Back to Journals » Clinical Ophthalmology » Volume 18
Evaluating the Efficacy of Conbercept and Dexamethasone Implants Sequentially in the Treatment of Refractory Macular Edema Secondary to Central Retinal Vein Occlusion (CRVO): A One-Year Follow-Up Study
Authors Xing P, Zhang Y, Zhang Y, Wang S, Hu X, Wang M, Xia F, Zhao Y, Qu W, Meng B
Received 16 July 2024
Accepted for publication 24 September 2024
Published 30 September 2024 Volume 2024:18 Pages 2721—2730
DOI https://doi.org/10.2147/OPTH.S487248
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Peiyu Xing,1,* Yucheng Zhang,2,* Yong Zhang,1 Shaowei Wang,2 Xiaojia Hu,1 Meihua Wang,1 Fan Xia,1 Yang Zhao,1 Wei Qu,2 Bo Meng2
1Department of Ophthalmology, China Medical University the Fourth People’s Hospital of Shenyang, Shenyang, People’s Republic of China; 2Department of Ophthalmology, The 2nd Affiliated Hospital of Harbin Medical University, Harbin, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Bo Meng, Department of Ophthalmology, The 2nd Affiliated Hospital of Harbin Medical University, Harbin, People’s Republic of China, Email [email protected]
Purpose: The objective of this research was to assess the effectiveness and safety of using Conbercept injection and dexamethasone implant (DEX I) in sequence for treating refractory macular edema (ME) caused by central retinal vein occlusion (CRVO) in patients.
Methods: A study was conducted on 34 patients with persistent macular edema caused by central retinal vein occlusion, reviewing their medical history and interventions performed. Sequential implantation of DEX I was performed 1 week after the Conbercept injection. OCTA images were used to measure central retinal thickness (CRT), best-corrected visual acuity (BCVA), intraocular pressure (IOP), and pre- and post-treatment vessel density of the superficial capillary plexus (SCP) and deep capillary plexus (DCP), with a 1-year follow-up period.
Results: At the 12-month follow-up, participants demonstrated notable improvements in central retinal thickness and intraocular pressure (p < 0.05). Throughout the monitoring period, no significant differences were found in BCVA improvement or vessel density reduction (p > 0.05). Two patients required topical treatment to lower their intraocular pressure during the study period.
Conclusion: In conclusion, patients experiencing persistent ME due to secondary CRVO may benefit from transitioning to a treatment regimen involving Conbercept and DEX I, potentially resulting in a reduction in CRT. However, no significant improvement was observed in BCVA or deep and superficial capillary plexus vessel density.
Keywords: macular edema, sequential, central retinal thickness, best corrected visual acuity
Introduction
Macular edema (ME) is the predominant cause of vision impairment in patients with central retinal vein occlusion (CRVO).1 The primary reason for CRVO patients’ visual impairment, the exact cause of ME remains unclear, a variety of factors contribute to the breakdown of the inner blood-retinal barrier, including vascular hyperpermeability, and heightened local inflammatory reaction.2 VEGF inhibitors, among ranibizumab, aflibercept, and Conbercept, have been proven effective in improving both visual function and macular structure over an extended period of time.3–5 Long-acting corticosteroid medications (DEX I; Ozurdex; Allergan Inc., Irvine, CA, USA, and Allergan Pharmaceuticals, Dublin, Ireland) can moreover serve as a viable option, whether as an initial or subsequent treatment, for macular edema in CRVO.6
However, patient responses to therapy vary widely, often due to the intensive treatment schedules required by clinical trials, which can affect compliance. Treatment does not seem to work well for a significant percentage of patients, according to studies, both anatomically and functionally, despite rigorous efforts.7 Studies have also shown that patients with CRVO who do not initially respond to anti-VEGF or steroid treatments represent a distinct subgroup. Additionally, some patients who experience early functional and anatomical improvements may later become refractory to these treatments.8 Approximately 28.6% of the eyes improved by more than 15 letters after receiving an anti-VEGF injection for 12 months according to an actual study. Additionally, 59.5% of the eyes maintained a stable visual acuity (less than 15 letters gained or lost), while 11.9% of the eyes saw a decrease of more than 15 letters over the course of the study.9 Conversely, DEX I demonstrates a decrease in efficacy after an average of 4 months post-injection, requiring more frequent reinjections than recommended in the European guidelines.10
Patients suffering from ME who do not have a positive reaction to anti-VEGF or DEX I by itself may consider combining anti-VEGF with steroids as a possible alternative treatment choice. To our knowledge, this is the first study to apply Conbercept and DEX I to the sequential treatment of patients with refractory CRVO-ME to evaluate patient vision and anatomic outcomes as well as safety. Previous treatment with anti-VEGF or DEX I as monotherapy was ineffective in these patients.
ME secondary to RVO is complex and involves multiple factors.11 A rise in intraluminal venous pressure prior to occlusion increases hydrostatic pressure as per Starling’s law, resulting in plasma. The heightened pressure within the extracellular space leads to increased fluid retention, exacerbating interstitial edema. Chronic ischemic damage occurs when retinal capillaries do not receive adequate blood supply. In the hypoxic retina, there is an increase in the production of VEGF as well as substances that cause inflammation that lead to the breakdown of the barrier between the retina and blood vessels.12 Macular thickening can occur despite the presence of collateral vessels because VEGF induces self-sustaining vascular hyperpermeability.
Prospective randomized controlled trials (RCTs) and real-world studies have confirmed the effectiveness of both anti-VEGF drugs and steroids, showing notable enhancements in visual acuity and macular structure. The safety and effectiveness of one or two intravitreal DEX I injections over a 12-month period were evaluated in the GENEVA trial for eyes with macular edema caused by either BRVO or CRVO and had not received previous treatment.13 Simultaneously, research papers are assessing the effectiveness and safety of Conbercept when used in conjunction with RVO for treating ME.5,14
The aim of this study is to evaluate the effectiveness and safety of sequential treatment with Conbercept and DEX I in patients with refractory ME secondary to CRVO, particularly those who did not respond adequately to prior anti-VEGF or steroid monotherapy, by assessing both visual and anatomical outcomes.
Material and Methods
Between February 2021 and February 2022, the Department of Ophthalmology at the 2nd Affiliated Hospital of Harbin Medical University received 34 patients with treatment-resistant ME caused by CRVO. A written informed consent form was signed by each patient, and the study protocol was followed the Helsinki Declaration on Human Subjects and was approved by the review board of the 2nd Affiliated Hospital of Harbin Medical University.
Patients over the age of 18 with confirmed CRVO on angiography, refractory ME due to CRVO, who had received a minimum of five ranibizumab injections and at least one DEX I as monotherapy in the study eye before enrollment, met the inclusion criteria. At one month post-ranibizumab (4th) injection and four months post-DEX I administration, optical coherence tomography (OCT) showed intraretinal or subretinal fluid in patients with refractory macular edema.
Uncontrolled glaucoma, characterized by ongoing visual field deterioration despite optimal IOP management, was among the exclusion criteria. Exclusion criteria included patients who had undergone vitrectomy or intraocular surgery within 6 months before experiencing retinal vein occlusion (RVO), with significant lens opacity that prevented high-quality fundus examination and OCT imaging, or someone who had recently experienced a cardiovascular event prior to receiving anti-VEGF medication, and patients with other retinal diseases that contributed to the formation of macular edema. Previous macular grid laser treatments were not considered as exclusion criteria.
At the time of RVO diagnosis, every patient received a thorough eye examination that included assessment of best-corrected visual acuity (BCVA), which was measured using the Snellen chart and subsequently converted to logarithm of the minimum angle of resolution (LogMAR) for statistical analysis, slit lamp biomicroscopy, Goldmann applanation Tonometry, and fundus examination. CRT was assessed using spectral domain optical coherence tomography (SD-OCT, OptovueRTVue XR, Optovue, Inc., Fremont, CA), while vascular retinal markers were evaluated with OCT angiography (OCTA, ReVue, Optovue, Inc., Fremont, CA).
The participants were followed up for a duration of 12 months. Demographic information, BCVA transformed into LogMAR, IOP, CRT, and VD of both the superficial and deep capillary plexus were examined and gathered.
AngioVue (Optovue RTVue XR Avanti; Optovue Inc, Fremont, CA) was utilized to obtain OCTA images. An 840 nm diode laser source was utilized by the system, operating at a rate of 70 kHz/s for A-scans. Both eyes in the study group and the control group were scanned using a 3.3 mm center focused on the center of the macula. Orthogonal registration algorithms were utilized to generate three-dimensional OCTA images. Following that, the AngioVue program (version A2017,1,0,151) autonomously divided the vascular region into four sections (SCP, DCP, outer retina, and choroid).SCP segmentation automatically includes vessels from the internal limiting membrane up to 10 mm above the inner plexus, while DCP segmentation includes vessels from 10 mm above the inner plexus down to 10 mm below the outer plexus. This version of AngioVue software incorporated projection artifact removal algorithms. Analysis was performed on OCTA images obtained when macular edema subsided. In cases where multiple OCTA images were available for a patient, only those of highest quality were selected for analysis purposes. Any segmentation errors encountered were manually rectified in each individual. Vascular density in a specific area is determined by the proportion of space taken up by both large and small blood vessels. AngioVue software automatically calculates and displays the vascular density of SCP and DCP.15,16
Initially, all patients received intravitreal Conbercept injections (0.05 mL/0.5 mg, Lumitin; Chengdu Kang Hong Biotech Co., Ltd., Sichuan Province, China), followed by intravitreal DEX I treatment (0.7 mg, OZURDEX®, Allergan, Inc., Irvine, CA) one week later. Conbercept treatment may be reconsidered for patients with recurrent or persistent central retinal vein occlusion-associated macular edema (CRVO-ME) if the effects of DEX I lasted only 3–4 months.
The primary objective was to assess changes in BCVA and CRT over 12 months, starting from the first intravitreal injection of Conbercept, followed by sequential treatment with DEX I. Additional measures consisted of visualization of superficial and deep capillary networks, alterations in intraocular pressure, and the quantity of necessary interventions.
Statistical Analysis
In order to analyze the data, IBM Corp. SPSS 22.0 software was used. Mean values data that follows a normal distribution will have measurements within 1 standard deviation. Injections intervals and OCTA parameters before and after switching were compared using paired samples t-tests. BCVA, CRT, and IOP were compared using one-way analysis of variance and the LSD post hoc test. All tests were conducted with a two-tailed approach, and a p value less than 0.05 was considered to be statistically significant.
Results
Initially, a total of 40 patients were included in the study, but 6 patients were later excluded due to following up is not being done. At the end, 34 participants’ eyes were examined (17 males, mean age 53.56 ± 9.02 years), 21 (61.8%) were pseudophakic, and 13 eyes (38.2%) were phakic. Before entering the study, the patients had undergone 5.69 ± 0.60 ranibizumab and 1.67 ± 0.52 DEX I injections, as a monotherapy. Table 1 displays the basic traits of the 34 individuals involved in the study.
 |
Table 1 Demographics and Clinical Characteristics of Patients |
Overall, the number of Conbercept injections were 4.2±1.1 required by the patients throughout the study. Compared to the starting point, the BCVA did not exhibit any notable enhancement at different intervals: 0.76 ± 0.39 after 1 month (p > 0.05), 0.75 ± 0.28 after 2 months (p > 0.05), 0.74 ± 0.22 after 3 months (p > 0.05), 0.75 ± 0.25 after 6 months (p > 0.05).and 0.76 ± 0.29 at 12 months (p > 0.05) (Figure 1).
 |
Figure 1 Best corrected visual acuity (BCVA, LogMar) changes before and after treatments. |
The initial CRT measurement was 648.72 ± 59.13 μm, which decreased to 325.69 ± 45.76 μm after one month of receiving the combined treatment, resulting in an average reduction of 323.03 μm. At 2 months, the CRT measured 329.07 ± 42.98 μm, which measured to 338.97 ± 51.27 μm at 3 months, then decreased to 320.07 ± 46.56 μm at 6 months and 316.76 ± 48.72 μm at 12 months. This reduction was statistically significant compared to the initial value (p < 0.001) as shown in Figure 2.
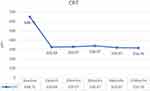 |
Figure 2 Central retinal thickness (CRT) changes before and after treatments. |
Prior to and after combination therapy, there were no significant differences in retinal vessel density (VD) of the SCP and DCP levels(all p > 0.05) as shown in Figures 3 and 4.
 |
Figure 3 Superficial capillary plexuses (SCP) changes before and after treatments. |
 |
Figure 4 Deep capillary plexuses (DCP) changes before and after treatments. |
Intraocular pressure (IOP) showed a significant difference pre- and post-combination therapy (p < 0.05) as illustrated in Figure 5.
 |
Figure 5 Intraocular pressure (IOP) changes before and after treatments. |
In total, 8 eyes experienced adverse events (AEs) at the 12-month follow-up. Among these cases, the majority (n = 6.75%) experienced elevated IOP, with two of them receiving IOP-lowering medications for management. Furthermore, there were two instances of subconjunctival hemorrhage documented throughout the duration of the research. There were no significant adverse events recorded.
Discussion
The findings of current study demonstrate that sequential treatment with Conbercept and DEX I significantly reduces CRT in patients with refractory macular edema secondary to CRVO. The reduction in CRT was observed as early as one month after treatment and was sustained throughout the 12-month follow-up period, highlighting the anatomical benefit of this combination therapy. Nevertheless, despite the notable reduction in CRT, no significant improvements in BCVA were observed at any of the follow-up intervals. This suggests that while the combination therapy is effective in addressing macular edema, it may not result in corresponding functional improvements in vision, potentially due to chronic damage to retinal structures that cannot be reversed. Additionally, no significant changes were noted in retinal vessel density of the superficial and deep capillary plexus, further emphasizing the limited functional response to the treatment. Elevated IOP was a common adverse event, affecting 75% of those who experienced complications, underscoring the need for careful monitoring of IOP during the treatment course. However, in actual clinical practice, there are patients with RVO who do not respond or respond incompletely to either drug as a monotherapy.17 The present study represents the first attempt to assess the effectiveness and safety of combining Combercept and DEX I in a sequential treatment approach for refractory RVO.
The lack of success with ranibizumab or DEX I monotherapy could be due to various root causes, as a single compound may only address a particular part of the pathway that leads to ME, a range of factors can contribute to rebound retinal edema, particularly when multiple factors are involved in its pathophysiology.18 For instance, the interval between injections may be extended as the drug’s pharmacological effect diminishes over time. Despite achieving a reduction in CRT initially, this improvement was not maintained consistently throughout the entire follow-up period. This indicates that ongoing or repeated swelling in the retina after microvascular damage could hinder the enhancement of BCVA.19
Our research found a notable decrease in CRT during the initial month after using Conbercept in combination with DEX I treatment, with BCVA showing improvement that did not reach statistical significance when compared to the starting point. Identified determinants linked to poor visual outcomes after resolving ME include prolonged ME duration, prior VEGF treatment, and inadequate response to initial DEX I treatment.20,21 A retrospective cohort study by Mizuki Tagami et al was recently published, focusing on patients with ME caused by RVO who were initially treated with ranibizumab and later switched to aflibercept, both being anti-VEGF agents. Their results indicated that there was no significant change in BCVA from the beginning to the 12-month follow-up, which is also consistent with the findings of our study from anti-VEGF switching to DEX I injection.22 Furthermore, Blanc et al conducted a retrospective cohort study on patients with ME caused by RVO. In this study, the patients initially received DEX I treatment and subsequently switched to anti-VEGF drugs. The results showed a notable decrease in CRT after 3 years compared to the baseline, and this change was not related to the final BCVA, aligning with the findings of our study.23 Chronic swelling may lead to permanent harm in eyes with neovascular age-related macular degeneration or diabetic macular edema.24,25 Other factors like initial CRT, visual function, age, treatment, RVO type, and BRB breakdown can also affect final BCVA.26 Furthermore, metabolic issues, toxic cytokines, inflammation in the surrounding area, physical stress on retinal cells, and harm to the outer layers of the retina may hinder the function of photoreceptors without the presence of macular fluid.27 The early initiation of sequential therapy is hypothesized to potentially mitigate irreversible retinal damage, thereby improving long-term visual outcomes.
Our data reveal substantial variability in the reduction of CMT at different follow-up intervals over the one-year period. We propose that the limited effectiveness of ranibizumab or DEX I as standalone therapies may stem from various factors. Each treatment may target specific components of the ME pathway, particularly in cases characterized by multiple underlying contributors to the disease process.28 Rebound retinal edema may occur if the time between injections is extended or if the drug’s effectiveness decreases over time. Alternative mechanisms of ME maintenance may be enhanced as the disease progresses to the chronic phase.29 There is a theory that sudden retinal ischemia in CRVO may trigger the production of VEGF by retinal pigment epithelial cells, endothelial cells, and Müller cells.30 In the acute phase of ME, VEGF-mediated vascular permeability increase may be the primary driving force. If restoration of the physiological blood-retinal barrier fails to occur spontaneously or through pharmacological intervention, persistent local secretion of pro-edema factors other than VEGF may ultimately result in capillary insufficiency, neuronal cell dysfunction, and photoreceptor damage.31 In patients with RVO who were treated with intravitreal anti-VEGF therapy, the levels of various cytokines related to the development of RVO, such as IL-1α, IL-6, IL-8, IP-10, MCP-1, and platelet-derived growth factor-AA, did not exhibit notable changes in aqueous humor concentrations. The findings potentially validate the presence of a VEGF-independent pathway in RVO-induced ME.32 It is anticipated that a combined therapeutic approach targeting multiple cytokines and growth factors will be effective in disrupting this pathological cycle.
Ren et al showed that treating 34 patients with macular edema caused by retinal vein occlusion with DEX I and ranibizumab in sequence led to notable enhancements in anatomical structure, BCVA, and VD over a year, along with a decrease in the number of intravitreal injections needed.33 The studies included untreated eyes or cases with shorter durations of ME. Nevertheless, our BCVA findings vary due to the connection between prolonged macular thickening and permanent harm to photoreceptors and retinal pigment epithelium (RPE).34 Chiara Giuffrè et al observed that roughly 66% of patients with persistent macular edema resulting from retinal vein occlusion experienced improvement after one year of treatment with a combination of aflibercept and DEX I. Nevertheless, consistent with our study, this improvement did not lead to a statistically significant increase in visual acuity.35
Throughout the study, we observed a modest decline in the vessel density of both the deep capillary plexus (DCP) and superficial capillary plexus (SCP) by the conclusion of the monitoring period. Previous research has shown that vessel densities in both the SCP and DCP are significantly lower in patients with CRVO compared to healthy eyes, with particularly notable damage evident in the DCP.36,37 The deeper retinal layers are highly vascularized and may be more vulnerable to central retinal vein occlusion (CRVO) than the superficial layers, with macular edema primarily affecting these deeper regions. Recurrent or persistent macular edema can lead to significant capillary loss, making recovery through anti-VEGF or DEX I treatments more challenging.38 Research conducted by Agnes Glacet-Bernard et al demonstrated that although DEX I was effective in addressing macular edema, OCTA showed only a slight decrease in average macular blood vessel density, which is consistent with our results.39
However, the findings of Min Zhang et al demonstrated a significant advantage of DEX I in preserving retinal perfusion in patients with RVO.40 We propose that the discrepancies in findings among various studies could stem from differences in instrumentation, the specific regions of focus, the methodologies used for calculating vascular density, and the timing of observations. A significant contributor to this variability is likely the duration and severity of the disease. Although treatments with anti-VEGF or DEX I may slow down the progression of ischemia or yield short-term benefits, they might not avert long-term ischemic damage. Our findings indicate a strong likelihood of progressive and irreversible ischemic injury to the deep retinal vessels.
The cumulative incidence of adverse events in this study was 6 cases of transient and mild elevated intraocular pressure (IOP <30 mmHg), 2 of which were effectively controlled by the use of antihypertensive medications. When patients have increased pressure inside their eyes, it is imperative to be aware of this possibility,15,41 as there is no agreement on the frequency of hormonal reaction and subsequent glaucoma in patients treated with dexamethasone in clinical trials.
This study has several limitations, including its retrospective design, the lack of a control group, and the small sample size. The sample size was determined based on feasibility, considering the relatively rare nature of refractory CRVO-ME and the availability of eligible patients within the study period. While no formal sample size calculation was performed prior to the study, we aimed to ensure adequate representation to observe meaningful clinical outcomes. However, we also acknowledge that this sample size may limit the generalizability of the findings. Due to the retrospective design, retinal ischemic progression could not be measured and it was not possible to determine whether disease characteristics affected treatment outcomes. Furthermore, the study’s validity was compromised by the unequal distribution of drug types used prior to switching. Additionally, it should be mentioned that the analysis using OCTA was restricted to the region surrounding the foveal ring, therefore the findings should not be extrapolated to the complete retinal vascular system. Future researchers are encouraged to conduct larger, prospective comparative trials to verify the advantages of sequential treatment strategies.
Conclusion
In conclusion, transitioning from monotherapy to sequential treatment with Conbercept and DEX can lead to improved retinal anatomy in patients with refractory ME caused by secondary CRVO. Nevertheless, there was no notable improvement in visual clarity or the small blood vessels in the retina detected. While our study did not explicitly compare injection frequencies, the combination therapy of Conbercept and DEX I appeared to maintain CRT reduction over 12 months, potentially reducing the overall treatment burden compared to monotherapy. Further research is needed to confirm this finding.
Data Sharing Statement
The data used to support the findings of this study are included in the article.
Acknowledgments
We thank Home for Researchers editorial team (www.home-for-researchers.com) for improving the English language in this manuscript.
Author Contributions
All authors made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; participated in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Rogers S, McIntosh RL, Cheung N, et al. The Prevalence of Retinal Vein Occlusion: pooled Data from Population Studies from the United States, Europe, Asia, and Australia. Ophthalmology. 2010;117(2):313–319.e1. doi:10.1016/j.ophtha.2009.07.017
2. Ascaso FJ, Huerva V, Grzybowski A. The Role of Inflammation in the Pathogenesis of Macular Edema Secondary to Retinal Vascular Diseases. Mediators Inflam. 2014;2014:1–6. doi:10.1155/2014/432685
3. Campochiaro PA, Sophie R, Pearlman J, et al. Long-term Outcomes in Patients with Retinal Vein Occlusion Treated with Ranibizumab. Ophthalmology. 2014;121(1):209–219. doi:10.1016/j.ophtha.2013.08.038
4. O’Day R, Ali N, Lim LL, Sandhu S, Chau T, Wickremasinghe S. A treat and extend protocol with Aflibercept for cystoid macular oedema secondary to central retinal vein occlusion – an 18-month prospective cohort study. BMC Ophthalmology. 2020;20(1). doi:10.1186/s12886-020-01346-8
5. H-y Z, Liu Q, X-x L, Y-x S, Z-j Z. One-year efficacy of intravitreal conbercept injection for macular oedema secondary to central retinal vein occlusion in Chinese patients. Eye. 2020;34(8):1459–1464. doi:10.1038/s41433-020-0827-y
6. Haller JABF, Belfort R, Blumenkranz MS, et al. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion twelve-month study results. Ophthalmology. 2011;118(12):2453–2460. doi:10.1016/j.ophtha.2011.05.014
7. Khurana RN, Chang LK, Bansal AS, Palmer JD, Wu C, Wieland MR. Aflibercept for Previously Treated Macular Edema Associated with Central Retinal Vein Occlusions: 1-Year Results of the NEWTON Study. Ophthalmol Retina. 2018;2(2):128–133. doi:10.1016/j.oret.2017.05.017
8. Pielen A, Bühler AD, Heinzelmann SU, Böhringer D, Ness T, Junker B. Switch of Intravitreal Therapy for Macular Edema Secondary to Retinal Vein Occlusion from Anti-VEGF to Dexamethasone Implant and Vice Versa. J Ophthalmology. 2017;2017:1–7. doi:10.1155/2017/5831682
9. Ozkaya A, Tulu B, Garip R. Aflibercept in macular edema secondary to retinal vein occlusion: a real life study. Saudi J Ophthalmol. 2017;31(4):211–215. doi:10.1016/j.sjopt.2017.09.009
10. Hoerauf H, Feltgen N, Weiss C, et al. Clinical Efficacy and Safety of Ranibizumab Versus Dexamethasone for Central Retinal Vein Occlusion (COMRADE C): a European Label Study. Am J Ophthalmol. 2016;169:258–267. doi:10.1016/j.ajo.2016.04.020
11. Terao R, Fujino R, Ahmed T. Risk Factors and Treatment Strategy for Retinal Vascular Occlusive Diseases. J Clin Med. 2022;11(21). doi:10.3390/jcm11216340
12. BD EDD. Recent advances in understanding and managing retinal vein occlusions. F1000Research. 7;467. doi:10.12688/f1000research.12886.1
13. Li X, Wang N, Liang X, et al. Safety and efficacy of dexamethasone intravitreal implant for treatment of macular edema secondary to retinal vein occlusion in Chinese patients: randomized, sham-controlled, multicenter study. Graefes Arch Clin Exp Ophthalmol. 2017;256(1):59–69. doi:10.1007/s00417-017-3831-6
14. ZQ DY, Zhang AQ, Cai XJ, et al. Microvascular changes after conbercept therapy in central retinal vein occlusion analyzed by optical coherence tomography angiography. Intern J Ophthal. 12(5):802–808. doi:10.18240/ijo.2019.05.16
15. Pacella E, Loffredo L, Malvasi M, et al. Effects of Repeated Intravitreal Injections of Dexamethasone Implants on Intraocular Pressure: a 4-Year Study. Clin Ophthalmol. 2020;14:3611–3617. doi:10.2147/opth.S265691
16. Suciu C-I, Suciu V-I, Nicoara S-D, Sokolovska J. Optical Coherence Tomography (Angiography) Biomarkers in the Assessment and Monitoring of Diabetic Macular Edema. J Diabetes Res. 2020;2020:1–10. doi:10.1155/2020/6655021
17. Jumper JM, Dugel P, Chen S, Blinder K, Walt J. Anti-VEGF treatment of macular edema associated with retinal vein occlusion: patterns of use and effectiveness in clinical practice (ECHO study report 2). Clin Ophthalmol. 2018;12:621–629. doi:10.2147/opth.S163859
18. Binder S. Loss of reactivity in intravitreal anti-VEGF therapy: tachyphylaxis or tolerance? Br J Ophthalmol. 2011;96(1):1–2. doi:10.1136/bjophthalmol-2011-301236
19. Parodi MB, Iacono P, De Benedetto U, Cascavilla M, Bandello F. Rebound Effect After Intravitreal Dexamethasone Implant for the Treatment of Macular Edema Secondary to Central Retinal Vein Occlusion. J Ocul Pharmacol Ther. 2012;28(6):566–568. doi:10.1089/jop.2012.0016
20. Farinha C, Marques JP, Almeida E, et al. Treatment of Retinal Vein Occlusion with Ranibizumab in Clinical Practice: longer-Term Results and Predictive Factors of Functional Outcome. Ophthalmic Research. 2016;55(1):10–18. doi:10.1159/000440848
21. Busch C, Rehak M, Sarvariya C, et al. Long-term visual outcome and its predictors in macular oedema secondary to retinal vein occlusion treated with dexamethasone implant. Br J Ophthalmol. 2019;103(4):463–468. doi:10.1136/bjophthalmol-2017-311805
22. Tagami M, Sai R, Fukuda M, Azumi A. Prolongation of injection interval after switching therapy from ranibizumab to aflibercept in Japanese patients with macular edema secondary to branch retinal vein occlusion. Clin Ophthalmol. 2017;11:403–408. doi:10.2147/opth.S128651
23. Blanc J, Deschasse C, Kodjikian L, Dot C, Bron A-M, Creuzot-Garcher C. Safety and long-term efficacy of repeated dexamethasone intravitreal implants for the treatment of cystoid macular edema secondary to retinal vein occlusion with or without a switch to anti-VEGF agents: a 3-year experience. Graefes Arch Clin Exp Ophthalmol. 2018;256(8):1441–1448. doi:10.1007/s00417-018-4016-7
24. Li Z, Gu X, Song S, et al. Structural and Visual Changes in Branch Retinal Vein Occlusion Patients with Retinal Atrophy. J Ophthalmology. 2022;2022:1–9. doi:10.1155/2022/8945467
25. Ablonczy Z, Dahrouj M, Marneros AG. Progressive dysfunction of the retinal pigment epithelium and retina due to increased VEGF‐A levels. FASEB J. 2014;28(5):2369–2379. doi:10.1096/fj.13-248021
26. Spooner K, Fraser-Bell S, Hong T, Chang A. Patient-reported outcomes from a Phase IV study of aflibercept in patients with refractory retinal vein occlusions. Taiwan J Ophthalmol. 2021;11(3):244–250. doi:10.4103/tjo.tjo_19_20
27. Yiu G, Welch RJ, Wang Y, Wang Z, Wang P-W, Haskova Z. Spectral-Domain OCT Predictors of Visual Outcomes after Ranibizumab Treatment for Macular Edema Resulting from Retinal Vein Occlusion. Ophthalmol Retina. 2020;4(1):67–76. doi:10.1016/j.oret.2019.08.009
28. K-TA Z-LK, Karska-Basta I, Pociej-Marciak W, Romanowska-Dixon B. Non-responsiveness and tachyphylaxis to anti-vascular endothelial growth factor treatment in naive patients with exudative age-related macular degeneration. J Physiol Pharmacol. 2019;70(5). doi:10.26402/jpp.2019.5.13
29. de Salles MC, Epstein D. Real-life study of the use of anti-VEGF therapy versus dexamethasone implant for treatment of macular edema in retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2021;259(9):2653–2660. doi:10.1007/s00417-021-05146-8
30. MR MSA, Bamakrid M, Lee Y, Muni RH. Changes in Aqueous and Vitreous Inflammatory Cytokine Levels in Retinal Vein Occlusion: a Systematic Review and Meta-analysis. J VitreoRet Diseases. 2019;4(1):36–64. doi:10.1177/2474126419880391
31. Yong H, Qi H, Yan H, Wu Q, Zuo L. The correlation between cytokine levels in the aqueous humor and the prognostic value of anti-vascular endothelial growth factor therapy for treating macular edema resulting from retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2021;259(11):3243–3250. doi:10.1007/s00417-021-05211-2
32. NM SY, Suzuki K, Yamazaki H, Miyagawa Y. Expression profiles of cytokines and chemokines in vitreous fluid in diabetic retinopathy and central retinal vein occlusion. Japanese J Ophthal. 2011;55(3):256–263. doi:10.1007/s10384-011-0004-8
33. Ren F, Gong H, Zhang H, et al. Combination Therapy Using Anti-Vascular Endothelial Growth Factor (VEGF) Drugs and Steroids for Macular Edema in Retinal Vein Occlusions. Med Sci Monit. 2023:29. doi:10.12659/msm.939277
34. Spooner K, Fraser-Bell S, Hong T, Chang AA. Five-year outcomes of retinal vein occlusion treated with vascular endothelial growth factor inhibitors. BMJ Open Ophthal. 2019;4(1). doi:10.1136/bmjophth-2018-000249
35. Giuffrè C, Cicinelli MV, Marchese A, Coppola M, Parodi MB, Bandello F. Simultaneous intravitreal dexamethasone and aflibercept for refractory macular edema secondary to retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2020;258(4):787–793. doi:10.1007/s00417-019-04577-8
36. Ouederni M, Khalifa MH, Sassi H, Nefaa F, Ayed O, Cheour M. Quantitative analysis of microvascular network with optical coherence tomography angiography and its correlation with visual acuity in retinal vein occlusion. J Current Ophthal. 2021;33(4). doi:10.4103/joco.joco_163_21
37. Fan L, Zhu Y, Liao R. Evaluation of macular microvasculature and foveal avascular zone in patients with retinal vein occlusion using optical coherence tomography angiography. Intl Ophthalmol. 2021;42(1):211–218. doi:10.1007/s10792-021-02015-5
38. Brar M, Sharma M, Grewal SS, Grewal D. Quantification of retinal microvasculature and neurodegeneration changes in branch retinal vein occlusion after resolution of cystoid macular edema on optical coherence tomography angiography. Indian J Ophthalmology. 2019;67(11). doi:10.4103/ijo.IJO_1554_18
39. Glacet-Bernard A, Sellam A, Coscas F, Coscas G, Souied EH. Optical Coherence Tomography Angiography in Retinal Vein Occlusion Treated with Dexamethasone Implant: a New Test for Follow-Up Evaluation. European J Ophthal. 2016;26(5):460–468. doi:10.5301/ejo.5000829
40. LY ZM, Song M, Yu Y, et al. Intravitreal Dexamethasone Implant Has Better Retinal Perfusion than Anti-Vascular Endothelial Growth Factor Treatment for Macular Edema Secondary to Retinal Vein Occlusion: a Five-Year Real-World Study. Ophthalmic Research. 2022;247–258. doi:10.1159/000527447
41. Korobelnik J-F, Kodjikian L, Delcourt C, et al. Two-year, prospective, multicenter study of the use of dexamethasone intravitreal implant for treatment of macular edema secondary to retinal vein occlusion in the clinical setting in France. Graefes Arch Clin Exp Ophthalmol. 2016;254(12):2307–2318. doi:10.1007/s00417-016-3394-y
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

