Back to Journals » Clinical Ophthalmology » Volume 19
Comparison of Stereoacuity Across Distances in Bilateral Intraocular Lens Implantation: Monofocal versus Diffractive Multifocal Lenses
Authors Ohashi T , Fujiya A, Yoshida M, Kojima T
Received 9 April 2025
Accepted for publication 4 July 2025
Published 16 July 2025 Volume 2025:19 Pages 2325—2332
DOI https://doi.org/10.2147/OPTH.S527617
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Tsutomu Ohashi,1 Akio Fujiya,1 Maiko Yoshida,1 Takashi Kojima2
1Ohashi Eye Center, Sapporo, Japan; 2Nagoya Eye Clinic, Nagoya, Japan
Correspondence: Tsutomu Ohashi, Ohashi Eye Center, Kita 1-1 Hondori 6, Shiroishi, Sapporo, 003-0027, Japan, Tel +81-11-864-4656, Fax +81-11-864-2344, Email [email protected]
Purpose: To evaluate stereopsis at various distances after bilateral implantation of multifocal and monofocal intraocular lenses (IOLs).
Patients and Methods: This study included 173 patients who underwent cataract surgery, with 70 receiving bilateral multifocal and 103 receiving bilateral monofocal IOLs. Stereoacuity was assessed without correction in the multifocal group and with correction in the monofocal group at far, intermediate, and near distances. Age-matched comparisons were conducted as the mean age was low in the multifocal group. Stereoacuity was assessed at 0.3, 0.5, 0.7, 3, and 5 m using a Binoptometer 4P.
Results: Stereoacuity was significantly better in the multifocal group than in the monofocal group at all distances (p < 0.05), except at 0.3 and 5 m after age matching. The proportion of patients achieving 100 arcsec or better was significantly higher in the multifocal group than in the multifocal group at all distances except 0.3 m (p < 0.05). Additionally, significant differences were noted only at 0.7 m after age matching (p < 0.05). The proportions of patients unable to identify 600 arcsec in the multifocal, monofocal, and age-matched monofocal groups were 3%, 11%, and 11% at 0.3 m; 0%, 9%, and 14% at 0.5 m; 0%, 9%, and 8% at 0.7 m; 0%, 5%, and 3% at 3 m; and 0%, 6%, and 6% at 5 m, respectively. After age matching, poor stereopsis was significantly reduced in the multifocal group at 0.5 m (p < 0.05) but not at 0.7 m.
Conclusion: Patients with bilateral implanted multifocal IOLs exhibited superior stereopsis across various distances than those with bilateral monofocal IOLs. Additionally, fewer patients with multifocal IOLs experienced poor stereopsis. These results suggest that multifocal IOLs may help patients in maintaining stereopsis by facilitating focus on multiple points from far to near distances daily.
Keywords: stereopsis, multifocal IOLs, monofocal IOLs, cataract surgery
Introduction
Multifocal intraocular lenses (IOLs) reportedly provide optimal vision at far, intermediate, and near distances, with a significantly higher proportion of patients achieving spectacle independence compared to those with bilateral monofocal IOLs.1–3 However, compared to monofocal IOLs, multifocal IOLs also present several visual function challenges, such as waxy vision, dysphotopsia, and reduced contrast sensitivity.1 These trade-offs may influence binocular visual function, particularly stereopsis, which is the highest-level function of binocular vision. Previous investigations have assessed stereopsis in patients with unilateral IOL implantation.4–6 However, few comparative studies have evaluated stereopsis in patients with bilateral IOL implantation, specifically comparing outcomes between those with bilateral monofocal IOLs and those with bilateral multifocal IOLs.7,8
One factor contributing to decreased stereopsis is reduced contrast sensitivity.9 Since multifocal IOLs tend to produce lower contrast sensitivity than monofocal IOLs, it is reasonable to hypothesize that multifocal IOLs could result in diminished stereopsis. However, studies have shown conflicting results. Some have reported that multifocal IOLs provide equivalent or even superior stereopsis compared to monofocal IOLs, particularly at near distances.7,8 Despite these findings, the current literature is limited in scope, often focusing solely on near stereopsis. Consequently, the effect of IOL type on stereopsis across a range of distances remains unclear.
Given the importance of stereopsis in daily visual function, these differences have meaningful clinical implications for IOL selection, particularly for patients with visual demands requiring robust depth perception, such as those engaging in daily tasks or precise work. Providing evidence on the impact of each IOL type on stereoacuity may help guide clinical decision-making and improve patient counseling.
In this study, we aimed to systematically evaluate stereopsis at far, intermediate, and near distances in patients with bilaterally implanted multifocal IOLs and compare the results with those of patients with bilaterally implanted monofocal IOLs.
Materials and Methods
Patients
This retrospective study included 173 patients who underwent bilateral cataract extraction and IOL implantation between May 2007 and March 2022. All surgeries were performed at the Ohashi Eye Center in Sapporo, Japan. The inclusion criteria were as follows: (i) absence of ocular pathologies affecting vision, other than cataract; and (ii) a distance best spectacle-corrected visual acuity (BSCVA) of 20/20 or better (logMAR 0) in either eye. Among the 173 patients, 70 received bilateral multifocal IOL implants, with a targeted refraction of emmetropia. The remaining 103 patients received bilateral monofocal IOL implants; among these, the targeted refraction was for far distance in 62 eyes, intermediate distance in 12 eyes, and near distance in 29 eyes. All patients visited our clinic for follow-up between November 2019 and March 2022. The mean ages of the multifocal and monofocal groups were 64.3±8.75 and 73.3±7.76 years, respectively. Considering that the mean age of the monofocal group was greater than that of the multifocal group, we selected 36 patients under 70 years of age to form the age-matched monofocal group (mean age: 64.3±5.16 years) and compared the stereoacuity of this group with that of the multifocal group (mean age: 64.3±8.75 years).
The study adhered to the tenets of the Declaration of Helsinki. The study protocol was approved by Chukyo Medical’s ethical review board (UMIN-Clinical Trials Registry ID: UMIN000054667). The opt-out method of consent was used.
Surgical Technique/ IOLs
Phacoemulsification was performed through a clear temporal corneal incision ranging from 2.4 mm to 2.8 mm. All IOLs were placed in capsular bags. Patients in the multifocal group were implanted with diffractive aspheric trifocal lenses: AcrySof IQ PanOptix (TFNT00, Alcon Laboratories, Inc.) or AcrySof IQ PanOptix toric IOL (TFNT30-60, Alcon Laboratories, Inc). Patients in the monofocal group were implanted with Vivinex XY1 (Hoya Surgical Optics, Inc.), Clareon CNA0T0 (Alcon Laboratories, Inc.), AF-1 YA-60BBR (Hoya Surgical Optics, Inc.), TECNIS 1-Piece VB ZCB00V (Johnson & Johnson), AcrySof IQ TORIC (SN6AT3-7, Alcon Laboratories, Inc.), or Vivinex XY1A toric IOL (Hoya Surgical Optics, Inc). To provide further clarity regarding the composition of the monofocal IOL group, details on the specific IOL models, manufacturers, and their available optical and material properties are summarized in Supplementary Table 1. When astigmatism correction was required, toric IOLs were implanted based on online TORIC power calculations.
Statistical Analysis
All statistical analyses were performed using EZR10 (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (R Foundation for Statistical Computing, Vienna, Austria). It is a modified version of the R commander designed to incorporate statistical functions frequently used in biostatistics. The Kolmogorov–Smirnov or Shapiro–Wilk test was used to evaluate the normality of data distribution. The Mann–Whitney U-test was used to compare uncorrected and corrected visual acuity (VA), spherical power, cylinder power, spherical equivalent power (SE), and stereoacuity between the multifocal and monofocal groups as well as between the multifocal and age-matched monofocal groups. The chi-square test was used to compare the proportion of patients with normal stereopsis and those with poor stereopsis between the groups. The Fisher’s exact test was used to compare the proportion of patients who could not identify the right cross at the 600 seconds of arc (arcsec) threshold at one or more distances between the groups. Statistical significance was set at p<0.05.
Stereopsis Measurement
Stereopsis was evaluated at five different distances: 5 m, 3 m, 0.7 m, 0.5 m, and 0.3 m, using the Binoptometer® 4P (OCULUS, Inc., Arlington, WA). This device employs an LCD shutter system to present slightly different visual stimuli to each eye, allowing for binocular stereopsis testing. It features a continuously adjustable optical system that enables testing across a wide range of distances—from 30 cm to infinity. The brightness of the examination field was approximately 300 cd/m². Stereoacuity was measured in arcseconds using the following threshold levels: 600, 400, 200, 100, 80, 60, 45, 30, and 15 arcsec.
The examination started at the 600 arcsec disparity level. In each step, five crosses were displayed, one of which was designed to stand out from the other four. Patients were instructed to identify the standout cross. If they responded correctly, the test proceeded to the next finer level. This process continued until the patient failed to identify the standout cross. If the patient could not identify the correct cross at the 600 arcsec level, stereoacuity was recorded as 700 arcsec, indicating poor stereopsis. Stereoacuity of 100 arcsec or better (≤100 arcsec) was defined as normal.
Eyes in the multifocal group were assessed without correction, whereas those in the monofocal group were corrected for both far- and near-distance vision. Far-distance vision was corrected using the best possible correction based on postoperative manifest refraction, and the near-distance vision was corrected with the addition of +3.0 D at 0.3 m, +2.0 D at 0.5 m, and +1.5 D at 0.7 m using the Binoptometer 4P’s built-in lens addition function.
Results
Table 1 shows the patients’ characteristics. The mean time interval between surgery and postoperative stereoacuity measurements for the multifocal and monofocal groups was 221±183 and 703±1047 days, respectively.
 |
Table 1 Postoperative Results |
The mean stereoacuity values of the multifocal, monofocal, and age-matched monofocal groups were 164±180 arcsec, 249±241 arcsec, and 249±247 arcsec at 0.3 m, respectively; 136±154 arcsec, 267±240 arcsec, and 260±259 arcsec at 0.5 m, respectively; 128±158 arcsec, 258±236 arcsec, and 249±245 arcsec at 0.7 m, respectively; 126±148 arcsec, 226±216 arcsec, and 222±223 arcsec at 3 m, respectively; and 126±130 arcsec, 219±219 arcsec, and 223±229 arcsec at 5 m, respectively. The multifocal group demonstrated significantly better stereoacuity than the monofocal group at every distance (p<0.05), but when compared with the age-matched monofocal group, the differences were not significant at 0.3 m and 5 m (Figure 1).
 |
Figure 1 Mean stereoacuity values in the multifocal, monofocal, and age-matched monofocal groups. *P<0.05, **P<0.01. |
The proportions of patients who achieved normal stereopsis (≤100 arcsec) in the multifocal, monofocal, and age-matched monofocal groups were 69%, 58%, and 61% at 0.3 m, respectively; 77%, 52%, and 61% at 0.5 m, respectively; 81%, 54%, and 61% at 0.7 m, respectively; 80%, 60%, and 64% at 3 m, respectively; and 80%, 62%, and 64% at 5 m, respectively. The proportion of patients with normal stereopsis was significantly higher in the multifocal group than that in the monofocal group at every distance except at 0.3 m (p<0.05). However, when compared with the age-matched monofocal group, the differences were not significant at 0.3 m, 0.5 m, 3 m, and 5 m (Figure 2).
 |
Figure 2 Proportions of patients with normal stereopsis (100 arcsec or better) in the multifocal, monofocal, and age-matched monofocal groups. *P<0.05, **P<0.01. |
The numbers of patients unable to identify the correct cross at the 600 arcsec threshold (indicating poor stereopsis) in the multifocal, monofocal, and age-matched monofocal groups were two (3%), eleven (11%), and four (11%) at 0.3 m, respectively; zero (0%), nine (9%), and five (14%) at 0.5 m, respectively; zero (0%), nine (9%), and three (8%) at 0.7 m, respectively; zero (0%), five (5%), and one (3%) at 3 m, respectively; and zero (0%), six (6%), and two (6%) at 5 m, respectively. The multifocal group had a significantly lower proportion of patients with poor stereopsis than in the monofocal group at 0.5 m and 0.7 m (p<0.05), but when compared with the age-matched monofocal group, the differences were not significant at 0.3 m, 0.7 m, 3 m, and 5 m (Figure 3). The numbers of patients who could not identify the correct cross at the 600 arcsec threshold at one or more distances were two (3%) in the multifocal group, 19 (18%) in the monofocal group, and eight (22%) in the age-matched monofocal group. The multifocal group had significantly fewer patients who could not identify the correct cross at the 600 arcsec threshold compared to the monofocal and age-matched monofocal groups (p<0.01).
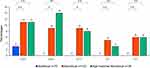 |
Figure 3 Proportions of patients with poor stereopsis (700 arcsec) in the multifocal, monofocal, and age-matched monofocal groups. *P<0.05, **P<0.01. |
Discussion
Previous studies have posited that stereopsis decreases with age due to reduced contrast sensitivity and neurophysiological factors;11,12 however, the exact mechanism remains unknown. We hypothesized that a decrease in contrast sensitivity, particularly following multifocal IOL implantation, as well as the multifocal nature of these lenses might adversely affect stereopsis in binocular vision. Therefore, we compared the stereoacuity between the multifocal and monofocal groups, which unexpectedly revealed that the multifocal group exhibited better stereoacuity than that of the monofocal group at all distances. Considering the influence of age on stereopsis, we also compared the stereoacuity between the multifocal and age-matched monofocal groups and found no significant differences between them at 0.3 m and 5 m. Additionally, the number of patients with normal stereopsis was comparable between the groups. In contrast, no patient in the multifocal group had poor stereopsis across most distances, whereas the monofocal group had nearly 10 patients with poor stereopsis at all tested distances. This represents the largest difference observed between the two groups. These findings suggest that the stereoacuity of older patients presenting with poor stereopsis in the monofocal group may have influenced the overall mean stereoacuity.
Oki et al7 compared near stereoacuity between patients bilaterally implanted with monofocal IOLs and multifocal IOLs and reported that the multifocal group without correction exhibited significantly better stereoacuity compared to the monofocal group without correction. They also noted that the multifocal group contained a slightly higher proportion of patients with a stereoacuity of 40 arcsec or better when the eyes were corrected for far distance, and the eyes of the monofocal group were corrected for near distance. They concluded that the multifocal and monofocal groups were comparable in terms of near stereoacuity. Arens et al8 also evaluated near stereoacuity following bilateral implantation of monofocal and multifocal IOLs, reporting that, without correction, the multifocal group with target emmetropia exhibited superior stereoacuity relative to that of the monofocal group with slight myopia. Our results showed that the multifocal group without correction had significantly better stereoacuity than that of the monofocal group.
Häring et al13 speculated that the Stiles–Crawford effect14 could elucidate the phenomenon whereby eyes implanted with multifocal IOLs achieved favorable stereoacuity despite the formation of multiple simultaneous retinal images. The multifocality of these IOLs may operate in a manner analogous to that of natural human lenses, as opposed to monofocal IOLs, which generate an unnaturally clear image at a single focal point. Ferrer-Blasco et al15 also reported no significant differences in stereoacuity prior to and following the implantation of multifocal IOLs. In this study, a considerably lower incidence of poor stereopsis was observed in the multifocal group than in the monofocal group. Given that monofocal IOLs possess a singular focal point, it is reasonable to presume that patients with monofocal IOLs concentrate solely on that focal point postoperatively, potentially contributing to a reduction in pseudo-accommodation and stereopsis. In contrast, multifocal IOLs provide three focal points at far, intermediate, and near distances, allowing patients implanted with these IOLs to continuously select the preferred focal point among the three options. This daily accommodation to focus at varying distances may assist in the maintenance of stereopsis.
In this study, stereoacuity was measured with correction in the monofocal group and without correction in the multifocal group. Patients in the monofocal group were anticipated to perceive each distance more clearly than those in the multifocal group; however, their stereoacuity did not match that of the patients in the multifocal group. The Binoptometer’s plus lens function was used to add diopters for distances of 0.3 m, 0.5 m, and 0.7 m, which may have led to inaccuracies in correction.
Clinically, we have often observed a higher prevalence of exotropia with age among outpatients. Hoshikawa et al16 conducted a 5-year follow-up study of ocular deviation and stereopsis and reported that a higher incidence of ocular deviation transitioning from exophoria to intermittent strabismus or exotropia was observed postoperatively in patients with a preoperative near exophoria angle exceeding 12 PD, along with a decline in near stereopsis 2 years post-surgery. This suggests that the gradual decline in stereopsis with age may be attributable to such ocular deviation shifts as well as a decrease in neural function in the brain.
Several limitations should be acknowledged. One concern relates to the measurement methodology. Numerous previous studies on stereopsis have utilized different tests to assess far and near stereoacuity, such as the Distance Randot test and the Titmus test, potentially introducing methodological inconsistencies. In this study, we employed the Binoptometer 4P to measure stereoacuity across all distances, thereby mitigating inconsistencies associated with using different tools for different distances. Mengdi et al17 reported that the Binoptometer 4P exhibited moderate consistency with the Titmus test and demonstrated sufficient reliability; however, relatively few studies have utilized this device,18–20 and normative data remain limited. Additionally, although the Binoptometer 4P’s plus lens function was used to add diopters for distances of 0.3 m, 0.5 m, and 0.7 m in the monofocal group, corrected visual acuity at each test distance was not verified. Thus, it remains unclear whether all patients achieved optimal clarity, which may have affected stereoacuity outcomes.
Another limitation is the variability in follow-up intervals between the groups. The monofocal group had a longer average follow-up period, which may have allowed more time for visual stabilization but also introduced subtle ocular changes that could influence stereoacuity.
A further limitation concerns the composition of the monofocal group, which included a variety of IOL models; however, all were single-focus designs without multifocal or extended depth-of-focus features. Despite differences in model and brand, these lenses were similar in their optical function, and all patients achieved a corrected distance visual acuity of 20/20 or better. In addition, stereoacuity was measured under distance-corrected conditions for each test distance, which minimized the influence of postoperative refractive targets. Nevertheless, the heterogeneity of the monofocal IOL group remains a limitation, and findings should be interpreted with caution. Future studies with more homogeneous control groups are needed to confirm these findings.
Conclusion
In conclusion, patients with bilateral implantation of multifocal IOLs demonstrated superior stereoacuity than those with bilateral implantation of monofocal IOLs. However, the proportion of patients exhibiting normal stereopsis was comparably high in both groups after age matching. The most significant difference was that fewer patients with multifocal IOLs exhibited poorer stereopsis compared to those with monofocal IOLs. These findings suggest that multifocal IOLs may aid in the maintenance of stereopsis by allowing patients to focus on multiple points across far to near distances on a daily basis. However, given the heterogeneity of the monofocal IOL group, further research using more uniform lens types is necessary to validate these findings.
Abbreviations
Arcsec, seconds of arc; IOLs, intraocular lenses; BSCVA, best spectacle-corrected visual acuity; logMAR, logarithm of the minimum angle of resolution; SE, spherical equivalent power; VA, visual acuity.
Data Sharing Statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval and Informed Consent
This study was approved by the ethical review board (Chukyo Medical Ethical Board, UMIN-Clinical Trials Registry ID: 000054667) and was conducted in accordance with the Declaration of Helsinki. All surgeries were performed at the Ohashi Eye Center in Sapporo, Japan. An opt-out method was used as an alternative to informed consent.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
Dr. Kojima declares personal fees from STAAR Surgical, Santen Pharmaceutical, SEED, HOYA, Ophtecs, Johnson & Johnson, and Alcon, outside of the submitted work. This organization had no role in the design or conduct of this research. All other authors have no conflicts of interest to declare.
References
1. Modi S, Lehmann R, Maxwell A, et al. Visual and patient-reported outcomes of a diffractive trifocal intraocular lens compared with those of a monofocal intraocular lens. Ophthalmology. 2021;128(2):197–207. doi:10.1016/j.ophtha.2020.07.015
2. Blehm C, Potvin R. Reported patient satisfaction and spectacle independence following bilateral implantation of the PanOptix® Trifocal intraocular lens. Clin Ophthalmol. 2021;15:2907–2912. doi:10.2147/OPTH.S323337
3. Kohnen T, Lwowski C, Hinzelmann L, et al. Presbyopia correction in astigmatic eyes using a toric trifocal intraocular lens with quadrifocal technology. J Refract Surg. 2020;36(10):638–644. doi:10.3928/1081597X-20200729-04
4. Jacobi PC, Dietlein TS, Lüke C, Jacobi FK. Multifocal intraocular lens implantation in prepresbyopic patients with unilateral cataract. Ophthalmology. 2002;109(4):680–686. doi:10.1016/S0161-6420(01)01029-6
5. Mesci C, Erbil HH, Olgun A, Yaylali SA. Visual performances with monofocal, accommodating, and multifocal intraocular lenses in patients with unilateral cataract. Am J Ophthalmol. 2010;150(5):609–618. doi:10.1016/j.ajo.2010.05.023
6. Hayashi K, Manabe S, Yoshimura K, Hirata A. Binocular visual function with a diffractive multifocal intraocular lens in patients with unilateral cataract. J Cataract Refract Surg. 2013;39(6):851–858. doi:10.1016/j.jcrs.2013.01.030
7. Oki S, Bissen-Miyajima H, Nakamura K, Yoshino M, Saito E. Stereopsis following implantation of diffractive multifocal intraocular lens. IOL & RS. 2009;23(3):371–374. In Japanese.
8. Arens B, Freudenthaler N, Quentin CD. Binocular function after bilateral implantation of monofocal and refractive multifocal intraocular lenses. J Cataract Refract Surg. 1999;25(3):399–404. doi:10.1016/S0886-3350(99)80089-3
9. Legge GE, Gu YC. Stereopsis and contrast. Vision Res. 1989;29(8):989–1004. doi:10.1016/0042-6989(89)90114-4
10. Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–458. doi:10.1038/bmt.2012.244
11. Song Y, Wang X, Liao M, Baldwin AS, Liu L. Binocular function in the aging visual system: fusion, suppression, and stereoacuity. Front Neurosci. 2024;18:1360619. doi:10.3389/fnins.2024.1360619
12. Wright LA, Wormald RP. Stereopsis and ageing. Eye. 1992;6(Pt 5):473–476. doi:10.1038/eye.1992.100
13. Häring G, Gronemeyer A, Hedderich J, de Decker W. Stereoacuity and aniseikonia after unilateral and bilateral implantation of the array refractive multifocal intraocular lens. J Cataract Refract Surg. 1999;25(8):1151–1156. doi:10.1016/S0886-3350(99)00136-4
14. Stiles WS, Crawford BH. The luminous efficiency of rays entering the eye pupil at different points. Proc R Soc Lond B. 1933;112(778):428–450.
15. Ferrer-Blasco T, Montés-Micó R, Cerviño A, Alfonso JF, González-Méijome JM. Stereoacuity after refractive lens exchange with AcrySof ReSTOR intraocular lens implantation. J Refract Surg. 2009;25(11):1000–1004. doi:10.3928/1081597X-20091016-05
16. Hoshikawa R, Ito M, Shimizu K, Ishikawa H, Amano R. Five-year follow-up of ocular deviation in bilaterally pseudophakic patients. Strabismus. 2013;21(2):110–115. doi:10.3109/09273972.2013.786734
17. Li MD, Wang Y, Zhao XH, et al. Application of binoptometer in stereoscopic screening. Rec Adv Ophthalmol. 2020;40(4):336–339. Article in Chinese.
18. Bai Z, Nie D, Zhang J, et al. Visual function assessment of posterior-chamber phakic implantable collamer lenses with a central port. Ann Transl Med. 2022;10(4):194. doi:10.21037/atm-22-107
19. Ochi S, Inoue Y, Koh S. Enhanced stereopsis of rotationally asymmetric multifocal intraocular lens with + 1.5 diopters near addition. Asia Pac J Ophthalmol. 2022;11(4):396. doi:10.1097/APO.0000000000000482
20. Zhu M, Fan W, Zhang G. Stereopsis and visual acuity: bilateral trifocal versus blended extended depth of focus and diffractive bifocal intraocular lenses. Front Med. 2022;9:1042101. doi:10.3389/fmed.2022.1042101
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Patient Preference, Visual Quality, and Multivariate Regression Analysis with Contralateral Bifocal and Trifocal Intraocular Lenses
Bucci Jnr FA
Clinical Ophthalmology 2022, 16:4097-4107
Published Date: 13 December 2022
Work Intensity of Postoperative Care Following Implantation of Presbyopia-Correcting versus Monofocal Intraocular Lenses
Maloney RK, Doane J, Weinstock R, Donaldson KE
Clinical Ophthalmology 2023, 17:1993-2001
Published Date: 17 July 2023

