Back to Journals » Clinical Ophthalmology » Volume 18
Evaluation of Intermediate Visual Outcomes in Eyes Implanted with Bilateral Advanced Monofocal Intraocular Lens Targeting for Mini-Monovision and Its Association with Age and Corneal Asphericity
Authors Haldipurkar TS, Haldipurkar S, Venkatramani D, Walavalkar R, Deshpande S, Setia MS
Received 8 August 2024
Accepted for publication 3 October 2024
Published 16 October 2024 Volume 2024:18 Pages 2929—2937
DOI https://doi.org/10.2147/OPTH.S484030
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Tanvi Suhas Haldipurkar, Suhas Haldipurkar, Devendra Venkatramani, Ruta Walavalkar, Sarita Deshpande, Maninder Singh Setia
Laxmi Eye Institute and Laxmi Charitable Trust, Panvel, India
Correspondence: Maninder Singh Setia, Laxmi Eye Institute and Laxmi Charitable Trust, Panvel, Maharashtra, 410206, India, Email [email protected]
Purpose: To assess the visual outcomes in patients bilaterally implanted with novel Clareon® intraocular lens when targeting mini monovision post-operatively.
Setting: The study was conducted at Laxmi Eye Institute; it is a tertiary care eye institution in Panvel, India.
Design: This is an investigator initiated, prospective, single-centre longitudinal study of 45 patients to assess the visual outcomes in patients who were implanted with Clareon ® IOL bilaterally.
Methods: Patients with corneal astigmatism of ≤ 0.75 D who underwent bilateral cataract surgery with pseudophakic mini-monovision and implanted with novel Clareon® intraocular lens were included. Patients having post op manifest refraction >± 0.25 D in the dominant eye and <− 0.5 D or >− 0.75 D in the non-dominant eye were excluded. The main study outcomes were assessed at 1 and 3 months; it included uncorrected visual acuities assessment, defocus curve, and patient reported spectacle use.
Results: The mean (SD) binocular distance corrected intermediate visual acuity at 3 months was 0.22 (0.09) LogMAR. At 3 months, 54% of patients enjoyed 0.4 LogMAR or better BUCNVA. The defocus curve showed good distance and intermediate visual acuity with > 0.2 LogMAR vision from +0.50 D to − 1.50 D. We found a positive correlation between the Q value of the dominant eye and the BCIVA at 3 months postoperatively, however it was not statistically significant. The Q value was more negative when the intermediate vision was closer to 0 LogMAR. Post operatively, at 3 months, 95% patients did not need glasses for distance and intermediate vision and 73% of patients were comfortable for intermediate vision without glasses all the time.
Conclusion: Mini-monovision with Clareon® monofocal IOL implantation can offer overall satisfactory vision for far and intermediate distances with minimal need for use of spectacles for near vision.
Keywords: intermediate vision, monofocal IOLs, mini monovision
Introduction
With the advent of digitalization, visual demands have changed. There is an increasing need for functional vision in the intermediate range, which includes the 40–70-centimeter distance. Conventional monofocal lenses provide excellent uncorrected distance visual acuity, but necessitate the need for spectacles for both near and intermediate ranges. Multifocal intraocular lenses (IOL) can achieve good visual acuity but with the drawbacks of cost, annoying dysphotopsias, and reduced contrast sensitivity. Monofocal lenses combined with the concept of monovision have been successfully used to bridge this gap. This combination has been found to also provide some amount of intermediate vision.1–5
Monovision is achieved by correcting the patient’s dominant eye for distance and non-dominant eye for near to intermediate vision. The image from the dominant eye is preferred for distance activities, and that from the fellow eye for near activities. Traditionally, monovision was achieved by aiming for a residual refractive error of −2.50 D in the non-dominant eye. However, this level of anisometropia is not often tolerable, and stereopsis is substantially impaired. Implanting monofocal IOLs with “mini” monovision helps to reduce this intolerance. In mini monovision, the target anisometropia is to the order of −0.5 D to −1.50 D. This yields good distance and intermediate vision with reduced spectacle dependence, while near tasks may still need use of spectacles. Implanting a monofocal lens lessens the economic burden and has a low dysphotopsia profile.6–10
The Clareon® monofocal (CNAOT0; Alcon; Texas, USA) intraocular lens is a monofocal aspheric hydrophobic acrylic IOL. Previous studies have demonstrated good distance vision with this IOL. However, there have been no reports describing the effectiveness of the Clareon® IOL for intermediate vision.11–15
The cornea has a natural asphericity, which is represented by the Q value. The Q value of each cornea represents its shape and optical properties including refractive power, spherical aberration, aberration distribution, etc. Change in the Q value seems to have an effect on the spherical aberration, which in turn may affect the depth of focus for the individual eye. A pre-existing spherical aberration can improve the intermediate visual acuity in an eye implanted with an aspheric monofocal lens.16–19As the Clareon® IOL (having −0.2 of spherical aberration) aims to partly correct the spherical aberrations of the cornea (+0.27) leaving behind some positive spherical aberration, we wanted to observe if there was any relation of improved intermediate visual acuity with different preoperative Q value.
The correlation between age and binocular intermediate visual acuity in conventional monovision has been observed in some studies. In another study by Hayashi et al, with eyes targeted for a modified monovision outcome, they found that younger age was significantly correlated with better binocular intermediate visual acuity postoperatively.7,20
The primary study objective was to evaluate binocular uncorrected intermediate visual acuity (BUCIVA) at 3 months postoperatively. While the secondary study objectives were to evaluate the association of intermediate vision with age and corneal asphericity, binocular uncorrected distance visual acuity (BUCDVA), binocular uncorrected near visual acuity (BUCNVA), binocular distance corrected visual acuity (BDCVA), binocular uncorrected defocus curve (+0.50 to −2.50D) and PRSIQ (Patient reported spectacle independence questionnaire) score.
Methods
We performed a prospective, single-centre longitudinal study of 90 eyes (of 45 patients) at Laxmi Eye Hospital & Institute, Panvel, India. The aim was to evaluate the intermediate visual performance of the Clareon monofocal IOL when implanted bilaterally in patients while targeting them for mini-monovision post-operatively.
Study Population
We included patients aged between 40 and 90 years, with uncomplicated age-related cataract having a preoperative astigmatism <0.75 D. They underwent phacoemulsification with implantation of the Clareon® monofocal IOL (CNAOT0; Alcon; Texas, USA) while targeting their dominant eye for emmetropia and their non-dominant eye for −0.50D of myopia. Patients were excluded from the study if they had any underlying ocular pathology that would affect visual function (eg macular degeneration, glaucoma, epiretinal membrane, amblyopia, diabetic eye disease, etc), experienced intra or postoperative complications, or had postoperative refractive error where the spherical equivalent >0.25D in the dominant eye and ≥0.75 D in the non-dominant eye.
Study Procedure
Preoperative Assessment
All included patients underwent a comprehensive preoperative ophthalmic examination. This included measurement of visual acuity using LogMAR visual acuity chart, manifest refraction, slit-lamp biomicroscopy to assess grades of cataract, and dilated retinal examination. Preoperative anterior corneal surface asphericity (Q-values) was obtained from Pentacam tomography (Pentacam Comprehensive Eye Scanner; Oculus Optikgeraete GmbH Wetzlar, Germany) while ocular parameters required for IOL power calculation (such as keratometry readings, axial length and optical anterior chamber depth) were measured using optical biometry (Lenstar 900; Haag Streit USA).
Intra Operative Procedures
The surgeries were performed by a single surgeon, where in routine phacoemulsification and in-the-bag implantation of a Clareon® monofocal IOL (CNAOT0; Alcon; Texas, USA) was performed for each patient. The IOL power was selected based on the predicted postoperative spherical equivalent using Barrett II formula while keeping a target refraction of plano for the dominant eye and −0.5D for the non-dominant eye (mini monovision). The procedures were performed under topical anesthesia using proparacaine hydrochloride (0.5%). Phacoemulsification was done using Centurion® Vision System by Alcon Vision LLC, Fort Worth, Texas, USA.
Postoperatively anti-inflammatory steroid eye drops were prescribed in a tapering dose for 6 weeks and antibiotic eye drops were prescribed for a week. Patients were monitored for any postoperative complications.
Postoperative Assessments
The postoperative assessments for the study were done at 1 month (± 7 days) post surgery and 3 months (±15 days) after surgery. It included measurement of binocular visual acuity, plotting of defocus curve and patients’ response on the Patient-Reported Spectacle Independence Questionnaire (PRSIQ) was obtained.
Uncorrected binocular visual acuity was measured postoperatively using ETDRS Charts at 3 distances − 6 meters (for distance), 70 cm (for intermediate) and 40 cm (for near), while distance corrected binocular visual acuity was measured 70 cm (for intermediate) and 40 cm (for near) at 1 month and 3 months. Defocus curves of binocular uncorrected acuity measured at distances of 6 meters were also plotted at 1 month and 3 months.
Patients were administered the PRSIQ for everyday activities (at distance, intermediate, and near distances) to gauge their spectacle independence. The patients were asked three questions which mainly assessed their need for glasses for distance vision, intermediate vision and near vision, how often the patients required to wear glasses for the three distances, and whether they were able to function comfortably without glasses for the three distances. The score was recorded as a yes or no for the first question and the spectacle dependence was recorded in a scale of 1–5 as shown in Figure 1, with score 1 for “All of the time” and score 5 for “None of the time”. For the purposes of analysis, scores 1 and 2 (“All of the time” and “Most of the time”) were classified as “Frequently”; scores 3 and 4 (“Some of the time” and “A little of the time”) were classified as ‘Occasionally’ and score 5 was considered as ‘Never’.
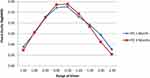 |
Figure 1 Figure showing the binocular defocus curve at one and three months. |
Statistical Analyses
All statistical analyses were performed using Stata version 17 (© StataCorp, College Station, Texas, USA). We estimated the means and standard deviations for continuous variables and proportions for categorical variables. The means were compared using the unpaired and paired t-test (for two group and paired data). The proportions across groups were compared using the chi-square test or Fisher’s exact test for low expected cell counts. The answers to each question on the patient questionnaire were calculated as a percentage. We estimated the Pearson’s correlation co-efficient (r) for two linear variables. A p value of <0.05 was considered statistically significant.
Ethics and CTRI Number
The study was approved by the Institutional Ethics Committee of Laxmi Eye Institute and Laxmi Charitable Trust (Reference No: EC/001/2022; Date: 21 January 2022). All the participants provided written informed consent prior to participation in the study. The study was registered with Clinical Trials Registry – India (CTRI) (CTRI/2022/06/043199). The study was conducted in accordance with the Declaration of Helsinki and International Good Clinical Practices Guidelines.
Results
The proportion of patients in the age group of 45–64 years was 53.3% (n = 24) and those ≥65 years was 46.7% (n = 21). In our study, 46.7% were male (n = 21) and 53.3% (n = 24) were female. We also found that the dominant eye was the right eye in 73.3% (n = 33) and left eye in 26.7% (n = 12) of the participants. The study population had a uniform distribution in gender as well as age. The refractive status is shown in Table 1.
 |
Table 1 Table Showing the Refractive Status in Patients Implanted with Clareon® Intraocular Lens, Panvel, India |
The dominant eye was targeted close to emmetropia with a mean predicted residual error of −0.15D ± 0.16. The postoperative Mean Residual Spherical Equivalent (MRSE) achieved for the dominant eye in the study was −0.13D ± 0.25. The non-dominant eye was targeted for slight myopia while keeping the monovision in view, and the mean predicted residual error was −0.47D ± 0.17. The MRSE achieved postoperatively at 3 months for the non-dominant eye was −0.26D ± 0.29.
The binocular corrected and uncorrected visual acuity (LogMAR) at 1 month and 3 months is shown in Table 2. The postoperative vision at 1 month and 3 months was not statistically different. The mean binocular uncorrected distance visual acuity (BUCDVA) (SD) was 0.03 (0.12), and the binocular uncorrected intermediate vision (BUCIVA) was 0.23 (0.12) both showing a satisfactory visual outcome for distance and intermediate vision range for the patient’s daily routine.
 |
Table 2 Table Showing the Binocular Uncorrected and Corrected Visual Acuity in Patients Implanted w |
In our study population, 68% of patients had BUCIVA of 0.2 LogMAR or better at 3 months postoperatively. The binocular distance corrected intermediate visual acuity (BDCIVA) (SD) at 3 months was 0.22 (0.09). At 3 months postoperatively, 68% of patients had 0.2 LogMAR BDCIVA or better, which showed that even after correcting for distance, intermediate vision remained decent in most patients. The binocular uncorrected near visual acuity (BUCNVA) in LogMAR at 1 month (0.42) and at 3 months (0.43) postoperatively were similar with an inter-quartile range of 0.4–0.5. At 3 months, 54% of patients enjoyed 0.4 LogMAR or better BUCNVA.
Figure 1 shows the Binocular Defocus curve at 1 month and 3 months postoperatively. The visual acuity with a defocus of −1.0 D (corresponding to intermediate range vision at 1 m) was nearly 0.1 LogMAR. The defocus curve was better at 3 months compared to 1 month, but the difference was not statistically significant.
The study patients underwent the PRSIQ “Patient Reported Spectacle Independence Questionnaire”.
The analysis of PRSIQ responses at 3 months postoperatively (Table 3) shows that 95% of the patients did not need glasses for distance and intermediate vision and 41% of patients did not need glasses for near vision work. When asked how often they wore glasses for intermediate vision, 51% of the patients reported that they did not wear glasses all day, while 41% wore it for occasional use. We found that 91% of patients could manage their daily activity at intermediate vision without the need for glasses. When asked if they were able to function comfortably without glasses for distance, intermediate and near work, 73% of patients were comfortable for intermediate vision without glasses all the time and an additional 16% patients were comfortable without glasses most of the time.
 |
Table 3 Table Showing the Response to Patient-Reported Spectacle Independence Questionnaire (PRISQ) in Patients Implanted with Clareon® Intraocular Lens, Panvel, India |
For analysis, we sub-grouped the study population by age and gender (Table 4). The requirement for glasses for intermediate vision appeared to be lower in the younger age group (45–64 years) compared to older patients (>65 years). The mean (SD) BUCIVA was better in the lower age group (45–64 years) as compared to the older patients (>65 years), however the difference was not statistically significant (p = 0.32).
 |
Table 4 Table Showing the Binocular Uncorrected Intermediate Visual Acuity (IVA) According to Age in Patients Implanted with Clareon® Intraocular Lens, Panvel, India |
We also looked at the asphericity of the cornea in the study population. The mean Q value (SD) in patients having <0.2 LogMAR intermediate vision in the dominant eye was −0.22 (0.16) and in the non-dominant eye was −0.19 (0.24). The mean Q value in patients having >0.2 LogMAR intermediate vision was −0.19 (0.15) in the dominant eye and −0.20 (0.17) in the non-dominant eye. The mean Q value in the dominant eye was more negative in patients having BUCIVA better than 0.2 LogMAR compared with those having BUCIVA worse than 0.2 LogMAR, the difference was not statistically significant (p = 0.64). Similarly, the Q value was not statistically different in both these groups for the non-dominant eye. We may need a larger sample size to assess for any correlation between the two.
There was a positive correlation between the Q value of the dominant eye and BUCIVA at 3 months; however, the correlation was not statistically significant (r = 0.23; p = 0.20) (Figure 2). The Q value was more negative when the vision was closer to 0 LogMAR.
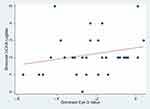 |
Figure 2 Scatter plot between the Q value of the dominant eye and bilateral uncorrected intermediate visual acuity (BUCIVALogMAR). |
Discussion
Binocular implantation of the Clareon IOL with a mini monovision concept seems to give a good distance and functional intermediate visual acuity in majority of patients. The mean BUCIVA achieved in the study population was 0.20 LogMAR and it remained similar even after correcting the patients for distance. We also found that the BUCIVA for distance and intermediate is stable over a period of 3 months postoperatively.
The defocus curve for the IOL showed a wide and smooth curve suggesting a good intermediate vision for a range of activities in the 30 cm to 60 cm distance. This is, however, an objective assessment and may not always correlate with patient comfort. Hence, we additionally studied patients’ self-reported comfort without, and need, for spectacles at different working distances. The spectacle independence score showed that most patients did not need glasses for distance and intermediate vision tasks. The frequency of wearing glasses was least for distance activities followed very closely by intermediate range tasks. The comfort without glasses was high for tasks in the 45 cm to 150 cm range and a large majority of patients were spectacle independent.
Intermediate range vision appears to vary depending on the patient’s age. Subgroup analysis dividing the patients into younger (age 45–64 years) and older (>65 years) showed better results among younger patients. The mean (SD) BUCIVA was better in the lower age group (45–64 years) as compared to the older patients (>65 years), however the difference was not statistically significant (p = 0.32). The proportion of younger patients who needed glasses for intermediate vision was slightly lower compared to the older patients; similarly, the proportion of younger patients who never wore glasses for intermediate vision was more as compared to the older population. All the younger age group patients were comfortable without glasses for intermediate vision, while the older age group had more patients needing glasses for intermediate vision occasionally or all the time. While our study was not powered to measure these differences, this may be an area for further study.
A functional intermediate vision that correlates with a 0.2 LogMAR or better vision is required for most routine activities like using a mobile phone, grocery shopping or driving.21–23 We tried to determine a cut-off value for intermediate visual acuity that correlated with spectacle independence for this distance. Our post-hoc analysis showed that no patient with BUCIVA<0.2 LogMAR needed glasses, compared to those with BUCIVA >0.2 LogMAR. Similarly, the proportion of patients who “never wore glasses for intermediate vision” was higher in those with BUCIVA <0.2 LogMAR. This group also reported that they were more frequently comfortable without glasses for intermediate vision. These results were, however, not statistically significant.
There are studies that have reported acceptable spectacle independence with mini monovision approach with monofocal IOLs (hydrophobic acrylic IOL (ZCB00), aspheric IOLs (AcrySof®IQIOL)), and enhanced IOLs (Tecnis Eyhance (ICB00) IOLs), where targeted residual myopia ranged from −0.75 Diopters to −1.75 Diopters.5,24 However, in our study, some patients attained good binocular distance and intermediate vision in spite of not achieving the targeted myopic residual (−0.50 D) for the monovision, which may be attributed to the aspheric IOL (−0.20) which only partly corrected the corneal positive spherical aberration. The binocular intermediate visual acuity remained similar even after correcting the patients for distance, and the proportion of patients who had visual acuity 0.2 LogMAR or better was largely unchanged. This showed that the patient may still get good functional intermediate vision even with a mini monovision target.3,5,7,10,25,26
Patients with good postoperative binocular intermediate visual acuity (0–0.20 LogMAR) had a mean Q value of −0.22 in dominant eye and −0.19 in non-dominant eye. The negative asphericity of the cornea was associated with better intermediate vision and this is an aspect that needs further study. The novelty of this study is its unique approach in exploring the relationship between corneal asphericity and intermediate vision in mini monovision that has not been examined together in any previous research.1–5
Conclusion
Minimonovision with Clareon® monofocal IOL implantation can provide overall satisfactory vision for far and intermediate distances. Spectacles would be required for most near activities. Patients implanted with this IOL using this approach had high self-reported levels of satisfaction, along with substantial reduction in spectacle dependence. The Q value may act as a preoperative biomarker to determine which patients would benefit from this approach.
Statement about the authors’ proprietary or financial interest in a product or lack thereof
The authors have no financial or proprietary interest in a product, method, or material described herein.
Funding
The study was funded by a research grant from Alcon # 69782731.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zhang F, Sugar A, Jacobsen G, Collins M. Visual function and patient satisfaction: comparison between bilateral diffractive multifocal intraocular lenses and monovision pseudophakia. J Cataract Refract Surg. 2011;37(3):446–453. doi:10.1016/j.jcrs.2010.10.045
2. Greenbaum S. Monovision pseudophakia. J Cataract Refract Surg. 2002;28(8):1439–1443. doi:10.1016/S0886-3350(02)01218-X
3. Goldberg DG, Goldberg MH, Shah R, Meagher JN, Ailani H. Pseudophakic mini-monovision: high patient satisfaction, reduced spectacle dependence, and low cost. BMC Ophthalmol. 2018;18(1):293. doi:10.1186/s12886-018-0963-3
4. Zettl S, Reiß S, Terwee T, Guthoff R, Beck R, Stachs O. Der Effekt der pseudophaken Minimonovision als Option einer Brillenunabhängigkeit im Alltag. Klin Monatsblätter Für Augen. 2014;231(12):1196–1202. doi:10.1055/s-0034-1383367
5. Park ES, Ahn H, Han SU, et al. Visual outcomes, spectacle Independence, and patient satisfaction of pseudophakic mini-monovision using a new monofocal intraocular lens. Sci Rep. 2022;12(1):21716. doi:10.1038/s41598-022-26315-7
6. Hayashi K, Yoshida M, Ichi MS, Hayashi H. Optimal Amount of Anisometropia for Pseudophakic Monovision. J Refract Surg. 2011;27(5):332–338. doi:10.3928/1081597X-20100817-01
7. Hayashi K, Ogawa S, Manabe SI, Yoshimura K. Binocular Visual Function of Modified Pseudophakic Monovision. Am J Ophthalmol. 2015;159(2):232–240. doi:10.1016/j.ajo.2014.10.023
8. Evans BJW. Monovision: a review. Ophthalmic Physiol Opt. 2007;27(5):417–439. doi:10.1111/j.1475-1313.2007.00488.x
9. Abdelrazek Hafez T, Helaly HA. Spectacle Independence And Patient Satisfaction With Pseudophakic Mini-Monovision Using Aberration-Free Intraocular Lens. Clin Ophthalmol. 2019;13:2111–2117. doi:10.2147/OPTH.S215229
10. Greenstein S, Pineda R. The Quest for Spectacle Independence: a Comparison of Multifocal Intraocular Lens Implants and Pseudophakic Monovision for Patients with Presbyopia. Semin Ophthalmol. 2017;32(1):111–115. doi:10.1080/08820538.2016.1228400
11. Auffarth GU, Fang H, Wang Q, et al. Silicone Oil Adhesion to Hydrophobic Acrylic Intraocular Lenses: a Comparative Laboratory Study of a New versus an Established Hydrophobic Acrylic Intraocular Lens Material. J Ophthalmol. 2021. 1–6. doi:10.1155/2021/1387987
12. Ukai Y, Okemoto H, Seki Y, et al. Quantitative assessment of photic phenomena in the presbyopia-correcting intraocular lens. PLoS One. 2021;16(12):e0260406. doi:10.1371/journal.pone.0260406
13. Lehmann R, Maxwell A, Lubeck DM, Fong R, Walters TR, Fakadej A. Effectiveness and Safety of the Clareon Monofocal Intraocular Lens: outcomes from a 12-Month Single-Arm Clinical Study in a Large Sample. Clin Ophthalmol. 2021;15:1647–1657. doi:10.2147/OPTH.S295008
14. Walters TR, Lehmann R, Moyes A, French JW, Sreenivasan V, Modi SS. Rotational Stability of the Clareon Monofocal Aspheric Hydrophobic Acrylic Intraocular Lens 6 Months After Implantation. Clin Ophthalmol. 2022;16:401–409. doi:10.2147/OPTH.S348551
15. Titiyal JS, Basak SK, Shetty N, et al. Twelve-Months Follow-Up Postmarket Study of a Hydrophobic Intraocular Lens Using a Preloaded Automated Injector in an Indian Population. Clin Ophthalmol. 2022;16:4215–4225. doi:10.2147/OPTH.S379054
16. Gatinel D, Haouat M, Hoang-Xuan T. Etude des paramètres permettant la description mathématique de l’asphéricite cornéenne [A review of mathematical descriptors of corneal asphericity]. J Fr Ophtalmol. 2001;25(1):81–90.
17. Queirós A, Villa-Collar C, Jorge J, Ár G, González-Méijome JM. Multi-aspheric description of the myopic cornea after different refractive treatments and its correlation with corneal higher order aberrations. J Optom. 2012;5(4):171–181. doi:10.1016/j.optom.2012.08.002
18. Savini G, Hoffer KJ, Barboni P. Influence of corneal asphericity on the refractive outcome of intraocular lens implantation in cataract surgery. J Cataract Refract Surg. 2015;41(4):785–789. doi:10.1016/j.jcrs.2014.07.035
19. Savini G, Hoffer KJ, Barboni P, Schiano Lomoriello D, Ducoli P. Corneal Asphericity and IOL Power Calculation in Eyes With Aspherical IOLs. J Refract Surg. 2017;33(7):476–481. doi:10.3928/1081597X-20170504-05
20. Labiris G, Toli A, Perente A, Ntonti P, Kozobolis VP. A systematic review of pseudophakic monovision for presbyopia correction. Int J Ophthalmol. 2017;10(6):992–1000. doi:10.18240/ijo.2017.06.24
21. Elliott DB, Hotchkiss J, Scally AJ, Foster R, Buckley JG. Intermediate addition multifocals provide safe stair ambulation with adequate ‘short-term’ reading. Ophthalmic Physiol Opt. 2016;36(1):60–68. doi:10.1111/opo.12236
22. Podborączyńska-Jodko K, Lubiński W, Post M. Intermediate vision and other visual function parameters in patients after uneventful cataract surgery with implantation of diffractive intraocular lenses using the blending procedure. Klin Oczna. 2020;122(2):49–53. doi:10.5114/ko.2020.96556
23. Micheletti JM, McCauley MB, Duncan N, Hall B. Biometric Indicators for Maximizing Intermediate Vision with a Monofocal IOL. Clin Ophthalmol. 2023;17:3739–3746. doi:10.2147/OPTH.S441172
24. Beltraminelli T, Rizzato A, Toniolo K, Galli A, Menghini M. Comparison of visual performances of enhanced monofocal versus standard monofocal IOLs in a mini-monovision approach. BMC Ophthalmol. 2023;23(1):170. doi:10.1186/s12886-023-02920-6
25. Rocha KM, Soriano ES, Chamon W, Chalita MR, Nosé W. Spherical aberration and depth of focus in eyes implanted with aspheric and spherical intraocular lenses: a prospective randomized study. Ophthalmology. 2007;114(11):2050–2054. doi:10.1016/j.ophtha.2007.01.024
26. Yi F, Iskander DR, Collins M. Depth of focus and visual acuity with primary and secondary spherical aberration. Vision Res. 2011;51(14):1648–1658. doi:10.1016/j.visres.2011.05.006
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

