Back to Journals » Orthopedic Research and Reviews » Volume 17
Correlation Analysis of Serum G-Protein-Coupled Receptor 4 and Biglycan Levels with the Severity of Intervertebral Disc Degeneration
Authors Gao B, Cui Y, Qin Y, Qu C, Zhao J, Li X
Received 27 February 2025
Accepted for publication 21 June 2025
Published 8 July 2025 Volume 2025:17 Pages 289—297
DOI https://doi.org/10.2147/ORR.S525337
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Bingjie Gao,1 Yizhi Cui,2 Yexiao Qin,2 Chuncheng Qu,3 Jiaqi Zhao,4 Xiaoning Li2
1Second Clinical Medical School, Heilongjiang University of Chinese Medicine, Harbin, Heilongjiang, People’s Republic of China; 2Department of Acupuncture, The Second Affiliated Hospital of Heilongjiang University of Chinese Medicine, Harbin, Heilongjiang, People’s Republic of China; 3School of Basic Medicine, Heilongjiang University of Chinese Medicine, Harbin, Heilongjiang, People’s Republic of China; 4Preventive Medicine Center, The First Affiliated Hospital of Heilongjiang University of Chinese Medicine, Harbin, Heilongjiang, People’s Republic of China
Correspondence: Xiaoning Li, Department of Acupuncture, The Second Affiliated Hospital of Heilongjiang University of Chinese Medicine, 411 Gogol Street, Nangang District, Harbin, Heilongjiang, People’s Republic of China, Tel +86 13313699268, Email [email protected]
Objective: To investigate the correlation between serum levels of G protein-coupled receptor 4 (GPR4) and Biglycan (BGN) with the severity of Intervertebral Disc Degeneration (IVDD).
Methods: A total of 162 patients with IVDD treated at our hospital from August 2023 to August 2024 were included. The general information of patients was retrospectively collected. MRI was used to assess IVDD severity using the Pfirrmann grading system. Serum GPR4 and BGN levels were measured by enzyme-linked immunosorbent assay (ELISA). Multiple linear regression analysis was performed to identify risk factors for IVDD severity. Spearman’s and Pearson’s correlation analyses were used to evaluate the relationships between serum GPR4, BGN, and IVDD severity. Receiver operating characteristic (ROC) curve analysis was used to evaluate the diagnostic value of serum GPR4 and BGN in IVDD.
Results: Significant differences in age and the proportion of diabetic patients as well as serum GPR4 and BGN were found among different Pfirrmann grades (P< 0.05). Serum GPR4 levels increased but BGN levels decreased with higher Pfirrmann grades (P< 0.05). Multiple linear regression analysis showed that age and serum GPR4 and BGN levels were risk factors for IVDD severity (P< 0.05). The results of the correlation analysis showed that serum GPR4 and age were positively correlated with the severity of IVDD (r=0.651, r=0.488, P< 0.001), while BGN was negatively correlated with the severity of IVDD (r=− 0.591, P< 0.001). The results of Spearman correlation analysis showed a negative correlation between serum GPR4 and BGN (P< 0.05). ROC curve analysis revealed that the AUC values for the diagnosis of IVDD using serum GPR4 alone, BGN alone, and the combination of GPR4 and BGN were 0.918, 0.811, and 0.919, respectively (P< 0.05). Moreover, the combination of GPR4 and BGN demonstrated higher sensitivity and specificity compared to either marker alone.
Conclusions: Serum GPR4 and BGN levels are identified as effective diagnostic indicators for IVDD, with serum GPR4 positively correlated but BGN negatively correlated with the severity of IVDD.
Keywords: G protein-coupled receptor 4, biglycan, intervertebral disc degeneration, correlation
Introduction
Intervertebral Disc Degeneration (IVDD) is a significant pathophysiological basis for lumbar spine diseases, such as lumbar disc herniation and lumbar spinal stenosis, which severely affect patients’ quality of life and work capacity. The pathogenesis of IVDD is complex, involving genetic factors, environmental factors, and an imbalance in the metabolism of the extracellular matrix, among others.1 Currently, the diagnosis of IVDD primarily relies on imaging examinations, such as the Pfirrmann grading on MRI,2 but these methods are difficult to achieve early diagnosis and lack specificity. Previous studies have found that various serum markers are associated with IVDD, such as matrix metalloproteinases and inflammatory factors.3,4 However, these markers have limited specificity and cannot comprehensively reflect the pathogenesis of IVDD. Therefore, the search for biomarkers that can diagnose early and assess the severity of IVDD has become a research hotspot.
G protein-coupled receptor 4 (GPR4) is an orphan receptor with a potential role in cell signal transduction, capable of activating inflammation and increasing the expression levels of nerve growth factor in acidic microenvironments, which has been confirmed in multiple organ systems.5 Moreover, GPR4 is expressed in rat nucleus pulposus cells and its expression is upregulated in an acidic microenvironment that mimics degenerative intervertebral discs (IVDs), closely associated with the elevated expression of the RANK/RANKL/OPG axis and neurotrophic proteins.6 Biglycan (BGN), a constituent of the leucine-rich proteoglycan family, is extensively present in the extracellular matrix.7 Animal studies have demonstrated that BGN plays a crucial role in maintaining the structural integrity of intervertebral discs and delaying degeneration. BGN achieves this by modulating the composition and function of the extracellular matrix, thereby protecting disc cells from damage and preserving disc health.8 Additionally, both cellular and animal studies have highlighted the critical importance of BGN and its fragment Bgm1 in maintaining the normal function and quantity of disc cells.9 Although a few cellular and animal experiments have explored the relationship between GPR4 and BGN with IVDD, clinical applications of these findings are limited, and the association between serum levels of GPR4 and BGN and the severity of IVDD remains unclear. This study aims to fill this research gap by investigating the correlation between serum levels of GPR4 and BGN and the severity of IVDD. Our goal is to provide new biomarker evidence for the early diagnosis and disease monitoring of IVDD, thereby improving diagnostic accuracy and offering more precise guidance for clinical treatment.
Objects and Methods
Study Object
A total of 162 patients with IVDD treated at our hospital from August 2023 to August 2024 were selected for this study, consisting of 76 males and 86 females, with ages ranging from 48 to 70 years. Inclusion criteria: (1) meeting the relevant diagnostic criteria for IVDD;10 (2) all patients underwent MRI examination; (3) all patients had complete clinical data. Exclusion criteria: (1) disc lesions caused by tumors or infections; (2) presence of significant organ dysfunction; (3) presence of hematological and immunological system diseases; (4) presence of bone metabolism-related diseases; (5) patients who had recently undergone spinal surgery; (6) patients receiving medication affecting disc metabolism or inflammatory responses; (7) patients with severe mental illness or cognitive impairment who could not understand the content of the study; (8) patients with concurrent lumbar spine fractures. Additionally, 78 individuals who underwent health check-ups during the same period were selected as the Control group, including 40 males and 38 females, with ages ranging from 47 to 70 years old. The baseline characteristics of the control and IVDD groups were presented in Table 1. No statistically significant differences were observed in the baseline characteristics between the Control and IVDD groups, indicating comparability (P>0.05).
 |
Table 1 General Information Comparison Between Control Group and IVDD Group |
Methods
General Information
The following information was retrospectively collected from patients: gender, age, Body mass index (BMI), smoking history, drinking history, and the presence of underlying diseases such as hypertension and diabetes.
Severity Grading of IVDD
All enrolled patients underwent magnetic resonance imaging (MRI) examination, and the severity of IVDD was graded using the Pfirrmann grading system, in which Grade I represents a normal intervertebral disc, and Grades II to V represent degenerated intervertebral discs.2 For the purpose of this study, patients with IVDD Grades II to V were included as study subjects. There were 42 patients with Grade II lesions, 36 patients with Grade III lesions, 46 patients with Grade IV lesions, and 38 patients with Grade V lesions.
Power Analysis: Utilizing G*Power version 3.1 software, we conducted a power analysis based on the Pfirrmann grading system (Grades I to V) and employed a linear multiple regression analysis (Fixed model, R² deviation from zero) to determine the sample size required for each subgroup. The analysis revealed that, with an alpha level (α) of 0.05, a desired power of 95%, and an effect size (f²) of 0.15 indicating a medium effect, each subgroup would necessitate a minimum of approximately 33 subjects. The current sample sizes for the subgroups (42, 36, 46, and 38 subjects) may be adequate for detecting medium effect sizes but may have limited capacity to detect smaller effect sizes. Furthermore, a post hoc power analysis based on the existing data indicated that the power, calculated with the smallest subgroup sample size (36 subjects per group), is 97%, which exceeds the pre-specified threshold of 95%. This suggests that the sample size for the subgroup analysis in this study is sufficient.
Detection of Serum GPR4 and BGN
Upon admission, 5 mL of venous blood was drawn from all enrolled patients. After centrifugation at 3000 r/min for 10 minutes, the supernatant was collected and stored at −80°C. Serum samples stored in the biobank of our hospital were used for detection in this study and the levels of GPR4 and BGN in the serum were measured according to the manufacturer’s instructions of the respective ELISA kits (EH1317, Wuhan Fine Biotech Co., Ltd., China; HM11655, Bioswamp, China). The optical density (OD) values were measured at 450 nm using a microplate reader (Multiskan Sky High, Thermo Fisher Scientific, USA). The concentrations of GPR4 and BGN were calculated by substituting the OD values into the standard curves.
Statistical Analysis
Data were analyzed using SPSS 26.0 software. Data conforming to a normal distribution were expressed as the mean ± standard deviation ( ), and one-way ANOVA was used for comparisons among multiple groups. Continuous variables not conforming to a normal distribution were described using the median and interquartile range [M (P25, P75)], and the Kruskal-Wallis rank sum test was used for comparisons among multiple groups. Categorical data were expressed as frequency (n) and percentage (%), and the chi-square test was used to analyze differences between groups. Multiple linear regression was employed to analyze risk factors affecting the severity of IVDD. Pearson correlation analysis was used for data between two groups that were normally distributed, while Spearman correlation analysis was applied for data between two groups that did not follow a normal distribution. A P-value of less than 0.05 indicated a statistically significant difference.
), and one-way ANOVA was used for comparisons among multiple groups. Continuous variables not conforming to a normal distribution were described using the median and interquartile range [M (P25, P75)], and the Kruskal-Wallis rank sum test was used for comparisons among multiple groups. Categorical data were expressed as frequency (n) and percentage (%), and the chi-square test was used to analyze differences between groups. Multiple linear regression was employed to analyze risk factors affecting the severity of IVDD. Pearson correlation analysis was used for data between two groups that were normally distributed, while Spearman correlation analysis was applied for data between two groups that did not follow a normal distribution. A P-value of less than 0.05 indicated a statistically significant difference.
Results
Comparison of General Information
There were no statistically significant differences in BMI levels, gender, smoking history, drinking history, and the proportion of hypertension among patients with different Pfirrmann grades (P>0.05); however, significant differences were observed in age and the proportion of diabetes patients (P>0.05) (Table 2).
 |
Table 2 Comparison of General Information Among Patients with Different Pfirrmann Grades in IVDD Group |
Comparison of Serum GPR4 and BGN Levels
There was a statistically significant difference in serum GPR4 and BGN levels among patients with different Pfirrmann grades (P<0.05), with serum GPR4 levels increasing and BGN levels decreasing as the grade increased (Table 3).
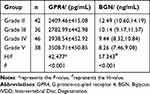 |
Table 3 Comparison of Serum GPR4 and BGN Levels in Patients with Different Pfirrmann Grades in IVDD Group |
Multivariate Linear Regression Analysis of IVDD Severity
With the Pfirrmann grade of patients as the dependent variable and age, history of diabetes (yes=1, no=0), and serum GPR4 and BGN levels as independent variables, a multivariate linear regression analysis was conducted. The results indicated that age and serum GPR4 and BGN levels are risk factors affecting the severity of IVDD (P<0.05) (Table 4).
 |
Table 4 Multivariate Linear Regression Analysis of IVDD Severity |
The Correlation Between Age, Serum GPR4, BGN, and the Severity of IVDD
The results of Pearson correlation analysis showed a positive correlation between serum GPR4 and the severity of IVDD (r=0.651, P<0.001). Spearman correlation analysis indicated a positive correlation between age and the severity of IVDD (r=0.488, P<0.001). In contrast, serum BGN was negatively correlated with the severity of IVDD (r=−0.591, P<0.001) (Figure 1).
Correlation Between Serum GPR4 and BGN
Spearman’s correlation analysis demonstrated a negative relationship between serum GPR4 and BGN (r=−0.446, P<0.001) (Figure 2).
 |
Figure 2 Correlation between Serum GPR4 and BGN. |
Diagnostic Value of Serum GPR4 and BGN in IVDD
The serum levels of GPR4 and BGN were compared between the control group and patients with IVDD. The diagnostic value of GPR4 and BGN in IVDD was further evaluated using ROC curve analysis. The results showed that the AUC for the diagnosis of IVDD using GPR4, BGN, and the combination of GPR4 and BGN were 0.918, 0.814, and 0.919, respectively (P<0.05). The combined diagnostic approach exhibited higher sensitivity and specificity compared to the use of either biomarker alone (Table 5 and Figure 3).
 |
Table 5 Diagnostic Value of Serum GPR4 and BGN in IVDD |
 |
Figure 3 ROC curves for the diagnosis of IVDD using serum GPR4 and BGN. |
Discussion
Although several biomarkers, such as matrix metalloproteinases (MMPs) and inflammatory cytokines, have been identified as potential diagnostic indicators for IVDD,11,12 these markers lack specificity and may not accurately distinguish IVDD from other inflammatory diseases. In this study, we report for the first time that serum GPR4 and BGN levels are dysregulated in IVDD and are associated with the severity of the condition. These findings provide novel biomarker evidence for the early diagnosis and disease monitoring of IVDD.
IVDD is a complex degenerative disease with a pathogenesis involving multiple factors, including inflammatory responses, acidic microenvironments, and metabolic imbalances of the extracellular matrix.13–15 As age increases, cellular metabolism in the intervertebral discs slows down, and nutrient supply decreases, leading to the loss of proteoglycans and water in the nucleus pulposus, fissures in the annulus fibrosus, calcification of the cartilaginous endplates, and ultimately resulting in IVDD.16 The results of this study show a positive correlation between age and the severity of IVDD, indicating that the older the age, the higher the severity of IVDD, which is consistent with the findings of Liebsch et al.17
GPR4, as a proton-sensing receptor, can accumulate cyclic adenosine monophosphate (cAMP) within nucleus pulposus cells under acidic conditions, activating inflammatory signaling pathways such as the MAPK and NF-κB pathways, thereby initiating inflammatory responses and regulating IVDD.18 In this study, as the severity of IVDD increased, the levels of GPR4 in serum showed a significant upward trend. This may be attributed to the formation of a more acidic microenvironment within the intervertebral disc, which in turn leads to the elevation of serum GPR4 levels. These findings suggest that GPR4 may play an important role in the process of IVDD. The increase in serum GPR4 levels may reflect the exacerbation of inflammatory responses during the progression of IVDD. This result is consistent with previous studies where GPR4 expression was upregulated in an acidic microenvironment similar to degenerated intervertebral discs, closely associated with the increased expression of the RANK/RANKL/OPG system and neurotrophic proteins, suggesting that GPR4 may promote the progression of IVDD by activating inflammatory responses and affecting the metabolism of the extracellular matrix.6
BGN constitutes an essential element of the intervertebral disc extracellular matrix and is vital for preserving disc architecture and functionality.19 It is released in response to tissue injury or stress, acting as a damage-associated molecular pattern to activate inflammatory responses.20 The findings of this study reveal a negative correlation between serum BGN levels and the severity of IVDD, indicating that the lower the BGN levels, the more severe the degeneration. This phenomenon may be related to the important role of BGN in maintaining the structure of the intervertebral disc. Proteomic analysis has revealed that BGN was downregulated in intervertebral discs with Modic changes, which may be associated with the inflammation and tissue destruction related to these changes.21 Additionally, animal studies have shown that mice with BGN knockdown exhibit more severe IVDD, and that adipose-derived stromal cells can promote an increase in BGN levels, thereby improving IVDD.22 The present study underscores the importance of BGN in intervertebral disc health and highlights its potential as a biomarker and therapeutic target for IVDD.
The results of our study revealed a positive correlation between serum GPR4 levels and the severity of IVDD, while serum BGN levels were negatively correlated with IVDD severity. Further investigation uncovered a negative correlation between serum GPR4 and BGN levels. The underlying mechanism may be that the activation of GPR4, which can influence inflammatory responses and the metabolism of the extracellular matrix, indirectly affects BGN levels. In an acidic microenvironment, the activation of GPR4 leads to the release of inflammatory factors. These factors not only promote the degradation of proteoglycans but may also inhibit their synthesis.23 Therefore, the increased levels of GPR4 in serum may, together with the decreased levels of BGN, reflect the pathological physiological processes of inflammatory responses and imbalances in extracellular matrix metabolism during the progression of IVDD.
Multivariate linear regression analysis indicated that age, as well as serum levels of GPR4 and BGN, are risk factors influencing the severity of IVDD. This further underscores the significance of age in the progression of IVDD and highlights the potential value of serum GPR4 and BGN as biomarkers. In univariate analysis, the prevalence of diabetes showed statistical significance. However, this variable was not identified as significantly associated in the multivariate regression model. The discrepancy may be attributed to the fact that age is a well-established risk factor for IVDD and may have complex interactions with diabetes. As individuals age, their metabolic functions gradually decline, and the risk of developing insulin resistance and subsequently diabetes increases. Moreover, aging is intrinsically linked to disc degeneration. Therefore, the association between diabetes prevalence and IVDD may be confounded by age and other related factors. Future studies should validate these findings in larger and more diverse populations. ROC curve analysis revealed that the combined detection of serum GPR4 and BGN significantly enhances diagnostic sensitivity and specificity to 91.36% and 83.33%, respectively, thus serving as a promising biomarker panel for the diagnosis of intervertebral disc degeneration (IVDD) (AUC = 0.919). When integrated with MRI, this combined approach not only achieves complementary advantages but also improves diagnostic accuracy. Moreover, it can reduce the need for additional unnecessary diagnostic tests, thereby lowering healthcare costs.
In summary, the levels of serum GPR4 and BGN are significantly correlated with the severity of IVDD, indicating that serum GPR4 and BGN levels could serve as potential biomarkers for early assessment and monitoring of IVDD, providing a basis for clinical intervention. However, the study has certain limitations: the relatively small sample size may compromise the statistical significance and limit the generalizability of the findings; the mechanisms of action within intervertebral disc tissue were not deeply explored and require further in vitro and in vivo experimental validation; IVDD is a multifactorial process, and it is necessary to consider genetic and lifestyle factors comprehensively to fully understand its pathogenesis.
Conclusion
This study, for the first time, demonstrates the correlation between serum GPR4 and BGN levels and the severity of IVDD, highlighting their potential as diagnostic biomarkers for IVDD. The combined detection of serum GPR4 and BGN significantly enhances diagnostic accuracy for IVDD, providing a novel biomarker basis for early diagnosis and disease monitoring. Future research should aim to validate these findings in larger and more diverse populations and explore their clinical application value.
Data Sharing Statement
The datasets used and/or analyzed in the current study are available from the corresponding author upon reasonable request.
Ethics Statement
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Heilongjiang University of Chinese Medicine [approval number: 2021-K-181] and was performed in accordance with the ethical standards of the Declaration of Helsinki. Given the retrospective nature of our study and the anonymization of the data, informed consent was waived by the Ethics Committee of the Second Affiliated Hospital of Heilongjiang University of Chinese Medicine.
Acknowledgments
All authors would like to thank all collaborators of this study.
Funding
No funding was received for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sakai D. Insights into IVDD pathogenesis in 2024. Nat Rev Rheumatol. 2025;21(2):71–72. doi:10.1038/s41584-024-01207-4
2. Chen XL, Li XY, Wang Y, Lu SB. Relation of lumbar intervertebral disc height and severity of disc degeneration based on pfirrmann scores. Heliyon. 2023;9(10):e20764. doi:10.1016/j.heliyon.2023.e20764
3. Dou Y, Zhang Y, Liu Y, et al. Role of macrophage in intervertebral disc degeneration. Bone Res. 2025;13(1):15. doi:10.1038/s41413-024-00397-7
4. Zou X, Zhang X, Han S, et al. Pathogenesis and therapeutic implications of matrix metalloproteinases in intervertebral disc degeneration: a comprehensive review. Biochimie. 2023;214(Pt B):27–48. doi:10.1016/j.biochi.2023.05.015
5. Li R, Guan Z, Bi S, et al. The proton-activated G protein-coupled receptor GPR4 regulates the development of osteoarthritis via modulating CXCL12/CXCR7 signaling. Cell Death Dis. 2022;13(2):152. doi:10.1038/s41419-021-04455-4
6. Li H, Liu H, Zhang N, Zhu Z. Involvement of the G-protein-coupled receptor 4 in the increased expression of RANK/RANKL/OPG system and neurotrophins by nucleus pulposus cells under the degenerated intervertebral disc-like acidic microenvironment. Biomed Res Int. 2020;2020(1):1328436. doi:10.1155/2020/1328436
7. Hua R, Han Y, Ni Q, et al. Pivotal roles of biglycan and decorin in regulating bone mass, water retention, and bone toughness. Bone Res. 2025;13(1):2. doi:10.1038/s41413-024-00380-2
8. Furukawa T, Ito K, Nuka S, et al. Absence of biglycan accelerates the degenerative process in mouse intervertebral disc. Spine. 2009;34(25):E911–917. doi:10.1097/BRS.0b013e3181b7c7ec
9. Zhu M, Scm W, Tam WK, et al. Biglycan fragment modulates TGF-β activity in intervertebral disc via an eIF6-coupled intracellular path. Sci Adv. 2025;11(7):eadq8545. doi:10.1126/sciadv.adq8545
10. Wu PH, Kim HS, Jang IT. Intervertebral disc diseases PART 2: a review of the current diagnostic and treatment strategies for intervertebral disc disease. Int J Mol Sci. 2020;21(6):2315. doi:10.3390/ijms21072315
11. Gao Y, Ma X, Shi Z, et al. MMP expression and its clinical significance in intervertebral disc destruction of spinal tuberculosis, brucellar spondylitis, and pyogenic spondylitis. J Orthop Surg Res. 2025;20(1):208. doi:10.1186/s13018-025-05622-5
12. Liu Y, Lei F, Feng D, et al. Tracing the pathways: how inflammatory cytokines and blood metabolites drive intervertebral disc degeneration. Eur Spine J. 2025.
13. Wang N, Rong W, Xie Y, Chen S, Xi Z, Deng R. Visualizing the bibliometrics of the inflammatory mechanisms in intervertebral disc degeneration. Exp Gerontol. 2024;188:112380. doi:10.1016/j.exger.2024.112380
14. Dai WY, Luo ZP. Paeoniflorin inhibits pyroptosis of nucleus pulposus cells in an acidic environment and alleviates the degeneration of the intervertebral disc in rats. Cell Signal. 2022;91:110243. doi:10.1016/j.cellsig.2022.110243
15. Stover JD, Lawrence B, Bowles RD. Degenerative IVD conditioned media and acidic pH sensitize sensory neurons to cyclic tensile strain. J Orthop Res. 2021;39(6):1192–1203. doi:10.1002/jor.24682
16. Wang F, Cai F, Shi R, Wang XH, Wu XT. Aging and age related stresses: a senescence mechanism of intervertebral disc degeneration. Osteoarthritis Cartilage. 2016;24(3):398–408. doi:10.1016/j.joca.2015.09.019
17. Liebsch C, Wilke HJ. The intradiscal pressure of the lumbar spine is affected by intervertebral disc degeneration, age, level, and motion direction: evaluation of an in vitro database comprising 107 specimens. Spine J. 2025;25(6):1276–1287. doi:10.1016/j.spinee.2025.01.024
18. Ma Y, Wang Y, Tang M, et al. Cryo-EM structure of an activated GPR4-Gs signaling complex. Nat Commun. 2025;16(1):605. doi:10.1038/s41467-025-55901-2
19. Zhang S, Liu W, Chen S, et al. Extracellular matrix in intervertebral disc: basic and translational implications. Cell Tissue Res. 2022;390(1):1–22. doi:10.1007/s00441-022-03662-5
20. Miguez PA. Evidence of biglycan structure-function in bone homeostasis and aging. Connect Tissue Res. 2020;61(1):19–33. doi:10.1080/03008207.2019.1669577
21. Rajasekaran S, Soundararajan DCR, Nayagam SM, et al. Modic changes are associated with activation of intense inflammatory and host defense response pathways - molecular insights from proteomic analysis of human intervertebral discs. Spine J. 2022;22(1):19–38. doi:10.1016/j.spinee.2021.07.003
22. Marfia G, Campanella R, Navone SE, et al. Potential use of human adipose mesenchymal stromal cells for intervertebral disc regeneration: a preliminary study on biglycan-deficient murine model of chronic disc degeneration. Arthritis Res Ther. 2014;16(5):457. doi:10.1186/s13075-014-0457-5
23. Justus CR, Marie MA, Sanderlin EJ, Yang LV. The roles of proton-sensing G-protein-coupled receptors in inflammation and cancer. Genes. 2024;15(9):1151. doi:10.3390/genes15091151
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


