Back to Journals » Clinical Ophthalmology » Volume 19
Comparison of Swept-Source Anterior Segment Ocular Coherence Tomography and Gonioscopy in Detecting Anterior Chamber Angle Closure
Authors Yaisiri P , Panarojwongse N, Treesit I, Choontanom R , Jatuthong O, Iemsomboon W, Funarunart P
Received 30 October 2024
Accepted for publication 18 February 2025
Published 27 February 2025 Volume 2025:19 Pages 699—711
DOI https://doi.org/10.2147/OPTH.S498949
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Panhathai Yaisiri, Natthanose Panarojwongse, Isaraporn Treesit, Raveewan Choontanom, Ornwasee Jatuthong, Wallop Iemsomboon, Panrapee Funarunart
Department of Ophthalmology, Phramongkutklao Hospital, Phramongkutklao College of Medicine, Bangkok, Thailand
Correspondence: Panrapee Funarunart., Department of Ophthalmology, Phramongkutklao Hospital, Phramongkutklao College of Medicine, 315 Ratchawithi Road, Thung Phaya Thai Sub-District, Ratchathewi District, Bangkok, 10400, Thailand, Email [email protected]
Purpose: To compare the diagnostic accuracy of swept-source anterior segment optical coherence tomography (AS-OCT) with gonioscopy in detecting angle closure among narrow-angle suspected eyes.
Patients and Methods: A total of 125 eyes determined narrow anterior chamber angles suspected by Van Herick’s technique grade 0, 1, or 2 were recruited. AS-OCT was undergone before any contact procedure. Intraocular pressure (IOP) measurements using applanation tonometry and gonioscopy were performed, respectively. AS-OCT images were blindly interpreted by 3 glaucoma specialists, involving both qualitative assessments at 0, 90, 180, and 270 degrees and quantitative analysis using iris-trabecular contact (ITC) index. The sensitivity and specificity of AS-OCT, compared with gonioscopy—the gold standard for identifying anterior chamber angle closure—were calculated.
Results: The mean age was 61± 12.9 years, and females constituted 67.6%. Eyes classified by Van Herick’s technique as grade 0, 1 and 2 were 16%, 58.40%, and 25.60%, respectively. Closed-angle identified by gonioscopy and AS-OCT were 100 eyes (80%) and 102 eyes (81.60%), respectively. The sensitivity and specificity of AS-OCT in detecting angle-closure were 92.16% (95% CI, 87.44– 96.87) and 73.91% (66.22– 81.61), respectively. For angle-closure identified by ITC index ≥ 55%, sensitivity was 86.36% (77.53– 95.20) and specificity was 92.86 (86.23– 99.49). The inter-observer agreement of gonioscopy was moderate (Kappa = 0.55), while the intra-observer and inter-observer agreement of AS-OCT was substantial (Kappa = 0.71– 0.80 and Kappa = 0.69, respectively).
Conclusion: AS-OCT enables a contactless qualitative and quantitative assessment of angle-closure in narrow-angle suspected eyes, demonstrating high sensitivity, acceptable specificity, and good inter-observer and intra-observer reliability.
Keywords: angle-closure, anterior segment ocular coherence tomography, gonioscopy
Introduction
Glaucoma is the leading cause of global irreversible blindness. The number of people with glaucoma worldwide will increase to 111.8 million in 2040.1 Primary angle-closure glaucoma (PACG) will significantly contribute to this increase, particularly in Asia, where cases are expected to reach 24.5 million, comprising 76.7% of global PACG cases.1 PACG can cause a high rate of monocular and binocular blindness.2 Foster et al estimated that 1.7 million people in China have bilateral blindness from glaucoma, and 91% of these cases are attributable to PACG.3 There are three stages of primary angle-closure disease, including primary angle-closure suspect (PACS), primary angle-closure (PAC), and primary angle-closure glaucoma (PACG).4,5 The population-based study reported that the five-year risk of progression of PACS to PAC was 22% and PAC to PACG was 28.5%.6,7 Early detection in an early stage of angle closure and appropriate management are crucial to prevent the conversion from PACS or PAC to PACG.
Therefore, anterior chamber angle examination is essential in classifying and identifying mechanisms of angle closure leading to appropriate management. The standard method for evaluating anterior chamber angle is gonioscopy which provides a 360-degree assessment of the angle width and angle abnormalities. Furthermore, indentation can be performed to identify the mechanism of angle closure. However, gonioscopy is an operator-dependent procedure, a contact technique, and the use of illumination can artificially widen the angle. Previous studies have shown that even experienced, trained examiners achieve only fair to moderate agreement in detecting angle closure.8,9 Anterior segment optical coherence tomography (AS-OCT) is an objective, non-contact method that provides high-resolution imaging of the anterior segment, serving as an alternative for identifying angle-closure suspected eyes. However, most previous studies on the effectiveness of AS-OCT in detecting angle closure compared to gonioscopy have not been conducted in Thailand, which has a high incidence of PAC spectrum. The majority of earlier studies focused on Asian populations; however, they were community-based and included both normal eyes and narrow-angle suspected eyes from the general population.10–12 In contrast, this study specifically examines the performance of AS-OCT in detecting angle closure, particularly in narrow-angle suspected eyes to correlate with real-world practice.
This study aimed to compare the diagnostic accuracy of swept-source AS-OCT with gonioscopy in detecting anterior chamber angle closure among narrow-angle suspected eyes in Thailand.
Materials and Methods
Study Participants
Institutional Review Board (IRB)/Ethics Committee approval from the Royal Thai Army was obtained, and informed consent was obtained from all participants. The study was conducted in fulfillment of the World Medical Association’s Declaration of Helsinki. Participants who were 18 years and above with one or both eyes determined narrow anterior chamber angles suspected by Van Herick’s technique grade 0, 1, or 2 on routine ophthalmic examination by a general ophthalmologist at the ophthalmic outpatient department in Phramongkutklao Hospital, Bangkok, Thailand were recruited. Participants who had a history of open globe injury, ocular laser treatment, and intraocular surgery were excluded. Additionally, those with abnormalities of the anterior segment that precluded examination by gonioscopy and AS-OCT, as well as individuals with ocular or periocular infections, were also excluded. After obtaining informed consent, all participants underwent AS-OCT, followed by comprehensive eye examinations conducted by one of three glaucoma specialists. These included visual acuity testing, anterior chamber depth (ACD) assessment using Van Herick’s technique, intraocular pressure (IOP) measurement with applanation tonometry, and gonioscopy—the gold standard for identifying anterior chamber angle closure.
Anterior Segment Optical Coherence Tomography
All participants underwent swept-source AS-OCT scanning (CASIA SS-1000, Tomey Corporation, Nagoya, Japan) in the darkroom before any eye contact examinations conducted by an experienced technician without conflicts of interest. The examiner gently opened the upper and lower eyelids and carefully avoided applying pressure to the globe. While the participant was fixing their gaze on the internal fixation target, a two-dimensional angle analysis scan was operated in 2.4 seconds. The horizontal image, vertical image, and 360-degree rotational animation display were exported for qualitative analysis on a personal computer at 0, 90, 180, and 270 degrees. The eye was classified as closed-angle if there was contact between the peripheral iris and the angle wall anterior to the scleral spur in at least two quadrants (Figure 1). Each eye underwent a single AS-OCT scan, and the images were interpreted independently by three glaucoma specialists who were blinded to the gonioscopic findings to evaluate the inter-observer agreement. For intra-observer agreement, the specialists re-evaluated the images two weeks later using new sequences.
The iris-trabecular contact (ITC) was quantitatively analyzed using a three-dimensional radial scan with a 16-mm range, which automatically selected 16 images every 11.25 degrees for identifying the scleral spur (SS) and the ITC end point (EP). The ITC index (percent) indicated the ITC ratio along the circumference, excluding invisible points and invisible range (degrees).
Before the study, the three glaucoma specialists reviewed reference images of angle closure and open-angle and participated in a training session on anterior chamber angle assessment, with those analyses excluded from the study. The SS and EP were marked manually by each examiner with a red “X” mark and a green “+” mark, respectively (Figure 2). Examples of open-angle and closed-angle are shown in Figures 2A and B, respectively.
 |
Figure 2 The Scleral Spur (SS) is labeled with a red “X” mark and the Iridotrabecular Contact End Point (EP) is labeled with a green “+” mark. (A) Open-angle (B) Closed-angle. |
Gonioscopy
A Dynamic gonioscopy was performed in a darkroom using an indirect 4-mirror goniolens while the eye was in the primary position. A narrow 1-mm beam of light with 16x magnification was vertically applied to assess the superior and inferior angles, while the horizontal beam was used for the nasal and temporal angles. The examination was undergone carefully to prevent light from affecting the pupil and to avoid applying pressure to the globe. The slightest movement of the eye was permitted to view over the hill of a steep iris. In the presence of an occludable angle, indentation gonioscopy was utilized to detect peripheral anterior synechiae (PAS). The first 12 eyes were undergone gonioscopy by three glaucoma specialists to calculate inter-observer agreement. The rest of the participants were examined by only one glaucoma specialist to reduce participants’ burden during the COVID-19 pandemic. Gonioscopic findings were recorded according to Modified Shaffer’s grading system. All raters were blinded from AS-OCT results. The eye was classified as closed-angle when the iridotrabecular contact was ≥ 180 degrees.
Statistics and Data Analysis
A minimum of 85 eyes was required for sensitivity calculation with an acceptable error of 0.08. Age, sex, underlying diseases, and eye examination including visual acuity, intraocular pressure, anterior chamber angle grading by Van Herick’s technique, lens status, gonioscopy, and optic nerve head examination were recorded. Demographic data was analyzed by mean and standard deviation (SD) for continuous data and frequency (%) for discrete data. The sensitivity and specificity of AS-OCT compared with gonioscopy in identifying anterior chamber angle closure were calculated. Kappa statistics were calculated for inter-observer and intra-observer agreement between glaucoma specialists in detecting anterior chamber angle closure by AS-OCT and inter-observer agreement by gonioscopic examination. For the ITC index, a Receiver Operating Characteristic (ROC) curve analysis was applied to obtain the optimal cut-point value. All statistical analyses were performed using Stata version 14.
Results
A total of 125 eyes from 68 Thai participants were recruited in this study, of whom 46 (67.6%) were female. The mean age was 61±12.9 years old. The numbers of eyes classified by Van Herick’s technique as grade 0, 1, and 2 were 20 (16.00%), 73 (58.40%), and 32 (25.60%) eyes, respectively. The median of ACD was 2.22 mm (IQR, 2.02–2.41) of which less than 2.5 mm was 105 (84.68%) eyes. Demographic data was shown in Table 1.
 |
Table 1 Demographic Data |
According to narrow-angle screening by using Van Herick’s grading, angle-closure eyes were identified by gonioscopy as 100%, 97.26%, and 34.38% compared with AS-OCT 90%, 93.15% and 43.75% in Van Herick grade 0, 1, and 2, respectively. The differences between the two methods were not statistically significant (Table 2). Superior angle (89.69%) was the most frequently found closed followed by inferior (88.57%), nasal (60.80%), and temporal (58.40%) for AS-OCT. Similarly, for gonioscopy superior angle was also the most frequently closed (79.2%) followed by inferior (76.8%), temporal (76.8%), and nasal (76.0%). For AS-OCT, despite the attempts to open both upper and lower eyelids, 4 angles can be identified in 60 eyes while 47 and 18 eyes can be identified at 3 and 2 angles, respectively. The most identifiable angle was the nasal and temporal angle (100%) followed by the superior (77.6%) and inferior angle (56%). The scleral spur was poorly identified in 46.67% of eyes, with 23 (21.90%) in the superior quadrant, 24 (22.86%) in the inferior quadrant, and 2 (1.90%) in the nasal quadrant. The overall sensitivity and specificity of AS-OCT in detecting anterior chamber angle closure were 92.16% (95% CI, 87.44–96.87) and 73.91% (95% CI, 66.22–81.61), respectively. The sensitivity and specificity of AS-OCT in detecting angle closure in eyes whose all 4 angles could be identified were 100.00% (95% CI, 100.00–100.00) and 64.29% (95% CI, 52.1–76.41), respectively (Table 3).
 |
Table 2 Detection of the Eyes with Anterior Chamber Angle Closure by Gonioscopy and Anterior Segment Optical Coherence Tomography (AS-OCT) Categorized Using Van Herick’s Grading Technique |
 |
Table 3 Detection of the Eyes with Anterior Chamber Angle Closure by Gonioscopy Compared with Anterior Segment Optical Coherence Tomography (AS-OCT) |
There were 41 eyes (32.8%) with slit opening angle, of which 77.5% were categorized as closed-angle from AS-OCT while 87.5% were classified as angle closure from gonioscopy. Subgroup analysis revealed that 35 of these eyes (85.3%) had ACD less than 2.5 mm. The sensitivity and specificity of AS-OCT in detecting anterior chamber angle closure among these eyes were 85.71% (95% CI, 69.74–95.19) and 83.33% (95% CI, 35.88–99.58), respectively. In contrast, among 85 eyes without a slit opening angle, the sensitivity was 95.52% (95% CI, 87.47–99.07) and the specificity was 72.22% (95% CI, 46.52–90.31).
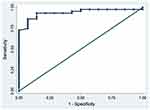
For the ITC index analysis, 58 eyes were analyzed in which SS, ITC, and EP were clearly marked, and the invisible range was equal to or less than 180 degrees. For angle closure identified by ITC index ≥ 51% (optimal cutoff point), sensitivity was 93.18% (95% CI, 86.69–99.67) and specificity was 85.71% (95% CI, 76.71–94.72) with a positive likelihood ratio (+LR) of 6.52. If the ITC index ≥ 55%, the sensitivity and the specificity were 86.36% (95% CI, 77.53–95.20) and 92.86% (95% CI, 86.23–99.49), respectively with a +LR of 12.09 (Table 4). The ROC curve compared sensitivity and specificity for various cutoff points of the ITC index in detecting anterior chamber angle closure, as shown in Figure 3.
 |
Table 4 Iridotrabecular Contact (ITC) Index Cutoff Values Comparing with Gonioscopy in Detecting Angle Closure |
The overall inter-observer agreement of gonioscopy was moderate (Kappa = 0.55), while AS-OCT was substantial (Kappa = 0.69). The inter-observer agreements of AS-OCT among the first and second, second and third, and first and third specialists were 0.76, 0.62, and 0.70, respectively, all indicating substantial agreement. The intra-observer agreement for AS-OCT interpretations by the first, second, and third specialists was also substantial, with Kappa values of 0.73, 0.71, and 0.80, respectively (Table 5).
 |
Table 5 Inter-Observer Agreement of Anterior Segment Optical Coherence Tomography (AS-OCT) (Closed Angles ≥180 Degrees) in Detecting Angle Closure |
Discussion
The sensitivity of AS-OCT in detecting angle closure compared with gonioscopy in narrow suspected eyes was high (92.16% with 95% CI, 87.44–96.87) while the specificity was acceptable (73.91% with 95% CI, 66.22–81.61). Gonioscopy, the gold standard for anterior chamber angle diagnosis, is a time-consuming and operator-dependent procedure, requiring skill and experience. It involves direct contact with the cornea, which can cause discomfort, and increase the risk of infection and trauma. Additionally, it is contraindicated in vulnerable eyes, such as those with open globe injuries, ocular infections, or corneal abrasions. Alternatively, the anterior segment OCT is an effective non-contact instrument for evaluating the anterior segment of the eye, enabling ophthalmologists to quickly assess the anterior chamber angle. It provides both qualitative and quantitative data by identifying an appositional angle. Angle closure can be clinically diagnosed by gonioscopy with at least 180 degrees of iridotrabecular contact. The ITC index can also determine the degree of angle closure. Nevertheless, the definite criteria for diagnosis of angle closure using AS-OCT remain disputed.
The anterior chamber angle was most frequently closed in the superior quadrant (89.69%), followed by the inferior quadrant (88.57%) in AS-OCT. Like gonioscopy, the most frequently closed angle was in the superior quadrant (79.2%), followed by the inferior quadrant (76.80%). Comparable to a community-based study in Singapore that compared the performance of gonioscopy and AS-OCT in detecting angle closure in different quadrants, they found that the superior quadrant had the highest frequency of closed-angle, followed by the inferior quadrant in both gonioscopy and AS-OCT.10 The higher prevalence of angle closure in the superior and inferior quadrants implied that failing to image these quadrants may result in missing many closed-angle eyes.10 The sensitivity of AS-OCT in detecting angle closure (defined as ≥ 2 quadrants of appositional angles from AS-OCT) compared with gonioscopy using Modified Shaffer’s grading system was high (92.16% with 95% CI, 87.44–96.87) while the specificity was acceptable (73.91% with 95% CI, 66.22–81.61). The systematic review and meta-analysis comparing the diagnostic accuracy of AS-OCT and gonioscopy for detecting angle closure revealed sensitivity of AS-OCT ranged from 46 to 100% (median 87%) and the specificity ranged from 55.3 to 100% (median 84%), reflecting variations in study design.12 There was insufficient evidence to determine which parameter is significantly better or worse for detecting angle closure.12 The hospital-based study in Singapore reported high sensitivity (94.1%) but low specificity (55.4%) of time-domain AS-OCT in detecting angle closure when compared with gonioscopy.11 However, the study recruited patients with suspected narrow-angle, and patients diagnosed with POAG and OHT. Moreover, the diagnostic criteria for the diagnosis of angle closure by gonioscopy and AS-OCT were different from our study. In a community-based study in Singapore, the sensitivity and specificity were 88.4% and 62.9%, respectively. They concluded that the low specificity may limit the usefulness of AS-OCT for screening of the narrow-angle.13 In contrast to our study, the specificity was higher than in the previous studies because we recruited the patients with narrow anterior chamber angles suspected by using Van Herick’s technique before performing AS-OCT to determine the performance of AS-OCT in detecting anterior chamber angle closure among narrow-angle suspected eyes. The Summary of studies on the diagnostic accuracy of AS-OCT and gonioscopy for detecting angle closure is shown in Table 6. The Van Herick’s technique is a subjective, non-invasive method used to estimate the depth of the anterior chamber angle, which is critical for assessing the risk of angle closure. Using slit-lamp biomicroscopy, a narrow slit beam of light is directed at the peripheral cornea at a 60-degree angle, and the examiner observes the ratio of anterior chamber depth to corneal thickness. The angle is traditionally graded into five categories (Van Herick grades 0–4): no visible space, <0.25:1, 0.25:1, 0.25–0.50:1, and ≥1:1, respectively. We postulated that the screening of narrow-angle by using Van Herick’s technique might increase the sensitivity and specificity of AS-OCT. Furthermore, performing AS-OCT following screening narrow-angle suspected eyes by Van Herick’s technique can reduce the cost and unnecessary use of AS-OCT for screening angle-closure eyes. However, AS-OCT in our study revealed a high false-positive rate, indicating that AS-OCT identified closed-angle despite open-angle on gonioscopy, consistent with previous studies. They reported that AS-OCT detected more angle-closure eyes than gonioscopy.9–11,13 There are many explanations for this finding. First, we presumed that the false-positive errors might be from an artificial widening of the angle while performing a gonioscopy. Despite the careful use of a minimal light beam, the light can cause pupil constriction leading to the artificial opening of an angle.11,13 Moreover, inadvertent placing a goniolens on the cornea might distort the anterior segment structure leading to a widening of the angle.11 Second, the criteria for diagnosis of angle closure using AS-OCT is different from gonioscopy. AS-OCT was classified as closed-angle when the contact between the peripheral iris and angle wall just above the scleral spur was presented which would have been classified as open-angle on gonioscopy.10,11,13 One study revealed that 71% of cases with short iridotrabecular contact just above the scleral spur were classified as closed-angle on AS-OCT but open-angle on gonioscopy10 as shown in Figure 4. Because this short contact does not extend up to the level of posterior pigmented trabecular meshwork, the angle may not be classified as closed-angle on gonioscopy.10 While gonioscopy was categorized as closed-angle when the posterior pigmented trabecular meshwork was not visible.10,11,13 Third, we postulated that the AS-OCT can detect angle closure before gonioscopy. Few longitudinal studies showed that AS-OCT was sensitive in detecting eyes that progress from open-angle to closed-angle on gonioscopy.14,15 The community-based study in Singapore found that angle closure detected on AS-OCT at baseline predicted subsequent angle closure on gonioscopy during the 4-year follow-up. Furthermore, the greater degrees of angle closure on AS-OCT at baseline increased the likelihood of angle closure developing on gonioscopy.14 They recommended that ophthalmologists should carefully monitor patients with closed-angle on AS-OCT, even though they had an open-angle on gonioscopy.14 A study that investigated quantitative AS-OCT parameters to predict the gonioscopic angle closure after a 4-year follow-up among participants initially categorized with gonioscopic open-angle.15 They found that a smaller angle opening distance at 750 μm (AOD750) and a larger lens vault (LV) are strongly associated with the future development of angle closure on gonioscopy.15 Another large community-based study aimed to identify factors associated with diagnostic disagreement between AS-OCT and gonioscopy. A deeper ACD and lower LV were significantly associated with a false-positive rate. In 90% of these cases, short ITC and irregular ITC were observed, with 52.57% showing short ITC and 39% showing irregular ITC. AS-OCT and gonioscopy generally agree when ACD is either narrow or deep; specifically, ACD measured < 2.2 mm for a true positive result and > 2.7 mm for a true negative result.16 However, the disagreement between the two techniques tends to arise when ACD is around 2.4 mm.16 Conversely, our study also identified a false-negative rate, indicating cases classified as open-angle on AS-OCT but closed-angle on gonioscopy. We found that 87.5% of these cases had a steep or convex iris configuration, and 62.5% had a slit opening angle on AS-OCT. We assumed that convex iris configuration could occlude the view of the angle while performing a non-indentation gonioscopy, potentially leading to a classification of closed-angle on gonioscopy. Moreover, the steep iris is typically associated with a slit opening angle on AS-OCT which shows a narrow-angle without any irido-angle contact indicating of open-angle on AS-OCT. There is no generally accepted guideline for determining the angle status based on the observation of slit opening on AS-OCT, whether the eye has an open or closed-angle. We classified a slit opening angle on AS-OCT as an open-angle when we could not identify any irido-angle contact (Figure 5). Consistent with a community-based study in Singapore, 51% of quadrants identified as open-angle on AS-OCT, but closed-angle on gonioscopy exhibited a steep iris configuration.10 Another community-based study reported that 66.7% of false-negative cases exhibited steep iris profiles, while 33.3% had irregular ITC.16 The qualitative analysis of AS-OCT in each quadrant, based solely on cross-sectional images at 0, 90, 180, and 270 degrees, might lack crucial information to determine the angle status, especially in cases of irregular ITC characterized by uneven iris profile along the circumstance, where some areas of the angle show ITC while others do not.16 Determining whether the angle is open or closed based on this scenario is challenging and could potentially lead to a misdiagnosis of angle status. Therefore, our study uses a quantitative analysis of AS-OCT to enhance diagnostic accuracy.
 |
Table 6 Summary of Studies on the Diagnostic Accuracy of AS-OCT and Gonioscopy for Detecting Angle Closure, Including the Current Study |
There are several parameters for quantitative assessment of angle closure such as angle opening distance (AOD), trabecular iris space area (TISA), trabecular iris angle (TIA), and ITC index. Lie et al17 evaluated the reproducibility of AS-OCT for detecting angle closure and identified angle parameters associated with measurement variability. They found that factors such as scan location, iris thickness variance, angle width, and axial length might affect AOD, TISA, and TIA, leading to increased variability in measurements.17 In contrast, using an ITC index analysis may be less affected by these variables because it provides an overall measurement of the percentage of angle closure extent.18 They also found that the ITC index had a moderate agreement and demonstrated good diagnostic performance for detecting angle closure compared with gonioscopy.18 Ho et al found that the ITC index had good and clinically acceptable inter-observer and intra-observer agreement and might be useful for discrimination even in borderline angle-closure cases.19 In our study, the ITC index with an optimal cutoff point of ≥51%—similar to the 180-degree angle closure identified by gonioscopy—demonstrates high sensitivity (93.18%; 95% CI: 86.69–99.67) and reasonable specificity (85.71%; 95% CI: 76.71–94.72), with an area under the curve (AUC) of 0.9 and a moderate +LR of 6.52. The cutoff point with high sensitivity can be useful for screening purposes. For the ITC index cutoff point ≥55%, the sensitivity was 86.36%, while the specificity was 92.86%, with a strong +LR of 12.09. As the ITC index cutoff point rises, the specificity increases, which might be more beneficial for confirming the condition. On the other hand, for the ITC index cutoff point ≥35%, the sensitivity was the highest (95.45%), but the specificity was the lowest (50%) with a minimal +LR of 1.91. In the previous study among predominantly Chinese populations, the optimal ITC index cutoff point was determined to be ≥35%. At this cutoff point, sensitivity and specificity were reported as 71.87% and 84.26%, respectively, with an AUC of 0.83 and a moderate +LR of 4.57. However, when the ITC index cutoff point was set at ≥50%, sensitivity and specificity were 43.75% and 91.67%, respectively, with a moderate +LR of 5.25.18 Another study found that the optimal cutoff point for the best performance was the ITC index ≥29%, yielding a sensitivity of 75.86% and specificity of 70.97%, with a +LR of 2.61.19 The optimal ITC index cutoff point in the previous studies were different compared to our study. There was no standard optimal ITC index cutoff point. A lower cutoff point exhibited higher sensitivity but lower specificity, making it suitable for screening angle closure. Conversely, a higher cutoff point showed lower sensitivity but higher specificity, proving beneficial for ruling in angle closure. However, our study used Van Herick’s technique for screening narrow-angle suspected eyes before participating in the study. Therefore, we recommend using the ITC index cutoff point ≥55%, which remains effective for both screening and confirming angle closure.
In terms of reliability, the overall inter-observer agreement of gonioscopy among glaucoma specialists in this study was moderate, with a Kappa of 0.55 based on the analysis of 12 eyes. Comparable with another study, Rigi et al9 found that inter-observer agreement of gonioscopy was moderate to good with a Kappa of 0.66 and 0.69, while intra-observer agreement ranged from moderate (Kappa = 0.53) to excellent (Kappa = 0.86). Another study investigating the repeatability of gonioscopy performed by optometrists, the intra-observer agreement was found to be fair (Kappa = 0.29), which was lower than Van Herick’s method (Kappa = 0.54) and AS-OCT (Kappa = 0.47).8 The variability in both inter-observer and intra-observer agreement of gonioscopy represents potential limitations of gonioscopic interpretation. This variability might be influenced by factors such as experience, technique, and dynamic anatomic variations in individual patients. Low kappa values for gonioscopy suggest that its use as the gold standard may introduce noise in patient evaluations. Prospective studies comparing the prognostic accuracy of gonioscopy and AS-OCT regarding treatment needs are warranted. On the other hand, AS-OCT was an objective, quantitative method for measuring the angle structure, potentially offering greater reliability than gonioscopy. In our study, the overall inter-observer agreement of AS-OCT was substantial, with a Kappa of 0.69. Intra-observer agreement was also substantial, ranging from Kappa values of 0.71 to 0.80. Comparable with another study, they focused solely on the superior angle and found that inter-observer agreement of AS-OCT ranged from moderate (Kappa = 0.58) to good (Kappa = 0.73), while intra-observer agreement varied from moderate (Kappa = 0.57) to almost perfect (Kappa = 0.83).9 In our study, three glaucoma specialists underwent a training session on anterior angle assessment together to enhance the accuracy of interpretation and increase the reliability of the test. For accurate detection of anterior chamber angle closure, training for both the operator and the reader is essential, and consensus criteria for detection of anterior chamber angle should be developed.
For clinical applications, AS-OCT serves various purposes. For angle closure screening, AS-OCT with high sensitivity is particularly useful for general ophthalmologists when gonioscopy is not feasible. It can also be used in telemedicine, particularly during a pandemic, to identify angle-closure eyes and refer patients to glaucoma specialists for further examination. Moreover, it proves beneficial for monitoring narrow-angle suspected eyes, facilitating early detection of potential angle-closure disease development. However, this study exclusively recruited participants with suspected narrow anterior chamber angles screened by Van Herick’s technique (grade 0, 1, and 2) to avoid extravagant over-investigation and ensure compatibility with real-world practice. While the Van Herick technique is effective for screening angle closure, combining it with AS-OCT can enhance the precision of AS-OCT as both a screening and diagnostic tool for detecting angle closure. Despite its advantages, the AS-OCT also has drawbacks. It cannot provide details about the angle structure or differentiate between appositional angle closure or synechiae closure, as gonioscopy does. This limitation is significant and can impact decision-making for treatment. Therefore, gonioscopy remains the gold standard for the diagnosis of angle closure.
There are some limitations in this study. Firstly, identification of the SS was challenging. In our study, SS was poorly identified in 46.67% of cases. The inferior angle had the highest rate of being unidentified at 22.86%, followed by the superior angle at 21.90%. A community-based study from Singapore found that SS could not be determined in approximately 30% of images. Additionally, they observed that the visibility of SS is significantly lower in superior and inferior quadrants compared to nasal and temporal quadrants, and in quadrants with angle closure. They suggested that some factors limited SS identification, such as imaging artifacts from the eyelid or eyelid manipulation, anatomical variations, and image acquisition. Even though the location of SS could not be identified, AS-OCT images could still be graded as open or closed-angle. They assumed that the SS was not necessary for the diagnosis of open-angle.20 Another community-based study found a 25% difficulty in determining the location of the SS, limiting its use for population screening for angle closure.21 The higher rate of unidentified SS in our study was attributed to the small eyes of Thai participants. Despite attempts to open both upper and lower eyelids adequately, completing a 360-degree AS-OCT scanning, especially for superior and inferior angle evaluations, remained difficult. Additionally, factors such as patient cooperation and the operator’s skill also influenced image quality. Secondly, the small number of participants in the ITC index analysis is a significant limitation, particularly if intended for screening purposes. Since we included only high-qualification images in which the SS and the EP could be clearly marked, and the invisible range was less than 180 degrees. New software algorithms for the automated detection of SS, an important landmark, could be beneficial for quantitative measurements of the anterior chamber angle and enhance the accurate diagnosis of angle closure. This study recruited narrow-angle suspected eyes, which may not be representative of the general population. However, AS-OCT is not frequently used for screening angle closure in general populations in real-world practice. The cost-effectiveness and accessibility of AS-OCT should be considered. Therefore, we recommend using AS-OCT in cases when angle closure is suspected, particularly when gonioscopy is not accessible.
Conclusion
In comparison with gonioscopy, the AS-OCT enables a contactless qualitative and quantitative assessment of anterior chamber angle closure in narrow-angle suspected eyes. AS-OCT also provides angle closure detection with high sensitivity, acceptable specificity, and good inter-observer and intra-observer reliability.
Disclosure
The author(s) report no conflicts of interest in this work.
References
1. Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040. Ophthalmology. 2014;121(11):2081–2090. doi:10.1016/j.ophtha.2014.05.013
2. Liu ML, Wang YX. The prevalence of blindness caused by primary angle closure glaucoma in middle-aged Chinese population: a systematic review and meta-analysis. Zhonghua Yan Ke Za Zhi Chin J Ophthalmol. 2017;53(5):373–377.
3. Foster PJ. Glaucoma in China: how big is the problem? Br J Ophthalmol. 2001;85(11):1277–1282. doi:10.1136/bjo.85.11.1277
4. Foster PJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86(2):238–242. doi:10.1136/bjo.86.2.238
5. Prum BE, Herndon LW, Moroi SE, et al. Primary angle closure preferred practice pattern(®) guidelines. Ophthalmology. 2016;123(1):P1–P40. doi:10.1016/j.ophtha.2015.10.049
6. Thomas R, George R, Parikh R, Muliyil J, Jacob A. Five year risk of progression of primary angle closure suspects to primary angle closure: a population based study. Br J Ophthalmol. 2003;87(4):450–454. doi:10.1136/bjo.87.4.450
7. Thomas R, Parikh R, Muliyil J, Kumar RS. Five-year risk of progression of primary angle closure to primary angle closure glaucoma: a population-based study. Acta Ophthalmol Scand. 2003;81(5):480–485. doi:10.1034/j.1600-0420.2003.00135.x
8. Campbell P, Redmond T, Agarwal R, Marshall LR, Evans BJW. Repeatability and comparison of clinical techniques for anterior chamber angle assessment. Ophthalmic Physiol Opt J Br Coll Ophthalmic Opt Optom. 2015;35(2):170–178. doi:10.1111/opo.12200
9. Rigi M, Bell NP, Lee DA, et al. Agreement between gonioscopic examination and swept source Fourier domain anterior segment optical coherence tomography imaging. J Ophthalmol. 2016;2016:1727039. doi:10.1155/2016/1727039
10. Sakata LM, Lavanya R, Friedman DS, et al. Comparison of gonioscopy and anterior segment ocular coherence tomography in detecting angle closure in different quadrants of the anterior chamber angle. Ophthalmology. 2008;115(5):769–774. doi:10.1016/j.ophtha.2007.06.030
11. Nolan WP, See JL, Chew PTK, et al. Detection of primary angle closure using anterior segment optical coherence tomography in Asian Eyes. Ophthalmology. 2007;114(1):33–39. doi:10.1016/j.ophtha.2006.05.073
12. Desmond T, Tran V, Maharaj M, Carnt N, White A. Diagnostic accuracy of AS-OCT vs gonioscopy for detecting angle closure: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2022;260(1):1–23. doi:10.1007/s00417-021-05271-4
13. Lavanya R, Foster PJ, Sakata LM, et al. Screening for narrow angles in the Singapore population: evaluation of new noncontact screening methods. Ophthalmology. 2008;115(10):1720–1727.e2. doi:10.1016/j.ophtha.2008.03.015
14. Baskaran M, Iyer JV, Narayanaswamy AK, et al. Anterior segment imaging predicts incident gonioscopic angle closure. Ophthalmology. 2015;122(12):2380–2384. doi:10.1016/j.ophtha.2015.07.030
15. Nongpiur ME, Aboobakar IF, Baskaran M, et al. Association of baseline anterior segment parameters with the development of incident gonioscopic angle closure. JAMA Ophthalmol. 2017;135(3):252. doi:10.1001/jamaophthalmol.2016.5847
16. Porporato N, Baskaran M, Tun TA, et al. Understanding diagnostic disagreement in angle closure assessment between anterior segment optical coherence tomography and gonioscopy. Br J Ophthalmol. 2020;104(6):795–799. doi:10.1136/bjophthalmol-2019-314672
17. Liu S, Yu M, Ye C, Lam DSC, Shun LCK. Anterior chamber angle imaging with swept-source optical coherence tomography: an investigation on variability of angle measurement. Invest Ophthalmol Vis Sci. 2011;52(12):8598–8603. doi:10.1167/iovs.11-7507
18. Baskaran M, Ho SW, Tun TA, et al. Assessment of circumferential angle-closure by the iris–trabecular contact index with swept-source optical coherence tomography. Ophthalmology. 2013;120(11):2226–2231. doi:10.1016/j.ophtha.2013.04.020
19. Ho SW, Baskaran M, Zheng C, et al. Swept source optical coherence tomography measurement of the iris-trabecular contact (ITC) index: a new parameter for angle closure. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol. 2013;251(4):1205–1211. doi:10.1007/s00417-012-2158-6
20. Sakata LM, Lavanya R, Friedman DS, et al. Assessment of the scleral spur in anterior segment optical coherence tomography images. Arch Ophthalmol Chic IL 1960. 2008;126(2):181–185.
21. Narayanaswamy A, Sakata LM, He MG, et al. Diagnostic performance of anterior chamber angle measurements for detecting eyes with narrow angles: an anterior segment OCT study. Arch Ophthalmol Chic IL 1960. 2010;128(10):1321–1327.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.