Back to Journals » Clinical Ophthalmology » Volume 19
Demographic Profile and Clinical Characteristics of Fuchs Endothelial Corneal Dystrophy in Thai Patients: A Retrospective Cohort in a Tertiary Referral Center
Authors Wannapanich T, Puangsricharern V , Satitpitakul V, Kittipibul T, Suphapeetiporn K
Received 30 September 2024
Accepted for publication 20 December 2024
Published 6 January 2025 Volume 2025:19 Pages 45—57
DOI https://doi.org/10.2147/OPTH.S498122
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Trakanta Wannapanich,1,2 Vilavun Puangsricharern,1,3 Vannarut Satitpitakul,1,3 Thanachaporn Kittipibul,1,3 Kanya Suphapeetiporn4– 6
1Center of Excellence for Cornea and Stem Cell Transplantation, Department of Ophthalmology, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand; 2Excellence Center for Cornea and Stem Cell Transplantation, Department of Ophthalmology, King Chulalongkorn Memorial Hospital, Thai Red Cross Society, Bangkok, Thailand; 3Department of Ophthalmology, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand; 4Department of Pediatrics, Faculty of Medicine, Chulalongkorn University Bangkok, Bangkok, Thailand; 5Excellence Center for Genomics and Precision Medicine, King Chulalongkorn Memorial Hospital, The Thai Red Cross Society, Bangkok, Thailand; 6Center of Excellence for Medical Genomics, Department of Pediatrics, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
Correspondence: Vilavun Puangsricharern, Department of Ophthalmology, Faculty of Medicine, Chulalongkorn University, 1873, Rama 4 Road, Pathumwan, Bangkok, 10330, Thailand, Email [email protected] Kanya Suphapeetiporn, Department of Pediatrics, Faculty of Medicine, Chulalongkorn University, 1873, Rama 4 Road, Pathumwan, Bangkok, 10330, Thailand, Email [email protected]
Purpose: To describe the demographic profile, clinical characteristics, and treatment trends of Fuchs endothelial corneal dystrophy (FECD) in Thai patients, reflecting the evolving landscape of corneal transplantation in this region.
Patients and Methods: This retrospective cohort study included 900 patients (1,743 eyes) diagnosed with FECD at a tertiary referral center in Thailand between January 2017 and June 2023. Demographic, clinical, and surgical data were analyzed, focusing on best-corrected visual acuity (BCVA), central corneal thickness (CCT), endothelial cell density (ECD), surgical interventions, and graft survival rate.
Results: The mean age was 63.9 years, with 77.2% of patients being female. Most eyes were classified as Adamis grade I (83.7%). Diabetes mellitus and hypertension were prevalent in 17.4% and 38.6% of patients, respectively. The rate of corneal transplantation was 8.1%, with DMEK accounting for 69.3% of transplants. Graft survival rates were 94.3% at 1 year and 76.2% at 5 years. The average post-operative ECD declined from 1667.8 ± 668.0 cells/mm² at 1 year to 1140.7 ± 684.4 cells/mm² at 5 years. Cataract surgery was performed in 20.4% of phakic eyes, with only 2.2% requiring corneal transplantation within five years.
Conclusion: FECD in Thailand, as reflected by this large cohort, predominantly presents at an early stage, allowing for conservative management. The growing use of DMEK highlights the shift towards less invasive procedures, mirroring global trends in Southeast Asia. These findings emphasize the importance of advancing surgical techniques and improving eye banking practices in the region.
Keywords: corneal transplantation, endothelial keratoplasty, DMEK, keratoplasty trends, eye banking
Introduction
Fuchs endothelial corneal dystrophy (FECD) is a progressive corneal disease characterized by endothelial cell loss and the accumulation of guttae on the inner corneal layer, leading to corneal edema and visual deterioration.1 The disease is influenced by both genetic and environmental factors, particularly oxidative stress, which plays a central role in the progressive endothelial damage observed in FECD.1 Most cases manifest in the fifth or sixth decade of life, with late-onset FECD being the predominant form.1
While the prevalence of FECD varies significantly across different populations, this study did not aim to determine the prevalence. However, existing data suggests a higher prevalence in Caucasians compared to Asian populations, with significant variability even among different Asian ethnicities.2,3 For example, Chinese Singaporeans show a higher prevalence of FECD (6.7%) compared to Japanese and Indian populations.4–6 In Thailand, a previous study reported genetic differences in FECD patients compared to Caucasians, highlighting the ethnic variability in the disease’s manifestation.7
Corneal transplantation remains the definitive treatment for advanced FECD, with endothelial keratoplasty (EK) now preferred due to its faster recovery and lower complication rates compared to penetrating keratoplasty (PK).8 However, PK remains prevalent in some regions, including parts of Southeast Asia, where resource constraints and limited surgical expertise influence treatment options.1,9 Understanding regional patterns in FECD management is crucial, particularly given the increasing demand for corneal transplants and the long waiting periods for corneal donors in Thailand.
This study, which involves one of the largest cohorts of FECD patients in Thailand, provides critical insights into the clinical characteristics and demographic profile of this population. The findings reflect trends in corneal transplantation and patient management in Southeast Asia, where corneal donor shortages and evolving surgical techniques play a key role in treatment decisions. By identifying key clinical features of FECD, this study aims to support decision-making in the allocation of corneal transplantation resources and improve the care of patients with this debilitating disease.
Materials and Methods
Study Design and Setting
This single-center, retrospective cohort study was conducted at the Department of Ophthalmology and the Excellence Center for Cornea and Limbal Stem Cell Transplantation, King Chulalongkorn Memorial Hospital, Bangkok, Thailand. The study was approved by the hospital’s Institutional Review Board (IRB No. 0590/66, Certificate of Approval No. 1238/2023) and adhered to the principles of the Declaration of Helsinki. The study collected the data from January 2017 to June 2023.
Study Population
Patients were identified from hospital-based electronic medical records (EMR) between January 2017 and June 2023.
The inclusion criteria were:
- All patients who received a definite diagnosis of FECD by a corneal specialist and presented in the outpatient clinic during the study period.
Exclusion criteria were:
- Eyes with a history of prior keratoplasty at the time of first presentation.
- Eyes with a history of topical medication that could affect corneal endothelial health, such as rho kinase inhibitors.
- Eyes with a history of intraocular surgery or intraocular laser, including laser iridotomy (only excluded from the corneal endothelial cell count analysis).
Operational Definitions
- FECD Diagnosis: The diagnosis of FECD was made based on slit-lamp biomicroscopy findings, specifically the presence of corneal guttae, and/or confirmed through specular microscopy. In cases where corneal edema or decompensation was present, diagnosis was confirmed if corneal guttae were detected in the contralateral eye or if histopathology supported the diagnosis.
- Disease Progression: Progression of FECD was defined by clinical indicators such as increased central corneal thickness (CCT) leading to significant visual impairment, the development of bullous keratopathy, or a marked reduction in endothelial cell density (ECD) that raised concerns for intraocular surgery.
- Candidates for Corneal: Transplantation: Eligibility for corneal transplantation required donor allocation from the Thai Red Cross Eye Bank (TRCEB), patient readiness for surgery, and consent for the procedure.
Data Collection
Approval to access and use data from the Thai Red Cross Eye Bank (TRCEB) and the Chulalongkorn Corneal Registration System (CUCRS) was obtained, ensuring adherence to data privacy and confidentiality protocols. No informed consent process was done as the study involved retrospective data collection. Data were collected and recorded in a manner that ensured subjects could not be identified. The collected data included demographic information (age, gender, systemic diseases) and clinical data from both eyes (visual acuity, intraocular pressure, lens status, central corneal thickness [CCT], endothelial cell density [ECD]). Disease severity was graded using the Adamis grading system (Table 1). In cases where the medical record used the modified Krachmer (MK) grading system, the severity was converted to align with the Adamis system for consistency.
 |
Table 1 Adamis’ Grading of Fuchs Endothelial Corneal dystrophy |
 |
Table 2 Demographic Profiles and Systemic Comorbidities of FECD Patients |
 |
Table 3 Clinical Characteristics of FECD Patients at the Initial Visit |
 |
Table 4 Annual Changes in Central Corneal Thickness and Endothelial Cell Density by FECD Stage |
 |
Table 5 Surgical Interventions in Phakic and Pseudophakic Eyes with FECD |
Details regarding corneal transplantation, such as the date of donor request, surgery type, and related data, were retrieved from the Thai Red Cross Eye Bank (TRCEB) and the Chulalongkorn Corneal Registration System (CUCRS).
Statistical Analysis
Descriptive statistics were used to summarize the demographic and clinical characteristics of FECD patients. Categorical variables were presented as frequencies and percentages, while continuous variables were summarized as means with standard deviations or medians with interquartile ranges (IQR), depending on the data distribution. Normality was assessed using visual inspection of histograms and descriptive statistics.
Comparisons between groups (such as different grades of disease severity or corneal transplantation status) were performed using chi-square tests for categorical variables and independent sample t-tests or Mann–Whitney U-tests for continuous variables, as appropriate. A p-value of <0.05 was considered statistically significant. Missing data were handled by excluding the affected variables from analysis, with the proportion of missing data reported where applicable.
Results
Demographics
A total of 900 patients (1,743 eyes) were included in the study. The mean age of the cohort was 63.94 years (±11.47), with an age range of 11 to 95 years. The sex distribution showed that 77.2% of patients were female (n=695) and 22.8% male (n=205). In terms of home location, 67.0% of patients (n=603) resided in Bangkok, while the remaining 33.0% (n=297) were from outside Bangkok. Systemic comorbidities included diabetes mellitus (17.4%) and hypertension (38.6%), as outlined in Table 2. A family history of FECD was reported in 9.1% of patients.
Baseline Clinical Characteristics
The baseline clinical characteristics were analyzed for the entire cohort of 1,743 eyes. The median best-corrected visual acuity (BCVA) was 0.2 LogMAR, with 81.23% of eyes having a BCVA of better than 20/63, while 5.06% had a BCVA worse than 20/200. The mean intraocular pressure (IOP) was 13.09 ± 3.38 mmHg. Glaucoma was present in 8.95% of eyes, and 27.83% had a history of prior intraocular surgery or laser procedures. Most eyes (83.71%) were classified as Adamis’ grade I. The mean central corneal thickness (CCT) was 565.04 ± 59.58 µm, and the mean endothelial cell density (ECD) was 2086.96 ± 639.99 cells/mm². Table 3 summarizes the clinical characteristics at baseline.
Clinical Course
Table 4 presents detailed annual changes in central corneal thickness (CCT) and endothelial cell density (ECD) over a 5-year follow-up period. Due to the high rate of surgical intervention, particularly cataract surgeries, only eyes without prior surgical interventions were included in this analysis to capture the natural progression of FECD. Most eyes classified as Adamis’ grade I showed stable ECD values over time, while Adamis’ grade II eyes exhibited a progressive decline in ECD, particularly after the first year. The percentage change in CCT and ECD for different stages of the disease is summarized in Table 4.
Disease Management
A total of 20.4% of phakic eyes (n=1,345) underwent cataract surgery during the follow-up period, with 6 eyes (2.2%) requiring corneal transplantation within five years. Pseudophakic eyes (n=394) had a higher rate of corneal transplantation (16.2%), with DMEK being the most common procedure (57.8%), followed by PK at 18.8%. Combined surgeries, particularly “Triple-DMEK” (corneal transplantation with DMEK), were performed in 96.5% of cases. The breakdown of surgical interventions for phakic and pseudophakic eyes is summarized in Table 5.
Cumulative Incidence of Corneal Transplantation
To evaluate the cumulative incidence of corneal transplantation, we focused on the 1,241 eyes diagnosed after 2017, for which complete follow-up data were available. A total of 8.1% of these eyes underwent corneal transplantation within the 5-year follow-up period. Among these, 26% received donor tissue from international sources, highlighting the reliance on imported donor tissue due to the limited availability of domestic donors. The cumulative incidence of corneal transplantation over time is shown in Figure 1.
 |
Figure 1 Cumulative incidence of corneal transplantation over time. |
Corneal Transplantation Trends
Between January 2017 and June 2023, 215 eyes underwent corneal transplantation at our institution, with 29 eyes (13.5%) receiving imported donor tissue. DMEK was the most common procedure, increasing from 26.3% of corneal transplants in 2017 to 90.9% in 2023, reflecting the growing preference for this less invasive method. The use of PK decreased from 15.8% to 9.1% during the same period, and Descemet stripping automated endothelial keratoplasty (DSAEK) was phased out entirely by 2023. Figures 2 and 3 illustrate the distribution of corneal transplantation procedures over time.
 |
Figure 2 Annual distribution of corneal transplantation procedures by type. |
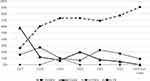 |
Figure 3 Percentage of corneal transplantation procedures by type. |
Corneal Transplantation Outcomes
A total of 215 corneal transplantations were performed. Graft survival rates were 94.8% at 6 months, 94.3% at 1 year, 91.8% at 2 years, 86.9% at 3 years, 83.6% at 4 years, and 76.2% at 5 years. These data are illustrated in Figure 4.
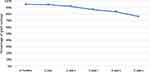 |
Figure 4 Graft survival rates over time following corneal transplantation. |
The average post-operative ECD decreased progressively over time. At 6 months, the average ECD was 1,707.6 ± 603.9 cells/mm², reducing to 1,667.8 ± 668.0 cells/mm² at 1 year, and further declining to 1,140.7 ± 684.4 cells/mm² at 5 years. These trends are presented in Figure 5.
 |
Figure 5 Average endothelial cell density over time after corneal transplantation. |
Donor Registration Data
Among the 1,241 eyes included in the cumulative incidence analysis, 67.4% registered for a corneal donor request during the 5-year follow-up period. The majority of registrations occurred at the first presentation visit (84.8%). Despite this, 45.6% of eyes remained on the waiting list by the final follow-up visit, underscoring the challenges posed by corneal donor shortages. Figure 6 presents the percentage of donor registrations by year of follow-up.
 |
Figure 6 Percentage of corneal donor registrations by year of follow-up since initial presentation. |
Discussion
FECD is a bilateral, progressive disorder characterized by corneal endothelial cell loss, guttae formation, and eventual stromal edema, which can significantly impair vision.1 Our study analyzed the demographic profiles, clinical characteristics, and treatment decisions in a cohort of 900 Thai FECD patients (1,743 eyes). This data is particularly valuable given the limited reports on FECD in Southeast Asian populations, and it provides new insights into the disease progression and management in this region.
Consistent with global findings, FECD was more prevalent in women, though the reasons behind this gender preference remain unclear.1 The mean age of diagnosis in our cohort was 63.8 years, aligning with reports from other Asian populations, such as India (59–62 years) and Japan (62.8 years).3,5,11,12 This supports the predominance of late-onset FECD, which typically begins in the fifth decade of life and progresses over subsequent decades.
One notable finding in our cohort was the high prevalence of systemic comorbidities. Diabetes mellitus (DM) affected 17.4% of patients, a higher rate than reported in Mexican (11.8%) and US (12%) studies.13,14 Hypertension was also prevalent in 38.6% of our patients. These findings underscore the importance of monitoring systemic comorbidities in FECD patients, as conditions like DM and hypertension may exacerbate endothelial dysfunction and accelerate disease progression.15,16
In terms of visual function, most eyes presented with early-stage FECD, as reflected by the high proportion of eyes classified as Adamis grade I (83.7%). The majority of FECD diagnoses were incidental, detected during routine check-ups or pre-operative cataract assessments. Early detection allows for appropriate planning of cataract surgery, a frequent intervention in this patient group. Only a small proportion of eyes were categorized as Adamis grade II or higher, and these more advanced cases were more likely to require corneal transplantation. Our data reinforces the importance of early detection and regular monitoring in managing FECD.
The progression of FECD was assessed through endothelial cell density (ECD) and central corneal thickness (CCT) over a five-year follow-up period. In early-stage FECD (Adamis grade I), a measurable decline in ECD was observed, but average ECD values remained above 2,000 cells/mm² after five years, indicating slow progression in many cases. However, more advanced disease (Adamis grade II or higher) was associated with lower baseline ECD and higher CCT, often leading to corneal transplantation. These findings align with previous studies that highlight the importance of ECD and CCT monitoring to determine the appropriate timing for surgical intervention.17
The rate of corneal transplantation in our study (8.1% over five years) was consistent with other studies reporting rates between 4.4% and 21%.3,13,14,18 DMEK was the most common procedure, accounting for 69.3% of cases, reflecting the global shift toward endothelial keratoplasty (EK) due to its superior visual outcomes and quicker recovery time compared to PK.19,20 This mirrors the global trend in regions such as the United States, Europe, and Singapore.19–22
Cataract surgery was also a key intervention in our cohort, with 20.4% of phakic eyes undergoing the procedure. Only 2.2% of these eyes required corneal transplantation within five years, suggesting that cataract surgery can effectively delay the need for keratoplasty in early-stage FECD.23 For more advanced cases, combined procedures, such as “Triple-DMEK” (corneal transplantation with DMEK and cataract surgery), were frequently performed, accounting for 73.1% of combined surgeries. Surgical decisions, as noted, depended on multiple factors, including cataract density, endothelial cell density, corneal thickness, graft waiting time, and both patient and surgeon preference. Patients with a preoperative central corneal thickness > 640 μm and/or an endothelial cell density < 1000 cells/mm² are at high risk of corneal decompensation following cataract surgery alone, as previously reported.23 These thresholds are typically used to guide discussions with patients about surgical options. However, variability in decision-making among surgeons remains a study limitation. This approach offers several advantages, including reducing the number of surgeries and overall healthcare costs, particularly for patients with advanced disease.24,25
Our study demonstrated a 5-year graft survival rate of 76.2%, which is lower than rates reported in other studies but reflects the inclusion of both PK and EK in our cohort.26–29 Dunker et al reported better 2-year graft survival for PK (97%) and DSAEK (93%) compared to DMEK (71%) in the European Cornea and Cell Transplantation Registry, highlighting variability in outcomes among different techniques.26 Similarly, Ang et al found superior 5-year survival for DSAEK over PK in Asian eyes with FECD and bullous keratopathy in the Singapore Corneal Transplant Registry.27 These findings suggest that while PK remains a viable option, EK techniques like DSAEK and DMEK generally yield better long-term outcomes, particularly in developed settings with standardized surgical techniques. Our study’s lower survival rates may reflect our inclusion of PK cases and the limited number of patients with long-term follow-up. However, the increasing trend toward EK in our population is expected to enhance graft survival rates in future reports. Further research with larger cohorts and extended follow-up is essential to validate these observations and explore additional factors influencing survival outcomes.
The corneal tissue shortage in Thailand presents a significant challenge, with average waiting times for non-urgent corneal transplantation ranging from 3 to 4 years. In our cohort, only 8.8% of eyes that registered for donor tissue received a transplant within the five-year follow-up period. The long waiting times contribute to early registration for donation, even when immediate surgery is not necessary, potentially burdening the eye banking system. Refining the criteria for donor registration could help reduce unnecessary registrations and alleviate strain on the system.
This study has several limitations. Its retrospective nature may introduce selection bias, particularly if patients with different clinical outcomes did not return for follow-up. Additionally, missing data were excluded from the analysis, which could affect the generalizability of the findings if the data were not missing completely at random. Lastly, the study’s focus on a Southeast Asian population means that the findings may not be fully applicable to other populations with different genetic and environmental factors. Despite these limitations, the study provides important insights into the management and progression of FECD in Thailand.
Conclusion
This study provides a comprehensive analysis of the demographic profile and clinical characteristics of FECD in Thai patients. It highlights the high prevalence of systemic comorbidities and the predominance of early-stage FECD, allowing for conservative management in many cases. The increasing use of DMEK, mirroring global trends toward less invasive surgical interventions, emphasizes the evolving treatment landscape in Southeast Asia. These findings underscore the need for continued advancements in surgical techniques and improved eye banking practices to address corneal tissue shortages in the region.
Acknowledgments
We gratefully acknowledge the 90th Anniversary of Chulalongkorn University Fund (Ratchadapisek Sompoch Endowment Fund), H.M. King Bhumibol Adulyadej’s 72nd Birthday Anniversary Fund, and the Faculty of Medicine, Chulalongkorn University for their support. We also extend our sincere thanks to the Thai Red Cross Eye Bank under the Thai Red Cross Society for providing essential data.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ong Tone S, Kocaba V, Böhm M, Wylegala A, White TL, Jurkunas UV. Fuchs endothelial corneal dystrophy: the vicious cycle of Fuchs pathogenesis. Prog Retinal Eye Res. 2021;80:100863. doi:10.1016/j.preteyeres.2020.100863
2. Soh YQ, Kocaba V, Pinto M, Mehta JS. Fuchs endothelial corneal dystrophy and corneal endothelial diseases: east meets West. Eye. 2020;34(3):427–441. doi:10.1038/s41433-019-0497-9
3. Das A, Chaurasia S. Clinical profile and demographic distribution of Fuchs’ endothelial dystrophy: an electronic medical record–driven big data analytics from an eye care network in India. Indian J Ophthalmol. 2022;70(7):2415. doi:10.4103/ijo.IJO_755_22
4. Kitagawa K, Kojima M, Sasaki H, et al. Prevalence of Primary Cornea guttata and Morphology of Corneal Endothelium in Aging Japanese and Singaporean Subjects. Ophthalmic Res. 2002;34(3):135–138. doi:10.1159/000063656
5. Higa A. Prevalence of and Risk Factors for Cornea Guttata in a Population-Based Study in a Southwestern Island of Japan: the Kumejima Study. Arch Ophthalmol. 2011;129(3):332. doi:10.1001/archophthalmol.2010.372
6. Nagaki Y, Hayasaka S, Kitagawa K, Yamamoto S. Primary cornea guttata in Japanese patients with cataract: specular microscopic observations. Jpn J Ophthalmol. 1996;40(4):520–525.
7. Okumura N, Puangsricharern V, Jindasak R, et al. Trinucleotide repeat expansion in the transcription factor 4 (TCF4) gene in Thai patients with Fuchs endothelial corneal dystrophy. Eye. 2020;34(5):880–885. doi:10.1038/s41433-019-0595-8
8. Matthaei M, Hribek A, Clahsen T, Bachmann B, Cursiefen C, Jun AS. Fuchs Endothelial Corneal Dystrophy: clinical, Genetic, Pathophysiologic, and Therapeutic Aspects. Annu Rev Vis Sci. 2019;5(1):151–175. doi:10.1146/annurev-vision-091718-014852
9. Kocaba V, Oellerich S, Melles GRJ. Toward a Paradigm Shift in the Therapeutic Approach to Fuchs Endothelial Corneal Dystrophy. JAMA Ophthalmol. 2021;139(4):431. doi:10.1001/jamaophthalmol.2020.7041
10. Adamis AP, Filatov V, Tripathi BJ, Tripathi RC. Fuchs’ endothelial dystrophy of the cornea. Surv Ophthalmol. 1993;38(2):149–168. doi:10.1016/0039-6257(93)90099-s
11. Das AV, Chaurasia S. Clinical Profile and Demographic Distribution of Corneal Dystrophies in India: a Study of 4198 Patients. Cornea. 2021;40(5):548–553. doi:10.1097/ICO.0000000000002450
12. Bhadra P, Sahoo S, Sahu S, Priyadarshini S, Mohanty A, Das S. Demographic profile and clinical characteristics of Fuchs’ endothelial corneal dystrophy in a tertiary eye care center. Indian J Ophthalmol. 2023;71(2):505. doi:10.4103/ijo.IJO_1288_22
13. Goldberg R, Raza S, Walford E, Feuer W, Goldberg J. Fuchs endothelial corneal dystrophy: clinical characteristics of surgical and nonsurgical patients. OPTH. 2014;1761. doi:10.2147/OPTH.S68217
14. Barrera-Sanchez M, Hernandez-Camarena JC, Ruiz-Lozano RE, Valdez-Garcia JE, Rodriguez-Garcia A. Demographic profile and clinical course of Fuchs endothelial corneal dystrophy in Mexican patients. Int Ophthalmol. 2022;42(4):1299–1309. doi:10.1007/s10792-021-02117-0
15. Zwingelberg SB, Lautwein B, Baar T, et al. The influence of obesity, diabetes mellitus and smoking on fuchs endothelial corneal dystrophy (FECD). Sci Rep. 2024;14(1):11596. doi:10.1038/s41598-024-61948-w
16. Nealon CL, Halladay CW, Gorman BR, et al. Association Between Fuchs Endothelial Corneal Dystrophy, Diabetes Mellitus, and Multimorbidity. Cornea. 2023;42(9):1140–1149. doi:10.1097/ICO.0000000000003311
17. Gain P, Jullienne R, He Z, et al. Global Survey of Corneal Transplantation and Eye Banking. JAMA Ophthalmol. 2016;134(2):167. doi:10.1001/jamaophthalmol.2015.4776
18. Heckenlaible NJ, Dun C, Prescott C, et al. Predictors of Receiving Keratoplasty for Fuchs’ Endothelial Corneal Dystrophy among Medicare Beneficiaries. Ophthalmology. 2022;2022:S0161642022005899. doi:10.1016/j.ophtha.2022.07.030.
19. Xiao G, Tsou BC, Soiberman US, Prescott CR, Srikumaran D, Woreta FA. Keratoplasty in the United States: trends and Indications From 2015 to 2020. Cornea. 2023;42(11):1360–1364. doi:10.1097/ICO.0000000000003180
20. Bigan G, Puyraveau M, Saleh M, et al. Corneal transplantation trends in France from 2004 to 2015: a 12-year review. European Journal of Ophthalmology. 2018;28(5):535–540. doi:10.1177/1120672118762224
21. Keane M, Coffey N, Jones V, Lawson C, Mills R, Williams K. The Australian Corneal Graft Registry: 2021/22 Report. Flinders Univ. 2022;2022:380. doi:10.25957/9VYP-0J93
22. Tan D, Ang M, Arundhati A, Khor WB. Development of Selective Lamellar Keratoplasty within an Asian Corneal Transplant Program: the Singapore Corneal Transplant Study (An American Ophthalmological Society Thesis). Trans Am Ophthalmol Soc. 2015;113:T10.
23. Moshirfar M, Huynh R, Ellis JH. Cataract surgery and intraocular lens placement in patients with Fuchs corneal dystrophy: a review of the current literature. Curr Opin Ophthalmol. 2022;33(1):21–27. doi:10.1097/ICU.0000000000000816
24. Agha B, Ahmad N, Dawson DG, Kohnen T, Schmack I. Refractive outcome and tomographic changes after Descemet membrane endothelial keratoplasty in pseudophakic eyes with Fuchs’ endothelial dystrophy. Int Ophthalmol. 2021;41(8):2897–2904. doi:10.1007/s10792-021-01850-w
25. Romano V, Passaro ML, Bachmann B, et al. Combined or sequential DMEK in cases of cataract and Fuchs endothelial corneal dystrophy—A systematic review and meta‐analysis. Acta Ophthalmologica. 2024;102(1). doi:10.1111/aos.15691
26. Dunker SL, Armitage WJ, Armitage M, et al. Outcomes of corneal transplantation in Europe: report by the European Cornea and Cell Transplantation Registry. J Cataract Refract Surg. 2021;47(6):780–785. doi:10.1097/j.jcrs.0000000000000520
27. Ang M, Soh Y, Htoon HM, Mehta JS, Tan D. Five-Year Graft Survival Comparing Descemet Stripping Automated Endothelial Keratoplasty and Penetrating Keratoplasty. Ophthalmology. 2016;123(8):1646–1652. doi:10.1016/j.ophtha.2016.04.049
28. Viberg A, Samolov B, Byström B. Descemet Stripping Automated Endothelial Keratoplasty versus Descemet Membrane Endothelial Keratoplasty for Fuchs Endothelial Corneal Dystrophy. Ophthalmology. 2023;130(12):1248–1257. doi:10.1016/j.ophtha.2023.07.024
29. Fu L, Hollick EJ. Comparison of Long-Term Outcomes of DSEK and DMEK in Fuchs Endothelial Dystrophy. Cornea. 2024;43(2):184–189. doi:10.1097/ICO.0000000000003310
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

