Back to Journals » Clinical Ophthalmology » Volume 19
Efficacy and Safety of Cataract Surgery Combined with Ab Interno Canaloplasty and Micro-Trabecular Bypass Stent Surgery in Open-Angle Glaucoma
Authors Porter MS, Flowers A, Wood BP, Gallardo MJ
Received 13 November 2024
Accepted for publication 4 February 2025
Published 11 February 2025 Volume 2025:19 Pages 469—481
DOI https://doi.org/10.2147/OPTH.S504247
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Matthew S Porter,1 Addie Flowers,1 Brandon P Wood,1 Mark J Gallardo2
1Texas Tech University Health Sciences Center School of Medicine, Lubbock, TX, USA; 2El Paso Eye Surgeons, El Paso, TX, USA
Correspondence: Matthew S Porter, Department of Ophthalmology and Visual Sciences, Texas Tech University Health Sciences School of Medicine, 3601 4th St, Lubbock, TX, 79430, USA, Tel +1-806-742-2011, Email [email protected]
Purpose: To evaluate the effectiveness of canaloplasty via an ab-interno technique using the iTrack (Nova Eye Medical, Fremont, USA) combined with microtrabecular bypass stent surgery with the Hydrus microstent (Ivantis, Inc, Irvine, CA) following cataract surgery (CE) in patients with primary open-angle glaucoma (POAG).
Methods: A retrospective, two-center, case series of 51 POAG eyes that underwent phacoemulsification followed by canaloplasty combined with microtrabecular bypass stent surgery. Eyes were categorized according to IOP and disease severity. A subgroup of patients on 3+ medications at baseline was included. Primary end points included the mean IOP and mean number of medications at 12 months, 24 months and at the last follow-up.
Results: Baseline IOP (mmHg) and number of medications were 19.1± 4.0 and 2.3± 1.2 and reduced to 13.9± 2.6 (p< 0.001) and 1.2± 1.4 (p< 0.001) at 12 months, 13.7± 2.0 and 1.5± 1.5 (p< 0.001, p=0.008, respectively) at 24 months (n=31) and 14.4± 3.2 and 2.1± 1.5 (p< 0.001, p=0.5, respectively) at 36 months. In the uncontrolled group (n=27), baseline IOP and number of medications were 21.9± 3.1 and 1.9± 1.3 and reduced to 14.6± 4.2 (p=0.006) and 1.7± 1.6 (p=0.821) at 36 months postoperatively. Baseline IOP and number of medications of severe patients (n=12) were 19.0± 4.8 and 1.9± 1.1. IOP reduced to 12.8± 2.4 (p=0.005) at 12 months while the number of medications did not show any statistically significant change: 1.9± 1.6 (p=0.4). No eyes underwent additional glaucoma surgery in the study period.
Conclusion: Canaloplasty combined with microtrabecular bypass stent surgery following cataract extraction demonstrated efficacy in reducing IOP and medication burden up to 24 months postoperatively. IOP reduction was also sustained up to 36 months postoperatively. The combined MIGS procedure is also effective in eyes with uncontrolled glaucoma.
Keywords: intraocular pressure, glaucoma medications, canaloplasty, microtrabecular bypass stent, primary open-angle glaucoma
Introduction
Open-angle glaucoma (OAG), a progressive optic neuropathy affecting millions worldwide, is characterized by irreversible optic nerve damage often associated with elevated intraocular pressure (IOP).1 Lowering IOP remains the primary target of both medical and surgical treatments.2,3
Minimally invasive glaucoma surgeries (MIGS) encompass a range of implants, devices, and techniques designed to reduce IOP and minimize the risks and complications associated with traditional glaucoma surgeries. These procedures are typically less invasive with quicker recovery times and fewer side effects.4–6
Ab-interno canaloplasty is a comprehensive MIGS procedure that addresses all resistance sites along the conventional outflow system: trabecular meshwork (TM), Schlemm’s canal (SC), and collector channels (CC) using 360° catheterization of SC, and pressurized viscodilation with a high molecular weight ocular viscosurgical device (OVD).7–9
Microtrabecular bypass stents are MIGS that bypass the obstructed trabecular meshwork and for the case of Hydrus microstent (Alcon) can act as a scaffold in SC.10,11
Advanced glaucoma often requires a multifaceted approach in order to achieve adequate IOP reduction and halt disease progression. Traditional treatment with filtration surgery, despite its effectiveness, involves significant intra- and postoperative risks.12,13 Instead, combining various MIGS procedures for advanced cases targets multiple points in the aqueous outflow pathway simultaneously. Literature suggests that combining MIGS reduces IOP and medication burden more effectively than single MIGS procedures, which is valuable for advanced cases.14,15 Advantages include an improved safety profile, reduced complication rates with respect to traditional filtration surgery, and possibly greater efficacy compared to single MIGS procedures. Preserving the conjunctival tissue for future surgery is particularly beneficial in younger patients at high risk of failure with traditional surgeries. Reducing the medication burden is essential for patients with advanced disease, as multiple medications may be poorly tolerated, costly, or produce side effects.16–19
This study aims to retrospectively evaluate the effectiveness of 360-degree canaloplasty via an ab-interno approach using the iTrack microcatheter (Nova Eye Medical, Fremont, USA) combined with microtrabecular bypass stent surgery using the Hydrus microstent (Alcon) following cataract extraction in patients with varying severities of primary open-angle glaucoma (POAG).
Patients and Methods
Study Design
This study was a two-center, retrospective case series of eyes with open-angle glaucoma treated with ab interno canaloplasty combined with microtrabecular bypass stent surgery, following phacoemulsification, between December 2018 and November 2020. This study was conducted in accordance with the tenets of the Declaration of Helsinki and an ethics approval for retrospective review of canaloplasty data was obtained through TTUHSC El Paso Institutional Review Board. Written informed consent was obtained from all patients before participation.
Patients diagnosed with POAG, aged 18 years or older, were included in the study. Glaucoma diagnosis was made based on glaucomatous optic disc changes and retinal nerve fiber layer thinning on OCT. Disease severity (mild, moderate, or severe) was determined as defined by Hodapp et al’s criteria as recommended by European Glaucoma Society: mild (−6dB or better), moderate (−6dB to −12dB), or severe (−12dB or worse).20,21
Patients were excluded if they presented any signs of secondary glaucoma, angle-closure glaucoma, or other ocular comorbidity like uveitis. Patients with a history of previous incisional glaucoma surgery and patients who had undergone laser trabeculoplasty, or another MIGS procedure, within the 6 months prior to the procedure were also excluded.
Groups
In order to assess the effect of combined canaloplasty and microtrabecular bypass stent surgery to lower uncontrolled IOP, eyes were categorized into uncontrolled IOP (above 18mmHg) on maximal glaucoma medical therapy (Uncontrolled IOP group) and controlled IOP glaucoma patients (equal or less than 18mmHg, Controlled IOP group).
Eyes were also categorized by glaucoma severity: mild (−6dB or better), moderate (−6dB to −12dB), or severe (−12dB or worse).
A separate subgroup was created for eyes requiring three or more medications at baseline to evaluate the effectiveness of this approach in reducing the need for glaucoma medications.
Primary endpoints included mean intraocular pressure (IOP) and mean number of medications at 12 months, 24 months and at the last follow-up. In the uncontrolled IOP group, an additional endpoint was the percentage of eyes under IOP control at 12 months postoperatively as defined by an IOP equal or below 18mmHg; in the controlled IOP group, a further endpoint considered was medication reduction to keep IOP under control.
Preoperative and Postoperative Assessment
Prior to the surgery, patients received full ophthalmological examination including measurement of corrected distance visual acuity (CDVA), IOP measurement using Goldmann tonometry, slit-lamp examination, gonioscopy, fundus, and optic disc examination, as well as a visual field test.
Postoperatively, follow-up visits were scheduled at day 1, months 1, 3, 6, 12, 24 and 36. At each follow-up visit, IOP, medication, and corrected distance visual acuity data were recorded.
Study Devices
Canaloplasty was performed using an iTrack device (Nova Eye Medical, Fremont, USA). It features a microcatheter with an illuminated tip to visualize the device during the surgery, thus ensuring that it is in the correct position in Schlemm’s canal. The device can deliver more than 100μL of viscoelastic via a process of pressurized viscodilation and allows the surgeon to titrate the volume of viscoelastic. It enables catheterization of the entire 360° of Schlemm’s canal to be performed in one single intubation.7–9
The Hydrus microstent (Alcon, Geneva, Switzerland) is an aqueous drainage device made from nitinol (nickel–titanium alloy), roughly the size of an eyelash. It is a small, flexible, and biocompatible device delivered into the eye by a special hand-held injector with the tip of the injector cannula designed to incise the trabecular meshwork and create an entry into Schlemm’s canal.10,11
Surgical Technique
All surgeries were performed by two surgeons (MP, MG) and their residents and fellows under attending guidance. All patients underwent canaloplasty through an ab-interno approach combined with microtrabecular bypass stent surgery following phacoemulsification.
The iTrack microcatheter was primed with high molecular weight OVD (Healon GV or Healon Pro, Johnson & Johnson) prior to the surgery. Standard phacoemulsification was performed first in all patients, a 27-gauge needle paracentesis was then created either superiorly or inferiorly, depending on patient access, and directed nasally. The tip of the microcatheter was then inserted into the anterior chamber and directed toward the nasal angle. Using a gonioprism, a 1- to 2-mm microgoniotomy was created in the nasal angle with a 25-gauge needle. Inside the anterior chamber, the distal end of the microcatheter was grasped with microforceps and directed into Schlemm’s canal via the goniotomy site. The iTrack microcatheter was advanced through the full 360° circumference of SC. The microcatheter was then retracted at a rate of 1 clock hour per 1.5 seconds, while simultaneously injecting 2 “clicks” of Healon GV per clock hour or 3 clicks of Healon Pro.
After performing canaloplasty, the patient’s head was tilted nasally to ensure a clear view of the angle, the AC was refilled with OVD, and the microstent injector was introduced into the AC through the clear corneal incision. A small incision was made in the trabecular meshwork using the injector cannula, and the microstent was injected into SC over a 90-degree span. The delivery system was withdrawn after ensuring proper positioning of the device inside the canal.
Thereafter, the AC was irrigated using an Alcon Centurion I/A handpiece (Alcon Laboratories) to remove any residual OVD, the corneal wounds were then hydrated, and the anterior chamber was pressurized to approximately 20 mmHg using a balanced-salt solution as measured intraoperatively using a Barraquer tonometer.
Postoperative Medications
Postoperatively, topical prednisolone acetate 1% for 4 times daily was prescribed for the first week and twice daily for the following 3 weeks; topical non-steroidal anti-inflammatory drugs (NSAIDs) and topical antibiotics were also administered during the first postoperative week.
Glaucoma medications were stopped on day 1 postoperatively and were reinstated if IOP rose above the target; this was dependent on various factors, most notably the stage of glaucoma.
Outcome Measures
Primary endpoints included IOP and number of glaucoma medications. Secondary endpoints included control of IOP at 18 or 15 mmHg or less, number of medication-free eyes at 12 months, and corrected distance visual acuity (CDVA). Any adverse events were also recorded.
Statistical Analysis
The comparisons between changes in IOP and number of medications at different timepoints were analyzed using Wilcoxon signed-rank test (SPSS Statistics for Windows, NY: IBM Corp). The overall comparison between changes in mean IOP and mean number of medications between groups was analyzed with non-parametric tests. Graphs were designed according to the Guidelines on Design & Reporting Glaucoma Trials.22 A p-value of <0.05 was considered statistically significant.
Results
Demographics
Demographics are summarized in Table 1. Of the 51 eyes, 14 (27.5%) eyes had mild glaucoma, 25 (49.0%) eyes had moderate glaucoma, and 12 (23.5%) eyes had severe glaucoma. The number of patients with an IOP ≤18mmHg (controlled group) were 24 (47.1%), while patients with an IOP >18mmHg (uncontrolled group) were 27 (52.9%).
 |
Table 1 Demographics |
Primary Outcomes
Intraocular Pressure (IOP)
Mean intraocular pressure at baseline and postop day 1 as well as 1, 3, 6, 12, 24 and 36 months postoperatively are shown in Figure 1A. The mean baseline IOP of 19.1±4.0 mmHg reduced significantly to 13.9±2.6 (n=50, p<0.001) at 12 months. Of the 51 eyes, 19 eyes had reached 36 months of follow-up, for which IOP significantly dropped to 14.4±3.2 (p<0.001) at 36 months (Table 2).
The scatterplot presented in Figure 1B represents IOP preoperatively and postoperatively (data imputed using the last observation carried forward or LOCF method, mean follow-up 27.1±13.5 months). The red line indicates at least 20% IOP reduction from baseline.
Table 3 reports the percentage of eyes with IOP less than or equal to 15 and to 18 mmHg at baseline, and postoperatively at 12, 24, and 36 months, medication-free or not, and the percentage of eyes with 20% IOP reduction versus baseline.
 |
Table 3 Success of Eyes (n, %) at Each Timepoint (Baseline, 12M, 24M, 36M) |
Glaucoma Medications
The number of glaucoma medications at baseline and postoperatively (LOCF data; mean follow-up 26.1±13.3 months) is presented in Figure 2. Mean baseline medications were reduced significantly from 2.25±1.2 to 1.2±1.4 (n=48, p<0.001) at 12 months and 1.5±1.5 (n=30, p=0.008) at 24 months but the reduction was not significant at 36 months 2.1±1.5 (n=20). The percentage of medication-free eyes was higher at all follow-up visits as compared to the baseline (Table 3). At 12 months, 52.9% of eyes in the uncontrolled group were medication-free, compared to 30% of the controlled group. Additionally, 56.8% of eyes with mild to moderate glaucoma were medication-free; however, no eyes in the severe group achieved this status. Furthermore, 50% of eyes that were on 3 or more medications preoperatively attained medication-free status.
 |
Figure 2 Bar diagram representing number of medications at preop and postop, with mean follow-up 26.1±13.3 months (n=51) (imputed using the LOCF method). |
Analysis of Uncontrolled/Controlled IOP and Multiple Medications at Baseline
In the uncontrolled IOP group (>18 mmHg at baseline; n=27), mean IOP and number of medications at baseline were 21.9±3.1 and 1.9±1.3 IOP was reduced significantly at all subsequent follow-ups, while the reduction in medications was significant only until the 12-month follow-up (Table 2). Figure 1C shows the scatterplot of those uncontrolled IOP eyes at the LOCF timepoint (25.3±14.3 months).
In the IOP controlled group (≤18 mmHg at baseline, n=24), mean IOP and number of medications at baseline were 15.9±2.1 and 2.7±0.9. In those eyes, the reduction in the number of medications was significant up to 24 months but not for the 10 eyes that reached the 36-month follow-up (Table 2).
Figure 3 reports the Kaplan–Meier analysis of all eyes (n=51), showing eyes that had an IOP of 18mmHg or higher at any timepoint following baseline (3, 6, 12, 24 and 36 months).
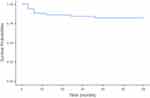 |
Figure 3 Kaplan-Meier analysis of eyes (n=51) reaching an IOP of 18 mmHg or higher in the succeeding timepoints (3, 6, 12, 24 and 36 months). |
Twenty-three eyes were receiving 3+ medications: for those eyes, baseline IOP and number of medications were 18.7±4.2 and 3.3±0.5 and reduced at 36 months to 13.8±2.0 (−26%, n=10) but the change was not statistically significant (p=0.1), while the reduction in medications to 2.2±1.2 (−33%; n=10; p=0.02) was significant (Table 2). Half of the eyes that reached 12 months data were medication-free. Five eyes still required the use of 3 or more medications and 1 of those eyes increased the number of medications from 3 to 4.
Analysis by Glaucoma Severity
Outcomes by preoperative IOP and glaucoma severity were also analyzed and are presented in Table 2.
Mean baseline IOP for the mild eyes (n=14) was 19.9±2.7 mmHg, which showed a significant reduction to 14±1.4 mmHg at 36 months follow-up (−30% reduction, n=8, p=0.02), while the IOP reduction was not significant in the moderate and severe groups at 36 months.
Baseline medications were 3.0±0.8 in the moderate group (n=25) and this showed a significant reduction in at 36 months to 2.2±1.2 (−27%; n=10; p=0.04) while the change was not significant in the mild and severe groups. Six severe eyes (50%) had an IOP above 18mmHg preoperatively, while all severe eyes (100%) were below 18mmHg postoperatively.
Three (3/14, 21.4%) of mild glaucoma eyes had ≤18mmHg IOP at baseline compared to 85.7% (12/14) at 12 months; 16.0% (4/25) of moderate eyes had ≤15mmHg at baseline compared to 70.8% (17/24) postoperatively; and 8.3% (1/12) of severe eyes had a preoperative IOP of ≤12mmHg vs 58.3% (7/12) at 12 months.
Visual Acuity Outcomes
Baseline and postoperative corrected distance visual acuity (CDVA) were compared, and logMAR VA was significantly improved from 0.51±0.43 at baseline to 0.27±0.49 at 36 months (p=0.008).
Safety Outcomes
There were no serious complications recorded. Postoperative hyphema and corneal edema were observed in some patients, but they were transient and resolved spontaneously.
Discussion
MIGS procedures with different mechanisms of action have been shown to significantly reduce IOP and medication burden. Several studies have reported the efficacy and safety of using canaloplasty via an ab-interno approach, and microtrabecular bypass stents standalone procedure or combined with cataract surgery.18,23–26
The effectiveness of canaloplasty was described by Gallardo et al in a consecutive case series which demonstrated the efficacy and safety of the procedure performed with iTrack over a 12-month period.9 Another study by Koerber et al published a narrative review with consolidated data using the iTrack on 365 eyes and found that IOP decreased from 20.0±2.5 mmHg preoperatively to 13.8±0.6 and to 14.0±0.9 at 12 and 24 months while the number of medications was reduced from 2.5±0.5 preoperatively to 0.8±0.4 and 0.9±0.6 at 12 and 24 months postoperatively—comparable results were observed if canaloplasty was performed as a standalone procedure or combined with cataract surgery.25
The HORIZON study, which is the largest prospective, randomized, controlled MIGS pivotal trial to date concluded that combining Hydrus microstent implantation with phacoemulsification significantly reduces IOP and medication use and that these reductions occur in a higher proportion of eyes in which the Hydrus was implanted in combination with cataract surgery than in those eyes in which only cataract surgery was performed. Furthermore, the implantation of the stent improved the likelihood of remaining medication-free at the 5-year follow-up.27 In comparison to the current study, the Horizon study—which included eyes with mild to moderate glaucoma—reported the following outcomes at 24 months: a 6.1% reduction in IOP (compared to a 26.6% IOP reduction in eyes with mild to moderate glaucoma of the current cohort), an 82.4% reduction in medication use (compared to 41.9% medication reduction in eyes with mild to moderate glaucoma of the current cohort), and 78% of patients being medication-free (compared to 44.4% in the current study).
Results from the literature, such as those from the Horizon study or Koerber et al narrative review show comparable reductions in IOP and medication use, or a balance of those. However, our cohort included cases with more severe glaucoma compared to the mild-to-moderate cases typically found in traditional canaloplasty or stent cohorts. This difference in baseline severity is important, as it suggests that the combined procedure may offer benefits even in more challenging cases. Furthermore, because the exact site of resistance in the outflow pathway can vary between patients, combining different MIGS procedures allows multiple points of blockage to be addressed simultaneously.
Combining MIGS procedures works by addressing various aspects of aqueous outflow simultaneously and, in some reports, it has been suggested to have a synergistic effect with respect to single MIGS procedures and can be of particular value in patients with more advanced disease.15,28 In 2017, Ferguson et al proposed the term ICE while examining the efficacy of phaco/iStent versus phaco/endocyclophotocoagulation (ECP)/iStent (ICE-1). Both groups were similar in terms of preoperative intraocular pressure (IOP) and medication count. One year after surgery, the ICE-1 technique demonstrated a more significant reduction in IOP; despite this, the phaco/iStent group showed a lower requirement for topical medications than the ICE-1 group, averaging 0.6 compared to 1.1 (p<0.01). However, a crucial distinction between the groups was the baseline severity of glaucoma; 51% of patients in the ICE-1 group had severe glaucoma, in contrast to only 10% in the phaco/iStent group: this difference likely accounts for the increased postoperative medication need observed in the ICE-1 group.19 Pantalon et al conducted the first investigation of the ICE-2 procedure, involving the insertion of two iStent inject devices and ECP during cataract surgery. In this retrospective study, they found that the ICE-2 procedure led to greater absolute IOP reduction after 12 months compared to phaco/iStent inject (6.9 vs 3.5 mmHg; p=0.03). Additionally, they noted a decrease in the number of glaucoma medications, with a higher likelihood of being medication-free at 12 months in the ICE-2 group despite similar baseline medication numbers.29
In another retrospective case series by Heersink et al, 86 eyes underwent cataract extraction + TM-bypass (iStent device) + catheterization of Schlemm’s canal using VISCO360 (CE + TM-bypass + CP group) device while 100 eyes underwent only cataract surgery + TM-bypass (CE + TM-bypass group). At 6 months they observed a greater mean IOP reduction in the CE + TM-bypass + CP group (2.9±3.6 mmHg) compared to the CE + TM-bypass group (1.7±3.1 mmHg), along with a higher proportion achieving ≥20% IOP reduction with IOP <18 mmHg on the same or fewer medications (46% vs 35%, respectively). Both groups experienced a decrease in mean number of medications (0.9 vs 0.7), with a notable percentage of all medications (56% vs 48%).28
In this retrospective study, we report the efficacy of combining canaloplasty and microtrabecular bypass stent surgery with concomitant phacoemulsification in patients with POAG. Both procedures performed simultaneously in conjunction with cataract surgery were found to be safe and effective in patients with mild, moderate, and severe glaucoma.
Our analysis of 51 eyes with OAG showed a significant and sustained reduction in terms of IOP, from 19.1±4.0 at baseline to 13.9±2.6 at 12 months (−26.9% reduction), 13.7±2.0 at 24 months (n=31, −39.2% reduction) and 14.4±3.2 at 36 months (n=19, −24.3% reduction).
They were also effective in reducing glaucoma medication burden, with 48% of eyes being medication-free at 12 months compared to only 7.8% at baseline.
Since patients with advanced disease typically receive several glaucoma medications, this can impact a patient’s quality of life. Multiple medications require high degree of patient adherence to be effective and can harm the ocular surface by the preservatives included, so reducing dependence on medications could be an advantage achieved using combining MIGS.30
Overall, we observed 27 eyes of uncontrolled preoperative IOP (>18mmHg) where IOP reduced significantly, from 21.9±3.1 at baseline to 14.6±4.2 at 36 months (p=0.006). Additionally, the Kaplan–Meier analysis (Figure 3) shows that the procedure was able to maintain IOP below 18 mmHg in the majority of eyes.
MIGS procedures were originally described for mild-moderate open-angle glaucoma with limited evidence into the effectiveness of different MIGS, whether single or combined, in cases with uncontrolled IOP, as well as in cases with severe glaucoma.9,14,31–33 In our study, 12 patients had severe glaucoma: those 12 eyes reported a significant IOP reduction of −32.5% at 12 months, while the number of medications remained stable. The results observed may encourage surgeons to use combined MIGS procedures in patients with more advanced disease given the synergistic effect generated when the procedures and devices are performed and utilized simultaneously.
Canaloplasty and Hydrus implantation reduce IOP by targeting different sites of outflow resistance. The process of microcatheterization during canaloplasty mechanically breaks adhesions within Schlemm’s canal, in addition to pushing the herniations of the trabecular meshwork and the inner wall of the canal out of the collector channels, thus enhancing the physiological drainage of aqueous. The pressurized injection of high molecular weight OVD into Schlemm’s canal (viscodilation) dilates the canal by 2–3 times and creates microperforations within the trabecular meshwork, which further enhances aqueous flow.34 On the other hand, Hydrus microstent creates an artificial drainage pathway, bypassing the trabecular meshwork and facilitating the flow of aqueous humor directly from the anterior chamber into SC. It also spans 3 clock-hours of SC, functioning as a mechanical scaffold within SC.35
By utilizing both MIGS procedures in combination, it can be conceptualized that canaloplasty primarily opens up Schlemm’s canal, as well as collector channels, and breaks down any blockages inside the canal, preparing it and rendering it more functional for the placement of the Hydrus microstent, thus promoting its action. Similarly, inserting the Hydrus microstent inside the canal following canaloplasty could ensure long-term results by keeping the canal open for a longer duration. Accordingly, we propose that targeting different levels of outflow resistance via the combination of canaloplasty and Hydrus implantation would achieve a better response.
The procedure showed a good safety profile, with hyphema and corneal edema being the most observed complications in our patients, and both resolved spontaneously. Corneal edema was most likely related to phacoemulsification given that it is a common event reported with phacoemulsification cataract surgery and usually resolves on its own.36 There was no VA loss noted in any of our patients and, in contrast, there was an average gain of 2 lines of CDVA, supposedly related to cataract removal. These findings emphasize that combining canaloplasty and microtrabecular bypass stent surgery is still within the single MIGS safety profile.
The limitations of this study include the modest sample size, the retrospective design, lack of randomization, and lack of comparison with a control group. Future research should explore the integration of multiple MIGS within a single surgery and their role in addressing various underlying causes of elevated IOP. This should include assessing the cost-effectiveness of combining MIGS procedures and identifying the most suitable candidates for such approaches.
Conclusion
This 24-month data demonstrated that canaloplasty performed through an ab-interno approach combined with microtrabecular bypass stent surgery following phacoemulsification results in a significant reduction in mean IOP as compared to baseline, along with a significant decrease in the mean number of glaucoma medications in POAG. Preoperatively uncontrolled cases showed significant reduction in IOP up to 36 months and significant reduction in medications up to 12 months. Severe POAG showed significant IOP reduction up to 12 months. Our results showed that the combined MIGS procedure is safe and effective in patients with POAG up to two years.
Acknowledgments
Medical writing assistance was provided by GP Communications and funded by Nova Eye Medical.
Disclosure
The authors have no financial or proprietary interest in any material or method mentioned. Dr. Gallardo is a consultant to Nova Eye Medical. Dr Matthew Porter reports personal fees from Glaukos, outside the submitted work.
References
1. Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global Prevalence of Glaucoma and Projections of Glaucoma Burden through 2040. Ophthalmology. 2014;121(11):2081–2090. doi:10.1016/j.ophtha.2014.05.013
2. Nemesure B, Honkanen R, Hennis A, Wu SY, Leske MC. Incident Open-angle Glaucoma and Intraocular Pressure. Ophthalmology. 2007;114(10):1810–1815. doi:10.1016/j.ophtha.2007.04.003
3. Yang Y, Zhang X, Chen Z, et al. Intraocular pressure and diurnal fluctuation of open-angle glaucoma and ocular hypertension: a baseline report from the LiGHT China trial cohort. Br J Ophthalmol. 2023;107(6):823–827. doi:10.1136/BJOPHTHALMOL-2021-320128
4. Gillmann K, Mansouri K. Minimally Invasive Glaucoma Surgery: where Is the Evidence? Asia-Pac J Ophthalmol. 2020;9(3):203–214. doi:10.1097/APO.0000000000000294
5. Lavia C, Dallorto L, Maule M, Ceccarelli M, Fea AM. Minimally-invasive glaucoma surgeries (MIGS) for open angle glaucoma: a systematic review and meta-analysis. PLoS One. 2017;12(8):e0183142. doi:10.1371/JOURNAL.PONE.0183142
6. Coleman AL, Richter G. Minimally invasive glaucoma surgery: current status and future prospects. Clin Ophthalmol. 2016;189. doi:10.2147/OPTH.S80490
7. B H, S GB. Canaloplasty in the spotlight: surgical alternatives and future perspectives. Rom J Ophthalmol. 2022;66(3):1. doi:10.22336/RJO.2022.44
8. Koerber N. Ab interno canaloplasty for the treatment of glaucoma: a case series study. Spektrum der Augenheilkunde. 2018;32(6):223–227. doi:10.1007/s00717-018-0416-7
9. Gallardo MJ. 36-Month Effectiveness of Ab-Interno Canaloplasty Standalone versus Combined with Cataract Surgery for the Treatment of Open-Angle Glaucoma. Ophthalmol Glaucoma. 2022;5(5):476–482. doi:10.1016/J.OGLA.2022.02.007
10. Manasses DT, Au L. The New Era of Glaucoma Micro-stent Surgery. Ophthalmol Ther. 2016;5(2):135–146. doi:10.1007/S40123-016-0054-6/FIGURES/6
11. Rai A, Ahmed II K. Glaucoma Surgery: Treatment and Techniques - Google Books. Springer International Publishing. 2017
12. Edmunds B, Thompson JR, Salmon JF, Wormald RP. The National Survey of Trabeculectomy. III. Early and late complications. Eye. 2002;16(3):297–303. doi:10.1038/sj.eye.6700148
13. Jampel HD, Solus JF, Tracey PA, et al. Outcomes and Bleb-Related Complications of Trabeculectomy. Ophthalmology. 2012;119(4):712–722. doi:10.1016/j.ophtha.2011.09.049
14. Yang SA, Mitchell W, Hall N, et al. Trends and Usage Patterns of Minimally Invasive Glaucoma Surgery in the United States: IRIS® Registry Analysis 2013–2018. Ophthalmol Glaucoma. 2021;4(6):558–568. doi:10.1016/J.OGLA.2021.03.012
15. Mai DD, Ingram Z, Oberfeld B, Solá-Del Valle D. Combined Microinvasive Glaucoma Surgery - A Review of the Literature and Future Directions. Semin Ophthalmol. 2023;38(6):529–536. doi:10.1080/08820538.2023.2181665
16. Bar-David L, Blumenthal EZ. Evolution of Glaucoma Surgery in the Last 25 Years. Rambam Maimonides Med J. 2018;9(3):e0024. doi:10.5041/RMMJ.10345
17. Kastner A, King AJ. Advanced glaucoma at diagnosis: current perspectives. Eye. 2020;34(1):116–128. doi:10.1038/s41433-019-0637-2
18. Khaimi MA. Long-term medication reduction in controlled glaucoma with iTrack ab-interno canaloplasty as a standalone procedure and combined with cataract surgery. Ther Adv Ophthalmol. 2021;13:251584142110457. doi:10.1177/25158414211045751
19. Ferguson TJ, Swan R, Sudhagoni R, Berdahl JP. Microbypass stent implantation with cataract extraction and endocyclophotocoagulation versus microbypass stent with cataract extraction for glaucoma. J Cataract Refract Surg. 2017;43(3):377–382. doi:10.1016/j.jcrs.2016.12.020
20. Hodapp E, Parrish IR, Anderson D. Clinical Decisions in Glaucoma. St Louis Mo, USA: CV Mosby Co. 2016
21. European Glaucoma Society Terminology and Guidelines for Glaucoma. Classification and terminologySupported by the EGS Foundation: part 1: foreword; Introduction; Glossary; Chapter 2 Classification and Terminology. Br J Ophthalmol. 2017;101(5):73–127. doi:10.1136/BJOPHTHALMOL-2016-EGSGUIDELINE.002.
22. Shaarawy TM, Sherwood MB, Grehn F. Guidelines on Design and Reporting of Surgical Trials. World Glaucoma Association.; 2009.
23. Koerber N, Ondrejka S. Four-Year Efficacy and Safety of iTrack Ab-interno Canaloplasty as a Standalone Procedure and Combined with Cataract Surgery in Open-Angle Glaucoma. Klin Monbl Augenheilkd. 2022;240(12):1394–1404. doi:10.1055/A-1737-4149/ID/R2539-7/BIB
24. Otarola F, Virgili G, Shah A, Hu K, Bunce C, Gazzard G. Ab interno trabecular bypass surgery with Schlemm´s canal microstent (Hydrus) for open angle glaucoma. Cochrane Database Syst Rev. 2020;2020(3). doi:10.1002/14651858.CD012740.PUB2/ABSTRACT
25. Koerber N, Ondrejka S. Clinical outcomes of canaloplasty via an ab-interno surgical technique using the iTrack device: a narrative review. Int Ophthalmol. 2023;43(6):2017–2027. doi:10.1007/S10792-022-02601-1
26. Samuelson TW, Katz LJ, Wells JM, Duh YJ, Giamporcaro JE. Randomized Evaluation of the Trabecular Micro-Bypass Stent with Phacoemulsification in Patients with Glaucoma and Cataract. Ophthalmology. 2011;118(3):459–467. doi:10.1016/j.ophtha.2010.07.007
27. Ahmed IIK, De Francesco T, Rhee D, et al. Long-term Outcomes from the HORIZON Randomized Trial for a Schlemm’s Canal Microstent in Combination Cataract and Glaucoma Surgery. Ophthalmology. 2022;129(7):742–751. doi:10.1016/j.ophtha.2022.02.021
28. Heersink M, Dovich JA. Ab interno canaloplasty combined with trabecular bypass stenting in eyes with primary open-angle glaucoma. Clin Ophthalmol. 2019;13:1533–1542. doi:10.2147/OPTH.S215667
29. Pantalon AD, Barata ADDO, Georgopoulos M, Ratnarajan G. Outcomes of phacoemulsification combined with two iStent inject trabecular microbypass stents with or without endocyclophotocoagulation. Br J Ophthalmol. 2020;104(10):1378–1383. doi:10.1136/bjophthalmol-2019-315434
30. Robin AL, Muir KW. Medication adherence in patients with ocular hypertension or glaucoma. Expert Rev Ophthalmol. 2019;14(4–5):199–210. doi:10.1080/17469899.2019.1635456
31. Patel S, Reiss G. Long-Term Clinical and Safety Outcomes of Canaloplasty Performed across All Grades of Glaucoma Severity. J Ophthalmol. 2023;2023:5625990. doi:10.1155/2023/5625990.
32. García-Feijoo J, Rau M, Grisanti S, et al. Supraciliary Micro-stent Implantation for Open-Angle Glaucoma Failing Topical Therapy: 1-Year Results of a Multicenter Study. Am J Ophthalmol. 2015;159(6):1075–1081.e1. doi:10.1016/J.AJO.2015.02.018
33. Buttram JOMCKKW. Outcome of combined photocoagulation with trabecular microbypass minimally invasive glaucoma surgeries in the treatment of advanced open angle glaucoma. Abstract. In:
34. Khaimi MA. Canaloplasty: a Minimally Invasive and Maximally Effective Glaucoma Treatment. J Ophthalmol. 2015;2015. doi:10.1155/2015/485065.
35. Samet S, Ong JA, Ahmed IIK. Hydrus microstent implantation for surgical management of glaucoma: a review of design, efficacy and safety. Eye Vis (Lond). 2019;6(1). doi:10.1186/S40662-019-0157-Y
36. Milec LL, Sekelj M, Konjevic-Pernar S. Postoperative Corneal Edema After Phacoemulsification. Eur Med J. 2022;6(1):113–120.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



