Back to Journals » Clinical Ophthalmology » Volume 19
Evaluating the Impact of Angle Kappa on Effective Optical Zone in Kerato-Lenticule Extraction (KLEx) Surgery with Intraoperative Angle Kappa Adjustment
Authors Tsai TH, Lin ET, Hsu JH, Sun CC
Received 4 February 2025
Accepted for publication 10 April 2025
Published 28 April 2025 Volume 2025:19 Pages 1417—1426
DOI https://doi.org/10.2147/OPTH.S517130
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Tsung-Hsien Tsai,1,2,* Erh-Tsan Lin,3,* Jui-Hung Hsu,3 Chi-Chin Sun1,2
1Department of Ophthalmology, Chang Gung Memorial Hospital, Keelung, Taiwan; 2School of Medicine, College of Medicine, Chang Gung University, Taoyuan, Taiwan; 3Department of Medical Education, Chang Gung Memorial Hospital, Keelung, Taiwan
*These authors contributed equally to this work
Correspondence: Chi-Chin Sun, Department of Ophthalmology, Chang Gung Memorial Hospital, 222 Maijin Road, Keelung, 204, Taiwan, Tel +886-2-24313131, Fax +886-2-24311190, Email [email protected]
Purpose: This study aimed to investigate the influence of preoperative angle kappa on postoperative effective optical zone (EOZ) in KLEx patients with intraoperative angle kappa adjustment.
Methods: This retrospective study included 174 eyes from 89 myopic patients who underwent the KLEx procedure with intraoperative angle kappa adjustments. Preoperative angle kappa (μ) was approximated as the chord distance between the pupil center and corneal vertex. The cohort was divided into two groups: large angle kappa (μ > 0.2 mm, n = 84) and small angle kappa (μ ≤ 0.2 mm, n = 90). EOZ parameters, including EOZ reduction ratio (RR=EOZ/planned optical zone, %), major and minor axis, decentration, and eccentricity, were measured at one month postoperatively. Linear regression analyses were performed to assess the relationships between preoperative angle kappa and postoperative EOZ parameters.
Results: Postoperatively, RR, major and minor axis, decentration and eccentricity did not differ significantly between groups. Univariate linear regression revealed significant but modest negative correlation of angle kappa with RR and minor axis (adjusted R² = 0.05 and 0.03; P = 0.003 and 0.02, respectively). Further, multivariate regression incorporating preoperative spherical equivalent demonstrated that angle kappa was not a significant predictor of EOZ parameters.
Conclusion: In conclusion, our study showed that preoperative angle kappa had minimal effect on EOZ parameters in KLEx surgery when appropriate intraoperative adjustments for angle kappa were implemented.
Keywords: KLEx, angle kappa, effective optical zone
Introduction
Kerato-lenticule extraction (KLEx) surgery has emerged as an effective, stable and safe refractive procedure in the past decade, distinguished by its minimal invasiveness, better postoperative corneal biomechanics and dry eye parameters as well as less induction of higher-order aberrations (HOAs) compared to conventional laser-assisted in situ keratomileusis (LASIK).1,2 Despite these advantages, precise centration of the treatment remains a significant challenge due to lack of active eye-tracking system.3 Intraoperative angle kappa adjustments had been proposed as an effective method, especially in patients with large angle kappa, to ensure the visual axis aligns correctly with the treatment zone, thereby minimizing the induction (Δ) of HOAs and enhancing the quality of vision postoperatively.4,5 Thus, routine preoperative measurement of angle kappa in KLEx patients is crucial.
In addition, postoperative effective optical zone (EOZ) —the actual ablated corneal region in refractive surgery providing optimal vision—has been shown to correlate with HOAs and visual quality.6–8 Numerous studies had investigated the influencing factors of EOZ including preoperative parameters such as the degree of myopia or astigmatism correction, Q value, corneal keratometry, epithelial thickness and eccentricity.7 However, the effect of preoperative angle kappa on EOZ in KLEx had not been fully studied. Therefore, our study aims to investigate whether preoperative angle kappa influences postoperative EOZ in patients undergoing KLEx surgery with intraoperative angle kappa adjustment.
Methods
Patients who underwent KLEx performed by the same refractive surgeon (Dr. Chi-Chin Sun) at Chang Gung Memorial Hospital between 2018 and 2022 were included. The inclusion criteria were: (1) Age ≥18 years old; (2) Baseline myopia or myopic astigmatism; (3) No history of ocular disease aside from refractive errors; and (4) Availability for at least one follow-up examination at 1 month postoperatively. The exclusion criteria were: (1) A history of refractive or ocular surgeries; (2) The presence of ocular diseases other than refractive errors; (3) Autoimmune diseases; (4) Postoperative follow-up of less than one month; and (5) Incomplete medical records during the follow-up period. A total of 174 eyes were enrolled in the study. The study was conducted in accordance with the tenets of the Declaration of Helsinki and received ethical approval from the Institutional Review Board (IRB) of Chang Gung Memorial Hospital (IRB No. 2407090041). Given the retrospective nature of the study and its lack of impact on patient treatment or outcomes, the IRB waived the requirement for obtaining patient consent to review their medical records. Confidentiality was ensured by removing personal identifiers during data collection.
KLEx Surgical Technique
All KLEx surgeries were performed using the small incision lenticule extraction (SMILE) procedure on the VisuMax 500kHz laser system (Carl Zeiss Meditec AG, Germany) with a pulse energy of 140 nJ. The cap diameter was set between 7.0 and 8.0 mm, with a thickness ranging from 100 to 120 μm, and the planned optical zone (POZ) was maintained between 6.0 and 7.0 mm. In each procedure, a precise 3.0 mm incision was made at the 11 o’clock position. Preoperative triple marking (0, 180 and 270 degrees, respectively) centration and intraoperative angle kappa adjustment based on Pentacam (Oculus, Wetzlar, Germany) were performed. The center of suction ring was centered on the corneal vertex (CV), adjusted based on preoperatively measured deviation from the pupil center (PC). Postoperatively, patients were instructed to follow a regimen of 1% prednisolone acetate ophthalmic suspension (Prednicone; Winston, Taiwan) and 0.5% levofloxacin ophthalmic solution (Cravit; Santen, Japan), administered four times daily for two weeks.
Preoperative and Postoperative Examinations
All patients underwent comprehensive preoperative examinations and at least one follow-up ophthalmologic examination at one month postoperatively. The evaluations including detailed history taking, manifest and cycloplegic refractions, non-contact intraocular pressure assessment, slit lamp and fundoscopic examinations, scotopic pupil size measurement, as well as corneal tomography, were performed before and after surgery. Scotopic pupil size was measured using the Hartmann-Shack aberrometer (iDesign; J&J Vision, Santa Ana, CA). Corneal topographic and tomographic data, including central corneal thickness (CCT), thinnest corneal thickness (TCT), mean keratometry (Km), anterior corneal Q-value, angle kappa, and corneal HOAs were obtained using the Pentacam HR (Oculus, Wetzlar, Germany). Pentacam images were obtained at least twice to ensure high-quality results, and technicians assisted in selecting the best image for further analysis. Corneal aberrations were measured within a 6.0 mm zone centered at CV up to the sixth order based on Zernike analysis. Since the Pentacam cannot directly measure angle kappa, it was approximated by calculating the chord distance (µ) between the PC and the CV, as described by Chang and Waring.9 The PC and CV were measured using the Pentacam. Additionally, the absolute values of X-Y Cartesian coordinates of PC were recorded as µ(x) and µ(y), respectively, representing the absolute x and y deviation of CV from PC.
EOZ Measurement
The EOZ was defined as the zero-curvature colored difference line on the tangential curvature difference map (TCDM) generated by the Pentacam.10 EOZ size, decentration, and eccentricity parameters were quantified using ImageJ software (version 1.54; National Institutes of Health, Bethesda, MD) by two investigators (THT and ETL), and the final values were obtained by averaging their measurements. For measurement, a color threshold was initially applied to isolate the EOZ, after which the images were converted to binary format. Following this, morphological operations were performed to refine the binary images. Finally, the EOZ parameters were measured and analyzed using appropriate ImageJ functions. The EOZ size parameters included measurements of the area (mm²), perimeter (mm), major axis (mm), and minor axis (mm). The change in optical zone size in area was calculated by the optical zone reduction ratio (RR=EOZ/POZ, %). Decentration parameters comprised the absolute decentration (mm) and the absolute decentration along the x- and y-axes (mm) of the EOZ centroid relative to the CV as captured by the Pentacam. Eccentricity was calculated as the ratio of the major axis to the minor axis, representing the degree of deviation from a perfectly circular EOZ.
Statistical Analysis
All statistical analyses were performed using SPSS software (version 26; IBM Inc., Chicago). Sample size calculation focused on linear regression between the preoperative angle kappa and EOZ parameters. The minimal estimated sample size was determined based on an R2>0.3 at a significance level of 0.05 and power of 0.8, resulting in a minimum required sample size of 21. The study cohort was stratified into two groups: large angle kappa (µ > 0.2 mm) and small angle kappa (µ ≤ 0.2 mm), consistent with previous studies.11,12 Additionally, patients were classified based on the mean values of µ(x) and µ(y), providing an alternative method to categorize the cohort. Furthermore, to validate our results against previous studies on the relationship between spherical equivalent (SE) and the EOZ, we also divided the cohort into high and low SE groups based on the −6.00D of high myopia definition.
The Kolmogorov–Smirnov test was applied to assess the normality of the data distribution, which indicated a non-parametric distribution of our cohort. Categorical variables were reported as numbers and percentages, while continuous variables were presented as mean ± standard deviation. Group differences in continuous data were analyzed using the Mann–Whitney U-test, and categorical variables were compared using Chi-square tests. Univariate and multivariate linear regression using stepwise selection method were employed to evaluate the relationships between preoperative angle kappa, µ(x), µ(y), SE and postoperative EOZ.
Results
Preoperative Patient Characteristics
A total of 174 eyes from 89 patients underwent KLEx surgery had been included in this study. Preoperative demographics were shown in Table 1. No statistically significant differences were found between large and small angle kappa, µ(x), and µ(y) groups including sex, age, sphere (D), cylinder (D), SE (D), scotopic pupil size, CCT, TCT, Km, Q value, POZ, and HOAs.
 |
Table 1 Preoperative Patient Characteristics |
The distribution of preoperative angle kappa was plotted in Figure 1. The scatter plot showed that 51.7% of eyes were in the µ ≤ 0.2mm group, and 48.3% were in the µ>0.2mm group. CV was distributed mainly inferotemporal comparing to PC (43.4%), while in the µ ≤ 0.2mm group inferonasal and inferotemporal were the most often observed (both 33.8%), the µ>0.2mm group mostly lied inferotemporal to PC (52.4%). The superotemporal had the lowest proportion of distribution in both groups (7.8%, 9.8%, respectively).
Postoperative Visual Outcomes One month After KLEx Surgery
The mean uncorrected distance visual acuity (UDVA) and corrected distance visual acuity (CDVA) one month postoperatively was −0.05 ± 0.10 and −0.07 ± 0.08 logMAR, respectively, resulting in a safety index of 1.12 and efficacy index of 0.97. Since the target refraction for two patients around 40 years old was −1.00 D, excluding these patients from the analysis improved the efficacy index to 1.01. Detailed refractive and visual outcomes were presented in Supplementary Figure 1.
EOZ parameters and ΔHOAs between different groups one month after surgery were detailed in Table 2. There was no statistically significant difference regarding all EOZ parameters and ΔHOAs between the large and small angle kappa, µ(x), and µ(y) groups.
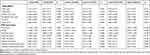 |
Table 2 Postoperative Outcomes One month After KLEx Surgery |
Relationships Between Preoperative SE and EOZ Parameters
Table 3 demonstrated the demographics and postoperative outcomes for both the high and low SE groups. Preoperative characteristics showed no significant differences between the two groups except for sphere (D), cylinder (D), and POZs. Due to the significant difference in POZ between the groups, we further analyzed the change in optical zone size by RR. The low SE group (SE>-6.0D) exhibited a smaller reduction in optical zone area compared to the high SE group (SE<-6.0D). As shown in Figure 2, linear regression analysis identified a significant correlation between preoperative SE and RR (adjusted R2 = 0.402, unstandardized beta (B) = 2.74; 95% confidence interval (CI): 2.24, 3.24; P <0.001). SE also correlated significantly with other EOZ parameters including perimeter (adjusted R2 = 0.332, B =0.63; 95% CI: 0.50, 0.77; P <0.001), major axis (adjusted R2 = 0.506, B = 0.20; 95% CI: 0.17, 0.23; P <0.001) and minor axis (adjusted R2 = 0.501, B = 0.16; 95% CI: 0.14, 0.18; P <0.001). Detailed linear regression analysis was shown in Supplementary Table 1.
 |
Table 3 Preoperative and Postoperative Outcomes Between High and Low SE Groups |
Linear Regression Analysis of Preoperative Angle Kappa and EOZ Parameters
To assess the effects of preoperative angle kappa on EOZ parameters, we performed univariate linear regression analysis assessing the relationships between angle kappa, µ(x), and µ(y) with EOZ parameters. Statistically significant linear associations were observed between angle kappa and µ(y) with RR (angle kappa: adjusted R2 = 0.046, B = −20.10; 95% CI: −33.08, −7.12; P = 0.003; µ(y): adjusted R2 = 0.032, B = −18.31; 95% CI: −32.2, −4.42; P = 0.010) and minor axis length (angle kappa: adjusted R2 = 0.026, B = −0.82; 95% CI: −1.51, −0.13; P = 0.020; µ(y): adjusted R2 = 0.021, B = −0.80; 95% CI: −1.54, −0.07; P = 0.032). No significant associations were found between µ(x) and any EOZ parameters. Linear regression analysis was detailed in Supplementary Table 1.
To further assess these associations, a multivariate regression analysis was conducted, incorporating preoperative SE, angle kappa, µ(x) and µ(y) as independent variables to predict RR and minor axis, as demonstrated in Table 4. In this model, only preoperative SE remained a significant predictor of both RR (adjusted R2 = 0.402, standardized beta = 0.64; P < 0.001) and EOZ minor axis (adjusted R2 = 0.501, standardized beta = 0.71; P < 0.001), while angle kappa, µ(x) and µ(y) did not show significant effects.
 |
Table 4 Multivariate Regression Analysis Between SE, Angle Kappa, and EOZ Parameters |
Discussion
Our study demonstrated that preoperative angle kappa had a minimal impact on the size of the EOZ, and no significant association was found between angle kappa and EOZ decentration or eccentricity if angle kappa was adjusted intraoperatively. Previous research has established links between angle kappa and HOAs, as well as between EOZ parameters and HOAs.8,11,13–18 This study advances the current understanding by further exploring the relationships between preoperative angle kappa and EOZ parameters in KLEx surgery with intraoperative angle kappa adjustment, providing additional insights into its potential effects on postoperative outcomes.
In our study, the preoperative CV was predominantly located in the inferotemporal quadrant relative to the PC, a finding consistent with Qian et al, who reported that most PCs were positioned superonasally to the CV before ICL implantation.19 In contrast, other studies have shown that the PC is typically located more temporally relative to the CV.20–23 This discrepancy is likely due to differences in study populations and SEs. While previous studies primarily focused on normal populations, our study examined myopic patients. Reinstein et al demonstrated a negative correlation between SE and the X-component of pupil offset, indicating that lower myopia is associated with a more temporal deviation of the PC.23 This variation in patient selection may account for the less temporal deviation of the PC observed in our study.
Our study found no significant differences in ΔHOAs or EOZ parameters between the large and small angle kappa groups one month after KLEx surgery, following intraoperative angle kappa adjustment. Previous research has suggested that a large angle kappa may negatively affect postoperative visual quality, including increased HOAs.12 For instance, Guo et al reported significant changes in spherical aberration and oblique trefoil in patients with larger angle kappa after KLEx surgery.24 However, our findings align with studies that utilized preoperative adjustments based on angle kappa. Xie et al found no significant differences in HOAs between large and small angle kappa groups when intraoperative angle kappa adjustment techniques were employed.5 Similarly, Liu et al demonstrated that using tear film mark (TFM) centration significantly reduced HOA parameters compared to PC centration, with no correlation between angle kappa and HOAs when the TFM method was applied.25 These results suggest that proper centration techniques can effectively mitigate the potential negative impact of angle kappa on postoperative visual outcomes.
Our univariate linear regression analysis showed that angle kappa and µ(y) were significantly related to RR and minor axis, however the R² values of these models were all below 0.05. This indicates that preoperative angle kappa accounts for only a small fraction of the variance in postoperative outcomes. Further multivariate regression analysis demonstrated that both angle kappa and µ(y) were insignificant. Therefore, our findings suggest that, with appropriate intraoperative angle kappa adjustment during the KLEx procedure, preoperative angle kappa does not significantly influence the postoperative EOZ, providing valuable insights for surgical planning.
We compared outcomes between high and low SE groups and identified positive correlations between preoperative SEs and EOZ parameters. The relationship between preoperative SE and EOZ has been a topic of debate in the literature. Some studies did not find a significant effect of SE on EOZ size or its reduction,15,26,27 while others reported a positive correlation between SE and EOZ size.14,28 For example, Fu et al demonstrated a larger functional optical zone and a smaller reduction in optical zone size in the low myopia group.14 Similarly, Moshirfar et al found that manifest SE was positively correlated with EOZ area and major diameter in KLEx.28 The positive association may be attributed to the greater amount of tissue ablated in higher myopic eyes, with the subsequent corneal remodeling potentially altering the corneal Q-value.15 As noted in previous studies, a more oblate cornea following tissue ablation could lead to a reduction in the size of the EOZ.15,29
Our study had several limitations. First, as a retrospective study, it is subject to inherent recall and missing data biases, which may affect the accuracy and completeness of the data. However, our preoperative variables—including refractive status, tomographic parameters, POZs, and HOAs—were well-matched, which helped minimize differences between the angle kappa groups. Second, the follow-up period was relatively short, limited to only one month. Nevertheless, previous studies have demonstrated that EOZ parameters tend to stabilize within one week after KLEx procedures, suggesting that our follow-up period may still provide meaningful insights.30 Finally, although our retrospective design did not allow for a dedicated control group without angle kappa adjustment, we emphasize that the primary focus of our study is to delineate the relationship between angle kappa and EOZ with adequate intraoperative adjustments.
In conclusion, our study demonstrated that preoperative angle kappa had minimal impact on EOZ parameters in KLEx surgery when appropriate intraoperative angle kappa adjustments were implemented. However, the absence of a control group without angle kappa adjustments limits direct comparisons of efficacy. Future prospective studies with a dedicated control group and a longer follow-up period are warranted.
Acknowledgments
The authors thank Jing-Yi Huang for the statistical consultation and wish to acknowledge for statistical and data analysis assistance and interpretation by the Center for Big Data Analytics and Statistics, Chang Gung Memorial Hospital, Linkou. Additionally, the authors would like to acknowledge the use of ChatGPT-4o, developed by OpenAI, for grammar and language editing assistance in the preparation of this manuscript. The authors have reviewed and verified the accuracy of the content.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ganesh S, Brar S, Arra RR. Refractive lenticule extraction small incision lenticule extraction: a new refractive surgery paradigm. Indian J Ophthalmol. 2018;66(1):10–19. doi:10.4103/ijo.IJO_761_17
2. Fuest M, Mehta JS. Advances in refractive corneal lenticule extraction. Taiwan J Ophthalmol. 2021;11(2):113–121. doi:10.4103/tjo.tjo_12_21
3. Liu Q, Yang X, Lin L, et al. Review on centration, astigmatic axis alignment, pupil size and optical zone in SMILE. Asia Pac J Ophthalmol. 2019;8(5):385–390. doi:10.1097/01.APO.0000580144.22353.46
4. Shao T, Wang Y, Ng ALK, et al. The effect of intraoperative angle kappa adjustment on higher-order aberrations before and after small incision lenticule extraction. Cornea. 2020;39(5):609–614. doi:10.1097/ICO.0000000000002274
5. Xie M, Deng Y, Sun C, Qiu L, Tang J. Higher-order aberrations and visual quality after incision lenticule extraction surgery with intraoperative angle kappa adjustments between small and large kappa patients: a 2-year follow-up. Indian J Ophthalmol. 2023;71(5):1849–1854. doi:10.4103/IJO.IJO_3017_22
6. Fan-Paul NI, Li J, Miller JS, Florakis GJ. Night vision disturbances after corneal refractive surgery. Surv Ophthalmol. 2002;47(6):533–546. doi:10.1016/s0039-6257(02)00350-8
7. Huang Y, Zhan B, Han T, Zhou X. Effective optical zone following small incision lenticule extraction: a review. Graefes Arch Clin Exp Ophthalmol. 2024;262(6):1657–1665. doi:10.1007/s00417-023-06263-2
8. Moshirfar M, Herron MS, Cha DS, Santos J, Payne CJ, Hoopes PC. Comparing effective optical zones after myopic ablation between LASIK, PRK, and SMILE with correlation to higher order aberrations. J Refract Surg. 2023;39(11):741–750. doi:10.3928/1081597X-20231016-02
9. Chang DH, Waring G. The subject-fixated coaxially sighted corneal light reflex: a clinical marker for centration of refractive treatments and devices. Am J Ophthalmol. 2014;158(5):863–874. doi:10.1016/j.ajo.2014.06.028
10. Liang C, Yan H. Methods of corneal vertex centration and evaluation of effective optical zone in small incision lenticule extraction. Ophthalmic Res. 2023;66(1):717–726. doi:10.1159/000529922
11. Lai X, Liu X, Zeng T, Huang Y, Yang X. Comparison of visual outcomes and optical aberrations after SMILE with intraoperative kappa angle adjustments between small and large kappa angles. Sci Rep. 2024;14(1):14551. doi:10.1038/s41598-024-65366-w
12. Shao T, Wang Y, Hao W, Zhang J, Cui T. Influence and significance of angle kappa on total ocular aberrations before and after SMILE surgery. Chin J Exp Ophthalmol. 2022;40(6):525–532. doi:10.3760/cma.j.cn115989-20190305-00098
13. Ding X, Fu D, Wang L, Zhou X, Yu Z. Functional optical zone and visual quality after small-incision lenticule extraction for high myopic astigmatism. Ophthalmol Ther. 2021;10(2):273–288. doi:10.1007/s40123-021-00330-9
14. Fu D, Wang L, Zhou X, Yu Z. Functional optical zone after small-incision lenticule extraction as stratified by attempted correction and optical zone. Cornea. 2018;37(9):1110–1117. doi:10.1097/ICO.0000000000001669
15. Hou J, Wang Y, Lei Y, Zheng X. Comparison of effective optical zone after small-incision lenticule extraction and femtosecond laser-assisted laser in situ keratomileusis for myopia. J Cataract Refract Surg. 2018;44(10):1179–1185. doi:10.1016/j.jcrs.2018.06.046
16. Liu S, Zhang X, Niu L, Yu Z, Zhou X, Zhao J. Comparison of the functional optical zone in eyes with high myopia with high astigmatism after SMILE and FS-LASIK. J Refract Surg. 2022;38(9):595–601. doi:10.3928/1081597X-20220725-01
17. Ozulken K, Kaderli A. The effect of different optical zone diameters on the results of high-order aberrations in femto-laser-assisted in situ keratomileusis. Eur J Ophthalmol. 2020;30(6):1272–1277. doi:10.1177/1120672119865688
18. Zhou C, Li Y, Wang Y, Fan Q, Dai L. Comparison of visual quality after SMILE correction of low-to-moderate myopia in different optical zones. Int Ophthalmol. 2023;43(10):3623–3632. doi:10.1007/s10792-023-02771-6
19. Qian Y, Ding L, Ding Y, Jiang L, Liu Z, Zhou X. Measurement of the distance between corneal apex and pupil center in patients following small-incision lenticule extraction or implantable collamer lens implantation and its correlation with the surgical-induced astigmatism. BMC Ophthalmol. 2024;24(1):110. doi:10.1186/s12886-024-03352-6
20. Erdem U, Muftuoglu O, Gundogan FC, Sobaci G, Bayer A. Pupil center shift relative to the coaxially sighted corneal light reflex under natural and pharmacologically dilated conditions. J Refract Surg. 2008;24(5):530–538. doi:10.3928/1081597X-20080501-12
21. Hashemi H, KhabazKhoob M, Yazdani K, Mehravaran S, Jafarzadehpur E, Fotouhi A. Distribution of angle kappa measurements with Orbscan II in a population-based survey. J Refract Surg. 2010;26(12):966–971. doi:10.3928/1081597X-20100114-06
22. Mabed IS, Saad A, Guilbert E, Gatinel D. Measurement of pupil center shift in refractive surgery candidates with caucasian eyes using infrared pupillometry. J Refract Surg. 2014;30(10):694–700. doi:10.3928/1081597X-20140903-07
23. Reinstein DZ, Archer TJ, Rowe EL, Gobbe M, Vida RS. Distribution of pupil offset and angle kappa in a refractive surgery preoperative population of 750 myopic, emmetropic, and hyperopic eyes. J Refract Surg. 2021;37(1):49–58. doi:10.3928/1081597X-20201109-01
24. Guo L, Cheng Z, Kong X, et al. The effect of different angle kappa on higher-order aberrations after small incision lenticule extraction. Lasers Med Sci. 2023;38(1):277. doi:10.1007/s10103-023-03934-8
25. Liu S, Zhang X, You Z, Zhou X. Comparison of the distribution of lenticule decentration following SMILE by pupil center or tear film mark centration. J Refract Surg. 2020;36(4):239–246. doi:10.3928/1081597X-20200310-01
26. Damgaard IB, Ang M, Mahmoud AM, Farook M, Roberts CJ, Mehta JS. Functional optical zone and centration following SMILE and LASIK: a prospective, randomized, contralateral eye study. J Refract Surg. 2019;35(4):230–237. doi:10.3928/1081597X-20190313-01
27. Huang Y, Ding X, Han T, Fu D, Yu Z, Zhou X. Effective optical zone following small incision lenticule extraction for myopia calculated with two novel methods. J Refract Surg. 2022;38(7):414–421. doi:10.3928/1081597X-20220608-02
28. Moshirfar M, Herron MS, Cha DS, Santos JM, Miller LT, Hoopes PC. Correlational analysis of the effective optical zone with myopia, myopic astigmatism, and spherical equivalent in LASIK, PRK, and SMILE. Clin Ophthalmol. 2024;18:377–392. doi:10.2147/OPTH.S440608
29. Holladay JT, Janes JA. Topographic changes in corneal asphericity and effective optical zone after laser in situ keratomileusis. J Cataract Refract Surg. 2002;28(6):942–947. doi:10.1016/s0886-3350(02)01324-x
30. He S, Luo Y, Chen P, et al. Prospective, randomized, contralateral eye comparison of functional optical zone, and visual quality after SMILE and FS-LASIK for high myopia. Transl Vis Sci Technol. 2022;11(2):13. doi:10.1167/tvst.11.2.13
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



