Back to Journals » Journal of Asthma and Allergy » Volume 18
Evaluation of Real-World Quality of Asthma Care According to the Spanish Consensus Protocol: The AsmaNET Project (ESR-20-20897)
Authors Dominguez-Ortega J , Narváez-Fernández E , Ramos J , Cancelliere N, García-Criado J , Sanchez-Ocando H, Gallardo-Higueras A , Dávila I
Received 5 March 2025
Accepted for publication 25 June 2025
Published 17 July 2025 Volume 2025:18 Pages 1119—1127
DOI https://doi.org/10.2147/JAA.S526389
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Luis Garcia-Marcos
Javier Dominguez-Ortega,1,2 Emilio Narváez-Fernández,1 Jacinto Ramos,3 Nataly Cancelliere,4 Jorge García-Criado,5 Humberto Sanchez-Ocando,1 Alicia Gallardo-Higueras,6 Ignacio Dávila6,7
1Department of Allergy, Hospital Universitario La Paz, Madrid, Spain; 2Institute for Health Research, IdiPAZ, Madrid, Spain; 3Pulmonology Service, University Hospital of Salamanca, Salamanca, Spain; 4Department of Emergency Medicine, Hospital Universitario La Paz, Madrid, Spain; 5Department of Emergency Medicine, University Hospital of Salamanca, Salamanca, Spain; 6Allergy Service, University Hospital of Salamanca, Salamanca, Spain; 7Department of Biomedical and Diagnosis Sciences, Faculty of Medicine, University of Salamanca, IBSAL, Salamanca, Spain
Correspondence: Javier Dominguez-Ortega, Department of Allergy, Hospital Universitario La Paz, Paseo de la Castellana 261, Madrid, 28046, Spain, Email [email protected]
Background: The emergency room (ER) approach for patients with asthma exacerbations (AEs) should be based on a comprehensive, multidisciplinary approach to ensure effective and timely care. This study aims to analyze the compliance level of recommended indicators, as defined in a consensus document, for the management of AEs in the ER using available electronic medical records.
Methods: An open-label, observational, non-interventional, retrospective study of adult patients treated in hospital ER for AEs was conducted at La Paz University Hospital and Salamanca University Hospital. Data were collected from medical records regarding a set of predefined measures and variables concerning asthma severity, ER stay, and subsequent discharge.
Results: During 2019, a total of 1,019 patients accounted for 1,089 AEs were evaluated. Clinical variables predominantly included historical data, such as previous hospitalizations, Intensive Care Unit admissions, and prior exacerbations, which were recorded in 45.8% of medical records. Auscultation details were extensively documented (99.8%), yet respiratory rate (25.4%) and spirometry (less than 10%) were notably lower. Regarding discharge planning, 69.6% of patients had a defined care plan, and 59.5% received Inhaled Corticosteroids plus Long-Acting Beta-Agonists combination treatment at discharge. Medical referrals resulted in 25.5% being referred for specialized care and 87.2% to primary care. 13.3% had a specific post-discharge care timeframe.
Conclusion: This study highlights significant variability in the documentation and adherence to recommended indicators for AE management in the ER. Moreover, discharge planning and follow-up care were suboptimal. These findings underscore the need for improved standardization and implementation of evidence-based protocols in emergency asthma care.
Keywords: asthma exacerbation, emergency room management, electronic medical records, quality indicators
Introduction
Asthma is one of the most prevalent chronic respiratory diseases worldwide, characterized by inflammation and constriction of the airways, can lead to irreversible airflow obstruction.1 The prevalence is increasing; in Spain, it affects approximately 6% of adults and around 10% of children.2
Regardless of the severity level, all asthmatics are susceptible to experiencing exacerbations.3 Asthma exacerbations (AEs) manifest as acute episodes characterized by worsening respiratory symptoms in patients with this chronic disease. These exacerbations frequently result in a progressive decline in lung function over time and significantly impact patients’ quality of life, leading to hospitalizations and an increased risk of asthma-related morbidity and mortality.4,5 Moreover, cost-of-illness studies focusing on asthma suggest that AEs impose a substantial economic burden.6–8
Existing literature has identified several risk factors that can contribute to AEs,1,2,9–11and for hospitalization,12 including clinical, lung function, and inflammatory outcomes and a very high T2-inflammatory pattern.13 Understanding these contributing factors is crucial for improving appropriate treatment and comprehensive follow-up care for individuals experiencing AEs.14
The emergency room (ER) approach for patients with AEs should be based on a comprehensive, multidisciplinary approach to ensure effective and timely care. This strategy is guided by established clinical guidelines and recommendations.1–3,15 It begins with a rapid evaluation and is followed by administration of bronchodilators and systemic corticosteroids. In severe cases, non-invasive ventilation techniques or endotracheal intubation are considered. Identifying and avoiding triggers is also an essential aspect of the approach. Moreover, at discharge, patients should receive education on proper disease management, and regular follow-ups with the treating physician should be scheduled to assess treatment response and make necessary adjustments to therapy.1–3
Recently, the Spanish medical societies for Allergy, Pulmonology, and Emergency Medicine developed a consensus document on the management of adverse events (AEs). A multidisciplinary team created a list of clinical questions and selected four clinical practice guidelines on asthma management. Their recommendations and clinical algorithms in the statement focused on how to detect the asthmatic patient on arrival at the emergency department, to establish the diagnosis and etiology of the AE, to follow unified treatment criteria, and, finally, criteria for hospitalization or for referring the patient to a respiratory medicine specialist, an allergy specialist, or a primary care physician, as appropriate. A set of indicators was recommended for inclusion in the clinical history taken in the ER,16 (Table S1). However, these indicators still required validation in a real-world setting.
The AsmaNET project was designed to analyze the compliance level of recommended indicators, as defined in the consensus document, for the management of AEs in the ER using available electronic medical records (MR). By conducting this analysis, we seek to evaluate the extent to which healthcare providers adhere to the recommended guidelines and identify potential areas for improvement in asthma care. Understanding the level of compliance can help to identify gaps in care delivery, inform quality improvement initiatives, and ultimately enhance patient outcomes. The findings obtained from this study can provide valuable insights for implementing and refining the protocol in future studies and daily clinical practice.
Materials and Methods
Study Design, Setting, and Patient Population
This was an open-label, observational, non-interventional, retrospective study of adult patients treated in hospital ER for AEs. It was conducted at La Paz University Hospital (HULP), a 1,200-bed tertiary referral center for more than 530,000 inhabitants in northern Madrid (www.madrid.org), and at Salamanca University Hospital (HUS), a 1,103-bed tertiary hospital in Salamanca (327,685 inhabitants in 2024 according to the Governmental Spanish National Registry, (www.ine.es). A protocol was developed, and the two Clinical Research Ethics Committees approved the study, and it was conducted in compliance with the Declaration of Helsinki. As a retrospective, anonymized, and non-interventional study, there was no need to obtain informed consent from any patient. We obtained authorization from both hospital administrations.
Eligible patients were patients older than 18 years evaluated in the ED for an acute asthma exacerbation between January 1 and December 31, 2019. Data were collected by two trained researchers at each site following a standardized protocol to minimize variability from patients’ electronic medical records (MR) identified based on the inclusion criteria. A specific search was performed following any of the International Statistical Classification of Diseases and Related Health Problems 9th Revision (ICD−9-CM) codes for asthma (493; 493.0; 493.1; 493.2; 493.8; and 493.9),17 and a supplementary search was later performed following other possible and noncoded diagnoses, namely, bronchial asthma, asthmatic bronchitis, asthmatic crisis, acute asthma attack, and asthma exacerbation. Events in which chronic obstructive pulmonary disease (COPD) or COPD exacerbation was mentioned as a possible cause for the ED visit were excluded. An isolated diagnosis of pneumonia was also excluded. Data were mainly obtained from the discharge ED reports, hospitalization reports, admission reports, or other electronic clinical records if needed. Data were only accessible to hospital-authorized personnel from both hospitals and were compiled in a Microsoft Access anonymized database for subsequent analysis. Traceability was guaranteed as any change in the records was associated with the researcher’s signature that made modifications.
Objectives
The following objectives were defined for the evaluation of the different measures and variables considered in this study:
Primary Objective
To analyze the degree of compliance with the quality indicators described in the multidisciplinary consensus document16 for patients with AEs attended in the ER of both hospitals.
Secondary Objectives
These objectives align with the quality indicators established in the consensus document to explore the degree of adherence to each of the consensus recommendations:16 Table S1 shows the quality indicators described in the multidisciplinary consensus document.
- The percentage of patients who underwent spirometry or peak flow measurement in the ER.
- The percentage of patients with medical records that inquire about the trigger of the crisis.
- Percentage of patients with medical records documenting previous asthmatic crises.
- Percentage of patients with a discharge treatment plan.
- Percentage of patients treated for asthmatic crisis who required a hospital admission.
- Percentage of patients returning to the ER within one week after discharge following an asthma crisis.
- Percentage of patients with a prescription for ICS (Inhaled corticosteroids) upon discharge from the ER.
- Percentage of patients referred to specialized care (SC) within one month with general referral criteria.
- Percentage of patients referred to SC within two weeks with priority referral criteria.
- Percentage of patients receiving ICS/LABA (long-acting beta(2)-agonist) upon discharge.
Exploratory Objective
Since the two hospitals included in the study serve populations in markedly different settings, an exploratory objective was included to compare the management of asthma exacerbations between the two hospitals to identify potential differences that could inform context-specific strategies for care improvement.
Measurements
According to the purpose of the ASMANET project, key variables included patients’ asthma historical data encompassing previous hospitalizations, prior admissions to the Intensive Care Unit, and prior exacerbations. Moreover, data regarding identified triggers of exacerbation and diagnostic procedures performed in the emergency room, as well as exacerbation treatment, were also observed. Treatment at discharge, including systemic glucocorticoids, ICS/LABA regimens, and care plans, were also recorded. Post-discharge outcomes, including referral to specialized care, waiting times, and ER reattendance within one week, were evaluated to assess continuity and quality of care. Table S2 shows the defined measures and variables.
Statistical Analysis
Continuous variables were described by their average, with a 95% confidence interval, median, 25 and 75 percentiles, standard deviation, and range. As most of the results are presented as frequencies and percentages, confidence intervals were not systematically applied. Discrete variables were presented as the distribution of frequencies and percentages. Comparisons were performed through bilateral tests, and statistical significance was set at a p-value < 0.05. We performed comparisons among two or more previously defined groups for discrete variable analysis using Pearson’s chi-square test or Fisher’s exact test, depending on the characteristics of each variable. Depending on the distribution of the data, assessed using normality tests, parametric analyses were conducted using the t-test. Non-parametric alternatives, such as the Mann–Whitney U-test or Kruskal–Wallis test, were applied when the assumptions for parametric testing were not met. In this study, missing values were reported descriptively and excluded from the corresponding analyses without imputation, given the observational and retrospective design of the study. We used SAS 9.3 (SAS Institute Inc., Cary, NC, USA) for data analysis.
Results
Global results
During 2019, a total of 1,019 patients, accounting for 1,089 adverse events (AEs), were evaluated. Nine hundred sixty-three patients had one crisis, 47 patients had 2, 6 patients had 3, 2 patients had 4, and 1 patient had 6. Of the 1,089 AEs, 64.4% (n=701) occurred at HULP and 35.6% (n=388) at HUS.
Clinical Variables Recorded in Medical History
The percentage of episodes with clinical variables recorded in patients’ MR in both centers are summarized in Figure 1. Globally, 45.8% of MR contained information regarding previous history of asthma and prior treatment. In 68.9% of the evaluated records, the cause of exacerbation was elucidated. Pulmonary auscultation was extensively documented, with a recording rate of 99.8%.
In contrast, the respiratory rate as available only for 25.4% of the patients. Heart rate was recorded in 97.1% of them. Other essential procedures recorded during the ED stay are presented in Figure 2. Remarkably, Peak Expiratory Flow and spirometry were performed in less than 5 and 10% of patients, respectively.
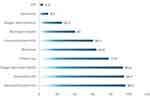 |
Figure 2 Percentages of procedures recorded on patients during the ED stay. |
The aspects related to patient management and discharge planning are presented in Figure 3. Regarding the discharge action plan, 69.6% of patients had a defined care plan in place after leaving the hospital. Regarding treatment, only 59.5% of patients had a record of an ICS-LABA combination at the time of discharge. Regarding medical referrals, 25.5% of patients were directed to specialists for additional medical care. Additionally, 87.2% of patients were referred to primary care, but only 13.3% had a defined time frame for post-discharge care.
Comparative Analysis Between Hospitals
Table 1 revealed the comparison data between HULP and HUS. Several statistically significant differences in various categories suggested potential variations in diagnostic and treatment approaches between the two hospitals. Only three items had at least 30% of registers in both hospitals (previous asthma diagnosis, previous treatment, and eosinophil counts). Registration for the remaining outcomes was overall deficient. Generally, data relative to anamnesis were better collected at the HUS, whereas specific techniques evaluating lung function showed higher percentages at the HULP. Thus, asking for a previous history of asthma was significantly higher in HUS (68.8%) than in HULP (32.9%). Previous treatment also exhibited a significant disparity, with 31.7% of patients recorded at HULP and 71.1% at HUS. The analysis revealed several statistically significant findings with a p-value <0.05. First, a significantly higher proportion of patients with previous asthma were recorded at HUS (68.8%) compared to HULP (32.9%), indicating a notable difference between the two (p < 0.001). Additionally, the percentage of recorded diagnosis dates significantly differed between the two hospitals, with HULP reporting an 8.0% rate compared to 4.1% at HUS (p = 0.015). Disease severity (p = 0.034), disease phenotype (p < 0.001), previous treatment (p < 0.001), spirometry results (p < 0.001), PEF values (p < 0.001), previous exacerbations (p < 0.001), hospitalizations in the previous year (p < 0.001), and previous emergency visits (p < 0.001) also showed statistically significant differences between the two hospitals. However, eosinophil counts (cells/mm3) (p = 0.651), eosinophil percentages (p = 0.727), and neutrophils (cells/mm3) (p = 0.212) did not exhibit significant differences between the two hospitals.
 |
Table 1 Comparative Analysis of Recorded Items Between Hospitals |
Discussion
In this study, we have observed that there are important gaps in the clinical data registered in the MR of asthmatic patients with an AE, particularly regarding variables that are highly relevant for the management, such as asthma severity, date of diagnosis, and patient phenotype or even more relevant since is a risk factor for future exacerbations, previous exacerbations in the last year (only 19,4%). Few studies have conducted this type of assessment in clinical practice for asthma. Although most healthcare professionals understand the nature, symptoms, and diagnoses of asthma disease and have quite a high knowledge of GINA guidelines, it could be a lack of adherence, awareness, and understanding of the recommendations in real-life settings18 The present study delves into the comprehensive assessment of AEs in two Spanish hospitals during the year 2019 to evaluate the real-world compliance level to the quality indicators outlined in the Spanish Consensus Document for managing AE in the ER16 using available electronic MR. However, the literature demonstrates an improvement in patient care quality and outcomes when adherence to the recommendations outlined in clinical practice guidelines is observed.19 Additionally, current attention toward managing asthma exacerbations focuses on adequately characterizing different types of exacerbations.20 Nevertheless, this task becomes challenging in real life due to a lack of documented patient clinical information, history data, physical examinations, and complementary tests.
The analysis in the present study provides a detailed account of the clinical characteristics of patients who experienced these exacerbations. We observed disparities in data collection practices, diagnostic techniques, and therapeutic approaches between the two hospitals, shedding light on potential variations in their management of asthma exacerbations.
The variables collected for evaluation were part of those indicators highlighted and essential in the Consensus Document, also considering GINA recommendations for the initial approach of patients with AEs arriving at the ER.1,16 The results, categorized into several key aspects, including patient history, physical examination variables (eg, respiratory rate, heart rate), pulmonary function tests, oxygenation evaluation, and discharge planning, offer a valuable snapshot of the clinical landscape.
Spirometry or Peak Expiratory Flow
Variables such as Peak Exploratory Flow recording are essential for the initial assessment of asthma severity and treatment response evaluation.1,2 Although GINA guidelines do not specially recommend the use of spirometry, the Spanish consensus highlighted the use of pulmonary function tests, specifically spirometry measurements, as tools to evaluate the patient’s situation upon arrival at the emergency department and their dynamic response to the prescribed treatment in those places in where is available.16 Furthermore, these indicators help assess potential triggers for the asthmatic crisis and the percentage of previous exacerbations, enabling the evaluation of future exacerbation risks and the need for hospitalization.21,22 Despite these recommendations, lung function was scarcely recorded (and performed) in the ER records. That suggests that specific educational work should be performed at this point.
Insights from Trigger Identification and Previous History Documentation
The findings regarding the presence of information in medical records related to previous asthma history and triggers of exacerbation are significant in shaping patient care and management strategies.23 The identification of these factors within medical records plays a pivotal role in understanding the patient’s condition, allowing for personalized treatment plans and targeted interventions.24 The observed percentages, where a substantial portion of records contain details about prior asthma history (45.8%) and triggers of exacerbation (68.9%), indicate a positive trend in clinical documentation. Literature emphasizes the importance of comprehensive medical records that encompass previous asthmatic crises and triggers that lead to exacerbation. Studies have shown that having a detailed history of previous crises enables healthcare providers to tailor treatment regimens, anticipate potential exacerbations, and employ preventive measures effectively.14,25 Additionally, documenting triggers provides insights into environmental or lifestyle factors that influence exacerbation, aiding in patient education and interventions to mitigate risks. It underscores the necessity of standardized record-keeping practices in healthcare, ensuring the inclusion of crucial information that significantly impacts patient outcomes and the overall management of asthma.
Discharge Treatment Plan
Currently, there is limited evidence regarding how to manage the discharge procedure after attending the emergency room with an AE. No functional parameter indicates when a patient with an asthmatic exacerbation should be discharged from the hospital. Recently, as in Spain some years ago, a task force has developed a step-by-step plan for emergency department/hospital discharge in the United Arab Emirates, based on the GINA 2023 guideline recommendations. However, to the best of our knowledge, this plan has not yet been validated. In our population, patients who had multiple ED visits in 1 year, those with uncontrolled asthma, wheezing, ≥400 blood eosinophils/μL, or who had been discharged at the first ED visit are at higher risk of relapse.26 However, a well-structured discharge plan is crucial as it is linked to reduced relapse and/or ER readmission risk.27 It is noteworthy that only over 60% of patients received ICS/LABA treatment upon discharge, which is essential for asthma patients experiencing exacerbations. Nevertheless, this percentage was expected to be higher, considering the mandatory ICS/LABA treatment for this level of asthma severity. Furthermore, our assessment included measuring the percentage of patients referred to SC within a month, based on general referral criteria or within two weeks, under priority referral criteria. Only 13.3% of the patients had a defined timeframe for post-discharge care, indicating that, in most cases, follow-up appointments were not scheduled on a specific timeline. This lack of structured post-discharge care highlights the need for better protocols to ensure adequate and timely specialized care for these patients.28
Comparative Analysis
Both tertiary hospitals have similar characteristics and are integrated into the national health system, but they are located in different regions and serve populations that are not equal. La Paz University Hospital is in Madrid, the capital of Spain, characterized by a dense urban environment and a service-oriented economy. In contrast, Salamanca University Hospital serves as a smaller city facility, with a significant proportion of the population residing in rural areas. Remarkably, the comparative analysis revealed statistically significant differences between the two hospitals, likely indicating potential variations in patient populations, diagnostic criteria used, and distinct asthma profiles among patients at each center. Disparities in data recording practices between the two hospitals may also have contributed to the observed differences. HUS appears to place a greater emphasis on the clinical history of patients, with a notably higher percentage of individuals having a history of asthma (68.8%).
In contrast, HULP seems to prioritize the technical aspects, with a lower percentage of patients with a previous asthma history (32.9%). This variation in data collection and clinical focus highlights the importance of standardized documentation procedures and underscores potential variations in patient demographics, diagnostic criteria, and the overall approach to asthma management between the two centers. That could also reflect different treatment approaches between centers on more significant attention to respiratory functional diagnosis at La Paz.
This study has limitations, and the generalizability of the findings is limited by the fact that the study was conducted in only two hospitals in a single country. For this reason, caution should be exercised when extrapolating the findings to settings beyond the studied ones. Moreover, the retrospective data carry some inherent limitations, such as the reliance on existing MR, which may be incomplete or subject to potential errors in documentation. Nevertheless, this study represents the first attempt to evaluate and validate ER indicators, as no prior studies worldwide have systematically examined these specific metrics. That represents a first approximation to understanding the potential utility of these indicators in assessing ER performance and patient outcomes.
Conclusions
In conclusion, this study highlights significant variability in the documentation and adherence to recommended indicators for managing asthma exacerbations in the ER. While specific clinical assessments, such as auscultation, were consistently recorded, key parameters like respiratory rate and spirometry were frequently overlooked. Discharge planning and follow-up care were suboptimal, with many patients lacking clear therapeutic guidance and continuity of care. These findings underscore the need for improved standardization and implementation of evidence-based protocols in emergency asthma care. However, further research is required to definitively describe the degree of adherence to guidelines for managing AEs in real-world scenarios or whether it is mandatory to implement enhanced discharge protocols, ensure quality care, and facilitate the transition to post-hospital care.
Acknowledgments
The authors acknowledge Mariana Díaz Almirón and Francisco Gaya, biostatisticians, for their contributions to the statistical analysis of the results. They also thank GOC Health Consulting for their support in the development of the study and their medical writing assistance, as well as AstraZeneca Spain for funding the project. The study was funded by the Biomedical Research Institute of Salamanca (IBSAL) without any influence on the results. We also would like to acknowledge AstraZeneca, Spain, for their financial support.
Disclosure
ID has received payment for lectures, including service on speaker’s bureaus from Allergy Therapeutics, AstraZeneca, Chiesi, Diater, GSK, Leti, Novartis, and Sanofi; for a consultancy from Allergy Therapeutics, ALK-Abello, AstraZeneca, GSK, Merck, MSD, Novartis, Sanofi; and grants for Thermofisher Diagnostics, ISCIII, and Junta de Castilla y León, outside the present work. JDO reports personal fees from AstraZeneca, Novartis, Sanofi, Teva, ALK, GSK, Chiesi, and Leti outside the submitted work. JR reports consulting fees from AstraZeneca and Sanofi and honoraria for lectures or presentations from GSK, AstraZeneca, Sanofi, Gebro, Novartis, and Menarini. JGC reports honoraria for lectures for AstraZeneca. All authors report no other conflicts of interest in this work.
References
1. Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2023. Available from: https://www.ginasthma.org/.
2. Plaza Moral V, Alobid I, Álvarez R, et al. GEMA 5.3. Spanish Guideline on the Management of Asthma. Open Respir Arch. 2023;5(4):100277. doi:10.1016/j.opresp.2023.100277
3. British Thoracic Society & Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma: a national clinical guideline. 2019. Available from: https://www.brit-thoracic.org.uk/quality-improvement/guidelines/asthma/.
4. Bai TR, Vonk JM, Postma DS, Boezen HM. Severe exacerbations predict excess lung function decline in asthma. Eur Respir J. 2007;30(3):452–456. doi:10.1183/09031936.00165106
5. O’Byrne PM, Pedersen S, Lamm CJ, Tan WC, Busse WW. Severe exacerbations and decline in lung function in asthma. Am J Respir Crit Care Med. 2009;179(1):19–24. doi:10.1164/rccm.200807-1126OC
6. Weiss KB, Sullivan SD. The health economics of asthma and rhinitis. I. Assessing the economic impact. J Allergy Clin Immunol. 2001;107(1):3–8. doi:10.1067/mai.2001.112262
7. Lane S, Molina J, Plusa T. An international observational prospective study to determine the cost of asthma exacerbations (COAX). Respir Med. 2006;100(3):434–450. doi:10.1016/j.rmed.2005.06.012
8. Kupczyk M, Kupryś I, Górski P, Kuna P. Long-term deterioration of lung function in asthmatic outpatients. Respiration. 2004;71(3):233–240. doi:10.1159/000077420
9. Busse WW, Morgan WJ, Gergen PJ, et al. Randomized trial of omalizumab (anti-IgE) for asthma in inner-city children. N Engl J Med. 2011;364(11):1005–1015. doi:10.1056/NEJMoa1009705
10. Newby C, Agbetile J, Hargadon B, et al. Lung function decline and variable airway inflammatory pattern: longitudinal analysis of severe asthma. J Allergy Clin Immunol. 2014;134(2):287–294. doi:10.1016/j.jaci.2014.04.005
11. Greenberg S. Asthma exacerbations: predisposing factors and prediction rules. Curr Opin Allergy Clin Immunol. 2013;13(3):225–236. doi:10.1097/ACI.0b013e32836096de
12. Pola-Bibian B, Dominguez-Ortega J, Vilà-Nadal G, et al. Asthma exacerbations in a tertiary hospital: clinical features, triggers, and risk factors for hospitalization. J Investig Allergol Clin Immunol. 2016;2016:1.
13. Domínguez-Ortega J, Luna-Porta JA, Olaguibel JM, et al. Exacerbations Among Patients With Asthma Are Largely Dependent on the Presence of Multimorbidity. J Investig Allergol Clin Immunol. 2023;33(4):281–288. doi:10.18176/jiaci.0816
14. Castillo JR, Peters SP, Busse WW. Asthma Exacerbations: pathogenesis, Prevention, and Treatment. J Allergy Clin Immunol Pract. 2017;5(4):918–927. doi:10.1016/j.jaip.2017.05.001
15. Piñera Salmerón P, Delgado Romero J, Domínguez OJ, et al. Management of asthma in the emergency department: a consensus statement. Emergencias. 2018;30(4):268–277.
16. Piñera-Salmeron P, Álvarez-gutiérrez FJ, Domínguez-Ortega J, et al. Referral recommendations for adult emergency department patients with exacerbated asthma. Emergencias. 2020;32(4):258–268.
17. Backer V, Harving H, Søes-Petersen U, Ulrik CS, Plaschke P, Lange P. Treatment and evaluation of patients with acute exacerbation of asthma before and during a visit to the ER in Denmark. Clin Respir J. 2008;2(1):54–59. doi:10.1111/j.1752-699X.2007.00021.x
18. Al-Hamaden RA, Abed A, Khader HB, Hasoun L, Al-Dulaimi AH, Alsayed AR. Knowledge and Practice of Healthcare Professionals in the Medical Care of Asthma Adult Patients in Jordan with a Particular Reference to Adherence to GINA Recommendations. J Multidiscip Healthc. 2024;17:391–404. doi:10.2147/JMDH.S433149
19. Weber H, Bassett G, Bartl D, et al. Successful implementation of evidence-based guidelines in a regional emergency department for children presenting with acute asthma. Aust J Rural Health. 2019;27:557–562. doi:10.1111/ajr.12544
20. Nair P, O’Byrne PM. Medical algorithms: approach to adult asthma exacerbations. Allergy. 2021;76(11):3556–3559. doi:10.1111/all.14976
21. Arrotta N, Hill J, Villa-Roel C, Dennett E, Harries M, Rowe BH. Factors associated with hospital admission in adult patients with asthma exacerbations: a systematic review. J Asthma. 2019;56(1):34–41. doi:10.1080/02770903.2018.1424189
22. Gonzalez-Barcala FJ, Calvo-Alvarez U, Salgado-Castro FJ, et al. Asthma exacerbations: factors related to longer hospital stay. Acta Clin Belg. 2017;72(6):379–384. doi:10.1080/17843286.2017.1295524
23. Heaney LG, Robinson DS. Severe asthma treatment: need for characterising patients. Lancet. 2005;365(9463):974–976. doi:10.1016/S0140-6736(05)71087-4
24. Sundaresan AS, Schneider G, Reynolds J, Kirchner HL. Identifying Asthma Exacerbation-Related Emergency Department Visit Using Electronic Medical Record and Claims Data. Appl Clin Inform. 2018;9(3):528–540. doi:10.1055/s-0038-1666994
25. Légaré F, Adekpedjou R, Stacey D, et al. Interventions for increasing the use of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2018;7(7):Cd006732. doi:10.1002/14651858.CD006732.pub4
26. Pola-Bibian B, Dominguez-Ortega J, Vilà-Nadal G, et al. Predictors of asthma relapse in patients who attended an emergency department. Allergy Asthma Proc. 2018;39(4):292–298. doi:10.2500/aap.2018.39.4130
27. Schnyder D, Lüthi-Corridori G, Leuppi-Taegtmeyer AB, Boesing M, Geigy N, Leuppi JD. Audit of Asthma Exacerbation Management in a Swiss General Hospital. Respiration. 2023;102(1):12–25. doi:10.1159/000527268
28. Buhumaid R, Alzaabi A, Mahboub B, et al. The need for implementing a standardized, evidence-based emergency department discharge plan for optimizing adult asthma patient outcomes in the UAE, expert meeting report. Int J Emerg Med. 2024;17(1):172. doi:10.1186/s12245-024-00757-4
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



