Back to Journals » Journal of Hepatocellular Carcinoma » Volume 12
Combining Hepatic Arterial Interventional Therapies with Lenvatinib and Programmed Cell Death-1 Inhibitors for Hepatocellular Carcinoma with Portal Vein Tumor Thrombosis: A Single-Center, Real-World Study
Authors Shen X , Shao T, Yu J, Zhang Z
Received 20 April 2025
Accepted for publication 24 June 2025
Published 2 July 2025 Volume 2025:12 Pages 1267—1278
DOI https://doi.org/10.2147/JHC.S530550
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Mohamed Shaker
Xuehan Shen,* Tianyin Shao,* Jun Yu, Zhiwei Zhang
Hepatic Surgery Center, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430030, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhiwei Zhang, Hepatic Surgery Center, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, No. 1095 Jiefang Avenue, Wuhan, 430030, People’s Republic of China, Email [email protected]
Background and Purpose: The survival of hepatocellular carcinoma (HCC) patients with portal vein tumor thrombosis (PVTT) was poor. This study aimed to investigate the efficacy and safety of hepatic arterial interventional therapies (HAIT) combined with lenvatinib and programmed cell death-1 (PD-1) inhibitors for HCC patients with PVTT.
Methods: In this retrospective study, HCC patients with PVTT treated with HAIT combined with lenvatinib and PD-1 inhibitors (H-L-P group) or lenvatinib plus PD-1 inhibitors (L-P group) between June 2020 and December 2023 were analyzed. Overall survival (OS), progression-free survival (PFS), and tumor response were evaluated to assess the efficacy, while treatment-related adverse events (TRAEs) were evaluated to assess the safety. Propensity score matching (PSM) was applied to balance the baseline differences.
Results: In this study, 208 HCC patients with PVTT were enrolled, including 120 patients in H-L-P group and 88 patients in L-P group. After PSM, there were 74 patients per group, the H-L-P group showed significantly better median OS (19 months vs 14 months, p < 0.001) and median PFS (10 months vs 4 months, p < 0.001) than L-P group; higher objective response rate (ORR) (37.8% vs 16.2%, p < 0.001) and disease control rate (DCR) (78.4% vs 47.3%, p < 0.001) were observed in the H-L-P group. All TRAEs were controlled, and the three most prevalent TRAEs in the H-L-P group were elevated aspartate aminotransferase (AST), elevated alanine aminotransferase (ALT), and vomiting.
Conclusion: Combining HAIT with lenvatinib and PD-1 inhibitors is a safe and promising treatment pattern for HCC patients with PVTT.
Keywords: hepatocellular carcinoma, hepatic arterial interventional therapies, lenvatinib, programmed cell death protein-1 inhibitors, portal vein tumor thrombosis
Introduction
Hepatocellular carcinoma (HCC) constitutes the third leading cause of cancer-related mortality worldwide.1 Approximately 44–62% of HCC patients have portal vein tumor thrombosis (PVTT) and are diagnosed as being in an advanced stage with an extremely poor prognosis.2–4 PVTT promotes the intrahepatic dissemination of tumor cells and increases the risk of distant metastasis. Furthermore, the elevated portal venous pressure resulting from PVTT contributes to the progressive impairment of liver function and exacerbates ascites formation.5
Systemic therapies, including tyrosine kinase inhibitors (TKIs) and programmed cell death-1 (PD-1) inhibitors, constitute the cornerstone of treatment strategies for HCC patients with advanced stage.6,7 Lenvatinib, one of the TKIs, has attracted growing attention and application in HCC owing to its dual anti-angiogenic and immunomodulatory effects.8 The combination of lenvatinib and PD-1 inhibitors may exert a synergistic anti-tumor effect.9 Although the IMbrave 150 study (atezolizumab plus bevacizumab) and the Keynote 524 study (lenvatinib plus pembrolizumab) achieved a benefit for advanced HCC, the prognosis for HCC patients with PVTT still remains poor after systematic therapies.10–12 This suggests that more effective treatment strategies for PVTT are needed.
Transcatheter arterial chemoembolization (TACE) and hepatic arterial infusion chemotherapy (HAIC) are the two most prevalent forms of hepatic arterial interventional therapies (HAIT) and are widely used for treating advanced HCC patients in Asia-Pacific region.13,14 HAIT can change the tumor immune microenvironment to improve the efficacy of systemic therapies in addition to performing local anti-tumor treatment.15,16 A multicenter study demonstrated that the combination of TACE and TKIs plus PD-1 inhibitors for HCC with PVTT led to longer overall survival (OS) and progression-free survival (PFS) than TKIs plus PD-1 inhibitors.17 Another multicenter study comparing camrelizumab plus rivoceranib with or without HAIC for HCC patients with PVTT showed that the addition of HAIC to camrelizumab plus rivoceranib significantly improve median OS (18.7 months vs 11.0 months, p < 0.001) and PFS (10.0 months vs 5.6 months, p < 0.001).18
Supported by growing evidence of clinical benefits,19,20 the combination of HAIT and systemic therapies has emerged as a promising treatment pattern for HCC patients with PVTT. Hence, we conducted this study to evaluate the efficacy and safety of HAIT combined with lenvatinib and PD-1 inhibitors for HCC patients with PVTT in a real-world setting. Additionally, we developed a nomogram model incorporating PVTT types to predict patients’ 6-month PFS and provide decision support for clinicians.
Materials and Methods
Study Population
This study included patients diagnosed with advanced HCC with PVTT between June 2020 and December 2023. These patients received either a treatment regimen consisting of HAIT in combination with lenvatinib and PD-1 inhibitors (H-L-P group) or a regimen involving lenvatinib plus PD-1 inhibitors (L-P group). The inclusion criteria were as follows: (1) HCC diagnosed radiologically or pathologically in accordance with the practice guidelines of the American Association for the Study of Liver Diseases (AASLD); (2) PVTT was diagnosed by intravenous contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI); (3) Child-Pugh stage A or B; (3) the score of Eastern Cooperative Oncology Group (ECOG) was within 1. The exclusion criteria included: (1) Patients with ruptured liver cancer; (2) Patients who received less than two cycles of treatment; (3) Patients who received a previous treatment; (4) Patients who had a history of other malignancies.
Treatment Procedures
HAIT included TACE or HAIC, the choice of HAIT was determined through communication between the patients and their attending physician. However, the general guidelines are as follows: TACE is not recommended for patients with the Vp4 type of PVTT, while HAIC is not advisable for patients with Child-Pugh stage B liver function. The basic procedures for HAIT were conducted as follows: Selinger’s technique was employed to percutaneously puncture the right femoral artery, a 5F catheter sheath was placed and matching catheters were then inserted into the celiac and superior mesenteric arteries. Digital subtraction angiography (DSA) was performed to ascertain the location, size, and feeding artery of the tumor. For TACE, emulsions (approximately 50 mg) of lipiodol and lobaplatin (at a ratio of 1:6) were administrated into the tumor’s feeding artery through a microcatheter for chemoembolization. For HAIC, after catheterizing the feeding artery of tumor, the microcatheter was connected to the arterial infusion pump, and patients were admitted to the ward for subsequent infusion chemotherapy. In our center, HAIC used the modified FOLFOX chemotherapy regimen: oxaliplatin, 85 mg/m2 for 2 hours on day 1; leucovorin, 200mg/m2 for 3 hours on day 1; 5-fluorouracil, 2400 mg/m2 for 46 hours. Every 3 to 4 weeks, TACE or HAIC was given again until the tumor progressed, or the toxicities were intolerable.
Lenvatinib and PD-1 inhibitors were administrated within 1 week depending on the recovery of liver function after the initial HAIT. Lenvatinib was taken orally daily (weight ≥ 60 kg: 12 mg; weight < 60 kg: 8 mg). PD-1 inhibitors (including camrelizumab, tislelizumab, pembrolizumab and sintilimab) were administered intravenously over 60 minutes at a dose of 200 mg every 3 weeks.
Data Collection and Follow Up
The data from the Laboratory, including alpha-fetoprotein (AFP), hepatitis B virus (HBV) load and liver function were recorded prior to the administration of initial HAIT. The data of the imaging, including tumor number and size, extrahepatic metastasis, and the type of PVTT were recorded through intravenous contrast-enhanced CT or MRI. The primary endpoint was PFS, which was defined as the duration from the admission to disease progression or death occurred from any cause. OS was defined as the duration from admission to death occurred from any cause. Tumor responses, including complete response (CR), partial response (PR), stable disease (SD) and progressive disease (PD), were evaluated every 2–3 cycles using the Modified Response Evaluation Criteria in Solid Tumors (mRECIST). The objective response rate (ORR) was defined as the proportion of patients who achieved CR or PR, and the disease control rate (DCR) was defined as the proportion of patients who achieved CR, PR or SD. Treatment-related adverse events (TRAEs) were evaluated by the National Cancer Institute Standard for Common Terminology for Adverse Events (version 5.0). The follow-up deadline was set for July, 2024.
Statistical Analyses
Statistical analyses were performed using the R software (version 4.4.2) and SPSS (version 26.0). Complete-case analysis was used to handle missing data. Categorical variables were analyzed by the chi-square (χ2) test and Fisher’s exact test. P values < 0.05 were considered to be statistically significant. 1:1 propensity score matching (PSM) was performed with a caliper width of 0.25. Covariates including age, sex, ECOG score, ALBI (Albumin-bilirubin) grade, Child-Pugh class, HBV load, AFP, tumor size, tumor number, PVTT, hepatic vein tumor thrombus (HVTT), tumor metastasis, and PD-1 inhibitors were used in the matching model. Univariate and multivariate analyses were based on Cox proportional analysis, factors with P values less than 0.1 in univariate analysis will be further included in multivariate analysis. Kaplan–Meier analysis and the Log rank test were employed to compare the outcomes of the two groups. The results of Cox regression analysis were used to construct nomogram model. Using the ROC curve to assess the prognostic accuracy of the nomogram. Calibration curve was used to illustrate the accuracy of the nomogram, while the clinical practicability was evaluated through analysis of the decision curve.
Results
Characteristics of Patients
Following the assessment of inclusion and exclusion criteria, 208 patients were enrolled in this study. Among them, 120 patients received HAIT combined with lenvatinib and PD-1 inhibitors (H-L-P group) and 88 patients received lenvatinib plus PD-1 inhibitors (L-P group). The screening process is illustrated in Figure 1. Detailed characteristics of patients before and after PSM were shown in Table 1. Most patients in both groups were male and had AFP levels ≥ 400 ng/mL, multiple lesions, and absence of HVTT. All patients had hepatitis B virus infection and PVTT. Twenty-six patients (12.5%) had vp1/2 type of PVTT and 182 patients (87.5%) had vp3/4 type of PVTT. Compared to the H-L-P group, metastasis was more frequently observed (p = 0.004) and the liver function was poorer (p = 0.049) in L-P group. Following a 1:1 PSM, the baseline characteristics between the two groups were well-matched.
 |
Table 1 Baseline Characteristics of Patients Before and After PSM |
 |
Figure 1 Flow chart of patient screening. |
Survival Outcomes and Tumor Response
The median follow-up time was 32 months. In the entire cohort, patients in the H-L-P group exhibited significantly longer median OS of 22 months (95% CI: 16.23–27.00) and median PFS of 10 months (95% CI: 8.20–12.00) compared to those in the L-P group, who had median OS of 12 months (95% CI: 10.00–15.00) and median PFS of 4 months (95% CI: 4.00–6.00). The H-L-P group showcased significantly higher OS rates at 6, 12, and 24 months (95.8%, 68.3%, 45.9%) compared to the L-P group (89.8%, 49.6%, 4.9%) (p < 0.001). Similarly, the H-L-P group showcased significantly higher PFS rates at 6, 12, and 24 months (70.8%, 38.2%, 27.2%) compared to the L-P group (26.1%, 6.2%, 3.1%) (p < 0.001).
After PSM, the OS and PFS of the H-L-P group were also longer than those in the L-P group. The median OS for the H-L-P group and L-P group were 19 months (95% CI: 14.10–21.00) and 14 months (95% CI: 11.00–15.00), while the median PFS was 10 months (95% CI: 8.00–12.00) and 4 months (95% CI: 4.00–6.00). Moreover, the H-L-P group also demonstrated superior OS rates at 6, 12, and 24 months (94.6%, 63.5%, 39.2%) compared to the L-P group (90.5%, 52.3%, 5.8%) (p < 0.001), and superior PFS rates at 6, 12, and 24 months (67.6%, 36.2%, 22.2%) compared to the L-P group (27.0%, 7.4%, 3.7%) (p < 0.001). Survival curves between the two groups before and after PSM were shown in Figure 2. In addition, subgroup analysis demonstrated that the H-L-P group resulted in trends of lower risk of progression and death compared to L-P group across nearly all subgroups (Figure 3).
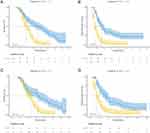 |
Figure 2 Survival analysis for OS and PFS between the two groups before PSM (A and B) and after PSM (C and D). |
 |
Figure 3 Subgroup analysis for OS (A) and PFS (B) between the two groups. |
The best tumor responses before and after PSM were shown in Table 2. Before PSM, the ORR for the H-L-P group and the L-P group was 37.5%, 18.2%, respectively (p < 0.001), while the DCR was 75.8%, 48.9% (p < 0.001). After matching, the H-L-P group also demonstrated superior ORR and DCR at 37.8% and 78.4%, respectively, compared to the L-P group at 16.2% and 47.3%.
 |
Table 2 Best Tumor Response Before and After PSM |
Univariate and Multivariate Analysis for Survival
The results of univariate and multivariate analysis for OS and PFS are shown in Table 3. Factors with P values less than 0.1 in univariate analysis will be further included in multivariate analysis. Univariate analysis revealed that AFP, tumor size, tumor number, type of PVTT, hepatic vein tumor thrombus (HVTT), metastasis, and treatment regimen were associated with OS. Ultimately, tumor size ≤ 10 cm, single tumor lesion, Vp1/2 type of PVTT, and receiving H-L-P treatment regimen were found to be strongly associated with favorable OS. Similarly, the same factors were identified as independent prognostic factors of PFS.
 |
Table 3 Univariate and Multivariate Analysis of Overall Survival and Progression-Free Survival |
Development of a Prognostic Nomogram Model
Based on the results of univariate and multivariate analyses, we constructed a prognostic nomogram model that incorporates AFP levels, tumor size, tumor number, PVTT types, presence of HVTT, presence of metastasis and treatment regimen to predict the 6-month PFS of HCC patients with PVTT in this study (Figure 4A). The ROC curve depicted in Figure 4B demonstrated the good performance of the nomogram in predicting 6-month PFS, and the AUC value at 6-month was 0.84 (95% CI: 0.78–0.90). Additionally, the calibration curves (Figure 4C) demonstrated good concordance between the predicted and observed outcomes. The decision curves in Figure 4D demonstrated the nomogram had great clinical application in predicting 6-month PFS.
Safety
The treatment-related adverse events (TRAEs) details were provided in Table 4. All TRAEs were controlled, and there were no treatment-related deaths. The three most prevalent TRAEs in the H-L-P group were elevated aspartate aminotransferase (AST), elevated alanine aminotransferase (ALT), and vomiting. Any grade of TRAEs, including abdominal pain (21.7% vs 9.1%, p = 0.015), nausea (34.2% vs 8.0%, p < 0.001), vomiting (37.5% vs 13.6%, p < 0.001), anorexia (27.5% vs 15.9%, p = 0.048), elevated ALT (45% vs 17.0%, p < 0.001), elevated AST (47.5% vs 27.3%, p = 0.003), and hyperbilirubinemia (23.3% vs 4.5%, p < 0.001), was more frequently reported in the H-L-P group. No significant differences were observed between the two groups in other TRAEs such as hypertension, fatigue, and pruritus. Additionally, grade 3 or 4 TRAEs were comparable between the H-L-P group and the L-P group.
 |
Table 4 Treatment-Related Adverse Events |
Discussion
PVTT in HCC patients has long been recognized as a prominent factor associated with unfavorable outcomes.5,21 There are notable disparities in the treatment strategies for PVTT between Eastern and Western countries. Systemic therapies, such as sorafenib and lenvatinib, are recommended as the first-line treatment option in Western countries.22,23 However, in addition to systemic therapies, Eastern countries emphasize that locoregional therapies (such as radiotherapy, TACE, and HAIC) can provide additional survival benefits for HCC patients with PVTT.24–26 In recent years, combining locoregional and systemic therapies has shown remarkable potential for treating advanced HCC.19,27 Hence, we investigated the efficacy and safety of HAIT in combination with lenvatinib and PD-1 inhibitors for HCC patients with PVTT in a real-world setting.
In our investigation, we utilized PSM to reduce the potential bias. After matching, we found that patients in the H-L-P group exhibited significantly better median OS (19 months vs 14 months, p < 0.001) and PFS (10 months vs 4 months, p < 0.001) compared to those in the L-P group. Additionally, the OS and PFS rates at 6, 12, 24 months were consistently higher in the H-L-P group than in the L-P group. Furthermore, the H-L-P group demonstrated superior ORR (37.8% vs 16.2%) and DCR (78.4% vs 47.3%) relative to the L-P group. Subgroup analyses also demonstrated that patients in the H-L-P group achieved better outcomes across most subgroups. A Phase II study demonstrated HAIC combined with camrelizumab and apatinib achieved a median PFS of 10.38 months in patients with advanced HCC, which is consistent with our findings. However, the ORR (77.1%) and DCR (97.1%) of the trial were higher than our study, which might be due to the different proportions of patients with PVTT. There were 87.84% of patients with vp3/4 type of PVTT in the H-L-P group in our study, but the phase II study only included 45.7% of patients who had vp3/4 type of PVTT.28
The excellent benefits of the triple treatment may be attributed to the potential synergistic interactions among HAIT, lenvatinib and PD-1 inhibitors. On the one hand, the local action of HAIT directly targets tumor and can boost the anti-tumor immune response by releasing tumor antigens.29 On the other hand, Lenvatinib not only inhibits tumor microvascular formation following HAIT but also remodels the tumor immune microenvironment, thereby enhancing the efficacy of PD-1 inhibitors.30,31 Furthermore, chemotherapy drugs in HAIT can induce immunogenic cell death in HCC, thereby synergizing with PD-1 inhibitors to enhance antitumor immunity.32
In this study, multivariate analyses demonstrated that treatment region and high tumor burden (such as tumor size > 10 cm, multiple tumor lesion, Vp3/4 type of PVTT) were significantly associated with poor survival of HCC patients with PVTT. The combination of HAIT, lenvatinib and PD-1 inhibitors was associated with favorable clinical outcomes, which aligns with the findings reported by Fu20 and Chen.33 However, the ORR and DCR in Fu’s research were higher than those in this study, which could potentially be attributed to the fact that their cohort also included 11% of patients with the vp0 type of PVTT, who may have a better treatment response. Based on the results of univariate and multivariate analyses, we developed a nomogram model to predict the 6-month PFS of HCC patients with PVTT. This nomogram model demonstrated excellent discrimination and calibration, as validated by the ROC and calibration curves. DCA curve indicated that the nomogram model possessed significant clinical application value. The survival rates for different types of PVTT can vary significantly, and patients with PVTT often present with complex clinical conditions.34 Therefore, emphasizing individual differences is essential for the effective management of PVTT. This model allows for personalized short-term PFS predictions based on patient’s specific condition, thereby providing support for clinical decision-making.
In terms of safety, we observed that the addition of HAIT was associated with an increased incidence of TRAEs. Digestive system symptoms (such as nausea and vomiting) and liver function impairment were more frequently reported in the H-L-P group than the L-P group. However, grade 3 or 4 TRAEs were comparable between the two groups. In addition, all TRAEs were controlled after appropriate therapeutic interventions, and there were no treatment-related deaths. Another study also reported that the combination therapy was associated with an increased incidence of abdominal pain and abnormal elevation of liver enzymes.35 Therefore, we should attach great importance to the management during the HAIT and enhance both symptomatic treatment and liver-protective measures.
This study has some limitations. Firstly, this is a retrospective, single-center study. A prospective multi-center study is needed to verify the reliability of the conclusion. Secondly, our study included a variety of PD-1 inhibitors and two types of HAIT, which may potentially influence the consistency of the results. Thirdly, the nomogram model established in this study has only undergone internal validation and lacks effective external validation. In addition, the relatively small sample size and the limited duration of the follow-up period in our study might potentially restrict the generalizability of the findings.
Conclusion
In conclusion, our study demonstrated that combining HAIT with lenvatinib and PD-1 inhibitors was a safe and promising treatment strategy for HCC patients with PVTT, and the development of the 6-month PFS nomogram model may provide support for personalized treatment and clinical decision-making. These findings may support the clinical integration of HAIT in the multidisciplinary management of advanced HCC with PVTT. However, more large-scale randomized controlled trials are warranted to validate the results.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval and Consent to Participate
This study was approved by the institutional ethics committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology (TJ-IRB202404110) and complied with the Declaration of Helsinki. Written informed consents were exempted because of retrospective analysis. All patients’ personal data are strictly confidential.
Disclosure
The authors report no conflict of interest in this work.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Lu J, Zhang XP, Zhong BY, et al. Management of patients with hepatocellular carcinoma and portal vein tumour thrombosis: comparing east and west. Lancet Gastroenterol Hepatol. 2019;4(9):721–730. doi:10.1016/S2468-1253(19)30178-5
3. Qiu G, Xie K, Jin Z, et al. The multidisciplinary management of hepatocellular carcinoma with portal vein tumor thrombus. Biosci Trends. 2021;15(3):148–154. doi:10.5582/bst.2021.01173
4. Li YK, Wu S, YS W, et al. Portal venous and hepatic arterial coefficients predict post-hepatectomy overall and recurrence-free survival in patients with hepatocellular carcinoma: a retrospective study. J Hepatocell Carcinoma. 2024;11:1389–1402. doi:10.2147/JHC.S462168
5. Khan AR, Wei X, Xu X. Portal vein tumor thrombosis and hepatocellular carcinoma - the changing tides. J Hepatocell Carcinoma. 2021;8:1089–1115. doi:10.2147/JHC.S318070
6. Reig M, Forner A, Rimola J, et al. BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol. 2022;76(3):681–693. doi:10.1016/j.jhep.2021.11.018
7. Finn RS, Qin S, Ikeda M, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382(20):1894–1905. doi:10.1056/NEJMoa1915745
8. Catalano M, Casadei-Gardini A, Vannini G, et al. Lenvatinib: established and promising drug for the treatment of advanced hepatocellular carcinoma. Expert Rev Clin Pharmacol. 2021;14(11):1353–1365. doi:10.1080/17512433.2021.1958674
9. Yi C, Chen L, Lin Z, et al. Lenvatinib targets FGF receptor 4 to enhance antitumor immune response of anti-programmed cell death-1 in HCC. Hepatology. 2021;74(5):2544–2560. doi:10.1002/hep.31921
10. Cappuyns S, Corbett V, Yarchoan M, Finn RS, Llovet JM. Critical appraisal of guideline recommendations on systemic therapies for advanced hepatocellular carcinoma: a review. JAMA Oncol. 2024;10(3):395–404. doi:10.1001/jamaoncol.2023.2677
11. Finn RS, Galle PR, Ducreux M, et al. Efficacy and safety of atezolizumab plus bevacizumab versus sorafenib in hepatocellular carcinoma with main trunk and/or contralateral portal vein invasion in IMbrave150. Liver Cancer. 2024;13(6):655–668. doi:10.1159/000539897
12. Finn RS, Ikeda M, Zhu AX, et al. Phase Ib study of lenvatinib plus pembrolizumab in patients with unresectable hepatocellular carcinoma. J Clin Oncol. 2020;38(26):2960–2970. doi:10.1200/JCO.20.00808
13. Sun J, Guo R, Bi X, et al. Guidelines for diagnosis and treatment of hepatocellular carcinoma with portal vein tumor thrombus in China (2021 edition). Liver Cancer. 2022;11(4):315–328. doi:10.1159/000523997
14. Iwamoto H, Shimose S, Shirono T, Niizeki T, Kawaguchi T. Hepatic arterial infusion chemotherapy for advanced hepatocellular carcinoma in the era of chemo-diversity. Clin Mol Hepatol. 2023;29(3):593–604. doi:10.3350/cmh.2022.0391
15. Cheu JW, Wong CC. Mechanistic rationales guiding combination hepatocellular carcinoma therapies involving immune checkpoint inhibitors. Hepatology. 2021;74(4):2264–2276. doi:10.1002/hep.31840
16. Montasser A, Beaufrere A, Cauchy F, et al. Transarterial chemoembolisation enhances programmed death-1 and programmed death-ligand 1 expression in hepatocellular carcinoma. Histopathology. 2021;79(1):36–46. doi:10.1111/his.14317
17. Zhang JX, Cheng Y, Wei J, et al. Transarterial chemoembolization combined with tyrosine kinase inhibitors plus immune checkpoint inhibitors versus tyrosine kinase inhibitors plus immune checkpoint inhibitors in unresectable hepatocellular carcinoma with first- or lower-order portal vein tumor thrombosis. Cardiovasc Intervent Radiol. 2024;47(6):751–761. doi:10.1007/s00270-024-03724-x
18. Li Y, Guo J, Liu W, et al. Hepatic artery infusion chemotherapy combined with camrelizumab plus rivoceranib for hepatocellular carcinoma with portal vein tumor thrombosis: a multicenter propensity score-matching analysis. Hepatol Int. 2024;18(4):1286–1298. doi:10.1007/s12072-024-10672-8
19. Zhong BY, Fan W, Guan JJ, et al. Combination locoregional and systemic therapies in hepatocellular carcinoma. Lancet Gastroenterol Hepatol. 2025;10(4):369–386. doi:10.1016/S2468-1253(24)00247-4
20. Fu S, Xu Y, Mao Y, et al. Hepatic arterial infusion chemotherapy, lenvatinib plus programmed cell death protein-1 inhibitors: a promising treatment approach for high-burden hepatocellular carcinoma. Cancer Med. 2024;13(9):e7105. doi:10.1002/cam4.7105
21. Li J, Quan B, Liu W, et al. Real-world study of hepatic artery infusion chemotherapy combined with anti-PD-1 immunotherapy for hepatocellular carcinoma patients with portal vein tumor thrombus. Ther Adv Med Oncol. 2024;16:17588359241231252. doi:10.1177/17588359241231252
22. Omata M, Cheng AL, Kokudo N, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int. 2017;11(4):317–370. doi:10.1007/s12072-017-9799-9
23. Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American association for the study of liver diseases. Hepatology. 2018;68(2):723–750. doi:10.1002/hep.29913
24. Cheng S, Chen M, Cai J, et al. Chinese expert consensus on multidisciplinary diagnosis and treatment of hepatocellular carcinoma with portal vein tumor thrombus (2018 edition). Liver Cancer. 2020;9(1):28–40. doi:10.1159/000503685
25. Kudo M, Kawamura Y, Hasegawa K, et al. Management of hepatocellular carcinoma in Japan: JSH consensus statements and recommendations 2021 update. Liver Cancer. 2021;10(3):181–223. doi:10.1159/000514174
26. Ji X, Zhang A, Duan X, Wang Q. Stereotactic body radiotherapy versus lenvatinib for hepatocellular carcinoma with portal vein tumor thrombosis: a propensity matching score analysis. Radiat Oncol. 2024;19(1):143. doi:10.1186/s13014-024-02527-1
27. Wang QB, Li J, Zhang ZJ, et al. The effectiveness and safety of therapies for hepatocellular carcinoma with tumor thrombus in the hepatic vein, inferior vena cave and/or right atrium: a systematic review and single-arm meta-analysis. Expert Rev Anticancer Ther. 2025;25(5):561–570. doi:10.1080/14737140.2025.2489651
28. Zhang TQ, Geng ZJ, Zuo MX, et al. Camrelizumab (a PD-1 inhibitor) plus apatinib (an VEGFR-2 inhibitor) and hepatic artery infusion chemotherapy for hepatocellular carcinoma in Barcelona Clinic Liver Cancer stage C (TRIPLET): a phase II study. Signal Transduct Target Ther. 2023;8(1):413. doi:10.1038/s41392-023-01663-6
29. Llovet JM, De Baere T, Kulik L, et al. Locoregional therapies in the era of molecular and immune treatments for hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol. 2021;18(5):293–313. doi:10.1038/s41575-020-00395-0
30. Chen YH, Dai SY, Cheng CS, Chen LY. Lenvatinib and immune-checkpoint inhibitors in hepatocellular carcinoma: mechanistic insights, clinical efficacy, and future perspectives. J Hematol Oncol. 2024;17(1). doi:10.1186/s13045-024-01647-1
31. Tachiiri T, Nishiofuku H, Maeda S, et al. Vascular normalization caused by short-term lenvatinib could enhance transarterial chemoembolization in hepatocellular carcinoma. Curr Oncol. 2023;30(5):4779–4786. doi:10.3390/curroncol30050360
32. Zhu H, Shan Y, Ge K, Lu J, Kong W, Jia C. Oxaliplatin induces immunogenic cell death in hepatocellular carcinoma cells and synergizes with immune checkpoint blockade therapy. Cell Oncol Dordr. 2020;43(6):1203–1214. doi:10.1007/s13402-020-00552-2
33. Chen S, Shi F, Wu ZQ, et al. Hepatic arterial infusion chemotherapy plus lenvatinib and tislelizumab with or without transhepatic arterial embolization for unresectable hepatocellular carcinoma with portal vein tumor thrombus and high tumor burden: a multicenter retrospective study. J Hepatocell Carcino. 2023;10:1209–1222. doi:10.2147/JHC.S417550
34. Yu SJ, Kim YJ. Effective treatment strategies other than sorafenib for the patients with advanced hepatocellular carcinoma invading portal vein. World J Hepatol. 2015;7(11):1553–1561. doi:10.4254/wjh.v7.i11.1553
35. Fu Y, Peng W, Zhang W, et al. Induction therapy with hepatic arterial infusion chemotherapy enhances the efficacy of lenvatinib and pd1 inhibitors in treating hepatocellular carcinoma patients with portal vein tumor thrombosis. J Gastroenterol. 2023;58(4):413–424. doi:10.1007/s00535-023-01976-x
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Comparison of the Efficacy and Safety of Transarterial Chemoembolization with or without Lenvatinib for Unresectable Hepatocellular Carcinoma: A Retrospective Propensity Score–Matched Analysis
Chen YX, Zhang JX, Zhou CG, Liu J, Liu S, Shi HB, Zu QQ
Journal of Hepatocellular Carcinoma 2022, 9:685-694
Published Date: 1 August 2022
Feasibility and Tolerability of Lenvatinib, Plus PD-1 Blockades for Patients with Unresectable Hepatocellular Carcinoma: A Retrospective Exploratory Study
Jia M, Jia JK, Xu J, Xue HZ
Cancer Management and Research 2022, 14:2625-2638
Published Date: 2 September 2022
Significance of Physical Status and Liver Function Reserve for Outcome of Patients with Advanced Hepatocellular Carcinoma Receiving Lenvatinib Treatment
Chan KM, Lai Y, Hung HC, Lee JC, Cheng CH, Wang YC, Wu TH, Lee CF, Wu TJ, Chou HS, Wang CT, Chai PM, Lien HY, Lee WC
Journal of Hepatocellular Carcinoma 2023, 10:281-290
Published Date: 18 February 2023
Lenvatinib Induces Immunogenic Cell Death and Triggers Toll-Like Receptor-3/4 Ligands in Hepatocellular Carcinoma

Zhou C, Yang ZF, Sun BY, Yi Y, Wang Z, Zhou J, Fan J, Gan W, Ren N, Qiu SJ
Journal of Hepatocellular Carcinoma 2023, 10:697-712
Published Date: 24 April 2023
Application and Resistance Mechanisms of Lenvatinib in Patients with Advanced Hepatocellular Carcinoma
Tao M, Han J, Shi J, Liao H, Wen K, Wang W, Mui S, Li H, Yan Y, Xiao Z
Journal of Hepatocellular Carcinoma 2023, 10:1069-1083
Published Date: 10 July 2023


