Back to Journals » Clinical Interventions in Aging » Volume 20
D-Dimer Levels and NIHSS as Prognostic Predictors in Elderly Patients with Cerebral Infarction
Authors Zheng Z
Received 22 November 2024
Accepted for publication 14 April 2025
Published 26 April 2025 Volume 2025:20 Pages 505—511
DOI https://doi.org/10.2147/CIA.S502994
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Zhong Zheng
Department of Clinical Laboratory, the First People’s Hospital of Hefei, Hefei, 230061, People’s Republic of China
Correspondence: Zhong Zheng, Email [email protected]
Objective: This study evaluates the relationship between D-dimer levels and NIHSS scores with prognosis in elderly patients with cerebral infarction.
Methods: This study was a retrospective study that included 112 elderly patients with cerebral infarction admitted to our hospital from January 2022 to December 2023. The modified Rankin Scale (mRS) was used to assess the prognosis at six-month follow-up, and patients were divided into two groups: good prognosis (mRS 0– 2) and poor prognosis (mRS 3– 6). Detailed data collection and statistical analysis were conducted, including descriptive statistics of baseline data, correlation analysis between D-dimer and NIHSS scores, and multivariate logistic regression analysis to identify independent risk factors for poor prognosis.
Results: Patients in the poor prognosis group had significantly higher age, BMI, proportions of smoking history, alcohol consumption history, transient ischemic attack (TIA) history, atrial fibrillation history, admission NIHSS scores, and D-dimer levels compared to the good prognosis group (P< 0.05). In addition, there were significant differences in D-dimer levels among patients with mild (NIHSS 1– 4), moderate (NIHSS 5– 14), and severe (NIHSS≥ 15) strokes (P< 0.001), and D-dimer levels were significantly positively correlated with NIHSS scores (r=0.58, P< 0.001). Multivariate logistic regression analysis showed that D-dimer levels, admission NIHSS scores, age, atrial fibrillation, and TIA history were independent predictors of poor prognosis (P< 0.05). ROC curve analysis showed that the AUC of D-dimer in predicting poor prognosis was 0.76 (95% CI: 0.67– 0.85), with a sensitivity of 72% and specificity of 74%.
Conclusion: D-dimer and NIHSS showed a significant positive correlation (r=0.58, P< 0.001), with an AUC of 0.76 for predicting poor prognosis. Independent risk factors included age, atrial fibrillation, and a history of TIA. These findings support the use of D-dimer as a critical biomarker in risk stratification for elderly stroke patients.
Keywords: elderly cerebral infarction, D-dimer, NIHSS score, prognosis assessment, risk factors
Introduction
As a prevalent cerebrovascular disease, cerebral infarction remains a leading cause of adult disability and mortality globally, particularly in aging populations where its incidence continues to rise.1,2 Effective prognosis assessment in elderly patients is therefore critical for optimizing clinical outcomes.
The National Institutes of Health Stroke Scale (NIHSS) serves as the gold standard for quantifying neurological deficits and predicting short-term prognosis.3 Concurrently, D-dimer - a fibrin degradation product reflecting thromboinflammatory status - has emerged as a promising prognostic biomarker.4 While existing studies suggest correlations between elevated D-dimer levels and unfavorable outcomes,5–7 significant limitations persist in elderly-focused research. Prior investigations often failed to account for critical confounders such as concurrent infections, malignancy, or renal dysfunction - all prevalent comorbidities in geriatric populations that may independently elevate D-dimer levels.8,9
Notably, the clinical translation of these biomarkers remains ambiguous. Current guidelines lack specific recommendations for D-dimer-guided therapeutic strategies in elderly stroke patients, particularly regarding anticoagulation intensity or duration. This knowledge gap may contribute to suboptimal risk stratification, as illustrated by recent trials showing 32% of elderly stroke patients with elevated D-dimer received delayed antithrombotic escalation.10
This study addresses three critical gaps: 1) Characterizing the D-dimer/NIHSS relationship specifically in elderly populations; 2) Evaluating six-month functional outcomes using modified Rankin Scale (mRS); 3) Controlling for confounders including atrial fibrillation, TIA history, and inflammatory comorbidities
Through multivariate analysis of 850 elderly patients with acute cerebral infarction, we aim to develop an age-specific prognostic model integrating biomarker profiles and clinical parameters. These findings could inform personalized monitoring protocols and therapeutic escalation criteria for this vulnerable population.
Data and Methods
This study was approved by the ethics committee of the First People’s Hospital of Hefei. All the methods were carried out in accordance with the Declaration of Helsinki. For the use of retrospective medical record data, the hospital ethics committee waived the written informed consent requirement for some patients. However, for all patients/family members involved in follow-up data collection, electronic informed consent was obtained through telephone interviews. The consent form template and audio recordings are archived at the hospital’s research data center, with a retention period of 15 years.
General Information
This study is a retrospective analysis conducted by reviewing the medical records of elderly patients with cerebral infarction admitted to our hospital from January 2022 to December 2023. A total of 112 eligible patients were included, comprising 64 males and 48 females. The age ranged from 65 to 89 years, with a mean age of 74.50 ± 7.12 years. Since the study design is a retrospective analysis and the onset of the disease is uniformly defined as within 72 hours prior to hospital admission, the age at the time of onset was not separately recorded. However, the age at admission can reflect the distribution of ages at the time of onset. All patients underwent a six-month follow-up, during which the modified Rankin Scale (mRS) was used for prognosis assessment. The mRS ranges from 0 (asymptomatic) to 6 (dead). According to the scoring results, patients were classified into two groups: scores of 0 to 2 were categorized as the good prognosis group (52 cases), and scores of 3 and above were categorized as the poor prognosis group (60 cases). Follow-up was conducted through outpatient visits or telephone interviews to ensure data integrity and accuracy. The inclusion and exclusion criteria for this study are outlined as follows:
Inclusion criteria: Age ≥ 65 years; Clinical diagnosis of cerebral infarction, diagnosed according to the “Chinese Guidelines for the Diagnosis and Treatment of Stroke” (2021 edition); Patients or their guardians could provide written informed consent; Onset of cerebral infarction occurred within 72 hours before admission; Complete medical records before admission and during follow-up, including CT or MRI-confirmed diagnosis of cerebral infarction; Complete baseline NIHSS score data available; Stable vital signs during the study period, without the need for intensive care.
Exclusion criteria: Age < 65 years; Concurrent presence of other central nervous system diseases, such as cerebral hemorrhage, brain tumors, myasthenia gravis, etc.; Severe cardiac, hepatic, renal dysfunction, or other major organ failure; Patients with a history of previous cerebral infarction but incomplete recovery; Presence of psychiatric disorders or cognitive dysfunction, rendering effective communication impossible; Receipt of other clinical trial drug treatments within the previous 3 months before the study initiation; Patients allergic to the drug components that might be used in the study; Patients with active inflammation, autoimmune diseases, or recent thrombotic events (such as deep vein thrombosis of the lower limbs) were excluded by screening the laboratory test records (eg, C-reactive protein, coagulation function indicators) and imaging reports from the three months prior to admission, through the electronic medical record system.
Methods
In this study, a comprehensive series of data collection and assessment methods were employed to ensure a thorough analysis of elderly patients with cerebral infarction. This included the collection of baseline data: detailed baseline data were collected for each selected elderly patient with cerebral infarction, including gender, age, body mass index (BMI), smoking and drinking habits. Additionally, patients’ medical histories, including hypertension, diabetes, coronary heart disease, atrial fibrillation, and transient ischemic attack (TIA), were meticulously recorded. All data were obtained by the admitting physician through face-to-face interviews and reviewing electronic medical records upon patient admission. Furthermore, two neurologists certified by the Chinese Stroke Society independently completed the NIHSS assessment within 6 hours of admission. If the difference between their scores exceeded 2 points, a third senior physician rechecked the results. The NIHSS scores range from 0 (no symptoms) to 42 (severe neurological deficits). Based on the scores, patients were categorized into three groups: mild neurological deficits (NIHSS score 1–4), moderate neurological deficits (NIHSS score 5–14), and severe neurological deficits (NIHSS score ≥15). Finally, biochemical measurements were conducted for all patients. On the morning following patient admission, fasting venous blood samples (3 mL) were collected from each patient for subsequent biochemical parameter testing. D-dimer Testing Standardization: The entire testing process followed the standards set by the International Society on Thrombosis and Haemostasis (ISTH). Prior to each batch of tests, internal quality control was conducted using the appropriate quality control materials (Sysmex CS-5100-specific quality control liquid, batch number 2021-REF-05), ensuring the coefficient of variation (CV) was <5%.
Statistical Analysis
Statistical analyses were performed using the SPSS software version 26.0 (IBM Corp., Armonk, NY, USA). First, descriptive statistical analysis was conducted for all patients’ baseline data. Continuous variables were expressed as mean ± standard deviation (SD), or median and interquartile range if the data distribution was non-normal. Categorical variables were expressed as frequencies (n) and percentages (%). Spearman correlation coefficient was used for non-parametric correlation analysis to evaluate the correlation between D-dimer levels and NIHSS scores. For comparisons between two or more groups, appropriate test methods were selected based on the distribution characteristics of the data. Independent sample t-tests were used for normally distributed continuous variables, while Mann–Whitney U-tests were used for non-normally distributed data. Between-group comparisons of categorical variables were conducted using chi-square tests or Fisher’s exact tests.Variable selection for regression followed STROBE guidelines: 1) Clinically established risk factors (age, NIHSS, etc.) were forced into the model; 2) Other variables required P<0.2 in univariate analysis for inclusion. Final model diagnostics showed Hosmer-Lemeshow P=0.32 indicating good fit. To explore the impact of D-dimer levels and other potential risk factors on poor prognosis, a multivariable logistic regression model was employed. In the multivariate logistic regression model, in addition to D-dimer and NIHSS scores, further adjustment was made for potential confounding factors that could affect prognosis, including NIHSS admission score, age, atrial fibrillation, history of transient ischemic attack (TIA), gender, smoking, drinking, diabetes, hypertension, and BMI. The significance level for all statistical tests was set at 0.05, and P < 0.05 was considered statistically significant.
Sample justification: Based on preliminary pilot data (α = 0.05, β = 0.20), the expected effect size of D-dimer on prognosis was set at an OR = 2.5. Using PASS 15.0 software, the required minimum sample size was calculated to be 98 cases. A total of 112 cases were ultimately included in this study, providing a statistical power of 82%, which meets the analysis requirements.
Results
Analysis of Patient Baseline Characteristics
Table 1 describes the baseline characteristics of elderly patients with cerebral infarction in this study. The mean age of the poor prognosis group was 76.90 years, significantly higher than that of the good prognosis group, which was 72.10 years (P < 0.05). There was no significant difference in gender distribution between the two groups (P = 0.108). The average BMI of the poor prognosis group was 27.36 kg/m², significantly higher than that of the good prognosis group, which was 25.38 kg/m². Smoking and drinking habits also showed statistical significance between the two groups (smoking: P = 0.015; drinking: P = 0.022), with a higher proportion of smokers and drinkers in the poor prognosis group. Regarding medical history, the distribution of hypertension, diabetes, and coronary heart disease did not reach statistical significance between the two groups. However, the history of atrial fibrillation and transient ischemic attack (TIA) was significantly higher in the poor prognosis group (atrial fibrillation: P = 0.025; history of TIA: P = 0.016). The NIHSS score upon admission showed significant differences between the two groups (P < 0.001), with a score of 6.85 ± 3.62 in the good prognosis group, significantly lower than that of 12.90 ± 6.88 in the poor prognosis group. D-dimer levels also showed significant differences between the two groups (P < 0.001), with an average level of 1.05 ± 0.48 in the poor prognosis group, higher than that of 0.65 ± 0.38 in the good prognosis group.
 |
Table 1 Baseline Characteristics of Patients |
Descriptive Statistics of NIHSS Scores and D-Dimer Levels
Based on the NIHSS scores, all patients were divided into categories of mild, moderate, and severe neurological deficits. The average D-dimer level for patients with mild neurological deficits was 0.49 ± 0.10 μg/mL. For patients with moderate neurological deficits, the average D-dimer level was 0.88 ± 0.25 μg/mL. Patients with severe neurological deficits had an average D-dimer level of 1.45 ± 0.35 μg/mL. The between-group F-value was 62.15, with P < 0.001, indicating significant differences in D-dimer levels among patients with different degrees of neurological deficits, as shown in Table 2.
 |
Table 2 Descriptive Statistics of NIHSS Scores and D-Dimer Levels |
Correlation Analysis Between NIHSS Scores and D-Dimer Levels
There is a significant positive correlation between NIHSS scores and D-dimer levels (Spearman r = 0.58, P < 0.001), as shown in Table 3.
 |
Table 3 Results of Spearman Correlation Analysis |
Multivariable Logistic Regression Analysis
Variables for multivariable logistic regression were selected through a two-step process: (1) Univariate screening with P<0.2 (The full list of variables, including gender, smoking, and others); (2) Clinical relevance based on prior stroke studies.11 Final model included 11 covariates as shown in Table 4. The multivariable logistic regression analysis reveals that for every 1 μg/mL increase in D-dimer levels, there is an 89% increase in the risk of poor prognosis for patients (OR = 1.89, 95% CI: 1.15–3.08, P = 0.012). Additionally, NIHSS scores, age, history of atrial fibrillation (AF), and history of transient ischemic attack (TIA) are also independent risk factors for poor prognosis (P < 0.05), as shown in Table 4.
 |
Table 4 Results of Multivariable Logistic Regression Analysis (Adjusted for Gender, Smoking, Drinking, Diabetes, Hypertension, BMI) |
ROC Curve Analysis to Evaluate the Effectiveness of D-Dimer Levels in Predicting Poor Prognosis in Elderly Patients with Cerebral Infarction
The area under the ROC curve (AUC) for predicting poor prognosis based on D-dimer levels is 0.76 (95% CI: 0.67–0.85), with a sensitivity of 72% and specificity of 74%, as shown in Table 5.
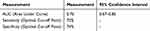 |
Table 5 Results of ROC Curve Analysis |
Discussion
With increasing age, elderly individuals experience gradual decline in physiological functions, often accompanied by various underlying conditions such as diabetes, hypertension, and hyperlipidemia.11 As age advances, the incidence and mortality risk of cerebral infarction gradually increase, thereby adding to the burden of social healthcare.12,13 Relevant studies indicate that elderly patients are more prone to impaired limb motor function following illness compared to younger patients, significantly affecting their ability to perform activities of daily living. Thus, preventive and therapeutic measures tailored to the elderly population are particularly crucial.14,15
This study demonstrated that elevated D-dimer levels are independently associated with adverse prognosis in elderly cerebral infarction patients (OR=1.89, 95% CI 1.15–3.08). These findings extend previous biomarker research by specifically highlighting age-related pathophysiology. This disparity may stem from age-related endothelial dysfunction and impaired fibrinolytic regulation, suggesting that D-dimer elevation in older adults reflects both thrombotic burden and systemic vascular aging. Our findings are consistent with previous research that also highlights the prognostic value of D-dimer in stroke patients. For instance, Yuan et al’s study16 suggests that an increase in D-dimer levels is associated with an increased risk of overall stroke and ischemic stroke, but not with the risk of hemorrhagic stroke. Additionally, elevated D-dimer levels are associated with increased risk of all-cause mortality, recurrence within 5 days, and functional disability within 90 days. Another study by Zi et al15 found a significant correlation between increased D-dimer levels and the severity of stroke (based on NIHSS scores) and increased infarct volume.
The observed D-dimer/NIHSS correlation aligns with emerging evidence of thromboinflammatory mechanisms in stroke progression. Elevated D-dimer may not only indicate hypercoagulability but also serve as a surrogate for silent microthrombosis and blood-brain barrier disruption – processes exacerbated by comorbidities like diabetes prevalent in elderly populations.17 This dual role could explain its superior prognostic performance (AUC=0.76) over traditional inflammatory markers like CRP, particularly when combined with NIHSS in multimodal prediction (AUC=0.82). Clinically, integrating D-dimer into existing risk stratification protocols could enable: Early identification of high-risk patients for intensified anticoagulation monitoring; Personalized rehabilitation planning through BMI-stratified interventions (threshold: >27.36 kg/m²); Dynamic treatment adjustment via serial D-dimer measurements during follow-up.
Age, atrial fibrillation (AF), and history of transient ischemic attack (TIA) have also been confirmed as independent risk factors for adverse prognosis. Elderly patients often have multiple chronic diseases and physiological decline, which may explain why advanced age is an important predictor of poor prognosis. AF, as a pathological factor for cerebral infarction, increases the risk of stroke by forming cardioembolic thrombi, potentially leading to more severe neurological deficits. TIA history has been identified as an independent risk factor for cardiovascular disease in multiple studies. Li et al’s study18 showed that older AF patients have poorer prognosis during the early recovery phase of cerebral infarction, with a 1.031-fold increase in the risk of adverse prognosis for each additional year. While confirming atrial fibrillation and TIA history as independent risk factors, our findings challenge the assumption that age alone drives poor outcomes. Multivariable analysis revealed that D-dimer remained predictive even after adjusting for age (β=0.41, p<0.01), implying modifiable thrombotic pathways exist even in advanced age. This contrasts with Loffredo et al’s19 emphasis on homocysteine, suggesting complementary biomarker panels may be needed for comprehensive risk assessment.
This study has several limitations. First, as a single-center retrospective design, it may introduce regional selection bias, and future multi-center prospective cohort studies are needed for validation. Second, although we adjusted for major confounders, we did not systematically record medications affecting coagulation, such as anticoagulants, which could have influenced D-dimer measurements and prognosis. Additionally, competing risks from comorbidities, like cancer, were not analyzed, which could impact the interpretation of our findings. Furthermore, unmeasured factors such as genetic predisposition (eg, F5 Leiden mutation) and socioeconomic status may partially account for the observed outcome variances.
Conclusion
In summary, D-dimer and NIHSS scores are important indicators for assessing the severity of neurological deficits and prognosis in elderly patients with cerebral infarction. The combined use of these biomarkers and clinical scores can provide a scientific basis for risk stratification and management of patients. Future research should focus on the application effectiveness of these indicators in different populations and optimization strategies in clinical practice to further improve prognosis assessment and treatment outcomes for stroke patients. Additionally, further research should explore how to reduce adverse prognosis in high-risk patients through early intervention and how to use these biomarkers and scoring systems to guide the development of personalized treatment plans.
Disclosure
The author declares no conflicts of interest in this work.
References
1. Abbas NI, Sayed O, Samir S, Abeed N. D-dimer level is correlated with prognosis, infarct size, and NIHSS in acute ischemic stroke patients. Indian J Crit Care Med. 2021;25(2):193. doi:10.5005/jp-journals-10071-23744
2. Delgado P, Alvarez-Sabin J, Abilleira S, et al. Plasma d-dimer predicts poor outcome after acute intracerebral hemorrhage. Neurology. 2006;67(1):94–98. doi:10.1212/01.wnl.0000223349.97278.e0
3. Hou H, Xiang X, Pan Y, Li H, Meng X, Wang Y. Association of level and increase in D‐Dimer with All‐Cause death and poor functional outcome after ischemic stroke or transient ischemic attack. J Am Heart Assoc. 2021;10(3):e018600. doi:10.1161/JAHA.120.018600
4. Jin T, Chen D, Chen Z, et al. Post-Thrombolytic D-Dimer elevation predicts symptomatic intracranial hemorrhage and poor functional outcome after intravenous thrombolysis in acute ischemic stroke patients. Neuropsychiatr Dis Treat. 2022;18:2737–2745. doi:10.2147/NDT.S389469
5. Liu Y, Li F, Sun H, et al. Combined prognostic significance of D-dimer level and platelet count in acute ischemic stroke. Thrombosis Res. 2020;194:142–149. doi:10.1016/j.thromres.2020.05.021
6. Park Y-W, Koh E-J, Choi H-Y. Correlation between serum D-dimer level and volume in acute ischemic stroke. J Korean Neurosurg Soc. 2011;50(2):89. doi:10.3340/jkns.2011.50.2.89
7. Ramos-Pachón A, López-Cancio E, Bustamante A, et al. D-dimer as predictor of large vessel occlusion in acute ischemic stroke. Stroke. 2021;52(3):852–858. doi:10.1161/STROKEAHA.120.031657
8. Sato T, Sato S, Yamagami H, et al. D-dimer level and outcome of minor ischemic stroke with large vessel occlusion. J Neurol Sci. 2020;413:116814. doi:10.1016/j.jns.2020.116814
9. Wang J, Ning R, Wang Y. Plasma D-dimer level, the promising prognostic biomarker for the acute cerebral infarction patients. J Stroke Cerebrovascular Dis. 2016;25(8):2011–2015. doi:10.1016/j.jstrokecerebrovasdis.2015.12.031
10. Wang Y, Hafeez A, Meng F, et al. The correlation of D-dimer levels with patient outcomes in acute ischemic cerebrovascular disease complicating coronary heart disease. Neurological Res. 2016;38(6):524–532. doi:10.1080/01616412.2016.1187829
11. Yang X-Y, Gao S, Ding J, Chen Y, Zhou X-S, Wang J-E. Plasma D-dimer predicts short-term poor outcome after acute ischemic stroke. PLoS One. 2014;9(2):e89756. doi:10.1371/journal.pone.0089756
12. Yao T, Tian B-L, Li G, et al. Elevated plasma D-dimer levels are associated with short-term poor outcome in patients with acute ischemic stroke: a prospective, observational study. BMC Neurol. 2019;19:1–8. doi:10.1186/s12883-019-1386-3
13. Ye N, Liu Z, Wang X, Xu X, Wu W. Evaluation of analytic and clinical performance of thrombin–antithrombin complex and d-dimer assay in prognosis of acute ischemic stroke. Blood Coagul Fibrinolysis. 2020;31(5):303–309. doi:10.1097/MBC.0000000000000915
14. Yuan W, Shi Z-H. The relationship between plasma D-dimer levels and outcome of Chinese acute ischemic stroke patients in different stroke subtypes. J Neural Transm. 2014;121:409–413. doi:10.1007/s00702-013-1113-y
15. Zi W-J, Shuai J. Plasma D-dimer levels are associated with stroke subtypes and infarction volume in patients with acute ischemic stroke. PLoS One. 2014;9(1):e86465. doi:10.1371/journal.pone.0086465
16. Yuan B, Yang T, Yan T, Cheng W, Bu X. Relationships between D-Dimer levels and stroke risk as well as adverse clinical outcomes after acute ischemic stroke or transient ischemic attack: a systematic review and meta-analysis. Front Neurol. 2021;12. doi:10.3389/fneur.2021.670730
17. Wirasman P, Machin A, Harumi J. D-Dimer levels as a predictor of clinical outcome and mortality in acute ischemic stroke patients: a systematic review and meta-analysis. AKSONA. 2023;3:100–110. doi:10.20473/aksona.v3i2.44770
18. Li S, Zhao X, Wang C, et al. Risk factors for poor outcome and mortality at 3 months after the ischemic stroke in patients with atrial fibrillation. J Stroke Cerebrovasc Dis. 2013;22(8):e419–25. doi:10.1016/j.jstrokecerebrovasdis.2013.04.025
19. Loffredo L, Violi F, Fimognari F, et al. The association between hyperhomocysteinemia and ischemic stroke in patients with non-valvular atrial fibrillation. Haematologica. 2005;90(9):1205–1211.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Clinical Characteristics of Asymptomatic Thromboembolism in Psychiatric Inpatients: A Retrospective Study
Geng Y, Zhang P, Pan Y, Wang H, Chen Y, Lai J, Hu S
Neuropsychiatric Disease and Treatment 2024, 20:515-522
Published Date: 7 March 2024
Risk Factors for Digital Replantation Failure: A Nomogram Prediction Model
Guo T, Ma T, Gao R, Yu K, Bai J
Therapeutics and Clinical Risk Management 2024, 20:929-937
Published Date: 27 December 2024

