrected Visual Acuity Among the Study Group |
 |
Table 6 The Visual Field Defect Mean Deviation Among the Study Group |
Most of the complications were not serious. Around 90% of the cases in both groups had mild degree of grade 1 hyphema. Six cases in the ab externo group and 3 cases in the modified ab externo group had grade 2 to 3 hyphema. Mild corneal edema was found in 4 cases of both groups. Shallow anterior chamber was found in the early postoperative period in 3 cases of the ab externo group and 2 cases in the modified ab externo group. None of the cases of both groups had hypotony (IOP < 5 mmHg). Four cases of the ab externo group had Descemet’s membrane detachment while only 1 case in the modified ab externo group suffered from this complication (p = 0.161).
Ab interno revision was needed in three cases from each group. Diode cyclophotocoagulation was done to 4 cases in the ab externo group and to 3 cases of the modified ab externo group. Ahmed glaucoma valve was needed for one case of the ab externo group.
Complete success rates for the ab externo group did not differ with statistical significance from the modified ab externo group. Figures 6 and 7 show the survival analysis for complete and qualified success rates for both groups. For ab externo group, the complete success rate was 70% at 1 month postoperative and 45% at 12 months postoperative. For the modified ab externo group, the complete success rate was 70% at 1 month postoperative and 55% at 12 months postoperative. The qualified success rate was 30% at 1 month postoperative for both groups and 45% at 12 months for both groups.
 |
Figure 6 Survival analysis for complete success for ab externo (blue) and modified ab externo (red) groups. |
 |
Figure 7 Survival analysis for qualified success for ab externo (blue) and modified ab externo (red) groups. |
Discussion
Combined phacoemulsification with 360 trabeculotomy is associated with better long-term control of IOP in patients with primary open angle glaucoma.21,22 The cases included in the current study had undergone combined phacoemulsification and 360-degree suture trabeculotomy ab externo for the treatment of primary chronic angle closure glaucoma. In the current study, it was found that both males and females, regardless of their age group, showed similar postoperative results with both techniques. This is similar to the study by Khalil et al.23 However, their study was on phacotrabeculectomy and the follow up period was 5 months postoperative.
In a study done by Sato et al,21 they conducted their treatment for open angle glaucoma with coexisting cataract. They used purely ab interno technique for 360 degree suture trabeculotomy with 24 months follow-up period. They concluded that 360 degree suture trabeculotomy ab interno with phacoemulsification appeared to be a more beneficial option for mild-to-moderate open-angle glaucoma with coexisting cataract than phacoemulsification alone. Mean IOP value was 18.4 mm Hg and 0.9 preoperative showed significant reduction to 11.8 mm Hg at 24 months. In the current study, the postoperative IOP reduction was significant in both groups immediately postoperatively and after 12 months follow-up showing that combined phacoemulsification with 360 suture trabeculotomy is effective in controlling the IOP with both techniques even after several months from the date of surgery.
The postoperative CDVA remained stationary in comparison with the preoperative CDVA. This stable CDVA means that the procedure with both techniques is a safe and an effective measure to halt the decline in VA as most of the presented patients included in the study were in an advanced stage of the disease. It is worth mentioning here that most of the cataracts were in early stages and phacoemulsification was performed mainly for glaucoma purpose. In early disease stages, visual acuity improves after 360 trabeculotomy as shown in the study done by Sato et al,21 and that by Mendicino et al.21,24
The immediate postoperative complications included hyphema, most of the cases showed only grade I hyphema, corneal edema, and shallow anterior chamber. All of them were not serious and resolved 1 week postoperatively. This was also similar to the study done by Dragosloveanu et al.25
Descemet’s membrane detachment is one of the intraoperative complications that can occur with 360 trabeculotomy. It occurred more in the conventional technique than the modified technique, which suggests that the modified technique is more controlled than the original ab externo.19,26 However, this difference was not statistically significant. This might be due to a small sample size.
In the current study, the need for re-intervention whether by ab interno revision or diode cyclophotocoagulation was in a small number of the included subjects and it was less with the modified technique. The modified 360 trabeculotomy was associated with better long-term results and lower re-intervention rates compared to the conventional 360 and 120 trabeculotomy in patients with PACG as it has shown good results with POAG patients. This was comparative to the results mentioned by a study done by Chin Shinki et al.27 In the current study, the need for glaucoma medication postoperatively decreased significantly equally in both groups emphasizing the benefit of 360 trabeculotomy in lower the IOP and replacing medications. Maria E. Lim et al19 found that fewer glaucoma medications were needed after surgery (p = 0.01).
One advantage of the study is the few literature studies that are discussing 360 trabeculotomy for treatment of chronic angle closure glaucoma. Another advantage is the 12-month follow-up period and adequate amount of included cases. Among the disadvantages of the study, are the retrospective nature, and the need for larger number of patients to prove that the safety of the modified technique is more than the conventional technique.
Conclusions
In conclusion, both ab externo 360 degree suture trabeculotomy and its modified technique with ab interno pulling of the suture when combined with phacoemulsification are safe and provide adequate decrease in the intraocular pressure. Modified technique of ab interno pulling of the prolene suture might be more gentle procedure with less severe hyphema and lower chance of rupture of trabeculo-Descemet’s membrane.
Abbreviations
IOP, intraocular pressure; PAGC, primary angle closure glaucoma; dB, decibel; CDVA, corrected distant visual acuity; PAS, peripheral anterior synechiae.
Data Sharing Statement
Available upon request from the corresponding author.
Ethics and Consent to Participate
This study was approved by the local ethics committee of the Faculty of Medicine, Alexandria University, Alexandria, Egypt. The tenets of the Declaration of Helsinki were followed for this study. All the included patients were recalled for the final follow-up visit and parents signed an informed consent form.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wright C, Tawfik MA, Waisbourd M, Katz LJ. Primary angle‐closure glaucoma: an update. Acta ophthalmologica. 2016;94(3):217–225. doi:10.1111/aos.12784
2. Sun X, Dai Y, Chen Y, et al. Primary angle closure glaucoma: what we know and what we don’t know. Prog Retinal Eye Res. 2017;57:26–45. doi:10.1016/j.preteyeres.2016.12.003
3. Nongpiur ME, Ku JY, Aung T. Angle closure glaucoma: a mechanistic review. Curr Opin Ophthalmol. 2011;22(2):96–101. doi:10.1097/ICU.0b013e32834372b9
4. Salmon JF. Predisposing factors for chronic angle-closure glaucoma. Progress in retinal and eye research. Progress in Retinal and Eye Research. 1999;18(1):121–132. doi:10.1016/s1350-9462(98)00007-x
5. Day AC, Baio G, Gazzard G, et al. The prevalence of primary angle closure glaucoma in European derived populations: a systematic review. Br J Ophthalmol. 2012;96(9):1162–1167. doi:10.1136/bjophthalmol-2011-301189
6. Cheng JW, Zong Y, Zeng YY, Wei RL. The prevalence of primary angle closure glaucoma in adult Asians: a systematic review and meta-analysis. PLoS One. 2014;9(7):e103222. doi:10.1371/journal.pone.0103222
7. Sawaguchi S, Sakai H, Iwase A, et al. Prevalence of primary angle closure and primary angle-closure glaucoma in a southwestern rural population of Japan: the Kumejima Study. Ophthalmology. 2012;119(6):1134–1142. doi:10.1016/j.ophtha.2011.12.038
8. Salmon JF. Presenting features of primary angle-closure glaucoma in patients of mixed ethnic background. South Afr Med J. 1993;83(8):594–597.
9. Saw SM, Gazzard G, Friedman D, et al. Awareness of glaucoma, and health beliefs of patients suffering primary acute angle closure. Br J Ophthalmol. 2003;87(4):446–449. doi:10.1136/bjo.87.4.446
10. Tarongoy P, Ho CL, Walton DS. Angle-closure glaucoma: the role of the lens in the pathogenesis, prevention, and treatment. Survey Ophthalmol. 2009;54(2):211–225. doi:10.1016/j.survophthal.2008.12.002
11. Marchini G, Chemello F, Berzaghi D, Zampieri A. New findings in the diagnosis and treatment of primary angle-closure glaucoma. Prog Brain Res. 2015;221:191–212.
12. Deng BL, Jiang C, Ma B, et al. Surgical treatment for primary angle closure-glaucoma: a Meta analysis. Int J Ophthalmol. 2011;4(3):223. doi:10.3980/j.issn.2222-3959.2011.03.01
13. Lai J, Choy BN, Shum JW. Management of primary angle-closure glaucoma. Asia-Pac J Ophthalmol. 2016;5(1):59–62. doi:10.1097/APO.0000000000000180
14. Sharkawi E, Artes PH, Lindegger DJ, et al. Gonioscopy-assisted transluminal trabeculotomy in primary angle-closure glaucoma. Graefes Arch Clin Exp Ophthalmol. 2021;259(10):3019–3026. doi:10.1007/s00417-021-05244-7
15. Hoskins HD, Shaffer RN, Hetherington J. Goniotomy vs trabeculotomy. J Pediatr Ophthalmol Strabismus. 1984;21(4):153–158. doi:10.3928/0191-3913-19840701-06
16. Anderson DR. Trabeculotomy compared to goniotomy for glaucoma in children. Ophthalmology. 1983;90(7):805–806. doi:10.1016/S0161-6420(83)34484-5
17. McPherson SD, Berry DP. Goniotomy vs external trabeculotomy for developmental glaucoma. Am J Ophthalmol. 1983;95(4):427–431. doi:10.1016/0002-9394(83)90260-X
18. Lim ME, Neely DE, Wang J, Haider KM, Smith HA, Plager DA. Comparison of 360-degree versus traditional trabeculotomy in pediatric glaucoma. J AAPOS. 2015;19(2):145–149. doi:10.1016/j.jaapos.2015.01.008
19. Lim ME, Dao JB, Freedman SF. 360-degree trabeculotomy for medically refractory glaucoma following cataract surgery and juvenile open-angle glaucoma. Am J Ophthalmol. 2017;175:1–7. doi:10.1016/j.ajo.2016.11.011
20. Celea C, Dragosloveanu S, Pop M, Celea C. Comparison of 360-degree circumferential trabeculotomy and conventional trabeculotomy in primary pediatric glaucoma surgery: part 1. J Pediatr Ophthalmol Strabismus. 2016;53(6):357–364. doi:10.3928/01913913-20160809-01
21. Sato T, Hirata A, Mizoguchi T. Outcomes of 360 suture trabeculotomy with deep sclerectomy combined with cataract surgery for primary open angle glaucoma and coexisting cataract. Clin Ophthalmol. 2014;11:1301–1310. doi:10.2147/OPTH.S64264
22. Jin GJC, Crandall AS, Jones JJ. Phacotrabeculectomy: assessment of outcomes and surgical improvements. J Cataract Refract Surg. 2007;33(7):1201–1208. doi:10.1016/j.jcrs.2007.03.050
23. Khalil ZK, Shah SA, Naseem A, Mudassir S, Orakzai AM. The efficacy of phacotrabeculectomy in reducing intraocular pressure. J Saidu Med College. 2024;14(2):70–73. doi:10.52206/jsmc.2024.14.2.809
24. Mendicino ME, Lynch MG, Drack A, et al. Long-term surgical and visual outcomes in primary congenital glaucoma: 360 trabeculotomy versus goniotomy. J AAPOS. 2000;4(4):205–210. doi:10.1067/mpa.2000.106201
25. Dragosloveanu CD, Celea CG, Dragosloveanu Ş. Comparison of 360 circumferential trabeculotomy and conventional trabeculotomy in primary pediatric glaucoma surgery: complications, reinterventions and preoperative predictive risk factors. Intl Ophthalmol. 2020;40:3547–3554. doi:10.1007/s10792-020-01544-9
26. Liu SS, Liu LM, Fan XJ, et al. Bedside anterior segment optical coherence tomography-assisted reattachment of severe hemorrhagic Descemet’s membrane detachment after ab externo 360-degree suture trabeculotomy combined with trabeculectomy. Int J Ophthalmol. 2023;16(2):316. doi:10.18240/ijo.2023.02.22
27. Chin S, Nitta T, Shinmei Y, et al. Reduction of intraocular pressure using a modified 360-degree suture trabeculotomy technique in primary and secondary open-angle glaucoma: a pilot study. J Glaucoma. 2012;21(6):401–407. doi:10.1097/IJG.0b013e318218240c
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

