Back to Journals » Clinical Ophthalmology » Volume 18
Effect of Acupuncture Treatment on the Ocular Pain, Mental State and Ocular Surface Characteristics of Patients with Dry Eye Disease: A Non-Randomized Pilot Study
Authors Duan H, Zhou Y, Ma B, Liu R, Yang T, Chu H, Huo Z, Qi H
Received 2 May 2024
Accepted for publication 16 September 2024
Published 3 October 2024 Volume 2024:18 Pages 2751—2764
DOI https://doi.org/10.2147/OPTH.S476573
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hongyu Duan,1,* Yifan Zhou,2,* Baikai Ma,1,* Rongjun Liu,3 Tingting Yang,4 Hongling Chu,5 Zejun Huo,6 Hong Qi1
1Department of Ophthalmology, Peking University Third Hospital, Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Beijing, People’s Republic of China; 2Department of Ophthalmology, Beijing Friendship Hospital, Capital Medical University, Beijing, 100050, People’s Republic of China; 3Department of Ophthalmology, Peking University First Hospital, Beijing, People’s Republic of China; 4Department of Ophthalmology, Guangdong Provincial People’s Hospital, Southern Medical University, Guangzhou, People’s Republic of China; 5Research Center of Clinical Epidemiology, Peking University Third Hospital, Beijing, People’s Republic of China; 6Department of Traditional Chinese Medicine, Peking University Third Hospital, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hong Qi, Department of Ophthalmology, Peking University Third Hospital, Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, 49 North Garden Road, Haidian District, Beijing, 100191, People’s Republic of China, Email [email protected] Zejun Huo, Department of Traditional Chinese Medicine, Peking University Third Hospital, 49 North Garden Road, Haidian District, Beijing, 100191, People’s Republic of China, Email [email protected]
Background: Ocular pain is a prevalent symptom of dry eye disease (DED), which often accompanies potential psychological issues. The study aimed to explore whether acupuncture could improve ocular pain, mental state, and dry eye parameters in patients with DED.
Methods: The non-randomized pilot study included 48 patients divided into two groups: the acupuncture group (n=27) and the 0.3% sodium hyaluronate (SH) group (n=21). Participants in the acupuncture group underwent treatments on six bilateral acupuncture points (BL1, BL2, ST1, LI 20, SI1 and SI3) 3 times per week for 4 weeks. Patients in the SH group received 0.3% SH 4 times per day for 4 weeks. Ocular pain was assessed using the numerical rating scale (NRS), and mental state was evaluated through the self-rating anxiety scale (SAS) and self-rating depression scale (SDS). Ocular surface parameters, concentrations of inflammatory cytokines, and corneal nerve morphological indicators were measured at baseline, the first week, and the fourth week. Randomization procedures were not used in this study, and outcome assessors and statistical analysts were blinded.
Results: Compared with baseline, both NRS scores (from 5.91 ± 1.52 to 1.94 ± 1.57) and ocular surface discomfort index (OSDI) scores (from 49.75 ± 14.92 to 29.64 ± 18.79) were decreased after 1 and 4 weeks of treatment in both groups (all p < 0.05). At 4 weeks, the acupuncture group showed significant improvements, including increased tear break-up time (TBUT) and corneal perception, decreased SAS and SDS scores, and reduced concentrations of interleukin (IL)-1β, IL-6, and tumor necrosis factor (TNF)-α concentration in tears (all p < 0.05). These changes were not observed in the SH group (all p > 0.05).
Conclusion: Acupuncture treatment could improve ocular surface characteristics in patients with DED, and more importantly, it alleviates their ocular pain and depressive state. The anti-inflammatory effect of acupuncture may be involved in this process. Future research with larger, randomized controlled trials (RCTs) is necessary to confirm these findings and clarify the mechanisms involved.
Keywords: acupuncture, dry eye disease, ocular pain, depression, inflammatory cytokines
Introduction
Dry eye disease (DED) is one of the most common eye diseases in clinic and affects millions of population worldwide.1 It is a multifactorial disorder that disrupts the homeostasis of the tear film and is accompanied by various ocular symptoms, including pain, eye dryness, foreign body sensation, visual fatigue, and blurred vision. Factors contributing to the development of DED include tear film instability, hyperosmolarity, ocular surface inflammation, damage, and neurosensory abnormalities.2 According to the Dry Eye Workshop (DEWS) II report, the prevalence of DED worldwide ranges from 5 to 50%.1
Although evaluated in less than 10% of existing studies, ocular pain was rated by patients with DED as one of the most significant symptoms that need to be examined by researchers.3 Patients frequently report a variety of unpleasant sensations, including irritation, burning, dryness, photosensitivity, aching, and so forth. Nowadays, the pathophysiological mechanisms underlying ocular pain in DED remain largely unknown. Generally, pain disorders are divided into two types, nociceptive and neuropathic pain, both of which may be involved in patients with DED.4 Nociceptive pain primarily arises from noxious stimulus or disruptions in the ocular surface anatomy, while neuropathic pain is caused by abnormalities in the neurosensory apparatus of the ocular surface, including peripheral or central nerves.5 In addition, clinical data indicate that DED is often correlated with anxiety and depression syndromes.6 The depressive state is linked to the appearance or worsening of DED resulting from chronic eye pain.7 Considering the complexity of pathophysiological mechanisms and psychiatric comorbidities, managing and treating DED remains a frequent challenge for clinicians, especially for patients suffering from ocular pain. The low rate of satisfaction underlines the need for further investigation of effective therapies.
Acupuncture is widely accepted as a form of complementary and alternative medicine, which works by inserting fine needles at specific points known as acupuncture points (acupoints). Numerous clinical trials have demonstrated that acupuncture works for various ophthalmic disorders, such as acute conjunctivitis, cataracts, central retinitis, and myopia.8 Furthermore, several systematic reviews have shown that acupuncture is effective for DED by alleviating non-painful symptoms like dryness, burning, etc.9 Considering that high-quality trials from meta-analysis have shown that acupuncture is effective in treating chronic pain, including chronic musculoskeletal, headache, and osteoarthritis pain,10 we hypothesize that acupuncture will significantly reduce ocular pain and improve the overall condition of patients with DED compared to artificial tears. The study aims to evaluate the effectiveness of acupuncture compared to artificial tears in alleviating DED-related ocular pain. Additionally, it examines the impact of acupuncture on overall DED symptoms and signs, as well as mental health conditions at the end of the treatment (1 week and/or 4 weeks). Tear inflammatory factor levels and Corneal subbasal nerve morphology were also measured before and after acupuncture and 0.3% sodium hyaluronate (SH) therapy to investigate the mechanism of acupuncture in the treatment of ocular pain in patients with DED.
Materials and Methods
Study Population
The nonrandomized pilot study was conducted in the ophthalmic clinic of Peking University Third Hospital from December 2020 to March 2022. A total of 48 patients diagnosed with DED complaining of ocular pain were included in the study. All participants were assigned to either the acupuncture group or the SH group for 4 weeks of therapy (Figure 1). The inclusion criteria were as follows: patients with DED diagnosed according to the Tear Film and Ocular Surface Society (TFOS) DEWS II criteria2 and numerical rating scale (NRS) score > 1. Participants were 20–70 years old and could be of either gender. The duration of ocular pain was not limited. The exclusion criteria were: 1) eye surgery history within the past 2 years; 2) topical drug use other than artificial tears within the past month; 3) use of systemic medications that could alter pain and mood status, including analgesics, antidepressants, and antiepileptics; 4) a history of ocular diseases other than DED; 5) pregnant or lactating women. Prior to participants enrollment, the study was approved by the Peking University Third Hospital Medical Science Research Ethics Committee (IRB00006761-M2020284) and was registered at ClinicalTrial.gov (Registration number: NCT04668131). The study adhered to the Declaration of Helsinki. Informed consent was obtained from all participants before the study commenced.
 |
Figure 1 Flow diagram of the study. Abbreviation: SH, sodium hyaluronate. |
Intervention
Acupuncture group. Participants received acupuncture treatment, which lasted for 30 minutes each time, three times per week (every other day) for 4 weeks. The acupuncture procedures were performed in accordance with the STRICTA guidelines.11 Based on previous literatures and the textbook named Ophthalmology of Traditional Chinese Medicine (TCM), acupuncture points were determined by a committee of experts specializing in acupuncture and TCM ophthalmology. Six acupoints (Figure 2), including Jingming (BL 1), Cuanzhu (BL 2), Chengqi (ST 1), Yingxiang (LI 20), Shaoze (SI 1), and Houxi (SI 3), were located in accordance with WHO Standard Acupuncture Point Locations in the Western Pacific Region.12 All six acupoints have been used in the treatment of DED and chronic pain. Among them, BL1, BL2, and ST1 are the most commonly used periocular points for alleviating symptoms of DED.13 Guo et al14 reported that the LI20 point is particularly effective in prolonging the tear break-up time (TBUT) and increasing tear secretion. Additionally, SI1 and SI3 points are widely used to treat various painful conditions affecting multiple parts of the body.15 Acupuncture was performed by one skilled Chinese medicine physician (Z.H). with 20 years of experience in acupuncture manipulation. He holds an M.D. degree and is a registered practitioner of traditional Chinese medicine (TCM), specializing in TCM treatment of chronic pain and neurological diseases. Disposable acupuncture needles (0.3×15mm; Suzhou Medical Appliance Factory, Suzhou, China) were inserted subcutaneously into the acupoints quickly, and then slowly advanced 3–15mm. The needles were not lifted or twisted once inserted and were retained for 30 minutes before removal. The deqi sensation (soreness, numbness, distension, and heaviness) was present in all patients after needle insertion.
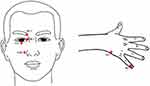 |
Figure 2 Location of the acupoints in the study. BL 1, Jingming acupoint. BL 2, Cuanzhu acupoint. ST 1, Chengqi acupoint. LI 20, Yingxiang acupoint. SI 1, Shaoze acupoint. SI 3, Houxi acupoint. |
SH group. Patients were treated with 0.3% SH eye drops (Sodium Hyaluronate Eye Drops, Santen Hialid® mini 0.3, Japan), 1 drop 4 times per day as needed for 4 weeks.
Participants were divided into either the acupuncture or control group according to their ability to complete 12 acupuncture treatments at Peking University Third Hospital. A stratified approach was used during the enrollment phase to ensure a balance of age, sex, and ocular pain severity between the two groups. Blinding was not implemented for clinicians and patients in this study because acupuncture and artificial tears treatments are easy to distinguish. In order to control the risk of bias, outcome assessors and statistical analysts were blinded. According to a systematic review and meta-analysis published in 2021, an acupuncture protocol of 21–30 days at a 2–3 times per week is optimal for treating typical DED9. We chose the 1-week time point to observe the short-term efficacy and the 4-week time point as the final data collection endpoint.
Primary Outcome Measurement
The primary outcome was the change from baseline in the NRS score at week 4. Participants were asked to rate the intensity of their average and worst eye pain over the past week using the NRS, which ranges from 0 to 10 [the most intense eye pain imaginable]. NRS values of 0 corresponded to no pain, 1–3 corresponded to mild pain levels, NRS values of 4–6 indicated moderate pain levels, and NRS values of ≥7 indicated severe pain levels.16 The 11-point NRS has been validated to evaluate pain intensity in multiple populations17,18 and was recommended as the primary outcome indicator in clinical trials for chronic pain.19 All patients completed the NRS assessments before treatment, and at 1 and 4 weeks post-treatment. The pain relief effective rate of treatment for DED-related ocular pain was calculated according to the NRS score. The decrease of pain level ≥ 1, such as a decrease from moderate pain to mild pain, was considered effective treatment and decrease of pain level < 1 indicating ineffective treatment. The effective rate of pain relief was calculated as the number of patients effective to the treatment divided by the total number of patients treated. NRS scores were collected at baseline, after 1st and 4th week of treatment.
Secondary Outcome Measurement
Ocular surface characteristics, including ocular surface discomfort index (OSDI), TBUT, corneal fluorescein staining (CFS) score, tear meniscus height (TMH), and corneal sensitivity data were collected at baseline, after 1 week, and after 4 weeks of treatment. Note that the TMH data was collected only at baseline and at the fourth week. Subjective symptoms of DED were assessed using the OSDI. Administering a moist fluorescein strip to the inferior fornix, TBUT was measured by calculating the average of three consecutive break-up times and CFS was performed following the National Eye Institute grading system,20 which reflects the tear film stability and ocular surface damage, respectively. TMH, an important indicator of tear secretion, was measured using a Keratograph 5M noninvasive ocular surface analyzer (Oculus, Germany). Corneal sensitivity was evaluated with a Cochet-Bonnet esthesiometer (Luneau Ophtalmologie, Chartres, France), which assess the perception function of the corneal nerves.
Other secondary outcomes included the self-rating anxiety scale (SAS) score, self-rating depression scale (SDS) score, tear inflammatory cytokine levels, and corneal nerve morphology parameters, which were assessed only at baseline and 4 weeks after treatment. These parameters reflect the patient’s psychological state, tear inflammatory levels, and changes in corneal nerve morphology, making them valuable for evaluating the effectiveness of acupuncture in treating ocular pain of patients with DED. Specific evaluation methods are detailed below.
Assessment of Psychological Conditions
Li et al found a correlation between OSDI scores and psychological states (SAS, SDS), indicating that the psychological state of patients with DED is related to their perceived quality of life. Moreover, patients of DED with ocular pain often experience psychological issues. Therefore, the SAS and SDS scales were chosen to assess patients’ anxiety and depression, respectively, at baseline and after 4 weeks of treatment. Both the SAS and SDS composes 20-item and a four-point Likert scale ranging from 1 (“little or none of the time”) to 4 (“most of the time”), with higher scores indicating higher levels of anxiety or depression. The total score is multiplied by 1.25 and then converted into a standardized score ranging from 25 to 100. Both scales have been validated and widely used to assess anxiety and depression associated with a variety of diseases.
Tear Collection and Testing
5 μL minimally stimulated basal tears from each eye were collected by placing a microcapillary glass tube (Microcaps; Drummond Scientific Co, Broomall, PA) over the temporal side of the lower lid. Tear samples were immediately placed on ice and then stored at –80°C. Cytokines, including interleukin (IL)-1β, IL-6, tumor necrosis factor (TNF)-α, and monocyte chemoattractant protein-1 (MCP-1) were measured by Luminex Assay (Luminex MAGPIX, Luminex Corp). using associated kit (MILLIPLEX MAP® Human Adipokine Magnetic Bead Panel) following the manufacturer’s instructions. The minimal detectable doses (picograms per milliliter, pg/mL) for IL-1β, IL-6, TNF-α, and MCP-1 were 0.4, 0.2, 0.3, and 1.2, respectively. All patients received tear sample collection before and after 4-week treatment.
Corneal Subbasal Nerve Analysis
In vivo confocal microscopy (IVCM) (Heidelberg Retina Tomograph 3/Rostock Cornea Module; Heidelberg Engineering GmbH, Heidelberg, Germany) was conducted to obtain corneal subbasal nerve images. Operation procedures and image acquisition were in accordance with our established protocol.21 Five non-overlapping images from the central corneal subbasal nerve plexus were selected per eye for automated image analysis using ACCMetrics software (ACCMetrics; M.A. Dabbah, Imaging Science and Biomedical Engineering, Manchester, UK). Corneal nerve fiber density (CNFD) (number of major nerves per mm2), corneal nerve branch number (CNBD) (number of nerve branches per mm2), and corneal nerve fiber length (CNFL) (total length of nerves in mm per mm2) were quantified. All subjects underwent IVCM before and 4 weeks after treatment.
Calculation of Sample Size and Statistical Analysis
We calculated sample size based on the primary outcome NRS score. There was no prior existing study on mean difference of NRS score in dry eye related pain after intervention. Referring to the changes of NRS score after acupuncture treatment for other chronic pain and our experience from two clinical experts, we think that the superiority of the acupuncture group over the SH group can be demonstrated when the mean difference of NRS score between two groups is reduced by more than 1.5, with standard deviation estimated to be 1.5.22 The number of subjects required for each group was 16 (α=0.05, β=0.2). Considering the 20% dropout rate, the final sample size was 20 per group. However, a total of 24 participants per group were included in the study to ensure adequate power and to accommodate any additional dropouts or data exclusions that might occur during the study.
Statistical analyses were performed using SPSS statistical software (version 22.0; SPSS, Chicago, IL). Data normality was verified using the Kolmogorov–Smirnov test. Data were presented as the mean±standard deviation. Categorical variables were described using composition ratios. An independent t-test and chi-square analysis were used to compare the baseline values between the acupuncture group and the SH group. For within-group comparisons to baseline values, paired samples t-tests was used. Analysis of covariance (ANCOVA) was used to explore between-group differences in different time-points after treatments. The potential effects of variables, including age, sex, and NRS and baseline parameters were corrected in the ANCOVA analysis. Chi-square test was used to compare the effective rate on pain relief between the two groups after treatment. For inflammatory factors and corneal neuromorphologic parameters, the nonparametric Wilcoxon test and the Mann–Whitney U-test were used for pre- and post-treatment comparisons within the same group and for between-group comparisons after 1 month of treatment in both groups, respectively. The statistical significance level chosen was p < 0.05.
Results
The Baseline Characteristics
Forty-eight subjects were eligible for the study to receive treatment of acupuncture (acupuncture group, n=27) or artificial tear (SH group, n=21). The demographic and baseline data are shown in Table 1, in which no significant differences between the two groups were observed in age, sex, duration of pain, SAS score, SDS score (p = 0.931, 0.675, 0.444, 0.105, and 0.086, respectively) and dry eye parameters (all p > 0.05). The baseline values of NRS were statistically different between the two groups (p = 0.034; acupuncture vs SH group: 5.91 ± 1.52 vs 4.90 ± 1.65).
 |
Table 1 The Baseline Characteristics of the Subjects |
NRS
For the primary outcome (Figure 3A), the NRS score was significantly reduced (both p < 0.05) in the acupuncture group after 1-week (3.98 ± 1.63) and 4-week (1.94 ± 1.57) treatment when compared with baseline (5.91 ± 1.52). Similarly, the NRS score was significantly reduced (both p < 0.05) in the SH group after 1-week (2.36 ± 1.54) and 4-week (1.88 ± 1.77) treatment when compared with baseline (4.90 ± 1.65). As shown in Table 2, the decrease in the NRS score at week 1 was greater in the SH group than in the acupuncture group, with a mean difference of 0.99 (95% CI, 0.19–1.79; p < 0.05). However, the NRS scores were not significantly different between both groups at week 4, indicating that the long-term benefits of acupuncture and artificial tears may be comparable. This suggests that while artificial tears might offer quicker relief, acupuncture could potentially offer sustained benefits that contribute to long-term pain management.
 |
Table 2 Changes in Ocular Pain, Mental State and Dry Eye Parameters in the Acupuncture Group and SH Group |
As presented in Figure 3B and C, the number of patients with ocular pain in the acupuncture group at baseline (1 mild pain, 14 moderate pain, and 12 severe pain), 1-week follow-up (10 mild pain, 15 moderate pain, and 2 severe pain) and 4-week follow-up (22 mild pain, 5 moderate pain, and 0 severe pain). In the SH group, the number of patients with ocular pain at baseline (2 mild pain, 14 moderate pain, and 5 severe pain), 1-week follow-up (13 mild pain, 8 moderate pain, and 0 severe pain) and 4-week follow-up (16 mild pain, 4 moderate pain, and 1 severe pain). After treatment, the short-term (1 week) pain relief effective rate of patients in the acupuncture group was 66.67%, while that in the SH group was 71.43%. The endpoint (4 weeks) pain relief effective rate of patients in the acupuncture group was 88.89%, while that in the SH group was 71.43%. There was no significant difference in pain relief effective rate between the two groups at 1st (P = 0.724) and 4th (P = 0.124) (Supplementary Table).
Mental State
Table 2, Figure 3D and E demonstrated the results of mental state in both treatment groups. After 4 weeks of treatment, the acupuncture group revealed a significant reduction in SAS scores compared to baseline (p < 0.05), while the SH group showed no significant change. Although there was no statistically significant difference in the SAS score changes between the two groups at week 4, the trend in the acupuncture group suggests potential benefits in reducing anxiety symptoms. In the acupuncture group, the SDS score showed a decreasing tendency during the treatment period, while those in the SH group rather increased. This difference became statistically significant between the groups at week 4 (p < 0.05), indicating that acupuncture may be more effective in alleviating depressive symptoms in patients with DED.
Dry Eye Parameters
The parameters for DED were summarized in Figure 3F and Table 2. OSDI is a comprehensive measure of the severity of dry eye symptoms and their impact on the patient’s quality of life. OSDI scores were significantly reduced in two groups after treatment throughout the study period (p < 0.05). There were no significant differences in the change of OSDI between both groups at week 1 and 4, indicating that while both treatments are beneficial, they may offer similar levels of symptom relief.
TBUT measures the stability of the tear film and provides insight into tear quality. After 1 week and 4 weeks of treatment, the acupuncture group revealed a significant reduction of TBUT compared to the baseline (p < 0.05), while the SH group still maintain a poor outcome in TBUT (Figure 3G). These results highlighted the potential advantage of acupuncture in enhancing tear film stability over artificial tears alone.
There was an overall decrease in CFS, assessing corneal damage, after 4 weeks of treatment in both groups, but the changes were not statistically different. No significant differences were found in the change of CFS between the two groups during the period of treatment (Figure 3H).
TMH is an indicator of tear production. Acupuncture led to a slight increase of TMH after 4 weeks treatment, although no statistical difference was indicated. However, the opposite trend was observed in the SH group, with a significant decrease in TMH after 4 weeks of treatment with artificial tears (p < 0.05). There were no significant differences in the change in TMH between the two groups after treatment (Figure 3I).
Corneal sensitivity is important for detecting and managing ocular discomfort. The acupuncture group revealed improvement at 1 week and 4 weeks of treatment (all p < 0.05) suggests a positive effect of acupuncture on nerve function and pain perception. In contrast, the SH group showed no significant change at the 1st and 4th week. There were no significant differences in the change of corneal sensitivity between both groups during treatment (Figure 3J).
Inflammatory Cytokines
As shown in Figure 4A–D, levels of IL-1β, IL-6, and TNF-α were decreased (p < 0.05) in the acupuncture group after 4-week treatment, compared to baseline. No changes were observed in the SH group after treatment. There were no significant differences in the changes of MCP-1 levels in both groups after 4 weeks of treatment.
Corneal Nerve Morphological Parameters
The results of corneal nerve morphological parameters were shown in Figure 4E–G. Both groups showed no significant changes in corneal nerve morphological parameters after treatment. No significant difference was found at 4-week treatment for CNFD, CNBD, and CNFL values between the acupuncture group and the SH group.
Discussion
In this pilot study, we compared the effect of acupuncture and 0.3% sodium hyaluronate for the treatment of DED-related ocular pain. Acupuncture led to greater improvements in tear film instability, corneal sensitivity, and mental state than artificial tears after 4 weeks of treatment. Additionally, acupuncture significantly reduced the levels of inflammatory cytokines IL-1β, IL-6, and TNF-α in the tears of DED patients post-treatment.
To the best of our knowledge, this is the first study to evaluate the effect of acupuncture on ocular pain and mental state in patients with DED. Nowadays, the pathophysiological mechanisms underlying ocular pain in DED remain largely unknown. Nociceptive pain and neuropathic pain, two types of disorders, may both be involved in the pathogenesis of DED. Nociceptive pain is typically transient, caused by tissue damage and inflammation, whereas neuropathic pain arises from a lesion or disease of the somatosensory nervous system. Neuropathic pain is manifested by an increased perception of pain in response to non-painful stimuli, and is more likely to be chronic.23 Ocular neuropathic pain is an exclusionary diagnosis, usually without visible abnormalities in objective exams, making it difficult to identify and often frequently misdiagnosed as DED or comorbid with DED.24 Although it is unclear whether the DED patients enrolled in our study experienced neuropathic ocular pain, both acupuncture and 0.3% SH were effective in alleviating their eye pain symptoms. The substantial reduction in NRS scores in both groups reflects meaningful improvements in pain levels, which are likely to enhance the patient’s overall quality of life and daily functioning.
We found the short-term effectiveness of acupuncture for DED-related ocular pain was 67%, increasing to 89% at the study endpoint. In contrast, the effectiveness of artificial tears remained consistent at 71% for both short-term and endpoint evaluations. These comparable outcomes highlight that while both treatments are effective, they may serve different roles in managing DED. Artificial tears provide valuable immediate relief for acute symptoms, while acupuncture may offer more sustained benefits by addressing underlying factors contributing to ocular pain in DED. Several studies have explored the mechanisms of acupuncture analgesia, such as promoting neurotransmitter release, increasing the local blood flow, and improving the muscle movement synergy.25 In our study, the acupuncture group showed improved mental states and reduced inflammatory cytokine levels after treatment compared to the SH group, which may be beneficial to alleviate ocular pain in DED. Currently, artificial tears remain the first-line eye drops of choice for patients with DED-related pain due to their high efficacy among topical ophthalmic medications.26 A cross-sectional study by Galor et al reported artificial tears use to treat DED-associated ocular pain, 19% reported no improvement, 62% reported partial improvement and 19% reported complete improvement.27 Similar results with 14% of patients who used artificial tears reporting no improvement, 55% partial improvement, and 31% “a lot” of improvement in ocular pain with artificial tears.26 Our study also showed a similar pain improvement effect of artificial tear.
Ocular pain in DED is closely associated with anxiety and depression. In 2017, a study from Florida assessed 181 patients with dry eye symptoms and categorized them based on the presence of corneal neuropathic pain symptoms (such as burning, sensitivity to wind, light, and temperature extremes) into “high corneal neuropathic pain” and “low corneal neuropathic pain” groups. The results indicated that patients with more severe corneal neuropathic pain symptoms often experienced greater depression.28 Addressing anxiety and depression is crucial in managing pain, as these psychological factors significantly affect the patient’s pain experience. Treating comorbid anxiety and depression can enhance the effectiveness of pain-specific treatments.29 Acupuncture’s efficacy in reducing anxiety has been well-documented. A review by the British Acupuncture Council highlighted that acupuncture could improve anxiety symptoms.30 Similarly, a systematic review, including 32 clinical and preclinical studies, affirmed the significant impact of acupuncture on anxiety.31 However, there are currently no clinical studies specifically reporting on the effects of acupuncture for treating ocular pain and its associated anxiety and depression symptoms in patients with DED. Only a case study of a 53-year-old male with DED and anxiety showed significant and sustained improvements in both DED and anxiety symptoms following 3 weeks of acupuncture treatment and a 3-month follow-up, suggesting that acupuncture may be effective for anxiety associated with DED.32
In our study, we observed that acupuncture improved anxiety and depression in patients with DED, potentially contributing to relief from ocular pain. Mechanistically, research suggests that electroacupuncture may alleviate anxiety related to neuropathic pain by reducing neurogenic inflammation in the amygdala and modulating the dopamine system.33 Currently, the exact mechanisms through which acupuncture alleviates ocular pain and associated anxiety and depression in DED patients remain unclear, and future research should explore these mechanisms from a neurobiological perspective.
Numerous systematic reviews have demonstrated that acupuncture is effective for DED, especially in improving the OSDI and TBUT.34,35 Unlike other studies that found the superiority of acupuncture in improving symptom scores, TBUT, CFS and Schirmer test compared to artificial tears, our study demonstrated no significant difference between acupuncture and artificial tears in improving OSDI and TBUT. Different acupuncture points and frequency and the choice of the control group may be the main contributions to the difference. An acupuncture protocol for 21–30 days at 2–3 times per week is recommended as an optimal frequency to maximize the therapeutic effects.9 The present study also aligns with these recommendations. Numerous studies have suggested that acupuncture has obvious curative effects in the treatment of DED, but the specific mechanism remains elusive. The proposed mechanisms include promoting tear section,36 reducing pain and inflammation,37 increasing local blood flow38 and regulating the autonomic nervous and immune systems.39 Additionally, the control group in the present study used 0.3% SH, whereas most previous studies used 0.1% SH. A higher concentration of SH has more advantages in improving tear film stability and ocular surface homeostasis,40 which may also be a reason why our results differ from the previous studies regarding dry eye parameters.
Inflammation is an important contributing factor to pain, and certain pro-inflammatory cytokines, including IL-1β, IL-6, TNF-α, and MCP-1, have been implicated in the process of pathological pain.41 A previous study demonstrated that the expression of IL-1β protein in the cornea was decreased after electroacupuncture treatment in a rat model of DED.42 In the present study, the levels of inflammatory cytokines (IL-1β, IL-6, and TNF-α) in tears was found to significantly decrease following acupuncture treatment. IL-1β has been well known as an important pain mediator which sensitizes or directly activates the nociceptors.43 In the eye, therapies that inhibit the production of IL-1β may help improve disease outcomes.44 Animal studies have shown that blocking IL-6 attenuates neuropathic pain.45 In addition, subcutaneous injection of TNF-ɑ in rats sensitized their injury receptors, reducing the threshold for 66.7% of nerve fibers to painful stimuli and triggering persistent electrical activity in about 14% of injury receptors.46 Therefore, it is hypothesized that the change of IL-1β, IL-6, and TNF-α may be involved in the mechanism of acupuncture efficacy in treating DED-related pain, which constitutes an exciting direction for future studies.
To our knowledge, there are no reports describing the effects of acupuncture on corneal nerve morphology and function. In our study, no significant changes in corneal nerve morphological parameters were observed after acupuncture or SH treatment. However, acupuncture treatment could improve the corneal perception of DED patient, which has never been reported in previous clinical study. According to the basic research of Shen et al,47 electroacupuncture can alleviate the damage of sensory neurons in dry eye model guinea pigs. We speculate that acupuncture may be beneficial to corneal function by influencing corneal neuronal activity.
DED is a multifactorial disease often associated with psychological or neurological disorders, such as depression, anxiety and neuropathic pain. While most studies on the association between DED and psychiatric or neurological disorders are cross-sectional and fail to show causality, the tight binding between DED and various psychiatric or neurological disorders suggests the existence of common pathophysiological mechanisms or interactions among them.48 Sometimes, approaches for the treatment of ocular pain require collaboration across various fields, including neuroscience, neurology, and pain management, beyond just ophthalmology.49 In such cases, integrated or alternative therapies may offer greater benefits, and acupuncture represents a promising option. Additionally, considering the varied acupuncture protocols and high heterogeneity in existing studies, there is an urgent need to establish a standardized and optical method for the treatment of DED.9 Combining acupuncture with 0.3% SH may be more effective than each alone in alleviating the ocular pain of DED patients. The focus on future research will inevitably be to provide safer and more effective treatments for DED-related eye pain.
The study has some limitations. Firstly, the present study design involves a nonrandomized intervention considering patient compliance, ethical concerns, and the nature of a pilot study, which may induce selection bias and affect the results of the findings. Consequently, ANCOVA was applied in the study to compare the difference in efficacy between the two treatments after correcting for baseline characteristics (particularly differences in NRS scores between the groups) and confounding factors. Stratified enrollment and matching are also solution to the nonrandomized research but not suitable for our study. Secondly, participant and clinician blinding is lack in the study due to the specificity of acupuncture treatment. However, we believe that the blinding of outcome assessors and statistical analysts, contribute to the overall robustness of our study results. Thirdly, the present sample size of the pilot study was not that large given the exploratory nature of the study, and further randomised controlled trials (RCTs) with larger sample sizes should be performed to confirm our results and further explore the effects of acupuncture on DED and associated symptoms. Additionally, the study was conducted in a specialized clinic with experienced acupuncture practitioners, which may not represent outcomes in general clinical settings or areas with limited access to specialized care. Future studies should include diverse clinical settings to improve generalizability.
Conclusion
Acupuncture significantly alleviates ocular pain, improves mental state, and enhances ocular surface parameters in patients with DED. These effects are potentially mediated by reductions in inflammatory markers such as IL-1β, IL-6, and TNF-α. The findings suggest that acupuncture may be a valuable complementary therapy for treating DED-related ocular pain. Future research should focus on larger RCTs and long-term studies (> 4 weeks) to further validate these results and explore the underlying mechanisms.
Data Sharing Statement
Study protocol and individual participant data that underlie the results reported in this study (after deidentification) can be obtained from the correspondence author based on reasonable request.
Author Contributions
All authors made substantial contributions to the work reported, including the conception and design of the study, execution, data acquisition, analysis, and interpretation. They participated in drafting, revising, or critically reviewing the manuscript; provided final approval for the version to be published; agreed on the journal to which the article has been submitted; and are accountable for all aspects of the work.
Funding
This work was supported by The Capital Health Research and Development of Special (2020-2-4097), National Natural Science Foundation of China (82371026, 82171022, 82301177).
Disclosure
The authors declare no conflict of interest.
References
1. Stapleton F, Alves M, Bunya V, et al. TFOS DEWS II epidemiology report. Ocular Surf. 2017;15(3):334–365. doi:10.1016/j.jtos.2017.05.003
2. Craig J, Nichols K, Akpek E, et al. TFOS DEWS II definition and classification report. Ocular Surf. 2017;15(3):276–283. doi:10.1016/j.jtos.2017.05.008
3. Saldanha I, Petris R, Han G, Dickersin K, Akpek E. Research questions and outcomes prioritized by patients with dry eye. JAMA Ophthalmol. 2018;136(10):1170–1179. doi:10.1001/jamaophthalmol.2018.3352
4. Galor A, Levitt R, Felix E, Martin E, Sarantopoulos C. Neuropathic ocular pain: An important yet underevaluated feature of dry eye. Eye. 2015;29(3):301–312. doi:10.1038/eye.2014.263
5. Mehra D, Cohen NK, Galor A. Ocular surface pain: A narrative review. Ophthalmol Ther. 2020;9(3):1–21. doi:10.1007/s40123-020-00263-9
6. Li M, Gong L, Sun X, Chapin W. Anxiety and depression in patients with dry eye syndrome. Current Eye Res. 2011;36(1):1–7. doi:10.3109/02713683.2010.519850
7. Vieira G, Rodrigues B, Cunha C, Morais G, Ferreira L, Ribeiro M. Depression and dry eye: A narrative review. Revista da Associacao Medica Brasileira. 2021;67(3):462–467. doi:10.1590/1806-9282.20200888
8. Stux G, Berman B, Pomeranz B. Basics of Acupuncture.
9. Na J, Jung J, Park J, Song P, Song C. Therapeutic effects of acupuncture in typical dry eye: A systematic review and meta-analysis. Acta Ophthalmol. 2021;99(5):489–498. doi:10.1111/aos.14651
10. Vickers A, Vertosick E, Lewith G, et al. Acupuncture for chronic pain: Update of an individual patient data meta-analysis. J Pain. 2018;19(5):455–474. doi:10.1016/j.jpain.2017.11.005
11. MacPherson H, Altman D, Hammerschlag R, et al. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): Extending the CONSORT statement. J Evidence-Based Med. 2010;3(3):140–155. doi:10.1111/j.1756-5391.2010.01086.x
12. WHO. Regional Office for the Western Pacific: WHO Standard Acupuncture Point Locations in the Western Pacific Region. Manila: World Health Organization; 2008.
13. Wei Q, Ding N, Wang J, Wang W, Gao W. Acupoint selection for the treatment of dry eye: A systematic review and meta-analysis of randomized controlled trials. Exp Ther Med. 2020;19(4):2851–2860. doi:10.3892/etm.2020.8561
14. Guo KLJ, Wang R. Clinical observation on the treatment of dry eye disease by penetration needling from Yingxiang point to bitong point and its effect on inflammatory factors. Jilin J Chinese Med. 2021;41(4):481–484. (in Chinese).
15. Liu J. Xie’s articular needling and four pain-relieving points. Chinese Acupunct Moxibustion. 2011;31(9):807–809. (in Chinese).
16. Shih M, Hootman J, Kruger J, Helmick C. Physical activity in men and women with arthritis national health interview survey, 2002. Am J Preventive Med. 2006;30(5):385–393. doi:10.1016/j.amepre.2005.12.005
17. Caraceni A, Cherny N, Fainsinger R, et al. Pain measurement tools and methods in clinical research in palliative care: Recommendations of an expert working group of the European association of palliative care. J Pain Sympt Manage. 2002;23(3):239–255. doi:10.1016/S0885-3924(01)00409-2
18. Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi:10.1016/S0304-3959(01)00349-9
19. Dworkin R, Turk D, Farrar J, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19. doi:10.1016/j.pain.2004.09.012
20. Lemp M. Report of the national eye institute/industry workshop on clinical trials in dry eyes. CLAO J. 1995;21(4):221–232.
21. Yang T, Ma B, Xie J, et al. Evaluation of ocular surface characteristics in dry eye disease with and without soft contact lens wear: A comparative study. Eye & Contact Lens. 2022;48(9):377–383. doi:10.1097/ICL.0000000000000904
22. Kim D, Park K-S, Lee J, et al. Intensive motion style acupuncture treatment (MSAT) is effective for patients with acute whiplash injury: A randomized controlled trial. J Clin Med. 2020;9:
23. Geber C, Baumgärtner U, Schwab R, et al. Revised definition of neuropathic pain and its grading system: An open case series illustrating its use in clinical practice. Am J Med. 2009;122:S3–12. doi:10.1016/j.amjmed.2009.04.005.
24. Moshirfar M, Benstead EE, Sorrentino PM, Tripathy K Ocular neuropathic pain. 2022
25. Qiao L, Guo M, Qian J, Xu B, Gu C, Yang Y. Research advances on acupuncture analgesia. Am J Chin Med. 2020;48(2):245–258. doi:10.1142/S0192415X20500135
26. Siedlecki A, Smith S, Siedlecki A, Hayek S, Sayegh R. Ocular pain response to treatment in dry eye patients. Ocular Surf. 2020;18(2):305–311. doi:10.1016/j.jtos.2019.12.004
27. Galor A, Batawi H, Felix E, et al. Incomplete response to artificial tears is associated with features of neuropathic ocular pain. Br J Ophthalmol. 2016;100(6):745–749. doi:10.1136/bjophthalmol-2015-307094
28. Crane AM, Levitt RC, Felix ER, Sarantopoulos KD, McClellan AL, Galor A. Patients with more severe symptoms of neuropathic ocular pain report more frequent and severe chronic overlapping pain conditions and psychiatric disease. Br J Ophthalmol. 2017;101(2):227. doi:10.1136/bjophthalmol-2015-308214
29. Scott EL, Kroenke K, Wu J, Yu Z. Beneficial effects of improvement in depression, pain catastrophizing, and anxiety on pain outcomes: A 12-month longitudinal analysis. J Pain. 2016;17(2):215–222. doi:10.1016/j.jpain.2015.10.011
30. Tu C-H, MacDonald I, Chen Y-H. The effects of acupuncture on glutamatergic neurotransmission in depression, anxiety, schizophrenia, and Alzheimer’s disease: A review of the literature. Front Psychiatry. 2019;10:14. doi:10.3389/fpsyt.2019.00014
31. Errington-Evans N. Acupuncture for anxiety. CNS Neurosci Ther. 2012;18(4):277–284. doi:10.1111/j.1755-5949.2011.00254.x
32. Pesavento F, Lovato A, Cappello S, Postiglione M. Acupuncture in the treatment of dry eye syndrome with anxiety symptoms. A case report. Eur J Trans Myol. 2022;32(2). doi:10.4081/ejtm.2022.10482
33. Zhang X-H, Feng -C-C, Pei L-J, et al. Electroacupuncture attenuates neuropathic pain and comorbid negative behavior: The involvement of the dopamine system in the amygdala. Front Neurosci. 2021;15:657507. doi:10.3389/fnins.2021.657507
34. Kim B, Kim M, Kang S, Nam H. Optimizing acupuncture treatment for dry eye syndrome: A systematic review. BMC Comple Alter Med. 2018;18(1):145. doi:10.1186/s12906-018-2202-0
35. Jones L, Downie L, Korb D, et al. TFOS DEWS II management and therapy report. Ocular Surf. 2017;15(3):575–628. doi:10.1016/j.jtos.2017.05.006
36. Jeon J, Shin M, Lee M, et al. Acupuncture reduces symptoms of dry eye syndrome: A preliminary observational study. J Alter Compl Med. 2010;16(12):1291–1294. doi:10.1089/acm.2009.0537
37. Nepp J, Tsubota K, Goto E, et al. The effect of acupuncture on the temperature of the ocular surface in conjunctivitis sicca measured by non-contact thermography: Preliminary results. Adv Exp Med Biol. 2002;506:723–726. doi:10.1007/978-1-4615-0717-8_102
38. Newberg A, Lariccia P, Lee B, Farrar J, Lee L, Alavi A. Cerebral blood flow effects of pain and acupuncture: A preliminary single-photon emission computed tomography imaging study. J Neuroimag. 2005;15(1):43–49. doi:10.1111/j.1552-6569.2005.tb00284.x
39. Kavoussi B, Ross B. The neuroimmune basis of anti-inflammatory acupuncture. Integr Cancer Ther. 2007;6(3):251–257. doi:10.1177/1534735407305892
40. You I, Li Y, Jin R, Ahn M, Choi W, Yoon K. Comparison of 0.1%, 0.18%, and 0.3% hyaluronic acid eye drops in the treatment of experimental dry eye. J Ocular Pharmacol Therapeutics. 2018;34(8):557–564. doi:10.1089/jop.2018.0032
41. Seong S, Kim JH, Kim N. Pro-inflammatory cytokines modulating osteoclast differentiation and function. J Rheumatic Dis. 2016;23(3):148–153. doi:10.4078/JRD.2016.23.3.148.
42. Yang Y, Zhang D, Wu L, et al. Electroacupuncture inhibits the corneal ROS/TXNIP/NLRP3 signaling pathway in a rat model of dry eye syndrome. Acupunct Med. 2022;40(1):78–88. doi:10.1177/09645284211039235
43. Binshtok A, Wang H, Zimmermann K, et al. Nociceptors are interleukin-1beta sensors. The J Neurosci. 2008;28(52):14062–14073. doi:10.1523/JNEUROSCI.3795-08.2008
44. Yerramothu P, Vijay AK, Willcox MDP. Inflammasomes, the eye and anti-inflammasome therapy. Eye. 2018;32(3):491–505. doi:10.1038/eye.2017.241
45. Arruda JL, Sweitzer S, Rutkowski MD, DeLeo JA. Intrathecal anti-IL-6 antibody and IgG attenuates peripheral nerve injury-induced mechanical allodynia in the rat: Possible immune modulation in neuropathic pain. Brain Res. 2000;879(1–2):216–225. doi:10.1016/S0006-8993(00)02807-9
46. Junger H, Sorkin LS. Nociceptive and inflammatory effects of subcutaneous TNFalpha. Pain. 2000;85(1–2):145–151. doi:10.1016/S0304-3959(99)00262-6
47. Shen H, Zheng X, Jin T, et al. Effect of electroacupuncture on ocular surface sensory neuralgia and expression of P2X3 receptor and PKC in cornea and trigeminal ganglion of dry eye Guinea pigs. Zhen Ci Yan Jiu. 2022;47(5):393–400. (in Chinese). doi:10.13702/j.1000-0607.20210607
48. Han S, Yang H, Hyon J, Wee W. Association of dry eye disease with psychiatric or neurological disorders in elderly patients. Clin Interventions Aging. 2017;12:785–792. doi:10.2147/CIA.S137580
49. Jacobs D. Diagnosis and treatment of ocular pain: The ophthalmologist’s perspective. Curr Ophthalmol Rep. 2017;5(4):271–275. doi:10.1007/s40135-017-0152-1
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



