Back to Journals » Clinical Ophthalmology » Volume 19
Evaluation of the Retinal Nerve Fiber Layer and Ganglion Cell Layer After Laser-Assisted in situ Keratomileusis, Femtosecond-Laser in-situ Keratomileusis, and Small Incision Lenticule Extraction Using Optical Coherence Tomography
Authors Shaaban YM, Badran TAF
Received 2 December 2024
Accepted for publication 9 March 2025
Published 19 March 2025 Volume 2025:19 Pages 973—984
DOI https://doi.org/10.2147/OPTH.S509766
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr John Miller
Yasmine Maher Shaaban,1,2,* Tamer Abdel Fattah Badran1,3,*
1Department of Ophthalmology, Faculty of Medicine, Ain Shams University, Cairo, Egypt; 2Ain Shams Specialized Hospital, Cairo, 11588, Egypt; 3Eye Subspeciality Center (ESC), Cairo, 11402, Egypt
*These authors contributed equally to this work
Correspondence: Yasmine Maher Shaaban, Department of Ophthalmology, Faculty of Medicine, Ain Shams University, Cairo, Egypt, Email [email protected]
Purpose: To compare the effects of applied suction using microkeratome Laser-assisted in situ keratomileusis. (LASIK), femtosecond-laser in-situ keratomileusis (Fs-LASIK), and Small Incision Lenticule Extraction (Fe-SMILE) on the thickness of the Retinal Nerve Fiber Layer (RNFL) and Ganglion Cell Layer (GCL).
Patients and Methods: This study included 72 eyes divided into three groups, each with 24 eyes. Each group underwent one of three different procedures. Preoperatively, at one day, one week, and three months postoperatively, Spectral Domain Optical Coherence Tomography (SD-OCT) was used to evaluate the thickness of RNFL and GCL.
Results: Preoperatively and at one day, one week, and three months postoperatively, the mean values for RNFL thickness in the LASIK group were 93.2 ± 3.2, 105.9 ± 3.8, 106.2 ± 3.3, and 93.3 ± 3.6 μm, respectively; for the Fs-LASIK group, they were 95.9 ± 3.1, 100.2 ± 3.3, 100.5 ± 3.3, and 96.1 ± 3.1 μm, respectively; and for the Fe-SMILE group, they were 95.6 ± 1.9, 99.8 ± 1.7, 100.2 ± 1.8, and 95.8 ± 1.9 μm, respectively. The mean values for GCL thickness in the LASIK group were 73.9 ± 4.7, 90.2 ± 2.8, 90.8 ± 2.2, and 74.8 ± 4.5 μm, respectively; for the Fs-LASIK group, they were 77.8 ± 4.2, 80.2 ± 3.7, 80.3 ± 3.7, and 77.8 ± 3.5 μm, respectively; and for the Fe-SMILE group, they were 77.0 ± 3.7, 79.8 ± 3.6, 80 ± 3.7, and 77.1 ± 3.6 μm, respectively.
Conclusion: All three procedures resulted in a transient increase in RNFL and GCL thicknesses. This increase was rapid, limited, transient, and reversible. It peaked for a week and returned to baseline by the end of this three-month study. At day one and day seven post-operatively, the Lasik group exhibited statistically significantly higher values than the Fs-Lasik and Fe-Smile groups.
Keywords: microkeratome, bladeless laser, neurons, axons, imaging
Introduction
Laser in situ keratomileusis (LASIK), femtosecond-laser in-situ keratomileusis (Fs-LASIK), and Femto-laser Small Incision lenticule Extraction (Fe-SMILE) are common refractive surgery procedures. During these procedures, there is an increase in intraocular pressure (IOP) during the use of a suction ring.1 The IOP values may reach up to 65 mmHg. This transient elevation of the IOP may cause retinal and optic nerve ischemia and damage that compromises the structure and function of these ocular tissues among glaucoma patients or suspects.2,3
LASIK is a common ophthalmologic surgical procedure used to correct refractive errors. It became popular due to its short recovery time and rare post-operative complications. The corneal flaps during surgery are created by either a mechanical microkeratome (MMK) or a femtosecond laser.
The femtosecond machines create the LASIK flaps with a neodymium laser at 1,053 nm, dissecting the corneal tissue through microphotodisruption. The femtosecond laser offers advantages over microkeratomes by enabling the non-mechanical creation of corneal flaps, which is more precise, has a low incidence of flap complications, and cuts thinner flaps without button-hole formation.4 Fs-LASIK flap creation causes less IOP fluctuations during suction than when using a microkeratome,5 but requires more time. However, a sudden rise in IOP, which can damage the eye, has been observed during LASIK.6
The Fe-SMILE is a minimally invasive procedure in corneal refractive surgery. It is a flap-free intrastromal laser-assisted surgery to correct myopia and myopic astigmatism. The lenticule removal reshapes, flattens the cornea, and corrects vision with better ocular surface stability and biomechanical strength.7
LASIK changes corneal biomechanical properties that may play a role in developing post-LASIK ectasia. Fe-SMILE may have biomechanical benefits over LASIK because there is no flap creation, and the stroma over the lenticule is intact.8
Fe-SMILE is less damaging to the corneal nerve fibers on the ocular surface than Fs-LASIK. The aberration in the Fe-SMILE group is superior to that in the Fs-LASIK, and the loss of biomechanical effects may occur less frequently after Fe-SMILE than after Fs-LASIK.9. The corneal hysteresis biomechanical measure may be required to predict and qualify refractive surgery outcomes in cases where corneal biomechanics are important.10
Aim of the Study
Is analyzing changes in RNFL and GCL during LASIK, Fs-LASIK, and Fe-SMILE procedures on the thickness of the retinal nerve fiber layer (RNFL) and the ganglion cell layer (GCL) using the Spectral Domain Optical Coherence Tomography (SD-OCT).
Materials and Methods
Ethical Consideration
The study was conducted at the Department of Ophthalmology, Faculty of Medicine, Ain Shams University Hospitals, Cairo, Egypt, and in the Eye Subspecialty Center, Cairo, Egypt. The study is adherent to the tenets of the Declaration of Helsinki and has administrative approval from the Medical and Ethical Committee (REC) FWA 000017585, [email protected] of Ain Shams University. Informed consent was obtained from each patient.
Inclusion Criteria
Patients’ ages ranged from 21 to <40 years, with stable refraction for at least one year before surgery. The spherical error was between −1.00 D and −6.00 D. The cylindrical error was less than −4.00 D. All patients had normal corneal topography, pachymetry ≥ 500 μm, and residual stromal bed after correction ≥ 300 μm. Goldmann applanation tonometry was performed, and all patients had IOP <21 mmHg. “Pupil examinations were conducted to exclude abnormally large pupils in the dark, as patients with large pupillary sizes may be at greater risk for glare and halos after LASIK”.
Exclusion Criteria
Unstable refraction, previous ocular or corneal surgery, moderate or severe dry eye, autoimmune diseases (lupus, rheumatoid arthritis), collagen or systemic diseases that may affect wound healing, cataract, glaucoma and glaucoma suspects, keratoconus, corneal ectasia, or edema, insufficient corneal thickness for the required ablation depth. A history of keloids and the use of some medications (retinoic acid, migraine drugs, and steroids) that may prevent proper healing after a refractive procedure were excluded from the study. All patients had corneal pachymetry and topography using Pentacam® (Oculus, Inc, Wetzlar, Germany) to rule out LASIK contraindications.
The ocular examination included uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest, and cycloplegic refraction. Lid examination for signs of meibomian gland dysfunction. Anterior segment slit lamp biomicroscopy for signs of dry eyes, punctate keratitis, corneal irregularities/abnormalities, interstitial or neurotrophic keratitis, corneal scarring or vascularization, old iritis, iris atrophy, old herpetic disease, or other inflammatory diseases. Goldmann applanation tonometry was done. A dilated fundus examination was done on the retinal periphery to detect any tears or holes that need treatment before performing LASIK. The optic nerve was normal.
Surgical Procedure
The procedure was performed in the operating room under complete aseptic conditions. Tropicamide 1.0% (Mydriacyl, Alcon Novartis, Couvreur, Belgium) was used for preoperative pupillary dilatation. Topical benoxinate hydrochloride 0.4% (Benox®, Eipico, Inc., Cairo, Egypt) was used to anesthetize the eye. An eyelid speculum was inserted, and the cornea was marked for a postoperative flap. The globe was held in place by a suction ring, and the pressure steadily increased.
In the Lasik procedure, the corneal flap was created using the Moria™ single-use (M2, MMK, Antony, France). The hinge was made at the 12 o’clock position. The Alcon/WaveLight® EX 500 Excimer laser system (Alcon Surgical, Fort Worth, Texas, USA) was used for ablation. Balanced Salt Solution (BSS®) irrigated the corneal stromal bed, and the flap was repositioned with an irrigation cannula. Micro-sponges were used to dry the corneal surface to ensure flap adherence. Variable ring sizes were selected based on corneal curvature (K readings), following the Moria Nomogram.
In the Fs-LASIK procedure, the corneal flap thickness was 110 μm. The superior hinge in all flaps had an angle of 90°, a diameter of 9 mm, and a 70-degree angled side cut. The suction ring was applied. The flap centration was done. The flap was created using the Alcon/WaveLight® FS200 (Alcon Surgical, Fort Worth, Texas, USA). The corneal flap and the side cut were done. The patient’s bed was moved to the Alcon WaveLight® EX 500 Excimer Laser system for Excimer laser ablation. Before ablation, the flap was dissected and raised from the corneal stromal bed. The patient was asked to look at a green target, and a micro-sponge was used to protect the flap during the Excimer laser application. The corneal stromal bed was irrigated with Balanced Salt Solution (BSS®), and the flap was repositioned with an irrigating cannula. The corneal surface was dried with micro-sponges to ensure flap adherence.
In the Femto-SMILE procedure, the thickness of the corneal cap was set to 100 μm with a cap diameter of 7.5 mm, the lenticule side-cut angle was set at 90°, and the lenticule diameter (optical zone) was set to 6.5 mm. The wound was positioned at 4 mm on the upper side. The Visumax® S cone (Carl Zeiss Meditec AG, Jena, Germany) patient interface was used. The patient was adjusted to ensure contact with the femtosecond laser’s glass interface, focusing directly on the green target. The corneal suction ports were activated for eye fixation and to complete the docking process. The lower interface of the intrastromal lenticule was created using an out-to-in technique. This was followed by creating the upper interface of the lenticule with an in-to-out technique. A 2 mm superior-temporal tunnel incision was then made to connect the cap interface to the corneal surface. Then, the patient was moved to the surgical microscope. The small incision was opened, allowing the upper and lower edges of the lenticule to be delineated. The upper interface was then dissected using a circular blunt dissector, followed by a dissection of the lower interface with a blunt spatula. After separating both layers, micro-forceps removed the lenticule from the cornea. The interface was washed with Balanced Salt Solution (BSS®), and the corneal surface was dried using micro-sponges.
Patients who experienced intraoperative complications during any of the three procedures were excluded from the study.
Postoperative treatment included topical antibiotics and a steroid combination, administered three times daily for two weeks and tapered over the following two weeks, along with preservative-free artificial tears used six times daily for two months.
The thicknesses of the RNFL and GCL, as well as the thickness of the four quadrants of the RNFL and the six sectors of the GCL, were measured and analyzed preoperatively and postoperatively at one day, one week, and three months using the Zeiss Cirrus-HD 5000 SD-OCT (Carl Zeiss Meditec AG, Jena, Germany).
Statistical Methods
In this prospective cohort comparative study, a one-way repeated measures ANOVA was performed to analyze the Retinal Nerve Fiber Layer and the Ganglion Cell Layer thicknesses. This analysis considered two factors: the time points (preoperative, one day, one week, and three months postoperative) and the procedure groups (LASIK, Femto-LASIK, and Femto-SMILE). If the interaction between these two factors is statistically significant, simple effects analyses can be conducted to present and compare the outcome variables. This involves comparing the thickness for each procedure across different time points and evaluating the thickness at each time point among the various procedures. Data management and statistical analysis were done using SPSS (Statistical Package for the Social Sciences) version 25 (Armonk, NY: IBM Corp, 2017).
Results
The study includes 72 eyes of 36 patients with simple myopia or myopic astigmatism. Twenty-four eyes had LASIK, 24 had Fs-LASIK, and 24 had Fe-SMILE procedures. The mean age was 26.25 ± 4.4 years in the LASIK group, 26.00 ± 2.5 years in the Fs-LASIK group, and 28.67 ± 4.2 years in the Fe-SMILE group. The mean spherical equivalent was −4.13 ± 2.2 D in the LASIK group, 4.95±2.5 D in the Fs-LASIK group, and −5.81± 2.0 D in the Fe-SMILE group. Regarding age, sex, and spherical equivalent, there was no statistically significant difference between the groups. The RNFL and the GCL thicknesses at different points of time in the three laser procedures are presented in Tables 1 and 2.
 |
Table 1 The RNFL Thickness in Microns at Different Points of Time Presented as Mean ± SD |
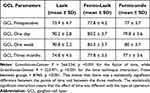 |
Table 2 The GCL Thickness in Microns at Different Points of Time Presented as Mean ± SD |
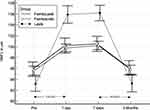
In the RNFL, the mean differences between the three groups of Laser procedures at each time points were compared (Table 3 and Figure 1).
 |
Table 3 The Mean Differences in RNFL Between Different Laser Procedures at Each Time Point |
The mean changes in RNFL thickness over time in the three groups of laser procedures (Table 4 and Figure 2).
 |
Table 4 Mean Changes in RNFL Thickness Over Time in the Three Laser Procedures |
In the GCL, the three groups of Laser procedures at the different points of follow-up times were compared (Table 5 and Figure 3).
 |
Table 5 The Mean Differences in GCL Thickness Between the Three Laser Procedures at Each Time Point |
The mean changes in GCL thickness over time in the three laser procedures have been reported (Table 6 and Figure 4).
 |
Table 6 Mean Changes in GCL Thickness Over Time in the Three Laser Procedures |
Preoperatively, the RNFL and GCL thicknesses were more or less the same in the three groups. They began to increase on days one and seven before returning to their pre-operative levels after three months. However, on days one and seven, the Lasik group demonstrated statistically significantly higher values than the other two groups, which exhibited similar and closer values.
Discussion
LASIK is a corneal refractive technique that enhances vision. Both microkeratomes and Fs-LASIK include the dissection of a superficial lamellar flap by suction and remodeling of the underlying corneal stroma.11
As reported in the literature, LASIK with a mechanical microkeratome does not damage the retinal nerve fiber layers in healthy individuals. However,12,13 LASIK treatment is not recommended in glaucoma patients and suspects, not only because of the intermittent IOP rise but also because changes in the corneal structure can lead to less reliable IOP measurements.
In glaucoma patients or suspects, the LASIK application remains controversial. IOP may increase during the suction ring application and the flap creation. This transient IOP elevation may compromise the structural and functional integrity of the retina and optic nerve.2,3 It had been reported that the incidence of posterior vitreous detachment (PVD) one month after Fs- LASIK was higher than after microkeratome LASIK. This may be due to longer suction time during Fs- LASIK despite lower suction pressure.14 LASIK showed temporary changes in retinal foveal measurements by OCT one hour and one day after LASIK surgery.15,16
Studies concerning Fs-LASIK are still limited and controversial. Some studies reported changes within the retina following Fs-LASIK,6 while others did not,17 and the clinical significance of such changes was variable.18,19
The Fe-SMILE is not supposed to induce complications related to a sudden increase in IOP. During the Fe-SMILE procedure, the suction pressure by the VisuMax laser system is lower than that in Fs-LASIK by approximately 35 mmHg.20 The pressure is low enough to maintain the intraocular tissue integrity. However, the Fe-SMILE takes significantly more time (25–28 seconds) than Fs-LASIK; therefore, eyes undergoing Fe-SMILE are exposed to a longer duration of increased IOP.21
The results of our study showed that on day one, the values for the mean, the four quadrants of the RNFL, and the six sectors of the GCL thickness significantly increased compared to preoperative values. This increase was rapid, limited, transient, and reversible. Day seven exhibited a similar pattern to day one, with no significant differences. Notably, the increase was more pronounced in the LASIK group compared to the Fs-LASIK and the Fe-SMILE groups. A statistically significant decrease was observed compared to the measurements taken on days one and seven, bringing the values closer to preoperative levels for LASIK, Fs-LASIK, and Fe-SMILE groups by the end of the three-month study.
Some studies showed no changes in the RNFL and GCL thicknesses following LASIK, FS-LASIK, or Fe-SMILE at different points of the postoperative follow-up period.16–18,22–26. All measurements remained stable after surgery.
Gürses-Ozden et al22 evaluated the effect of LASIK on RNFL thickness in 20 eyes measured with OCT one week before, one week after, and four weeks after surgery. The mean RNFL thicknesses remained unchanged one week and four weeks after LASIK. They concluded that LASIK does not affect RNFL thickness.
Rodriguez et al23 investigated the impact of LASIK on RNFL thickness in fifty myopic eyes using SD-OCT for measurement. No statistically significant differences were found in the mean, superior, inferior, nasal, and temporal RNFL thicknesses, comparing preoperative values to those measured two weeks postoperatively.
Feng et al18 utilized Time-Domain (TD-OCT) to compare retinal measurements before and after myopic LASIK. Their goal was to assess the impact of LASIK on retinal structures. The study found that most retinal OCT measurements exhibited no significant changes following the myopic LASIK procedure.
Zhao et al16 studied macular and peripapillary RNFL thickness in 56 eyes of children with refractive amblyopia: high myopes, moderate myopes, and hypermetropes who underwent Fs-LASIK procedures. Thicknesses were measured using Fourier Domain (FD-OCT) before surgery and one day, three days, and one week after surgery. In the high myopes, the foveal and parafoveal retinal thicknesses were thicker one day and three days after surgery than before surgery, and no significant difference was found one week after surgery. In the mild myopic and hyperopic eyes, the foveal and parafoveal retinal thicknesses were greater one day after surgery than before, and no significant difference was found three days or one week after surgery. In all patients, no significant difference was found in the macular inner retinal or peripapillary RNFL thickness one day, three days, or one week after surgery.
Zivkovic et al17 studied the effects of suction during LASIK surgery on the RNFL and macular ganglion cell-inner plexiform layer (GC-IPL) in 124 myopic eyes. The SD-OCT measurements were taken before surgery and at one and six months afterward. All measurements remained stable following the surgery.
Özülken et al24 evaluated the early effects of LASIK surgery on GCL thickness, RNFL thickness, and central macular thickness (CMT) using SD-OCT in 40 healthy subjects. The preoperative, postoperative one-hour, and postoperative three weeks GCLT, NFLT, and CMT values were compared. There were no changes in values following Fs-LASIK surgery.
In fifty eyes, Zhao et al25 used SD-OCT to assess changes in IOP, RNFL thickness, and macular GCC thickness after Fe-SMILE surgery. Measurements taken before surgery and three months postoperatively showed no statistically significant changes in RNFL or GCC thickness. SMILE surgery did not affect peripapillary RNFL or macular GCC thickness.
Kubravi et al26 assessed the changes in the RNFL thickness following the LASIK procedure in young myopic patients. They measured RNFL thickness using SD-OCT before the surgery and at one and three months postoperatively. The differences observed were not statistically significant, suggesting that LASIK does not significantly impact RNFL thickness, according to the OCT analysis.
Other studies compared the effect of LASIK, Fe-LASIK, and Fe-SMILE on RNFL and GCL thickness. They showed no significant differences in preoperative and postoperative measurements for either procedure.15,27–29
Hosney et al27 studied the effect of transient IOP elevation during suction in LASIK on the RNFL thickness, comparing MMK LASIK to Fs-LASIK. Using SD-OCT, they measured the RNFL thickness preoperatively and one month postoperatively. The findings revealed no significant differences between the preoperative and postoperative RNFL thickness. The temporary rise in IOP during the suction process did not impact RNFL thickness for either technique.
Zhang et al15 conducted a study comparing the effects of suction on macular and RNFL thickness during Fs-LASIK and Fe-SMILE procedures using the Visumax FS system. The FD-OCT was used to assess retinal thickness preoperatively and at one, three, and six months postoperatively. The results showed no significant differences in retinal thicknesses between the two groups at any postoperative time, concluding that suction did not have an important clinical impact on macular thickness or RNFL during either procedure.
Zhang et al6 studied the effects of suction on macular thickness, ganglion cell complex thickness, and RNFL thickness in 204 eyes; 102 eyes had the Ziemer Fs-LASIK, and 102 eyes had the Moria M2 microkeratome using FD-OCT before and up to one year after surgery. They reported a temporary increase in macular thickness and a short-term decrease in RNFL thickness. In both groups, the thickness of the GCC did not change significantly. The decreased RNFL thickness was less in the Fs-LASIK group. The RNFL thickness had recovered to the preoperative level one day after surgery.
Ghanem et al28 compared the effect of the IOP elevation during suction on the macular and RNFL thickness after Fs-LASIK and Fe-SMILE using SD-OCT preoperatively and at one week, one, three, and six months postoperatively. The mean RNFL thickness did not change significantly from the preoperative to any postoperative time points in Fs-LASIK and Fe-SMILE procedures.
Jiang et al19 studied the effects of Fs-LASIK on the retinal fovea and RNFL thickness in 37 patients using OCT. Assessments were made before surgery, one hour after, and one day after. Results showed significant decreases in macular foveal thickness, volume, and RNFL thickness at both post-surgery time points. The RNFL thickness decreased in the temporal and superior regions one hour post-procedure, while an increase was noted in the inferior region by the first day. Macular and RNFL measurements increased from one hour to one day after the surgery.
El Feky et al29 studied the impact of suction on the posterior segment after LASIK, involving 30 eyes treated with Fs-LASIK and 30 eyes with MM-LASIK for myopia. The findings revealed no significant changes in central macular or RNFL thickness one week post-surgery. There were slight localized alterations in macular thickness and a reduction in RNFL thickness after LASIK, regardless of whether Fs-Laser or MMK was used for flap creation.
Conflicting evidence exists regarding RNFL and GCL thickness measurements using SD-OCT across different LASIK procedures. These inconsistencies may stem from retinal edema caused by significant increases in IOP during the suction phase. Traditional LASIK tends to reach higher levels of IOP, while Fs-LASIK maintains lower IOP for a longer duration. However, both procedures exhibit similar unequal responses.
The observed increase in RNFL and GCL thickness across the three LASIK groups may represent an immediate “rebound response” of the tissues to the sudden rise in IOP during the use of a suction ring, followed by a decrease in IOP to normal or even subnormal levels as soon as the suction is released. This reaction could also be linked to the subsequent microvascular response of the retinal blood vessels. The increase in thickness is proportional to the pressure applied, with traditional LASIK showing a more significant rise compared to the smaller increases observed with Fs-LASIK and Fe-SMILE.
Conclusion
This study likely represents the first comparison of the effects of LASIK, Fs-LASIK, and Fe-SMILE on the thickness of the RNFL and the GCL, pre-and post-operatively, over various periods. The results showed that on day one, the values of the mean, the four quadrants of the RNFL, and the six sectors of the GCL thickness significantly increased compared to the preoperative values. This increase was rapid, limited, transient, and reversible, peaked for a week, and returned to baseline by the end of this three-month study. Notably, the increase was more pronounced in the LASIK group compared to the Fs-LASIK and Fe-SMILE groups.
Abbreviations
CDVA, Corrected Distance Visual Acuity; CH, Corneal Hysteresis; CRF, Corneal Resistance Factor; D, diopter; Fe-SMILE, Femto Small Incision Lenticule Extraction; FD-OCT, Fourier Domain Optical Coherence Tomography; Fs-LASIK, Femtosecond-Laser in-Situ Keratomileusis; GCC, ganglion cell complex; GC-IPL, Ganglion cell-inner plexiform layer; GCL, Ganglion Cell Layer; IOP Intra Ocular Pressure; LASIK, Laser in Situ Keratomileusis; MMK, Mechanical Microkeratome; OCT, Optical Coherence Tomography; PVD, Posterior Vitreous Detachment; RD, Retinal Detachment; RNFL, Retinal Nerve Fiber Layer; SD-OCT, Spectral Domain Ocular Computed Tomography; TD-OCT, Time Domain Optical Coherence Tomography; UDVA, Uncorrected Distance Visual Acuity.
Data Sharing Statement
All data supporting the results of this study are included in the manuscript. There is no unpublished data available.
Acknowledgments
The authors thank Professor Dr Mustafa El Hossini, Professor of Community and Public Health, Faculty of Medicine, Ain University, for his precious time and effort in assisting with the Statistics of this study.
Author Contributions
Both authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; they took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Shrivastava A, Madu A, Schultz J. Refractive surgery and the glaucoma patient. Curr Opin Ophthalmol. 2011;22(4):215–221. doi:10.1097/ICU.0b013e3283477c73
2. Kasetsuwan N, Pangilinan RT, Moreira LL, et al. Real-time intraocular pressure and lamellar corneal flap thickness in keratomileusis. Cornea. 2001;20(1):41–44. doi:10.1097/00003226-200101000-00008
3. Bashford KP, Shafranov G, Tauber S, Shields MB. Considerations of glaucoma in patients undergoing corneal refractive surgery. Surv Ophthalmol. 2005;50(3):245–251. doi:10.1016/j.survophthal.2005.02.006
4. Diekmann H, Fischer D. Glaucoma and optic nerve repair. Cell Tissue Res. 2013;353(2):327–337. doi:10.1007/s00441-013-1596-8
5. Sutton G, Hodge C. Accuracy and precision of LASIK flap thickness using the IntraLase femtosecond laser in 1000 consecutive cases. J Refract Surg. 2008;24(8):802–806. doi:10.3928/1081597X-20081001-06
6. Zhang J, Zhou YH. Effect of suction on macular thickness and retinal nerve fiber layer thickness during LASIK used femtosecond laser and Moria M2 microkeratome. Int J Ophthalmol. 2015;8(4):777–783. doi:10.3980/j.issn.2222-3959.2015.04.24
7. Sekundo W, Kunert KS, Blum M. Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6-month prospective study. Br J Ophthalmol. 2011;95(3):335–339. doi:10.1136/bjo.2009.174284
8. Agca A, Ozgurhan EB, Demirok A, et al. Comparison of corneal hysteresis and corneal resistance factor after small incision lenticule extraction and femtosecond laser-assisted LASIK: a prospective fellow eye study. Cont Lens Anterior Eye. 2014;37(2):77–80. doi:10.1016/j.clae.2013.05.003
9. Yan H, Gong LY, Huang W, Peng YL. Clinical outcomes of small incision lenticule extraction versus femtosecond laser-assisted LASIK for myopia: a Meta-analysis. Int J Ophthalmol. 2017;10(9):1436–1445. doi:10.18240/ijo.2017.09.17
10. Luce DA. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg. 2005;31(1):156–162. doi:10.1016/j.jcrs.2004.10.044
11. Gil-Cazorla R, Teus MA, de Benito-Llopis L, Mikropoulos DG. Femtosecond laser vs. mechanical microkeratome for hyperopic laser in situ keratomileusis. Am J Ophthalmol. 2011;152(1):16–21.e2. doi:10.1016/j.ajo.2011.01.009
12. Dementyev DD, Kourenkov VV, Rodin AS, Fadeykina TL, Diaz Martines TE. The retinal nerve fiber layer changes after LASIK is evaluated with optical coherence tomography. J Refract Surg. 2005;21(5):S623–7. doi:10.3928/1081-597X-20050902-13
13. Aristeidou AP, Labiris G, Paschalis EI, Foudoulakis NC, Koukoula SC, Kozobolis VP. Evaluation of the retinal nerve fiber layer measurements after photorefractive keratectomy and laser in situ keratomileusis, using scanning laser polarimetry (GDX VCC). Graefes Arch Clin Exp Ophthalmol. 2010;248(5):731–736. doi:10.1007/s00417-009-1273-5
14. Osman MH, Khalil NM, El-Agha MS. Incidence of posterior vitreous detachment after femtosecond LASIK compared with microkeratome LASIK. Cornea. 2017;36(9):036–1039. doi:10.1097/ICO.0000000000001277
15. Zhang J, Zhou Y, Zheng Y, Liu Q, Zhai C, Wang Y. Effect of suction on macular and retinal nerve fiber layer thickness during femtosecond lenticule extraction and femtosecond laser-assisted laser in situ keratomileusis. J Cataract Refract Surg. 2014;40:1994–2001. doi:10.1016/j.jcrs.2014.03.027
16. Zhao PF, Zhou YH, Zhang J, Wei WB. Analysis of macular and retinal nerve fiber layer thickness in children with refractory amblyopia after femtosecond laser-assisted laser in situ keratomileusis: a retrospective study. Chinese Med J. 2017;130(18):2234–2240. doi:10.4103/0366-6999.213959
17. Zivkovic M, Jaksic V, Giarmoukakis A, et al. The effect of LASIK procedure on peripapillary retinal nerve fiber layer and macular ganglion cell-inner plexiform layer thickness in myopic eyes. Biomed Res Int. 2017;2017:8923819. doi:10.1155/2017/8923819
18. Feng L, Lei F, Burns SA, Shao L, Yang Y. Retinal measurements using time domain OCT imaging before and after myopic LASIK. Ophthalmic Physiol Optics. 2012;32(3):222–227. doi:10.1111/j.1475-1313.2012.00905.x
19. Jiang Y, Wang Z, Li Y, Li Y, Lu TC. Retinal nerve fibre layer thickness change following femtosecond laser-assisted in situ keratomileusis. Front Med. 2021;8:778666. doi:10.3389/fmed.2021.778666
20. Titiyal JS, Kaur M, Shaikh F, Gagrani M, Brar A, Rathi A. Small incision lenticule extraction (SMILE) techniques: patient selection and perspectives. Clin Ophthalmol. 2018;12:1685–1699. doi:10.2147/OPTH.S1571722-s2.0-8505771314
21. Ang M, Chaurasia SS, Angunawela RI, et al. Femtosecond lenticule extraction (FLEx): clinical results, interface evaluation, and intraocular pressure variation. Invest Ophthalmol Visual Sci. 2012;53(3):1414–1421. doi:10.1167/iovs.11-8808
22. Gürses-özden R, Liebmann JM, Schuffner D, Buxton DF, Soloway BD, Ritch R. Retinal nerve fiber layer thickness remains unchanged following laser-assisted in situ keratomileusis. Am J Ophthalmol. 2001;132(4):512–516. doi:10.1016/S0002-9394(01)01094-7
23. Rodríguez-Agirretxe I, García Gómez de Segura M, Etxebarria Ecenarro J, Dios Castro M. Influencia del LASIK en la capa de fibras nerviosas retinianas [Influence of LASIK on retinal nerve fiber layer]. Arch Soc Esp Oftalmol. 2004;79(12):605–608. Spanish. doi:10.4321/s0365-66912004001200006
24. Özülken K, Ilhan Ç. Evaluation of retinal ganglion cell layer thickness in the early period after femtosecond LASIK surgery. Turk J Ophthalmol. 2020;50(4):211–215. doi:10.4274/tjo.galenos.2020.29939
25. Zhao Z, Michée S, Faure JF, Baudouin C, Labbé A. Effects of SMILE surgery on intraocular pressure, central corneal thickness, axial length, peripapillary retinal nerve fiber layer, and macular ganglion cell complex thickness. J Ophthalmol. 2020;2020:1–6. doi:10.1155/2020/4934196
26. Kubravi SH, Kawoosa K, Mufti H. Changes in retinal nerve fiber layer thickness after mechanical microtome-assisted lasik. Global J Res Anal. 2022;11(12):9–11. doi:10.36106/GJRA
27. Hosny M, Zaki RM, Ahmed RA, Khalil N, Mostafa HM. Changes in retinal nerve fiber layer thickness following mechanical microkeratome-assisted versus femtosecond laser-assisted LASIK. Clin Ophthalmol. 2013;7:19191922. doi:10.2147/OPTH.S51774
28. Ghanem AA, Mady SA, Attia TN, Salem TI. Femtosmile vs Fs- LASIK. Macular and retinal nerve fiber layer thickness changes after small-incision lenticule extraction and femto-LASIK. Delta J Ophthalmol. 2015;16(2):50–75. doi:10.4103/1110-9173.168528
29. El-Feky HM, Saeed AM, Abdel Aziz AS. Effect of suction on the posterior segment after LASIK using femtosecond laser vs microkeratome. BJAS. 2021;6(3):177–18.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.