Back to Journals » Infection and Drug Resistance » Volume 18
Development and Validation of a Nomogram for Predicting Multidrug-Resistant Pseudomonas Aeruginosa Pneumonia in Hospitalized Patients
Authors Du Z , Yang D, Pan L, Zeng Q, Chen X
Received 8 April 2025
Accepted for publication 11 July 2025
Published 16 July 2025 Volume 2025:18 Pages 3543—3559
DOI https://doi.org/10.2147/IDR.S527949
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sandip Patil
Zhuman Du,1 Dan Yang,2 Linhai Pan,1 Qianglin Zeng,1 Xiaoju Chen1
1Department of Respiratory and Critical Care Medicine, Clinical Medicine College & Affiliated Hospital of Chengdu University, Chengdu, People’s Republic of China; 2Center of Gerontology and Geriatrics, West China Hospital, Sichuan University, Chengdu, People’s Republic of China
Correspondence: Qianglin Zeng; Xiaoju Chen, Department of Respiratory and Critical Care Medicine, Clinical Medicine College & Affiliated Hospital of Chengdu University, No. 82 North Section 2, Second Ring Road, Chengdu, Sichuan Province, People’s Republic of China, Email [email protected]; [email protected]
Objective: The management of multidrug-resistant Pseudomonas aeruginosa (MDR-PA) pneumonia remains challenging due to increasing antibiotic resistance and high mortality rates. Current prediction models often neglect three critical factors: comorbidities, medical interventions, and prior antibiotic exposure. This study created a practical risk assessment tool incorporating these clinical elements.
Methods: This retrospective study collected 3132 bronchoalveolar lavage fluid specimens from a large tertiary comprehensive hospital in southwestern China over a two-year period (20232024). A total of 209 patients with Pseudomonas aeruginosa pneumonia were ultimately enrolled, including 94 cases of multidrug-resistant and 115 drug-sensitive cases. Data included demographics, comorbidities, invasive procedures, antibiotic histories, and laboratory findings. Key predictors were selected using LASSO regression, followed by logistic regression to build a predictive model. Performance was evaluated through ROC analysis, calibration tests, and bootstrap validation.
Results: Thirteen predictors were identified: Age, prolonged hospitalization; Cor pulmonale, cardiac insufficiency, old cerebral infarction, chronic renal failure; ventilation, tracheostomy, nasogastric intubation; Cefoperazone-sulbactam, aminoglycosides, antifungals; Hemoglobin levels. The model showed strong predictive accuracy with AUC values of 0.853 (95% CI 0.793– 0.914) in training and 0.972 (0.931– 1.000) in validation cohorts. Calibration demonstrated excellent consistency (Hosmer-Lemeshow P=0.989).
Conclusion: In this study, we developed and validated a predictive model for MDR-PA pneumonia risk by integrating host comorbidities, iatrogenic interventions, and antimicrobial exposure. The model demonstrates potential utility in early identification of high-risk patients and may inform antimicrobial stewardship strategies in regions with predominant cephalosporin/aminoglycoside resistance patterns.
Keywords: pseudomonas aeruginosa, multidrug resistance, nomogram, risk factor
Introduction
Pseudomonas aeruginosa (P. aeruginosa) is a monotrichous, non-spore-forming, Gram-negative, facultative aerobic bacterium.1 According to the 2019 Global Burden of Disease Study, P. aeruginosa ranks as the fifth leading cause of infection-related mortality among all bacterial pathogens investigated and is the second most common pathogen responsible for both community-acquired and hospital-acquired pneumonia.2 A prevalence survey identified P. aeruginosa as the fifth most common cause of healthcare-associated infections, with a prevalence of 7.1% in tertiary hospitals and an overall prevalence of 24.7% in Asia.3,4 In China, the prevalence of P. aeruginosa-related infections in tertiary healthcare institutions is 28.7%, with its isolation frequency ranking second only to Acinetobacter baumannii.5
The antimicrobial resistance of P. aeruginosa has garnered significant concern, as it is one of the six leading pathogens responsible for resistance-related mortality and is included in the ESKAPE pathogen group.6 The World Health Organization (WHO) has classified carbapenem-resistant P. aeruginosa as a “critical priority” pathogen.7 Current studies demonstrate that P. aeruginosa exhibits resistance to multiple commonly used antimicrobial agents, including carbapenems (imipenem resistance rate: 31.3%; meropenem: 24.4%), cephalosporins (ceftazidime: 18.5%; cefepime: 12.0%), and aminoglycosides (gentamicin: 25.1%).8–10 Notably, the resistance rates of P. aeruginosa exhibit geographical variations globally. The European Centre for Disease Prevention and Control (ECDC) 2021 report indicated that 18.7% of P. aeruginosa isolates were resistant to carbapenems, while 13.4% were resistant to three or more antimicrobial classes.9 Indian studies have shown an increasing trend in P. aeruginosa resistance.11 In Asian regions, the resistance situation of P. aeruginosa remains severe, with an overall prevalence of multidrug-resistant P. aeruginosa (MDR-PA) reaching 46.0%, extensively drug-resistant P. aeruginosa (XDR-PA) at 19.6%, extended-spectrum β-lactamase-positive P. aeruginosa (ESBL-positive PA) at 33.4%, and metallo-β-lactamase-positive P. aeruginosa (MBL-positive PA) at 16.0%.3 Among Chinese patients with hospital-acquired pneumonia, the infection rates of MDR-PA and XDR-PA were as high as 44.4% and 18.2%, respectively.12 And the PA resistance rates also vary among different populations, with ICU patients showing the MDR-PA infection rate of 48.7%.13 Among various pneumonia patients, ventilator-associated pneumonia patients exhibit the highest MDR-PA infection rate, followed by hospital-acquired pneumonia patients.12
Mortality associated with P. aeruginosa infections remains a critical concern,14 particularly in immunocompromised and hospitalized patients, with rates ranging from 25–39% for pneumonia and 18–61% for bacteremia.15,16 Notably, infections caused by multidrug-resistant isolates correlate with even higher mortality rates (40–70%).14–17
Therefore, infection risk prediction tools are critical for reducing mortality and alleviating the economic burden associated with MDR-PA infections. Previous predictive models for P. aeruginosa infections have each focused on different aspects. Wang et al developed a predictive model using Cox regression analysis and nomograms to estimate the risk of recurrent hemoptysis following bronchial artery embolization and P. aeruginosa infection, providing valuable clinical insights; however, this model did not specifically address antibiotic resistance.18 Tartof et al’s model specifically evaluates the resistance of P. aeruginosa to carbapenems and broad-spectrum β-lactams in hospitalized patients, with its applicability primarily centered on specific antibiotics.19 Wijit et al’s research focused on the risk of P. aeruginosa infection in community-acquired pneumonia,20 which, while valuable for specific populations, does not cover hospital-acquired infections. Therefore, this study base on multiple dimensions such as demographic characteristics, antibiotic use, and laboratory examinations of hospitalized patients, and focuses on developing and validating a predictive model for the risk of MDR-PA pneumonia in hospitalized patients.
Materials and Methods
Study Design and Data Source
This retrospective study was conducted at Chengdu University Affiliated Hospital (a large tertiary comprehensive teaching hospital with over 1400 open beds in Southwest China) from January 1, 2023 to April 30, 2024. The analysis exclusively included bronchial lavage fluid specimens from patients with P. aeruginosa-positive cultures. Exclusion criteria comprised: 1) negative P. aeruginosa cultures, 2) specimens without bacterial culture, and 3) cases of recurrent infection (only the initial episode was retained) (Figure 1).
 |
Figure 1 The flowchart of patients’ enrollment. |
Patient demographics and clinical parameters were extracted from electronic medical records and analyzed using WHONET 5.6. Bacterial identification and antimicrobial susceptibility testing were performed with the MicroScan WalkAway 40 automated system, following standardized protocols for clinical microbiological specimen processing. All bronchoscopic procedures adhered to current guidelines for specimen collection and laboratory analysis. Quality control was ensured using P. aeruginosa ATCC27853 reference strains. Antimicrobial susceptibility interpretations complied with the most recent CLSI guidelines, with annual updates applied. The study protocol received ethical approval from the Institutional Review Board of Chengdu University Affiliated Hospital (PJ2024-048-01), with waiver of informed consent granted for retrospective data analysis. The research will follow the principles of the Declaration of Helsinki and the Measures for Ethical Review of Biomedical Research Involving Human Subjects issued by China’s National Health Commission.
Measures of Variables
The following variables were systematically extracted from electronic medical records:
Demographic parameters: Age and sex; Clinical characteristics: Smoking history; total hospital length of stay; ICU admission status; pre-sampling hospitalization duration; pre-sampling ICU stay duration; pre-existing respiratory disorders; major comorbidities (cardiovascular diseases, neurological disorders, diabetes mellitus, malignancies, renal insufficiency); ventilation modalities; mechanical ventilation duration; nasogastric intubation; indwelling urinary catheterization; arteriovenous catheterization; thoracic drainage; grade III/IV surgical procedures during hospitalization; antibiotic exposure profiles; and duration of systemic corticosteroid administration (intravenous or oral); Laboratory parameters: Leukocyte count; hemoglobin concentration; platelet count; high-sensitivity C-reactive protein (hs-CRP); interleukin-6 (IL-6); procalcitonin (PCT) levels; serum albumin; D-dimer; and antimicrobial susceptibility profiles for P. aeruginosa.
Definitions
Pneumonia is an acute lower respiratory tract infection caused by pathogens such as bacteria, viruses, or fungi, characterized by inflammatory cell infiltration and exudative changes in alveolar spaces, accompanied by fever, cough, and radiographic pulmonary infiltrates.21 Multidrug resistance is defined as acquired resistance to at least one agent from three or more antimicrobial classes: carbapenems, β-lactamase inhibitor combinations, cephalosporins, aminoglycosides, and fluoroquinolones.22 Carbapenem-resistant P. aeruginosa is defined as P. aeruginosa that is resistant to one or more carbapenem agents.23 Definitions of Antimicrobial Susceptibility Categories for P. aeruginosa: Susceptible (S): A P. aeruginosa strain is classified as susceptible to a specific antimicrobial agent when the minimum inhibitory concentration (MIC) is ≤ the established susceptibility breakpoint, indicating that standard dosing regimens are highly likely to achieve clinically effective plasma and tissue concentrations for therapeutic success. Intermediate (I): A strain is designated intermediate when the MIC exceeds the susceptibility breakpoint but remains ≤ the resistance breakpoint. This category suggests uncertain therapeutic efficacy, as clinical response may be achievable only under specific conditions (eg, higher-than-standard doses or localized infections where the drug accumulates at elevated concentrations).Resistant (R): Resistance is confirmed when the MIC exceeds the resistance breakpoint, signifying a high probability of therapeutic failure even with maximum tolerated doses, due to established resistance mechanisms or inadequate drug penetration at the infection site.24
Statistical Analysis
Continuous variables with normal distribution were described as mean ± standard deviation, while non-normally distributed variables were presented as median (interquartile range). Categorical variables were expressed as frequency (percentage). Comparative analyses between MDR-PA and DS-PA groups were performed using unpaired t-test or Wilcoxon rank-sum test for continuous variables, and Pearson’s chi-square test or Fisher’s exact test for categorical variables. The Least Absolute Shrinkage and Selection Operator (LASSO) regression technique was applied for data dimensionality reduction and predictor selection. A multivariate logistic regression analysis was employed to develop the MDR-PA prediction model and corresponding nomogram. Internal validation was conducted through bootstrap resampling (resamples=1000). The model’s discriminative performance was assessed using receiver operating characteristic (ROC) curves and area under the curve (AUC). All statistical analyses were performed using R software (version 4.4.1), with statistical significance set at P<0.05.
Results
Baseline Characteristics
During the study period (January 1, 2023–April 30, 2024), 3132 bronchoalveolar lavage fluid (BALF) specimens were initially collected. After applying inclusion/exclusion criteria, 209 patients with P. aeruginosa-positive cultures were enrolled, comprising 44.98% (94/209) multidrug-resistant (MDR) strains and 55.02% (115/209) non-MDR (drug-sensitive, DS) strains. The demographic and clinical characteristics of the study cohort are summarized in Table 1. Antibiotic usage are presented in Table 2, with laboratory findings documented in Table 3. Univariate analysis revealed statistically differences between the two groups (P<0.05):age, total hospitalization duration, hospitalization duration before specimen collection, cor pulmonale, cardiac functional insufficiency, remote cerebral infarction, chronic renal insufficiency, ventilator support, ventilator use duration, mechanical ventilation, tracheostomy, nasogastric tube insertion, urinary catheter insertion, arteriovenous catheterization, thoracic drainage tube, cefoperazone-sulbactam exposure, aminoglycosides administration, imipenem-cilastatin therapy, linezolid use, combination therapy (≥2 antibiotics),concomitant antifungal treatment, leukocyte count, neutrophil percentage, hemoglobin level, serum albumin concentration, procalcitonin (PCT) level, d-dimer value.
 |
Table 1 Demographic and Clinical Characteristics of Study Participants |
 |
Table 2 Antibiotic Usage of Study Participants |
 |
Table 3 Laboratory Findings of Study Participants |
Construction of Predictive Models
1) Univariate Analysis: After conducting univariate analysis on 66 variables, we identified 26 variables that were statistically significant. These variables covered demographic and clinical characteristics, antibiotic usage, and laboratory findings. 2) LASSO Regression Analysis: Although the 26 variables identified in the univariate analysis were statistically significant, not all of them had a substantial impact on the outcome. Therefore, we chose to use LASSO regression analysis to select the most important predictors from the pool of potential variables. LASSO regression effectively reduces model complexity by penalizing less important variables, thereby enhancing the model’s generalizability and preventing overfitting. In this study, we employed cross-validation for predictor selection (Figure 2) and determined the tuning parameter (lambda) based on both the minimum criterion (left dashed line) and the 1-SE criterion (right dashed line). Ultimately, we followed the 1-SE criterion (right dashed line) for predictor selection (Figure 3). Through LASSO regression analysis, we selected 13 predictors, including age, total hospitalization duration, comorbidities (cor pulmonale, heart failure, old cerebral infarction, chronic renal insufficiency), clinical interventions (mechanical ventilation requirement, tracheostomy status, indwelling gastric tube), antimicrobial therapies (cefoperazone-sulbactam, aminoglycoside antibiotics, antifungal agents), and hemoglobin levels. 3) Model Development and Validation: Patients included in the study were randomly divided into training and validation cohorts (7:3 ratio) using a random number table In the training cohort, we developed a multivariable logistic regression model to predict the risk of MDR-PA infection using the variables selected by LASSO regression. The model was subsequently validated in the validation cohort. The model demonstrated good discriminative ability, with an area under the ROC curve (AUC) of 0.853 (95% confidence interval [CI], 0.793–0.914) in the training cohort and 0.972 (95% CI, 0.931–1.0) in the validation cohort (Figures 4 and 5). To make the model more intuitive and clinically applicable, we constructed a nomogram (Figure 6). The nomogram converts the regression coefficients of each predictor into scores, sums them to obtain a total score, and then translates the total score into a predicted probability, providing clinicians with a practical tool for estimating infection risk. 4) Model Calibration: The calibration performance of the model was assessed using the Hosmer-Lemeshow test, which showed non-significance (p=0.989) (Figure 7), indicating a close agreement between predicted and observed outcomes in the training cohort. These results suggest that the model has good discrimination and calibration consistency, effectively identifying high-risk patients for MDR-PA infection and providing strong support for clinical decision-making.
 |
Figure 2 Selection of predictive factors using LASSO regression analysis with cross-validation. |
 |
Figure 3 Tuning parameter (lambda) selection for LASSO regression deviance based on the minimum criterion (left dashed line) and the 1-SE criterion (right dashed line). |
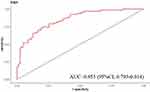 |
Figure 4 AUC of the predictive and validation models-train. |
 |
Figure 5 AUC of the predictive and validation models-test. |
 |
Figure 6 Nomogram for assessing multidrug-resistant Pseudomonas aeruginosa infection risk. |
 |
Figure 7 Calibration curve of the predictive model. |
Discussion
The threat of multidrug-resistant MDR-PA infection is on the rise, and there is an urgent need for predictive tools to guide early clinical intervention. Utilizing data from a comprehensive tertiary hospital in Southwest China, we developed and validated a nomogram that integrates multidimensional information, including demographics, clinical invasive procedures, antibiotic exposure, and laboratory tests, to predict MDR-PA pulmonary infection.
In recent years, the prevalence of P. aeruginosa has surged dramatically, raising concerns. Our study found that MDR-PA accounted for 44.98% of all P. aeruginosa-infected patients, which is consistent with the 2025 study by Zulkifli et al, reporting a prevalence of 46.0% for MDR-PA strains in Asia and Africa.3 This study developed a predictive model for MDR-PA infections using exclusively BALF specimens. Compared to prior studies incorporating heterogeneous specimen types, the sterile collection protocol of BALF effectively mitigates oropharyngeal flora contamination,25 thereby significantly enhancing the specificity of lower respiratory tract pathogen detection. This specimen standardization strategy improves the model’s applicability to severe infection scenarios, such as ventilator-associated pneumonia.26 However, the requirement for bronchoscopy in BALF acquisition necessitates the exclusion of hemodynamically unstable patients and non-severe cases, which may result in potential underestimation of MDR-PA infection risks in specific populations.
The risk factors for MDR-PA infection identified in this study are in line with global epidemiological trends while revealing regional specificity. Age is one of the key host factors influencing the risk of MDR-PA pneumonia. The results show that the risk of MDR-PA pneumonia increases with age. From a pathophysiological perspective, the age-related decline in immune function may be the reason why elderly patients are susceptible to MDR - PA.20,27 Moreover, elderly patients often have multiple underlying diseases, which increase the burden of comorbidities. These diseases not only disrupt the respiratory barrier function but also exacerbate the drug resistance of P. aeruginosa through long-term use of corticosteroids/antibiotics. Our study found that cor pulmonale, heart failure, chronic renal insufficiency, and old cerebral infarction increase the risk of MDR - PA pneumonia. Among them, old cerebral infarction as a risk factor is particularly noteworthy, as this finding has been underestimated in previous literature.27,28 This association may stem from chronic neuroinflammation or post-stroke immune suppression, which creates a favorable environment for the colonization or infection of MDR - PA.
Prolonged hospitalization is one of the significant risk factors for MDR-PA pneumonia. Our study revealed that the risk of MDR-PA pneumonia in long-term hospitalized patients is significantly higher than that in short-term hospitalized patients, with a higher isolation rate of MDR-PA. As the length of hospital stay increases, patients are exposed to a greater variety of pathogens in the hospital environment, including drug resistant bacteria.29 In long-term care hospitals, the multidrug resistance rate of P. aeruginosa is higher than that in general hospitals.30 Reducing the length of hospital stay is an important strategy to decrease P. aeruginosa infections.31 However, long-term hospitalized patients often have multiple underlying diseases and complex medical conditions, which may also have a confounding effect on the results.29 Future studies need to further control these confounding factors to more accurately assess the relationship between prolonged hospitalization and MDR-PA pneumonia.
Invasive procedures also impact the occurrence of MDR-PA pneumonia, with ventilator support and tracheostomy being significant risk factors.32 Studies have shown that P. aeruginosa is one of the main pathogens of ventilator-associated pneumonia (VAP), and the emergence of MDR-PA has made the treatment of VAP more complex and difficult.33 In patients with mechanical ventilation, intubation or tracheostomy disrupts the natural defense barrier of the respiratory tract, increasing the chances of P. aeruginosa entering the lower respiratory tract.34 Meanwhile, the surfaces of medical devices such as ventilator tubing are prone to biofilm formation, in which drug-resistant bacteria can survive and reproduce, further increasing the risk of infection.34 MDR-PA infection is associated with ventilator treatment failure,33 and the crude mortality rate of VAP patients caused by MDR-PA is as high as 42.1%–87%, which remains high even with appropriate antibiotic therapy.34 Notably, in this study, nasogastric tube placement was one of the 13 independent predictors identified, indicating its clinical predictive value. Nasogastric tube placement directly damages the neuromuscular coordination of the pharynx, weakening the swallowing reflex and increasing the risk of aspiration.35 Aspirated gastric acid and bile can damage the mucosal barrier of the lower respiratory tract, creating conditions for MDR-PA colonization. According to research results in the literature, the use of nasogastric tubes (enteral/nasogastric tubes) is one of the independent risk factors for carbapenem-resistant P. aeruginosa.36 In a study of 157 patients with P. aeruginosa, 78.26% had used enteral/nasogastric tubes.36 Previous studies reported a significantly higher frequency of nasogastric tube use among patients infected with non-mucoid P. aeruginosa, with 18.5% of these non-mucoid isolates being carbapenem-resistant P. aeruginosa, suggesting that nasogastric tube placement may serve as a risk factor for non-mucoid strain acquisition.37
Although carbapenem resistance remains a major concern in high-income countries, our cohort study showed that, compared with resistance to cephalosporins/aminoglycosides, carbapenem resistance has relatively lower predictive value for resistance phenotypes. This difference may reflect the unique antimicrobial management landscape in China. Under the national antibiotic restriction policy, the use of carbapenems is strictly regulated, while third-generation cephalosporins (eg, cefoperazone-sulbactam) are still widely used for respiratory infections. This regional prescription pattern may drive different resistance trajectories.8,38
Notably, hemoglobin decline emerged as an independent predictor of MDR-PA infection, corroborating the emerging “host iron metabolism-bacterial virulence” axis proposed in recent studies.39 This finding resonates with Peng et al’s 2024 report linking reduced admission hemoglobin levels to increased 30-day mortality in septic patients.40 Physiologically, hemoglobin reduction often reflects chronic disease burden or immunocompromised status. While host iron restriction mechanisms typically inhibit pathogen proliferation through free iron sequestration, chronic anemia may compromise this defensive strategy.41 Existing MDR-PA prediction models mainly focus on inflammatory biomarkers (CRP/PCT) or antibiotic exposure history. By incorporating hemoglobin levels, we expanded the predictive framework, which may enhance risk stratification for multidrug-resistant infections.19
The limitations of this study should be acknowledged. First, the single center retrospective design introduced potential selection bias, especially regarding the exclusion of non-BALF specimens. Second, the relatively small sample size (n = 209) and the geographical scope limited to Southwest China may restrict the generalizability. Third, although internal validation supported the robustness of the methodology, external validation through multicenter prospective cohorts is still crucial for confirming clinical applicability. Lastly, this study was limited to MDR-PA pulmonary infection, and the applicability of similar models to other respiratory pathogens, such as Streptococcus pneumoniae and Klebsiella pneumoniae, needs to be explored.42,43 Future research should address these limitations while investigating the mechanistic relationships between iron homeostasis, chronic cerebrovascular pathology, and the pathogenesis of MDR-PA.
Conclusion
The nomogram developed and validated in this study integrates host comorbidities, iatrogenic interventions, and antimicrobial exposure to predict the risk of MDR-PA pneumonia, which is of importance in clinical practice. The nomogram enhances the early identification of high-risk patients and optimizes antimicrobial stewardship in regions with cephalosporin/aminoglycoside-dominated resistance patterns, thereby reducing the incidence of MDR-PA. Additionally, the nomogram can serve as a reference for formulating public health policies and infection control guidelines. Future research should focus on validating the nomogram in multicenter cohorts and exploring its integration into clinical decision-making systems.
Abbreviations
MDR-PA, multidrug-resistant Pseudomonas aeruginosa; DS-PA, drug-sensitive Pseudomonas aeruginosa; ICU, intensive care unit; BALF, bronchoalveolar lavage fluid; WHO, World Health Organization; ECDC, European Centre for Disease Prevention and Control; CLSI, Clinical and Laboratory Standards Institute; ROC, receiver operating characteristic; AUC, area under the curve; CI, confidence interval; LASSO, least absolute shrinkage and selection operator; SE, standard error; CRP, C-reactive protein; hs-CRP, high-sensitivity C-reactive protein; PCT, procalcitonin; IL-6, interleukin-6; MIC, minimum inhibitory concentration; S, susceptible; I, intermediate; R, resistant.
Data Sharing Statement
The data are available from reasonable request to corresponding authors.
Ethics Approval and Consent to Participate
This study was approved by the Ethics Committee of Chengdu University Affiliated Hospital] (Approval No. PJ2024-048-01). The research adheres to the principles of the Declaration of Helsinki and the relevant ethical guidelines, including the Measures for Ethical Review of Biomedical Research Involving Human Subjects issued by China’s National Health Commission. This study is a retrospective analysis of existing medical records. All patient identifiers have been removed, and the data were anonymized prior to analysis. Given the retrospective nature of the study and that there is no risk to participants or harm to their rights and health, a waiver of informed consent was granted by the Ethics Committee. The privacy and confidentiality of all participants have been strictly protected in accordance with applicable laws and regulations.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declared no conflicts of interest in this work.
References
1. Qin S, Xiao W, Zhou C, et al. Pseudomonas aeruginosa: pathogenesis, virulence factors, antibiotic resistance, interaction with host, technology advances and emerging therapeutics. Signal Transduct Target Ther. 2022;7(1):199. doi:10.1038/s41392-022-01056-1
2. Diggle SP, Whiteley M. Microbe Profile: pseudomonas aeruginosa: opportunistic pathogen and lab rat. Microbiology. 2020;166(1):30–33. doi:10.1099/mic.0.000860
3. Mohd Zulkifli S, Nik Mohd Noor NZ, Zakuan Zainy D, et al. Current trends in the epidemiology of multidrug-resistant and beta-lactamase-producing Pseudomonas aeruginosa in Asia and Africa: a systematic review and meta-analysis. PeerJ. 2025;13:e18986. doi:10.7717/peerj.18986
4. Suetens C, Latour K, Kärki T, et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Euro Surveill. 2018;23(46):1800516. doi:10.2807/1560-7917.ES.2018.23.46.1800516
5. Oliveira VD, Rubio FG, Almeida MT, Nogueira MC, Pignatari AC. Trends of 9,416 mult idrug-resistant Gram-negative bacteria. Rev Assoc Med Bras. 2015;61(3):244–249. doi:10.1590/1806-9282.61.03.244
6. Murray CJL, Ikuta KS, Sharara F. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–655. doi:10.1016/S0140-6736(21)02724-0
7. Tacconelli E, Carrara E, Savoldi A, et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18(3):318–327. doi:10.1016/S1473-3099(17)30753-3
8. Li Y, Lv Y, Xue F, Zheng B, Liu J, Zhang J. Antimicrobial resistance surveillance of doripenem in China. J Antibiot. 2015;68(8):496–500. doi:10.1038/ja.2015.25
9. Elfadadny A, Ragab RF, AlHarbi M, et al. Antimicrobial resistance of Pseudomonas aeruginosa: navigating clinical impacts, current resistance trends, and innovations in breaking therapies. Front Microbiol. 2024;15:1374466. doi:10.3389/fmicb.2024.1374466
10. Cosentino F, Viale P, Giannella M. MDR/XDR/PDR or DTR? Which definition best fits the resistance profile of Pseudomonas aeruginosa. Curr Opin Infect Dis. 2023;36(6):564–571. doi:10.1097/QCO.0000000000000966
11. Choudhuri AH, Chakravarty M, Uppal R. Epidemiology and characteristics of nosocomial infections in critically ill patients in a tertiary care Intensive Care Unit of Northern India. Saudi J Anaesth. 2017;11(4):402–407. doi:10.4103/sja.SJA_230_17
12. Ding C, Yang Z, Wang J, et al. Prevalence of Pseudomonas aeruginosa and antimicrobial-resistant Pseudomonas aeruginosa in patients with pneumonia in mainland China: a systematic review and meta-analysis. Int J Infect Dis. 2016;49:119–128. doi:10.1016/j.ijid.2016.06.014
13. Horcajada JP, Montero M, Oliver A, et al. Epidemiology and Treatment of Multidrug-Resistant and Extensively Drug-Resistant Pseudomonas aeruginosa Infections. Clin Microbiol Rev. 2019;32(4):e00031–19. doi:10.1128/CMR.00031-19
14. Wannigama DL, Hurst C, Monk PN, et al. tesG expression as a potential clinical biomarker for chronic Pseudomonas aeruginosa pulmonary biofilm infections. BMC Med. 2025;23(1):191. doi:10.1186/s12916-025-04009-x
15. Rojas A, Palacios-Baena ZR, López-Cortés LE, Rodríguez-Baño J. Rates, predictors and mortality of community-onset bloodstream infections due to Pseudomonas aeruginosa: systematic review and meta-analysis. Clin Microbiol Infect. 2019;25(8):964–970. doi:10.1016/j.cmi.2019.04.005
16. Behzadi P, Baráth Z, Gajdács M. It’s Not Easy Being Green: a Narrative Review on the Microbiology, Virulence and Therapeutic Prospects of Multidrug-Resistant Pseudomonas aeruginosa. Antibiotics. 2021;10(1):42. doi:10.3390/antibiotics10010042
17. Liu T, Zhang Y, Wan Q. Pseudomonas aeruginosa bacteremia among liver transplant recipients. Infect Drug Resist. 2018;11:2345–2356. doi:10.2147/IDR.S180283
18. Wang LL, Lu HW, Li LL, et al. Pseudomonas aeruginosa isolation is an important predictor for recurrent hemoptysis after bronchial artery embolization in patients with idiopathic bronchiectasis: a multicenter cohort study. Respir Res. 2023;24(1):84. doi:10.1186/s12931-023-02391-9
19. Tartof SY, Kuntz JL, Chen LH, et al. Development and Assessment of Risk Scores for Carbapenem and Extensive β-Lactam Resistance Among Adult Hospitalized Patients With Pseudomonas aeruginosa Infection. JAMA Network Open. 2018;1(6):e183927. doi:10.1001/jamanetworkopen.2018.3927
20. Wijit K, Sonthisombat P, Diewsurin J. A score to predict Pseudomonas aeruginosa infection in older patients with community-acquired pneumonia. BMC Infect Dis. 2023;23(1):700. doi:10.1186/s12879-023-08688-w
21. Olson G, Davis AM. Diagnosis and Treatment of Adults With Community-Acquired Pneumonia. JAMA. 2020;323(9):885–886. doi:10.1001/jama.2019.21118
22. Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi:10.1111/j.1469-0691.2011.03570.x
23. Sendra E, Fernández-Muñoz A, Zamorano L, et al. Impact of multidrug resistance on the virulence and fitness of Pseudomonas aeruginosa: a microbiological and clinical perspective. Infection. 2024;52(4):1235–1268. doi:10.1007/s15010-024-02313-x
24. Subedi D, Vijay AK, Willcox M. Overview of mechanisms of antibiotic resistance in Pseudomonas aeruginosa: an ocular perspective. Clin Exp Optom. 2018;101(2):162–171. doi:10.1111/cxo.12621
25. Peres RL, Palaci M, Loureiro RB, et al. Evaluation of oral antiseptic rinsing before sputum collection to reduce contamination of mycobacterial cultures. J Clin Microbiol. 2011;49(8):3058–3060. doi:10.1128/JCM.00541-11
26. Martin-Loeches I, Chastre J, Wunderink RG. Bronchoscopy for diagnosis of ventilator-associated pneumonia. Intensive Care Med. 2023;49(1):79–82. doi:10.1007/s00134-022-06898-5
27. Kothari A, Kherdekar R, Mago V, et al. Age of Antibiotic Resistance in MDR/XDR Clinical Pathogen of Pseudomonas aeruginosa. Pharmaceuticals. 2023;16(9):1230. doi:10.3390/ph16091230
28. Liao Q, Feng Z, Lin H, et al. Carbapenem-resistant gram-negative bacterial infection in intensive care unit patients: antibiotic resistance analysis and predictive model development. Front Cell Infect Microbiol. 2023;13:1109418. doi:10.3389/fcimb.2023.1109418
29. Gill CM, Nicolau DP. Carbapenem-resistant Pseudomonas aeruginosa: an assessment of frequency of isolation from ICU versus non-ICU, phenotypic and genotypic profiles in a multinational population of hospitalized patients. Antimicrob Resist Infect Control. 2022;11(1):146. doi:10.1186/s13756-022-01187-8
30. Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63(5):e61–e111. doi:10.1093/cid/ciw353
31. Micek ST, Reichley RM, Kollef MH. Health care-associated pneumonia (HCAP): empiric antibiotics targeting methicillin-resistant Staphylococcus aureus (MRSA) and Pseudomonas aeruginosa predict optimal outcome. Medicine. 2011;90(6):390–395. doi:10.1097/MD.0b013e318239cf0a
32. Li S, Jia X, Li C, et al. Carbapenem-resistant and cephalosporin-susceptible Pseudomonas aeruginosa: a notable phenotype in patients with bacteremia. Infect Drug Resist. 2018;11:1225–1235. doi:10.2147/IDR.S174876
33. Song JH, Yoon SY, Park TY, et al. The clinical impact of drug-induced hepatotoxicity on anti-tuberculosis therapy: a case control study. Respir Res. 2019;20(1):283. doi:10.1186/s12931-019-1256-y
34. Foucrier A, Dessalle T, Tuffet S, et al. Association between combination antibiotic therapy as opposed as monotherapy and outcomes of ICU patients with Pseudomonas aeruginosa ventilator-associated pneumonia: an ancillary study of the iDIAPASON trial. Crit Care. 2023;27(1):211. doi:10.1186/s13054-023-04457-y
35. Karadogan E, Sertcelik A, Dizman GT, et al. A scoring system to predict resistance to ceftolozane/tazobactam in respiratory isolates of Pseudomonas aeruginosa. J Antimicrob Chemother. 2025;2025:dkae476.
36. Rossi Gonçalves I, Dantas R, Ferreira ML, et al. Carbapenem-resistant Pseudomonas aeruginosa: association with virulence genes and biofilm formation. Braz J Microbiol. 2017;48(2):211–217. doi:10.1016/j.bjm.2016.11.004
37. Luo M, Li S, Luo W. Comparative analysis of antibiotic susceptibility patterns and clinical features of mucoid and non-mucoid Pseudomonas aeruginosa infections: a retrospective study. Front Public Health. 2024;12:1333477. doi:10.3389/fpubh.2024.1333477
38. Han M, Zhang X. Impact of medical professionals on Carbapenem-resistant Pseudomonas aeruginosa: moderating effect of workload based on the panel data in China. BMC Health Serv Res. 2020;20(1):670. doi:10.1186/s12913-020-05535-5
39. Mouriño S, Wilks A. Extracellular haem utilization by the opportunistic pathogen Pseudomonas aeruginosa and its role in virulence and pathogenesis. Adv Microb Physiol. 2021;79:89–132.
40. Peng H, Su Y, Luo J, Ding N. Association between admission hemoglobin level and prognosis in sepsis patients based on a critical care database. Sci Rep. 2024;14(1):5212. doi:10.1038/s41598-024-55954-1
41. Kassebaum NJ, GBD 2013 Anemia Collaborators. The Global Burden of Anemia. Hematol Oncol Clin North Am. 2016;30(2):247–308. doi:10.1016/j.hoc.2015.11.002
42. Wannigama DL, Amarasiri M, Phattharapornjaroen P, et al. Streptococcus pyogenes surveillance through surface swab samples to track the emergence of streptococcal toxic shock syndrome in rural Japan. J Infect Dis;2025. jiaf234. doi:10.1093/infdis/jiaf234
43. Abe S, Wannigama DL. Quick Sequential Organ Failure Assessment (qSOFA) and Performance Status Scoring Systems as Prognostic Predictors in Pneumococcal Community-Acquired Pneumonia. Cureus. 2024;16(11):e73201. doi:10.7759/cureus.73201
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Development and Validation of a Diagnostic Nomogram for Pneumocystis jirovecii Pneumonia in Non-HIV-Infected Pneumonia Patients Undergoing Oral Glucocorticoid Treatment
Lang Q, Li L, Zhang Y, He X, Liu Y, Liu Z, Yan H
Infection and Drug Resistance 2023, 16:755-767
Published Date: 4 February 2023
Platelet-to-Lymphocyte Ratio (PLR), Neutrophil-to-Lymphocyte Ratio (NLR), Monocyte-to-Lymphocyte Ratio (MLR), and Eosinophil-to-Lymphocyte Ratio (ELR) as Biomarkers in Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease (AECOPD)
Liao QQ, Mo YJ, Zhu KW, Gao F, Huang B, Chen P, Jing FT, Jiang X, Xu HZ, Tang YF, Chu LW, Huang HL, Wang WL, Wei FN, Huang DD, Zhao BJ, Chen J, Zhang H
International Journal of Chronic Obstructive Pulmonary Disease 2024, 19:501-518
Published Date: 23 February 2024
A Nomogram for Predicting Mortality in Patients with Pneumonia-Associated Acute Respiratory Distress Syndrome (ARDS)
Huang D, He D, Gong L, Jiang W, Yao R, Liang Z
Journal of Inflammation Research 2024, 17:1549-1560
Published Date: 8 March 2024
A Novel Nomogram for Predicting the Risk of Pneumonia After Intracerebral Hemorrhage
Sun Y, Zhang L, Huang B, He Q, Hu B
Journal of Inflammation Research 2025, 18:1333-1351
Published Date: 30 January 2025
Successful Treatment of Fournier’s Gangrene in Child with Relapsed Acute Lymphoblastic Leukemia: Case Report and Review of the Literature
Kołodziejczyk J, Czarny J, Królak S, Rutkowska S, Moryciński S, Mańkowski P, Bartkowska-Śniatkowska A, Wachowiak J, Derwich K, Zając-Spychała O
Infection and Drug Resistance 2025, 18:1667-1673
Published Date: 1 April 2025

