Back to Journals » Clinical Interventions in Aging » Volume 20
Development, Reliability, and Validity of Comprehensive Frailty Assessment Tool for Older Adults with Cancer (FOAC) in China
Authors Jiang N , Abdul Kadir A, Xie H, Wang L, Yu H, Hassan II
Received 14 December 2024
Accepted for publication 20 June 2025
Published 1 July 2025 Volume 2025:20 Pages 951—967
DOI https://doi.org/10.2147/CIA.S512322
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Nannan Jiang,1,2 Azidah Abdul Kadir,3 Hui Xie,2 Li Wang,4 Hua Yu,5 Intan Idiana Hassan1
1School of Health Sciences, Health Campus, Universiti Sains Malaysia, Kubang Kerian, Kelantan, 16150, Malaysia; 2Bengbu Medical University, Bengbu, Anhui, People’s Republic of China; 3Department of Family Medicine, School of Medical Sciences, Health Campus, Universiti Sains Malaysia, Kubang Kerian, Kelantan, 16150, Malaysia; 4Nursing Department, The First Affiliated Hospital of Bengbu, Medical College, Bengbu, Anhui, People’s Republic of China; 5Nursing Department, Bengbu Third People’s Hospital, Bengbu, Anhui, People’s Republic of China
Correspondence: Intan Idiana Hassan, School of Health Sciences, Health Campus, Universiti Sains Malaysia, Kubang Kerian, Kelantan, 16150, Malaysia, Tel/Fax +60-1116966697, Email [email protected]
Purpose: With the accelerating ageing population, frailty has emerged as a critical concern among older cancer patients. The purpose of the study was to develop a valid and reliable Comprehensive Frailty Assessment Tool for Older Adults with Cancer (FOAC) in China.
Patients and Methods: The FOAC was developed in 4 phases. Phase 1: Conceptualization and Item Generation:32 items were formulated from the literature. Phase 2: Content validation of the FOAC by modified Delphi method. Phase 3: Face validity index (FVI) was calculated by recording the views of two groups, including older adults with cancer and those with professional roles. Phase 4:Using CGA-determined frailty as the dependent variable, receiver operating characteristic (ROC) curve analysis was conducted using FOAC, FP, and aCGA frailty screening scales as independent variables and their area under the curve (AUC), sensitivity, specificity, cut-off value, predicted value, and accuracy were determined. Internal consistency reliability measurement was assessed with Cronbach’s alpha.
Results: The FOAC has 30 items. Physiological dimension (11 items). Psychological & cognitive dimension (12 items). Social support (7 items). the results of this study demonstrated that the overall Cronbach’s alpha coefficient of the scale was 0.869.
Conclusion: The FOAC is a valid and reliable frailty screening tool that significantly addresses the problems of existing frailty assessment tools, such as single dimension, low sensitivity, complex scoring, and insufficient clinical applicability. It contributes to guiding healthcare professionals in providing more accurate diagnosis, treatment, and cancer management for older adults.
Keywords: frail elderly, cancer survivors, geriatric assessment, ROC curve, sensitivity, specificity
Introduction
The malignant tumor prevalence is gradually rising with the growth of the older adult population and the prolongation of their life span.1 By 2050, the global aging population will reach 1.6 billion, with China reaching 430 million. According to the cancer prevalence rate of older adults (278.07/100,000), 1.2 million Chinese will develop cancer, posing a huge burden to social medical resources.2 The physiological reserves of patients with cancer are reduced because of the disease itself, and diverse treatments further increase the body burden, making their physiological reserves tenser.3 Therefore, frailty is particularly prevalent in patients with cancer. The frailty prevalence in the older adult population with cancer ranges from 6 to 86%, with a 42% median prevalence.4
The International Association of Gerontology and Geriatrics (IAGG) consensus defines frailty as “a state of decreased strength and abnormal physiological function that increases an individual’s dependence, vulnerability, and susceptibility to death”.5 Thus, frailty is an important cause of heterogeneity in the health status of older adults with cancer.6 Nieman et al’s research shows that frailty is not only an independent predictor of death for inpatients with head and neck cancer but also increases the incidence of postoperative complications in these patients.7 Nieman et al’s research shows that frailty is not only an independent predictor of death for inpatients with head and neck cancer but also increases the incidence of postoperative complications in these patients.8 Frailty can also shorten the survival period of patients undergoing tumour surgery, radiotherapy and chemotherapy,9 reduce the quality of life,10 increase the length of hospital stay, costs, and readmission rates among patients.11 In summary, among older cancer patients, frailty has been proven not only to predict adverse outcomes but also to directly cause the occurrence of various adverse outcomes.
If timely identification and corresponding measures can be taken to prevent frailty, it can delay death and improve the quality of life of older adults.12 In 2013, the European Union Geriatrics Association proposed to incorporate frailty screening in routine clinical work to better comprehend the survival prognosis, risk of complications, and hospitalization expenses of older adult inpatients better.13 The risk of adverse outcomes (complications, discharge from home, length of stay, and total hospitalization expenses) of patients in a weakened state during hospitalization was found to be much higher than that of those in a non-weakened state by Rossello in 91618 patients with prostate cancer.14 Preoperative screening was suggested to be conducted to prevent or reduce the prevalence of adverse events.14 Therefore, it is essential to determine frailty in older adults with cancer, prompting the development of various frailty assessment tools over the past few decades.
However, more universally accepted reference standards and optimal assessment methods are required for frailty. The most widely used is the Fried frailty phenotype, while most of the others are derived from these tools.15 According to the Fried phenotype theory, introduced in 2001, frailty in the physical domain is defined using indicators like natural weight loss, self-reported fatigue, slow walking speed, low grip strength, and low physical activity. The most widely used tool for general frailty assessment is the frailty phenotype (FP) scale. However, its application in older adults with cancer is limited owing to its single-dimensional focus on physical frailty.16 The FRAIL scale is brief and easy to use but lacks a psychosocial dimension.17 The subsequently developed Edmonton Frail Scale (EFS) integrates cognitive and emotional dimensions.18 Groningen Frailty Indicator (GFI) have begun to incorporate the assessment of social participation.19 However, these scales were all developed based on the normal older population in Western cultural contexts. They thus cannot fully capture the specific expressions related to cancer in different cultural backgrounds.
Currently, frailty, in the context of the comprehensive geriatric assessment (CGA), is the reference standard for identifying and managing frailty. The assessment extends over aspects such as patient psychology, physiological function, comorbidities, cognition, nutrition, social support, the status of medication treatment, and fatigue.20 Although the gold standard for diagnosing frailty is CGA, it has a complex assessment process and takes several hours to complete. The tools for measuring CGA dimensions are still being determined, with no unified standard for defining the critical value of frailty.6 The development of abbreviated comprehensive geriatric assessment (aCGA) is aimed at pre-screening older patients with frailty to assess who will ultimately benefit from a complete CGA.21 In 2005, Overcash et al initially formulated the dimensions and items of the aCGA scale, including three dimensions of depression, physical function, and cognition, with 15 items.22 In 2021, the Chinese scholar Lin Yan developed a widely used multidimensional frailty assessment tool by adding the dimensions of nutrition, comorbidity burden, and geriatric syndrome to the traditional aCGA scale.23 The aCGA has a certain standardized framework; however, the evaluation content and methods applied in different regions and medical institutions may differ.
Although frailty assessment tools have been used worldwide, the following issues are noted in their application: (1) With the development of modern medical biology and health ecology concepts, and the proposal of multidimensional frailty concepts,24,25 some measurement items, such as social function levels, need to be reflected in the frailty assessment, which cannot reflect the multidimensional frailty concept;16 (2) Most assessment tools were initially developed in the Western countries. Therefore, their theoretical basis and the criteria of evaluation may not completely align with the actual situation of older adults with cancer in China. The assessment of “weight loss” is primarily based on Western dietary habits and lifestyle and is considered an essential indicator of frailty.26 Changes in weight among elderly individuals in China are often closely related to factors such as different dietary structures or lack of nutrition.27 Subsequently, this leads to different manifestations of frailty symptoms, affecting assessment accuracy. (3) Complex scoring methods may be observed in some frailty assessment tools that require more time and effort by the clinicians,28 thereby affecting the popularization and implementation of the tools. Furthermore, most assessment tools focus on disease assessment or nutritional function, lacking an integrated perspective that incorporates “patient matters”, such as self-management ability and subjective experience, into the assessment system. Moldovan et al proposed that the sustainability of medical services should be based on a systematic assessment of patient matters. Therefore, assessing frailty in older cancer patients should incorporate multi-dimensional factors such as “patient matters”.29
Thus, international and government agencies have advised all healthcare personnel to comprehend frailty better and timely identify and manage vulnerable groups to facilitate successful and effective management of frailty in old adults with cancer.15
The Social Determinants Of Health (SDOH) emphasize the crucial role of social factors in shaping frailty trajectories and proposes the integration of “social frailty” into the frailty screening framework.30 Guided by the health ecological model,31 this study developed a comprehensive frailty assessment tool (FOAC) that integrates social support as an essential dimension with physical and cognitive-psychological factors. This tool embodies the concept of multi-dimensional health and resonates with the latest paradigm in international frailty research. Furthermore, the study also proposed standardized criteria for the evaluation of clinical frailty.
Materials and Methods
Theoretical Framework
The theory of the health ecology model (HEM) proposes that the health of individuals and populations is the result of mutual dependence and restriction among individual factors, behavior, and lifestyle factors, and affects the health through multi-layer interactions.31 Thus, this study generated the initial items and dimensions based on the HEM.
The development of the assessment tool and validation of items for the comprehensive frailty assessment tool for older adults with cancer (FOAC) was undertaken in the following four phases: Phase 1, generating items that suit the study purposes by reviewing the relevant literature; Phase 2, evaluating content validity using the modified Delphi method; Phase 3, assessing face validity by conducting a pilot test of the modified instrument; and Phase 4, using the CGA (Comprehensive geriatric Assessment, CGA) scale as the gold standard.32 The screening accuracy of aCGA, FP, and FOAC, which are currently widely used globally was compared and their clinical application value was explored. The development and validation process is shown in Figure 1.
 |
Figure 1 The development and validation process flow diagram. |
Phase 1: Conceptualization and Item Generation
First, according to the HEM, the three dimensions of the FOAC were determined for physical function, psychological cognition, and social support, and the specific connotation of the dimensions in nursing research leadership was discussed by the research group of this study based on the literature review. After discussion with team members, a consensus was reached that the “physical functional dimension” should cover individuals’ physiological characteristics and states, including the structure, function, functionality, and health status of the body.33,34 How individuals process, understand, and respond to information at the psychological level comprises the psychological cognitive dimension. This dimension includes the psychological processes such as thinking, perception, memory, and emotions in humans.35,36 The social support dimension should include individual support and assistance from family, friends, colleagues, and social networks and emphasize the impact of social relationships on individual psychological and physiological health.37,38 The potential subject of the scale was also considered during the conceptualization procedure.
The items were generated using a literature review. The literature was searched on several databases, including PubMed, Web of Science, Cochrane Library, and Embase, using combined theme and free words, with theme words determined based on the MeSH thesaurus and searched in both Chinese and English languages, eg, “frailty” OR “frail*” OR “frailty” OR “frailty syndrome” OR “weak” OR “decline” OR “feeble”) AND (“oncology” OR “cancer” OR “neoplasms” OR “tumo*r” OR “cancer” OR “malignancy”) AND (“Olderly” OR “older” OR “aged” OR “aging” OR “elder” OR “the old” OR “old*patient” OR “old*person” OR “seniors” OR “senior citizen” OR “geriatric”) AND (“assessment tool” OR “instrument” OR “indicator” OR “scale”). Moreover, the guidelines and latest updates for clinical and community management of frailty by the World Health Organization, the National Comprehensive Cancer Network, and IAGG were reviewed and analyzed for quantitative content. A total of 32 items were generated for the initial questionnaire after the literature review.
Phase 2: Content Validity
The content validity indices (CVI) were calculated for both the individual items (I-CVl) and the entire scale (S-CVl) to ensure the legitimacy of the preliminary questionnaire’s content using the modified Delphi method.39,40 Considering that this study uses the modified Delphi method to verify content validity, the number of experts was selected according to the requirements of content validity. The minimum acceptable expert number is two for content validation; however, most recommendations propose a minimum of six experts. Considering the recommendations (5–8) and the author’s experience, the number of experts for content validation should be at least 6, not exceeding 10.41
The Modified Delphi Technique commenced with an invitation round and two written rounds. Thus, a CVl tool and the first draft of the FOAC scale were sent to 10 expert reviewers who were cautiously selected based on their expertise in academics, instrument development research, and healthcare. The expert panel included two oncologists, four registered nurses, two nursing professors, and two geriatricians. The inclusion criteria for experts are as follows: ①Degree: Possessing a master’s or doctoral degree and holding a professional title of associate senior or above; ② Working experience: Having over 10 years of experience in the relevant professional field; ③ Professional field: Having experience in oncology, geriatrics, nursing education or scale development. ④ Geographical coverage: Experts come from different levels of medical institutions in Anhui Province, China, including cities, counties and towns, to ensure the applicability in different regions. For specific information, please refer to Supplementary Table 1. Based on the relevance of the item content to frailty, each expert was asked to rate each questionnaire item. The experts were asked to assess how well each item corresponds to or reflects a specific domain on a four-point Likert scale. The scoring method was as follows: 1, not relevant; 2, somewhat relevant; 3, relevant; and 4, highly relevant.39 The experts were also invited to comment on each item and the general formulations of the initial questionnaire. Post-completion of the first round of expert consultation, content validation indices (state here) were computed using Excel and the comments were reviewed by the researcher and supervisors. Corrections were performed according to the scale as indicated. Following this, the corrected scale was sent again for the second round of expert consultation as the first round. The requirements and process for each round of inquiry were the same. When no differences in the results of the expert inquiry and consensus were reached, the inquiry ended. No further correspondence was needed when the problems in the evaluation index system could reach the concentration of expert opinions in the second round. If there is no consensus, the next round of consultation is performed, the specific process is shown in Supplementary Figure 2. Finally, all the contents achieving a consensus were included in the new version of the FOAC.
Phase 3: Face Validity
This study used the face validity index (FVI) to develop FOAC, which is primarily used to measure the frailty status of older adults with cancer.42
The face validity was determined by recording the views of two groups, including older adults with cancer and those with professional roles. The recorded items were presented to 18 participants, including 10 older adults with cancer aged 60 to 75 years, and eight professional roles (three geriatric nurses, three oncology nurses, and two geriatric nursing educators). This study adopted face-to-face surveys, where researchers held face-to-face meetings with participants to introduce the methods and objectives of the meeting, applicable conditions, the definition of time points, scoring methods, and precautions of the scale. The raters were asked to assess how well each item corresponds to or reflects a specific domain on a 4-point Likert scale. The scoring method was as follows: 1, not relevant; 2, somewhat relevant; 3, relevant; and 4, highly relevant. During the filling process, researchers encourage participants to express their opinions and opinions to ensure a consistent understanding of the items and dimensions. They were asked to answer every item, to comment on the ease of understanding each item, and to identify any ambiguous words or phrases. Moreover, the average length of time used to complete the questionnaire was assessed.
Phase 4: Criterion Validity
The validation of calibration validity is primarily based on a recognized and valid scale, investigating the correlation between the measurement results of the current scale and standard scales’ measurement results. The measured correlation coefficient is the validity of the current scale, and the larger the correlation coefficient, the better the calibration validity of the scale.43
This study used CGA as the calibration standard for the dichotomous population determined by the gold standard, that is, “frail” and “non-frail”. The diagnostic tests that should be evaluated were used to predict, and the diagnostic results were written as positive and negative. Additionally, the screening accuracy of three frailty screening scales, the FOAC, FP, and aCGA, were compared using CGA-determined frailty as the dependent variable, and their clinical application values were explored to provide a reference for clinical cancer frailty treatment in China.
Sample and Data Collection
After item generation, content validation, and face validation, systematic sampling methods based on registration for outpatients in the First affiliated hospital of Bengbu Medical University were recruited. Bengbu Medical College First Affiliated Hospital is an important cancer treatment centre in Anhui Province that serves patients who are directly or indirectly referred from Bengbu city and its surrounding areas. Therefore, the eligible participants represent a diverse group of participants from all districts in Bengbu and could thus be said to represent the older adults with cancer within the district area from which they live.
The inclusion criteria were as follows: ① age ≥60 years; ② those diagnosed with a malignant tumor by pathological examination and were fully aware of their condition; ③ those with normal reading, comprehension, and expression skills and could undergo physical assessment tests; ④ those who signed the informed consent and voluntarily participated in the study; and ⑤ those with the expectation of life ≥ 6 months. Based on information such as tumor type, tumor stage, and patient condition, specialized medical personnel made judgments based on their experience).44 According to the literature, the ratio of frailty to non-frailty is 0.42/0.58. The sensitivity and specificity of the standard method (aCGA) are 85% and 80%, respectively.45 However, the sensitivity and specificity of the new method (FOAC) were anticipated to reach 90% (taking α =0.05, β=0.2. Using the PASS 2021 software and considering a 10% invalid response, the calculated sample size was 72 cases of frailty and 99 cases of non-frailty, totaling 171 cases.
Research Instruments
- Sociodemographic data questionnaire: age (based on the date of birth, calculate the actual age of the older adults); sex; education level; marital status; living conditions (Living alone or with family members);per capita monthly income of the family; and type of medical insurance. Disease history: tumor type; metastasis status; surgical type; and the coexistence of multiple diseases.
- FP: It was proposed by Fried et al22 in 2001 and comprises weight loss, low grip strength, fatigue, and standing and walking timing tests. After the Chinese translation, this scale has become one of China’s most commonly used frailty assessment tools, with five dimensions of low physical activity.46 Among them, the physical activity level assessment adopts the International Physical Activity Short Questionnaire.47 The scoring method is as follows: “Yes” scored 1 point, “No” scored 0 points, and the total score ranges from 0 to 5 points. Based on the FP evaluation criteria, ≥ 3 points indicated frailty. The Cronbach’s alpha of this scale is 0.801.
- CGA: The CGA assessment system includes functional status, comorbidities, combination therapy, nutrition, cognition, psychology, socio-economic status, and geriatric syndrome.48 (a) Functional dependence:49,50 The Katz Activities of Daily Living (ADL) scale evaluates whether patients can independently complete tasks such as bathing, dressing, toileting, moving, eating, and controlling urination and defecation. Each item is scored 1 point, with<6 points indicating impaired ADL. The Lawton Instrumental Activities of Daily Living (ADL) Scale evaluates whether patients can independently complete 8 daily activities, including household chores, financial management, phone use, medication, etc. 1 point for each item<8 points indicates IADL limited. (b) High risk of falling:51 Perform a 3 m standing-up walking test to evaluate the patient’s walking gait and balance ability. If the timing is more significant than 13 seconds or cannot be completed, it is defined as a high risk of falling. Have a history of falls or not in the past year. (c) Combined diseases:49,50 The Charlson comorbidity index (CCI) evaluates the severity of comorbidities in patients, with a score of ≥ 4 indicating severe comorbidities. (d) Multiple use of medication: taking at least 5 oral medications. (e) Cognition:49,50 The Mini-Mental State Examination (MMSE) scale has a total score of 30 points, adjusted for educational level, with an illiterate (uneducated) group scoring 17 points; 20 points for primary school (education years ≤ 6 years) group; 24 points for high school or above (education years>6 years) group. Below the threshold value is cognitive impairment, while above is expected. (f) Depressive state:49,50 The Geriatric Depression Scale (GDS-15) has a total score of 15 points, with a score of ≥ 7 indicating depression. (g) High risk of malnutrition/malnutrition:49,50 Mini nutritional assessment (MNA) scale, 17–23 malnutrition risk <17 malnutrition. (h) Have there been any symptoms of urinary incontinence in the past year? (i) Insufficient social support,50 including the availability of caregivers and the ability to pay for medical expenses. (j) Visual and hearing impairments: Visual or hearing impairments affect daily life. (k) Pain: Numerical Analog Scale (NAS), with a total score of 10 points, with a score greater than 7 indicating pain. According to the recommendations of the Gerontology Oncology working group,49,52 if a patient has ≥ 2 abnormal indicators, it is defined as frailty.
- aCGA: To add three dimensions of functional indicators, concurrent diseases, and geriatric syndrome to Overcash, This study used the Chinese version of aCGA by Lin Yan et al.23 The Chinese version of the aCGA grading criteria is revised as follows: including Activities of Daily Living (ADL),53 Instrumental ADL,54 Mini Nutritional Assessment Short form,55 Geriatric Depression Scale,56 comorbidity burden,57 and geriatric syndrome, totaling 5 dimensions and 40 items. This scale covering the primary content of the overall assessment compared to a single physical condition score assigns a total score of 9 points.
- FOAC: After surface validity and content validity tests, FOAC had three dimensions namely, physical function, psychological cognition, and social support, with a total of 30 items. Of these, 29 were scored using the Likert 4-point scoring method (language repetition items were not scored in the psychological cognition dimension), with a score range of 29 to 116 points.
Statistical Analysis
The statistical software used in this study was IBM® SPSS Statistics (version 26.0, manufacturer: IBM Corporation, USA). The ROC curve analysis was also completed using MedCalc® 20.010 software (manufacturer: MedCalc Software Ltd, Belgium).
Statistical significance was set at p<0.05. Demographic characteristics were described using descriptive statistics, such as means and frequency for continuous and categorical variables, respectively, as appropriate. As for the expert panel evaluation, Microsoft Excel was used to analyze the content validity index (CVI) and Face validity index (FVI) in content and face validity, respectively.
Using CGA-determined frailty as the dependent variable, receiver operating characteristic (ROC) curve analysis was conducted using FOAC, FP, and aCGA frailty screening scales as independent variables. The ROC curves of each variable were plotted using MedCalc, and their area under the curve AUC (Area Under Curve), sensitivity, specificity, cut-off value, predicted value, and accuracy were determined. The AUC differences of various variables were compared using the DeLong test and statistical significance was determined. Generally, AUC values of 0.5–0.7, 0.7–0.9, and 0.9–1.0 represent low, high, and extremely high prediction accuracies, respectively.58 The test level α=0.05.
Ethical Consideration
The institutional review board/ethics committee reviewed and approved the study protocol. The Jawatankuasa Etika Penyelidikan (Manusia) JEPeM University Sains Malaysia (JEPeM Code: USM/JEPeM/KK/24010126) and Ethics Committee of Bengbu Medical University (protocol code KLZP [2023] No.257) provided the ethical approval. Potential study participants were provided with a detailed study description and were assured of confidentiality. Written and informed consent was obtained from each participant. The participants were also informed regarding the voluntary nature of the study participation and completion without any negative consequences.
Results
Demographic Characteristics
A total of 171 older adults with cancer participated in this cross-sectional study. There were 87 men and 84 women. Participant details are presented in Table 1. The collected questionnaires were screened according to the standard and all items with the same answer that remained unanswered within the specified time were deleted. The final distribution of 195 questionnaires resulted in 171 valid responses, with an effective response rate of 87.69%.
 |
Table 1 Characteristics of the Study Participants |
Phase 1: Item Generation
In the preliminary phase, after reviewing the relevant literature and guidelines, 32 items were extracted. Then, items were organized into four subscales with sub-domains. After removing three repetitive items, the first draft of FOAC included 32 items (12, 13, and 7 items on the physical functional, psychological and cognitive, and social support dimensions, respectively).
Phase 2: Content Validity
The standard of expert consensus was set at I-CVI (Item Content Validity Index) ≥ 0.7. Meanwhile, following the suggestions of Polit et al, items with I-CVI values below the standard were deleted or modified.39
Based on the comments of the expert panel, two items with item-level content validity index (I-CVI) values of 0.40 and 0.60 were excluded, three items were revised and 27 items were retained (Table 2). After excluding two items with unsatisfactory I-CVI, the scale-level content validity index (S-CVI)/Ave and S-CVI/UA values of the 30 items were 0.89 and 0.94, respectively (Table 2). Item-wise modified kappa statistics for FOAC ranged between 0.245–1.
 |
Table 2 Rating and Calculation of Item-Level Content Validity Index (I-CVI) and S-CVI of the Comprehensive Frailty Assessment Tool for Older Adults with Cancer (FOAC) |
Based on both the indices (I–CVI and S–CVI) and Modified Kappa Statistics, the FOAC elicited overall acceptable content validity.
Phase 3: Face Validity
This study adopted the method proposed by Yusoff et al (2019) to calculate FVI.42 I-FVI = Number of rater scoring 3 or 4/ number of rater42 and the criterion for expert consensus was established as I-FVI ≥ 0.7.
The FOAC was applied to 18 participants to assess the face validity of the test items. Based on the comments of the participants, most of the items with I-FVI values of over 0.7, 3 items were revised. Only a few minor issues were reported during the discussion meetings considering the phrasing and wording of the FOAC. Therefore, minor revisions were made during this phase. For example, the eighth item in the psychological and cognitive dimension provides three cards printed with lions, rhinoceroses, and camels, modified to incorporate goats, roosters, and water buffaloes that are more common among elderly individuals in China. The seventh connecting question will modify the sequence of Chinese characters such as “甲, 乙, 丙, 丁, and 戊” to more easily comprehensible Arabic numerals ranging from 1 to 10. Additionally, according to the evaluation opinions of the expert group, in the social support dimension, “Is there anyone who can help you with daily activities?” Was modified to “Is there anyone who can help you with daily tasks such as shopping, cooking, and cleaning in daily life?” The fluency and comprehensibility for the FOAC were confirmed by all the participants, indicating the good face validity of the test.
Phase 4: Criterion Validity
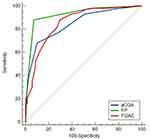
The frailty determined by CGA was taken as the dependent variable (CGA ≥ 2 and < 2 assigned a value of 1 and 0, respectively). The total score and its constituent dimensions of the FOAC, FP, and aCGA scales (variable input method was to input the original value) were used as independent variables for ROC curve analysis. The optimal cut-off values, sensitivity, specificity, predictive values, and accuracy values of each screening scale are shown in Figures 2, 3 and Table 3.
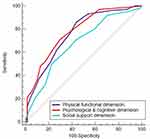 |
Figure 3 Receiver operating characteristic (ROC) curve analysis of various dimensions of the comprehensive frailty assessment tool for older adults with cancer (FOAC) scale. |
AUC is the area under the ROC curve. The range of the AUC value from 0 to 1, and the closer the AUC is to 1, the stronger is the discriminative ability.59 The results demonstrate that the FOAC and aCGA scales have high screening values, while the FP scale has an extremely high screening value for frailty.
The various components of the FOAC scale such as the physical function dimension, psychological cognition dimension, and social support dimension have specific predictive values for the frailty risk. The Delong test results exhibited that the AUC difference between the FOAC and aCGA scale was 0.008, with no statistically significant difference (Z = 0.215, P = 0.830). Table 4 details the comparison of the area under the ROC curve of the three scales.
Discussion
The aging of the global is intensifying, leading to an increased cancer risk.1 The elderly are the main affected population, and because of their limited physiological reserves, they are more vulnerable to social and functional harm. However, management and care of tumors in this population pose significant challenges.60 High-risk patients with frailty who require close monitoring or follow-up can be identified using the frailty screening tools for elderly patients with cancer, thereby making more effective use of existing medical resources.61 However, the frailty in elderly patients with cancer has not received sufficient attention in China, with most studies citing relevant frailty screening tools from abroad, whose reliability and validity fluctuate significantly in different studies, lacking local frailty assessment tools for such patients.62 Therefore, a frailty assessment tool suitable for elderly patients with cancer in China must be developed, considering the cultural background, medical conditions, health concepts, and social support methods.
The frailty evaluation of FOAC in a sample of older adults with cancer was developed and demonstrated. The frailty assessment provided sound evidence for its validity and reliability in evaluating evaluating physical functional dimension, psychological and cognitive dimension and social support dimension in older adults with cancer. This study’s findings exhibited acceptable content, face, criterion validities, and reliability.
The CVI of the total scale was 0.95, indicating that the items have been recognized by the experts and can effectively express the central content of their respective dimensions. The scale has good content validity.62 FOAC was deemed reasonable and acceptable because this study validated face validity through two different groups of participants, with a total surface validity index greater than 0.8. Additionally, the results of this study demonstrated that the overall Cronbach’s alpha coefficient of the scale was 0.869. This indicates a high internal consistency of this scale.
This study used CGA as the gold standard. Moreover, the AUC of FP, FOAC, and aCGA were 0.927, 0.856, and 0.848, respectively, indicating a better diagnostic performance of FP than FOAC and aCGA. In contrast, there was no statistically significant difference in diagnostic performance between FOAC and aCGA. By pairwise comparison of the AUC, the screening performance of FP was superior to that of FOAC and aCGA, while the screening performance of FOAC and aCGA was the same. Additionally, the optimal threshold values for each tool were determined using the screening tool’s ROC curve. The optimal critical values for FP and aCGA were 3 and 5, respectively, consistent with critical values set by Fried et al16 and Lin Yan et al,23 respectively. The optimal critical value of FOAC was 50, indicating that when FOAC was used to identify frailty in elderly patients with cancer, it could provide 88% sensitivity and 70.4% specificity.
Additionally, this study explores the optimal threshold values suitable for the elderly cancer patient population in China from the three dimensions of FOAC. The measurement of physical function is clinically significant in discovering and addressing potential functional limitations and nutritional status in older adults with cancer to further assess and intervene. Psychological and cognitive dimensions include measuring the patient’s psychological status and cognition level. The patient’s psychological and cognitive situation should be given attention and timely guidance and intervention when the score is ≥ 18. The aCGA, and other comprehensive assessment tools for the elderly, FOAC has added a dimension of social support compared to FP. The social support dimension covers various forms of assistance and resources that older adults with cancer can receive during the disease’s survival. When the social support score of older adults with cancer is ≥ 13, the patients have limited access to social assistance and resources.
The FOAC scale includes three dimensions (Physical functional dimension Psychological & cognitive dimension Social support dimension) in clinical practice, which is in accordance with the concept of multidimensional health under modern medical biology and health ecology.24,63 Compared with FP, which is currently the most widely used, although FP demonstrated good screening accuracy in this study, it primarily focuses on the physiological dimension of frailty assessment. Secondly, it requires professional medical staff and equipment during use, such as grip strength testers, and the cooperation of patients is needed to complete pace tests, which increases patient risk and is not conducive to clinical promotion.64 Lastly, the FOAC adjusted the standard of the physical function dimension compared with the FP scale. Based on the significant differences in dietary habits (such as types of meals and frequency of eating) between Chinese elderly and Western countries, FOAC modified “weight loss” to “weight change” to objectively demonstrate the relationship between weight changes and symptoms of frailty.65
Compared with the Chinese version of the comprehensive assessment tool aCGA, although the aCGA scale includes dimensions such as physical function and psychological cognition, patients should have a certain level of education.23 Most elderly patients were born in the early days of the discovery of the People’s Republic of China, and their educational level is generally low.65 Therefore, certain complex items are difficult to complete by them. Secondly, different scale dimensions have different scoring methods, and it takes more than 10 min for medical staff to assess patients and complete accurate scoring, increasing their workload in clinical applications.23 Furthermore, FOAC performs similarly in screening frailty in older adults with cancer and also has good frailty screening ability.22 However, FOAC has increased the measurement of social support levels in older adults with cancer as a multidimensional screening tool. Social support refers to individual spiritual or material assistance and support provided by organizations or individuals such as family, relatives, friends, and colleagues.66 Social support has been proven to be essential to multidimensional health.67,68 Additionally, the FOAC scale adopts the Likert four-point scoring method, unifying the scoring methods between different dimensions, reducing medical staff workload, and making it more convenient for clinical promotion and application.
In summary, the FOAC is a reliable and effective screening and evaluation tool for distinguishing and diagnosing elderly cancer patients with frailty symptoms. The medical staff can determine which patients require further evaluation and can adjust their treatment plans accordingly. The optimal FOAC threshold for screening frailty in older adults with cancer includes a satisfactory sensitivity-specificity balance. Thus, this study provides compelling evidence to support the putative diagnosis of frailty symptoms in older adults with cancer using FOAC.
This is the first frailty assessment tool constructed based on elderly cancer patients in China. To the best of our knowledge, this is the first study to use CGA as the gold standard and compare the FP and CGA scales to assess the screening ability of FOAC frailty. This helped in filling the gap in China’s lack of local frailty assessment tools. Future research can combine frailty assessment with clinical data to explore artificial intelligence prediction models based on machine learning or deep learning. By establishing a frailty risk stratification system for older cancer patients, early warning of individualized outcomes can be achieved to assist in the formulation of precise intervention plans in clinical practice.
Limitations
The study has several limitations. Firstly, this study was only conducted at the First Affiliated Hospital of Bengbu Medical College in Anhui Province. Although it included patients referred from multiple regions, it still cannot represent the overall situation of elderly cancer patients in different regions and hospitals of various medical levels across the country. Future research should expand the sample range and adopt a multi-centre survey design to enhance the external validity of the results. Secondly, the health status of older adults with cancer may vary significantly over time and be influenced by factors such as progression of disease and response to treatment. This cross-sectional study did not reflect the development trajectory of frailty in older adults with cancer. Therefore, further studies are recommended to investigate the occurrence and development trajectory of multidimensional frailty based on a large prospective cohort study to develop intervention strategies and provide reliable references for reversing or delaying the frailty process in older adults with cancer. What’s more, this study has self-report bias and cultural factor influence. Some items rely on self-perception (such as social support, psychological feelings, etc)., which may be affected by cultural expression habits. The application in Western populations needs to be adjusted. Future studies will combine objective indicators to further improve the objectivity and accuracy of the scale.
Conclusion
This study showed that FOAC is a 30-item multidimensional scale with good reliability and validity. It is a valid instrument that assesses physiological, psychological, cognitive, and social support levels, and its high sensitivity (88%) and multi-dimensional assessment provide an essential basis for the early identification and stratified management of older cancer patients.In clinical practice, FOAC can be a practical and efficient frailty screening tool in outpatient and inpatient settings. It assists healthcare providers in promptly identifying patients at high risk of frailty, optimizing individualized treatment plans, and proactively implementing appropriate measures to mitigate frailty, promote functional recovery, improve survival rates, and enhance the quality of life. Meanwhile, its scoring method is simple and straightforward, making it highly suitable for promotion and application in medical environments with limited resources.
Data Sharing Statement
Data analyzed for the current study are available from the corresponding author upon reasonable request.
Ethics
The institutional review board/ethics committee reviewed and approved the study protocol. The Jawatankuasa Etika Penyelidikan (Manusia) JEPeM University Sains Malaysia (JEPeM Code: USM/JEPeM/KK/24010126) and Ethics Committee of Bengbu Medical University (protocol code KLZP [2023] No.257) provided the ethical approval. Potential study participants were provided with a detailed study description and were assured of confidentiality. Written and informed consent was obtained from each participant. The participants were also informed regarding the voluntary nature of the study participation and completion without any negative consequences.
Acknowledgments
An unauthorized version of the Chinese MMSE was used by the study team without permission, however this has now been rectified with PAR. The MMSE is a copyrighted instrument and may not be used or reproduced in whole or in part, in any form or language, or by any means without written permission of PAR (www.parinc.com).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work is supported by the Key Humanities and Social Sciences Project of Bengbu Medical College [2020byzd214sk] and Key Projects of Humanities and Social Sciences in Anhui Province’s Universities[2024AH052825]. The funding body had no role in the study design, the collection, analysis, and interpretation of the data nor the preparation of the manuscript.
Disclosure
All authors declared no conflicts exist in this study, including employment, consultancies, stock ownership, honoraria, paid expert testimony, patent applications/registrations, and grants or other funding.
References
1. Dugue PA, Bassett JK, Joo JE, et al. DNA methylation-based biological aging and cancer risk and survival: pooled analysis of seven prospective studies. Int J Cancer. 2018;142(8):1611–1619. doi:10.1002/ijc.31189
2. Zheng R, Zhang S, Zeng H, et al. Cancer incidence and mortality in China, 2016. J Natl Cancer Cent. 2022;2(1):1–9. doi:10.1016/j.jncc.2022.02.002
3. Morley JE, Thomas DR, Wilson MM. Cachexia: pathophysiology and clinical relevance. Am J Clin Nutri. 2006;83(4):735–743. doi:10.1093/ajcn/83.4.735
4. Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. 2014;165–173. doi:10.1300/J018v05n01_09
5. Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–397. doi:10.1016/j.jamda.2013.03.022
6. Ethun CG, Bilen MA, Jani AB, et al. Frailty and cancer: implications for oncology surgery, medical oncology, and radiation oncology. Ca A Cancer J Clinicians. 2017;67(5):362–377. doi:10.3322/caac.21406
7. Nieman CL, Pitman KT, Tufaro AP, et al. The effect of frailty on short-term outcomes after head and neck cancer surgery. Laryngoscope. 2018;128(1):102–110. doi:10.1002/lary.26735
8. Runzer-Colmenares FM, Urrunaga-Pastor D, Aguirre LG, et al. Frailty and vulnerability as predictors of radiotoxicity in older adults: a longitudinal study in Peru. Medicina Clínica. 2017;149(8):325–330. doi:10.1016/j.medcle.2017.09.005
9. Kumar A, Langstraat CL, DeJong SR, et al. Functional not chronologic age: frailty index predicts outcomes in advanced ovarian cancer. Gynecol Oncol. 2017;147(1):104–109. doi:10.1016/j.ygyno.2017.07.126
10. de Arruda FN, Oonk MHM, Mourits MJE, et al. Determinants of health-related quality of life in elderly ovarian cancer patients: the role of frailty and dependence. Gynecol Oncol. 2019;153(3):610–615. doi:10.1016/j.ygyno.2019.03.249
11. Woldu SL, Sanli O, Clinton TN, et al. Validating the predictors of outcomes after radical cystectomy for bladder cancer. Cancer. 2019;125(2):223–231. doi:10.1002/cncr.31799
12. Kojima G, Iliffe S, Walters K. Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing. 2018;47(2):193–200. doi:10.1093/ageing/afx162
13. Cesari M, Abellan Van Kan G, Ariogul S, et al. The European Union Geriatric Medicine Society (EUGMS) working group on frailty in older persons. J Frailty Aging. 2013;2(3):118–120. doi:10.14283/jfa.2013.15
14. Rosiello G, Palumbo C, Knipper S, et al. Preoperative frailty predicts adverse short-term postoperative outcomes in patients treated with radical prostatectomy. Prostate Cancer Prostatic Diseases. 2020;23(4):573–580. doi:10.1038/s41391-020-0225-3
15. Shuli J, Birong D. Interpretation of the clinical practice guidelines for elderly frailty management in the Asia Pacific Region. Chin J Rehab Med. 2020;35(5):680–686. doi:10.36684/33-2020-1-680-686
16. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56. doi:10.1093/gerona/56.3.m146
17. Morley JE, Miller DK, Miller DK. A simple frailty questionnaire (frail) predicts outcomes. J Nutr Health Aging. 2012;16(7):601–608. doi:10.1007/s12603-012-0084-2
18. Hong GX. Study on the Chinese Version of Edmonton Frailty Scale (EFS) and the Frailty Status of Elderly Diabetes Patients. China Medical University; 2020.
19. Peters LL, Boter H, Buskens E, et al. Measurement properties of the Groningen frailty indicator in home-dwelling and in stitutionalized elderly people. J Am Med Dir Assoc. 2012;13(6):546–551. doi:10.1016/j.jamda.2012.04.007
20. Wildiers H, Heeren P, Puts M, et al. International society of geriatric oncology consensus on geriatric assessment in older patients with cancer. J Clin Oncol. 2014;32(24):2595–2603. doi:10.1200/jco.2013.54.8347
21. Yanyan Z, Juntao Y. Research progress on application of frailty screening tools in elderly cancer patients. J Chinese Oncol. 2020;26(5):245–249. doi:10.11735/j.issn.1671-170X.2020.03.B016
22. Overcash JA, Beckstead J, Extermann M, et al. The abbreviated comprehensive geriatric assessment (aCGA): a retrospective analysis. Crit Rev Oncol Hematol. 2005;54(2):129–136. doi:10.1016/j.critrevonc.2004.12.002
23. Lin Y, Song Y, Xu Y, et al. Application value of abbreviated comprehensive geriatric assessment in elderly female breast cancer patients. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2021;43(3):395–401. doi:10.3881/j.issn.1000-503X.13752
24. Xueting Q. Design of Personal Health Management Method Based on Multidimensional Data Model. Chongqing University; 2019.
25. Linlin Z, Qi L, Qinghua H, et al. Research on the multidimensional frailty in community-dwelling older adults. Chin Gen Pract. 2024;07(08):1–7. doi:10.12114/j.issn.1007-9572.2023.0719
26. Bandeen-Roche K, Seplaki CL, Huang J, et al. Frailty in older adults: a nationally representative profile in the United States. J Gerontol a Biol Sci Med Sci. 2015;70(11):1427–1434. doi:10.1093/gerona/glv133
27. Wang J, Zhao L, Yu D, et al. Status of nutrition and associated factors among the Chinese aged 60 and above in 2010-2012 in China. J Hyg Res. 2019;48(2):200–207.
28. Xing X, Guifang G, Jing S. Research progress on frailty assessment tools for the elderly and their applications. Chinese J Gerontol. 2015;20(10):5993–5996. doi:10.3969/j.issn.1005-9202.2015.20.153
29. Moldovan F, Moldovan L. Assessment of Patient Matters in Healthcare Facilities. Healthcare. 2024;12(3):325. doi:10.3390/healthcare12030325
30. Karen Freer SLW. Social frailty: the importance of social and environmental factors in predicting frailty in older adults. Br J Community Nurs. 2019;24(10):1462–4753. doi:10.12968/bjcn.2019.24.10.486
31. Li Y, Mai C. Research progress in health ecology. J Jining Med Univ. 2022;45(4):229–233. doi:10.3969/j.issn.1000-9760.2022.04.001
32. Yanrui J. The Research of Comprehensive Geriatric Assessment (Cga)in Elderly Cancer Patients for Chemotherapy. Shandong University; 2016.
33. Cespedes feliciano EM, Vasan S, Luo J, et al. Long-term trajectories of physical function decline in women with and without cancer. JAMA Oncol. 2023;9(3):395–403. doi:10.1001/jamaoncol.2022.6881
34. Demark-Wahnefried W, Pinto BM, Gritz ER. Promoting health and physical function among cancer survivors: potential for prevention and questions that remain. J Clin Oncol. 2006;24(32):5125–5131. doi:10.1200/jco.2006.06.6175
35. King S, Green HJ. Psychological intervention for improving cognitive function in cancer survivors: a literature review and randomized controlled trial. Front Oncol. 2015;5:72. doi:10.3389/fonc.2015.00072
36. Reis JC, Antoni MH, Travado L. Emotional distress, brain functioning, and biobehavioral processes in cancer patients: a neuroimaging review and future directions. CNS Spectr. 2020;25(1):79–100. doi:10.1017/S1092852918001621
37. Kadambi S, Soto-Perez-de-Celis E, Garg T, et al. Social support for older adults with cancer: young International Society of Geriatric Oncology review paper. J Geriatr Oncol. 2020;11(2):217–224. doi:10.1016/j.jgo.2019.09.005
38. Freer K, Wallington SL. Social frailty: the importance of social and environmental factors in predicting frailty in older adults. Br J Community Nurs. 2019;24(10):486–492. doi:10.12968/bjcn.2019.24.10.486
39. Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007;30(4):459–467. doi:10.1002/nur.20199
40. Shi J, Mo X, Sun Z. Content validity index in scale development. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2012;37(2):152–155. doi:10.3969/j.issn.1672-7347.2012.02.007
41. Yusoff MSB. ABC of content validation and content validity index calculation. Educ Med J. 2019;11(2):49–54. doi:10.21315/eimj2019.11.2.6
42. Yusoff MSB. ABC of response process validation and face validity index calculation. Educ Med J. 2019;11(10.21315). doi:10.21315/EIMJ2019.11.3.6
43. Chin Y. Reliability and Validity OfChinese Version Endometriosis Health Profile-5 Author. Shanghai Jiao-Tong University School; 2018.
44. Morita T, Tsunoda J, Inoue S, et al. The palliative prognostic index: a scoring system for survival prediction of terminally ill cancer patients. Support Care Cancer. 1999;7(3):128–133. doi:10.1007/s005200050242
45. Smets IH, Kempen GI, Janssen-Heijnen ML, Deckx L, Buntinx FJ, van den Akker M. et alFour screening instruments for frailty in older patients with and without cancer: a diagnostic study. BMC Geriatr. 2014;14(1):26. doi:10.1186/1471-2318-14-26
46. Lirong L, Limei S, Liyi L, et al. Overview of weakness assessment and its application in cancer patients. Intern Med. 2021;16(4):485–488.
47. Ningning Q, Keji L. Physical activity questionnaire study on the reliability and validity of international. China J Epidemiol. 2004;25(3):265–268.
48. Parker SG, McCue P, Phelps K, et al. What is Comprehensive Geriatric Assessment (CGA)? An umbrella review. Age Ageing. 2018;47(1):149–155. doi:10.1093/ageing/afx166
49. Hurria A, Wildes T, Blair SL, et al. Senior adult oncology, version 2.2014: clinical practice guidelines in oncology. J National Comprehen Canc Network. 2014;12(1):82–126. doi:10.6004/jnccn.2014.0009
50. Li D, Soto-Perez-de-Celis E, Hurria A. Geriatric assessment and tools for predicting treatment toxicity in older adults with cancer. Cancer J. 2017;23(4):206–210. doi:10.1097/ppo.0000000000000269
51. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi:10.1111/j.1532-5415.1991.tb01616.x
52. Mohile SG, Velarde C, Hurria A, et al. Geriatric assessment-guided care processes for older adults: a delphi consensus of geriatric oncology experts. J Natl Compr Cancer Netw. 2015;13(9):1120–1130. doi:10.6004/jnccn.2015.0137
53. Katz S, Downs TD, Cash HR, et al. Progress in development of the index of ADL. Gerontologist. 1970;10(1):20–30. doi:10.1093/geront/10.1_part_1.20
54. Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983;31(12):721–727. doi:10.1111/j.1532-5415.1983.tb03391.x
55. Kaiser MJ, Bauer JM, Ramsch C, et al. Validation of the mini nutritional assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9):782–788. doi:10.1007/s12603-009-0214-7
56. Dias F, Teixeira AL, Guimaraes HC, et al. Accuracy of the 15-item Geriatric Depression Scale (GDS-15) in a community-dwelling oldest-old sample: the Pieta study. Trends Psychiatry Psychother. 2017;39(4):276–279. doi:10.1590/2237-6089-2017-0046
57. Miller MD, Paradis CF, Houck PR, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the cumulative illness rating scale. Psychiatry Res. 1992;41(3):237–248. doi:10.1016/0165-1781(92)90005-n
58. Yangchun Z, Xueli J, Li Z, et al. Reliability and validity of trauma team activation criteria in emergency triage. J Nurs Sci. 2021;l36(19):39–43.
59. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36. doi:10.1148/radiology.143.1.7063747
60. Gironés Sarrió R, Antonio Rebollo M, Molina Garrido MJ, et al. General recommendations paper on the management of older patients with cancer: the SEOM geriatric oncology task force’s position statement. Clin Transl Oncol. 2018;20(10):1246–1251. doi:10.1007/s12094-018-1856-x
61. Handforth C, Clegg A, Young C, et al. The prevalence and outcomes of frailty in older cancer patients: a systematic review. Ann Oncol. 2015;26(6):1091–1101. doi:10.1093/annonc/mdu540
62. Zhi L, Xiuying H. Research progress on screening tools for frailty in elderly cancer patients and their applications. Chinese J Gerontol. 2018;38(4):1786–1789.
63. Yanru F, Xuan D. Quality of life evaluation-a multidimensional health evaluation index. Chin Urban Rural Enterp Heal. 1996;(4):18–19.
64. Qin Z, Ming Y, Hui W, et al. Comparison of four frailty screening tools in elderly cancer patients. J Nurs Sci. 2023;38(15):92–96.
65. Zhenwu Z, Jiaju C, Long L. The general trend, new characteristics and corresponding pension policies of China’s aging population. J Shandong Univ. 2016;(3):27–35.
66. Jing B, Min S, Lili S, et al. Frailty in elderly patients with multiple myeloma and its influencing factors bian. Shang Hai Nurs. 2022;16(1):1–23.
67. Nishijima TF, Shimokawa M, Esaki T, et al. A 10-item frailty index based on a comprehensive geriatric assessment (FI-CGA-10) in older adults with cancer: development and construct validation. Oncologist. 2021;26(10):e1751–e1760. doi:10.1002/onco.13894
68. Yijuan Z, Xia H, Caiping Y, et al. The effect of social support on the psychological and quality of life of elderly patients with breast cancer. Heilongjiang Med J. 2019;32(4):995–997.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.