Back to Journals » Clinical Ophthalmology » Volume 18
Evidence in Practice: A Review of Real-Life Studies and Clinical Experience with the Preservative-Free Tafluprost (0.0015%) and Timolol (0.5%) Fixed-Dose Combination
Authors Hollo G
Received 25 May 2024
Accepted for publication 12 September 2024
Published 8 November 2024 Volume 2024:18 Pages 3185—3196
DOI https://doi.org/10.2147/OPTH.S479852
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Gábor Hollo1,2
1Tutkimusz Ltd., Solymár, Hungary; 2Eye Center, Prima Medica Health Centers, Budapest, Hungary
Correspondence: Gábor Hollo, Tutkimusz Ltd., Solymár, Hungary, Email [email protected]
Abstract: The preservative-free fixed-dose combination formulation of 0.0015% tafluprost and 0.5% timolol (PF tafluprost/timolol FC) is among the topical intraocular pressure (IOP)-lowering therapies commonly used second-line for the management of ocular hypertension (OHT) and open-angle glaucoma (OAG), according to recommended treatment pathways. A growing body of evidence has developed in recent years regarding efficacy, safety and tolerability outcomes with PF tafluprost/timolol FC in both randomized controlled trials (RCTs) and real-life studies. This review aims to summarize key evidence from published Phase IV trials and real-life studies to highlight those data that complement RCT findings and support implementation of evidence-informed clinical practice. Real-life efficacy and safety outcomes are discussed through the lens of common clinical scenarios that ophthalmologists may encounter in the management of OHT/OAG. Phase IV studies conducted to date have demonstrated that the majority of OHT/OAG patients insufficiently controlled on topical prostaglandin or beta-blocker monotherapy may achieve IOP reductions of ≥ 20% following a switch to PF tafluprost/timolol FC therapy. Statistically significant IOP reductions were reported from 4 weeks and maintained through 6 months. Real-life studies and case series data also indicated that patients with poor IOP control on maximal/complex topical regimens benefited from a step down to PF tafluprost/timolol FC therapy, achieving significant and sustained IOP reductions. A number of studies have shown improvements in tolerability and the signs and symptoms of ocular health with PF tafluprost/timolol FC therapy, both in patients stepping up from monotherapy and in those simplifying their topical regimen. Clinicians reported better treatment adherence with PF tafluprost/timolol FC compared with prior treatments, which may have been associated with enhanced patient experience regarding treatment tolerability and is likely to have contributed to the long-term IOP-lowering efficacy outcomes observed. Real-life safety data for PF tafluprost/timolol FC reflect outcomes reported in published RCTs.
Keywords: intraocular pressure, ocular hypertension, ocular tolerance, open-angle glaucoma, preservative-free tafluprost/timolol fixed combination
Introduction
Glaucoma is a leading cause of irreversible vision loss and is associated with a significant negative impact on quality of life (QoL).1–4 Intraocular pressure (IOP) is the only modifiable risk factor for deterioration of the visual functions associated with glaucoma.3,5–8 Following diagnosis, most glaucoma patients receive long-term topical IOP-lowering medication encompassing a broad range of monotherapy and combination therapies, the latter of which have been shown to be of particular clinical importance in slowing glaucomatous progression.4,6,9–11 Compared with separate instillations of IOP-lowering monotherapy agents, fixed-dose combination (FC) therapies offer the clinical advantages of reduced daily instillations and lower multiple exposures to preservatives, such as benzalkonium chloride (BAK), which can commonly cause ocular surface toxicity and local tolerability issues.8–17 Historically, FC treatments that comprise a prostaglandin analogue (PGA) and a beta-receptor blocker (beta-blocker) have been widely introduced second-line in the management of open-angle glaucoma (OAG).4 However, in selected cases, such as advanced glaucoma and/or very high untreated IOP, a combination treatment may be used from the beginning of treatment.4 Beta-blocker-containing FCs should be used where appropriate and considering contraindications. The preservative-free (PF) FC formulation of 0.0015% tafluprost and 0.5% timolol (PF tafluprost/timolol FC) was the first PF PGA/timolol formulation introduced worldwide (outside of the USA) in clinical practice (approximately 10 years ago), offering OAG and ocular hypertensive (OHT) patients a clinically significant IOP reduction in a once-daily regimen that avoids ocular exposure to preservative agents.18–21 While no PGA/beta-blocker FC therapies are licensed for use in the USA as statistical superiority was not demonstrated against unfixed combinations of the relevant component agents, the PF tafluprost/timolol FC has fulfilled non-inferiority criteria in studies comparing it against its individual components and other PGA/timolol FC formulations.18,20,22,23 A large body of evidence now exists concerning PF tafluprost/timolol FC treatment, from randomized prospective clinical trials and real-life studies, reporting data on IOP-lowering efficacy, tolerance and patient preference.18–45 In particular, outcomes captured in real-life studies may support clinicians working to optimize and personalize selection of topical glaucoma medication for their patients. Significant IOP reductions have been shown in patients switched to PF tafluprost/timolol FC from various monotherapies, FC formulations and unfixed combinations.25,26,28,30–36 Baseline IOP under topical treatment is known to be predictive of the level of IOP reduction achieved with PF tafluprost/timolol FC in clinical practice, regardless of the prior treatment regimen used.25,31,32,35,36 This review paper focuses on the needs of ophthalmologist clinicians for optimal glaucoma care: it examines currently available Phase IV and real-life data concerning the use of PF tafluprost/timolol FC in the treatment of OAG and OHT. The data discussed include treatment outcomes observed in patients insufficiently controlled on monotherapy, in those simplifying treatment from more complex topical regimens or in cases where treatment switches have been made to address tolerability issues with existing medications.
While randomized controlled trials (RCTs) remain the gold standard approach for studies supporting regulatory approval during the drug development process, the value of real-life evidence is gaining increasing recognition in the era of big data.46–48 Real-life studies enable treatment outcomes to be examined in a more heterogenous population that includes groups of patients who would otherwise be excluded from RCTs due to confounding factors, such as comorbidities, age, sex and lifestyle influences (eg smoking).46–48 When reviewing outcomes from observational studies, it is critical that we are mindful of potential biases that may impact the data.46–48 For example, some real-life glaucoma studies compare treatment results against baseline measures, rather than a control/placebo arm, and regression to the mean issues should be considered when evaluating observational data.24,25,35,49 Compliance with medical regimens may also be improved following a treatment switch in observational studies, particularly when the subject has been selected for study inclusion due to poor tolerance with an existing therapy and is better able to tolerate the new medication.49 Nonetheless, data obtained from real-life clinical practice provides an important and valid contribution to the total body of evidence in any given therapy area.46–48 The aim of the current review is to provide a summary of published real-life data relating to the PF tafluprost/timolol FC, to inform evidence-based clinical practice for the benefit of patients with OAG/OHT.
IOP-Lowering Efficacy with PF Tafluprost/Timolol FC Therapy
Real-life IOP-lowering efficacy data reported in Phase IV studies and case series reflect data from published randomized and cross-over design trials examining treatment outcomes with PF tafluprost/timolol FC.18,19,22,24–35,42,43,45,50 A switch to PF tafluprost/timolol FC therapy has generally been associated with a significant reduction in mean IOP from baseline in patients with suboptimal IOP control under prior topical medication or IOP has been maintained for those people who were stable on their existing medication (but tolerating treatment poorly) before the change to PF tafluprost/timolol FC therapy was performed.25–32,34–36,38
Treatment Intensification to PF Tafluprost/Timolol FC Therapy from Topical Monotherapy
Figure 1 summarizes the mean change in IOP from baseline at the final study visit for patients with OAG/OHT who were switched to PF tafluprost/timolol FC treatment from commonly used monotherapies in three key real-life studies.24,25,32,35,50 As reported by Oddone et al (2020 and 2022; the VISIONARY study), Pillunat et al (2017) and Oddone et al (2024; the HERO study), IOP was significantly reduced from baseline at the final visit in each study after a switch from PGA or beta-blocker monotherapy to PF tafluprost/timolol FC.24,25,32,35,50 Improvement in IOP may, in part, have been due to greater compliance with treatment following a switch to the PF tafluprost/timolol FC.24,25,35,49 As discussed later in the article, IOP reduction was accompanied by enhanced tolerability with PF tafluprost/timolol, compared with prior medication, and data have indicated that patient-reported adherence was better when treatment was well-tolerated.24,25,33,35,49
 |
Figure 1 Mean IOP change from baseline at the final study visit for OAG/OHT patients previously treated with beta-blocker or PGA monotherapy who were switched to PF tafluprost/timolol FC therapy. Results from (A) the VISIONARY study, (B) Pillunat et al, (C) the HERO study.24,25,32,35,50 VISIONARY study: The full patient population was the full analysis set (FAS), which comprised all patients prescribed PF tafluprost/timolol FC treatment with at least 1 IOP measurement at Month 6. Pillunat et al: The full patient population used for the evaluation of efficacy and tolerability outcomes included all patients who were treated with the PF tafluprost/timolol FC as the only medication at the final visit. Hero study: Baseline monotherapy was preserved latanoprost. N = number of patients included in the analysis set/subgroup. Abbreviations: FC, fixed-dose combination; IOP, intraocular pressure; OAG, open-angle glaucoma; OHT, ocular hypertension; PF, preservative-free, PGA, prostaglandin analogue. |
The European, 6-month, prospective, multicenter VISIONARY study comprised the first and largest observational study specifically designed to mirror clinical practice, exploring treatment outcomes for OAG/OHT patients changing from a PGA or a beta-blocker monotherapy to the PF tafluprost/timolol FC without any washout period.25,31,32 The VISIONARY study was conducted in 577 patients with OHT/OAG attending 66 ophthalmology clinics in Italy, Hungary, Spain, Russia, the United Kingdom (UK), Latvia, Ireland, Norway, Denmark, the Netherlands and Sweden.25,31,32 The study showed that mean ± standard deviation (SD) IOP reduction from under baseline monotherapy was significant at all study visits: 5.4 ± 3.76 mmHg (23.7%) at Week 4, 5.9 ± 3.90 mmHg (25.6%) at Week 12, and 5.7 ± 4.11 mmHg (24.9%) at Month 6 (p<0.0001 for all visits).25 Given that the mean ± SD IOP under monotherapy was 21.5 (4.45) mmHg in the VISIONARY study population, the clinically significant IOP reductions observed from Week 4 through Month 6 with PF tafluprost/timolol FC therapy should be considered highly favorable.25 At Month 6, 69.2%, 53.6%, 40.0%, and 25.8% were responders based on ≥20%, ≥25%, ≥30%, and ≥35% cut-off values for mean IOP reduction from baseline, respectively, demonstrating that the majority of patients switching to PF tafluprost/timolol FC therapy from topical monotherapy in routine clinical practice should achieve IOP reductions of at least 20% within the first 6 months.25 Case series data (reported by Ansari et al, 2022) in patients with OAG and OHT switching from latanoprost (0.005%) or bimatoprost (0.03%) monotherapy to PF tafluprost/timolol FC reflected the VISIONARY study outcomes, with IOP being lowered from 18–24 mmHg to 14–16 mmHg during routine follow-up at ophthalmology clinics.33
Analysis of the VISIONARY data according to the monotherapy used at baseline revealed that IOP reductions from baseline at Week 4 were statistically and clinically significant and sustained through Month 6 (p<0.001) for all prior monotherapy subgroups (Table 1).32 Mean ± SD IOP change at Month 6 according to baseline treatment was 6.6 ± 4.16 mmHg (beta-blocker), 6.3 ± 4.39 mmHg (preserved latanoprost), 5.6 ± 3.67 mmHg (PF-latanoprost), 4.9 ± 2.97 mmHg (tafluprost), 4.6 ± 4.39 mmHg (bimatoprost), and 4.7 ± 3.64 mmHg (travoprost).32 The largest IOP change was observed in the subgroup treated with preserved latanoprost at baseline.32 For each of the ≥20%, ≥25%, ≥30%, and ≥35% IOP reduction categories at Month 6, prior preserved latanoprost users demonstrated respective reductions of 8.06, 9.20, 10.64, and 11.55 mmHg.32 Country-level VISIONARY study data indicated that stepping up to PF tafluprost/timolol FC from PGA or beta-blocker monotherapy resulted in IOP reductions from baseline that were clinically and statistically significant irrespective of the country (European region) where the data were collected, IOP at baseline, prior monotherapy, diagnosis or dosing time (p<0.0001).25–32 Country-level data showed that mean IOP reductions at Month 6 ranged from 5.0 mmHg (22.6%, Hungary) to 7.8 mmHg (31.8%, Latvia) and varied significantly between countries (p<0.001).31 In line with randomized study data, the greatest IOP reductions were found in those countries (Latvia and Russia) where baseline IOP under topical treatment was highest.31,42
 |
Table 1 VISIONARY Study Summary: Mean Change in IOP from Baseline Following a Switch to PF Tafluprost/Timolol FC therapy |
The potential influence of preservative agents on treatment outcomes has been highlighted across the literature and, as mentioned above, the VISIONARY study also showed that patients using preserved latanoprost at baseline achieved slightly higher mean IOP reductions with PF tafluprost/timolol FC therapy at Month 6 compared with prior PF-latanoprost users.12,32,51–53 The improvement in IOP observed when switching away from a preserved topical formulation may be associated with the lowering of ocular surface toxicity and inflammation and greater adherence with the new PF treatment regimen for patients who had tolerated the preserved formulation poorly.33,54–56 Recent randomized study data have highlighted the dual improvements observed in IOP reduction and severity of ocular surface toxicity markers that may accompany a switch away from preserved latanoprost to PF tafluprost when used as part of a triple glaucoma therapy regimen.57 In the real-world setting, a recent Phase IV, multicenter, prospective, interventional study (the HERO study) has explored 3-month treatment outcomes in clinical practice among OAG/OHT patients switching from preserved latanoprost to PF tafluprost/timolol FC treatment due to inadequate IOP control and presence of ocular surface disease (OSD) signs and symptoms.24 As seen in the VISIONARY population, HERO study participants demonstrated significant IOP reductions from baseline after the switch (p<0.001).24 The estimated mean 24-hour IOP was 17.8 mmHg at baseline and 15.3 mmHg at Month 3 (14% reduction; p<0.001).24 Mean daytime IOP was lowered from 16.9 mmHg under preserved latanoprost monotherapy to 14.6 mmHg (13.6% reduction; p<0.001) after 3 months of PF tafluprost/timolol FC therapy, and nighttime IOP was reduced from 19.4 mmHg to 16.5 mmHg (14.9% reduction; p<0.001).24 These data are reflective of the outcomes in the preserved latanoprost subgroup from the VISIONARY subanalysis, although the percentage IOP change at Month 3 was not as high in the HERO study (14%) as that seen in the VISIONARY study (25.6%) and could, perhaps, have been influenced by the lower baseline IOP under monotherapy in the HERO investigation.14,17,18,24,32
Studies conducted in Japan using a formulation of tafluprost/timolol FC containing low concentrations of BAK (0.001%) also revealed significant IOP reductions from Month 1 through Month 3 (p<0.001) following a switch away from PGA monotherapy or beta-blocker monotherapy.37–39 These data indicate that the combined effects of the constituent agents (tafluprost and timolol) convey powerful IOP-lowering efficacy.37–39 Stratification of data from the Takagi et al study revealed that mean ± SD IOP was reduced from 17.4 ± 4.0 mmHg under PGA monotherapy (latanoprost, travoprost, tafluprost or other PGA [not specified]) to 14.2 ± 3.3 mmHg at Month 3 with tafluprost/timolol FC treatment.37 Likewise, IOP was reduced from 16.7 ± 3.7 mmHg under beta-blocker monotherapy to 13.4 ± 3.1 mmHg at Month 3 with the tafluprost/timolol FC.37
Beyond the real-life studies relating to IOP-lowering outcomes in OAG/OHT patients moving to PF tafluprost/timolol FC therapy from PGA or beta-blocker monotherapies, observational data from the large, 16-week study conducted in Germany by Pillunat et al revealed significant IOP reductions at the final visit following a switch to PF tafluprost/timolol FC in a population that included patients using a broad selection of topical therapies at baseline (preserved and PF monotherapies, FC therapies and non-fixed combinations; p<0.001).35 When IOP-lowering efficacy was specifically examined by previous monotherapy type, Pillunat et al reported IOP reductions from baseline of 6.4 mmHg (alpha2-agonists), 5.7 mmHg (beta-blockers), 5.2 mmHg (carbonic anhydrase inhibitors [CAIs]) and 4.7 mmHg (PGAs).35
Switching from Other FC Therapies to PF Tafluprost/Timolol FC
Figure 2 shows IOP-lowering efficacy with PF tafluprost/timolol FC therapy in patients with OAG/OHT switching from other PGA/beta-blocker FC treatments and various different FC therapies, as reported by Pillunat et al.35 Of the 238 individuals who were switched from FC therapy to PF tafluprost/timolol FC treatment, 163 were using PGA/beta-blocker FC treatments at baseline and the mean ± SD IOP was lowered from 19.1 ± 4.1 mmHg prior to the switch to 16.7 ± 3.1 mmHg at the final visit (12.7% reduction; p<0.001) in this subgroup.35 Further analysis by individual baseline FC therapy revealed that significant IOP reductions from baseline were observed at the final study visit in patients switching from latanoprost/timolol FC (p<0.001) or bimatoprost/timolol FC (p<0.001) to PF tafluprost/timolol FC.35 Patients previously using CAI/beta-blocker FC formulations showed mean IOP reductions from baseline of 19.3% at the final study visit (p<0.001).35 The mean IOP reduction among users of “other” FC therapies at baseline was 26.7% at the final visit (although patient numbers were low in this subgroup [n=9]).35 The majority of participants in the Pillunat et al study (72%) had switched to PF tafluprost/timolol FC treatment due to insufficient IOP control on prior therapy and this is probably the reason that significant additional IOP-lowering efficacy was observed following the change in topical therapy.35 In contrast, a 12-week, open-label multicenter European study, conducted by Bourne et al, provided evidence that patients with OAG/OHT who had a stable IOP on bimatoprost/timolol FC therapy (but were experiencing tolerability issues) maintained their IOP control when switching to PF tafluprost/timolol FC treatment.34 The change in topical treatment was associated with improvements in tolerability outcomes, which are discussed later in this review.34
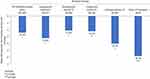 |
Figure 2 Pillunat et al: mean change in IOP from baseline at the final study visit for patients switching to PF tafluprost/timolol FC therapy from prior PGA/beta-blocker FC therapies, CAI/beta-blocker FCs and other FC therapies.35 N = number of patients included in the analysis set/subgroup. Abbreviations: CAI, carbonic anhydrase inhibitor; FC, fixed-dose combination; IOP, intraocular pressure; PF, preservative-free, PGA, prostaglandin analogue. |
Switching from Multiple Topical Therapies to PF Tafluprost/Timolol FC
Interestingly, the Pillunat et al study showed that a change to PF tafluprost/timolol FC therapy from multiple non-fixed combinations of PGA/beta-blocker treatments (p<0.001) or concomitant CAI and beta-blocker therapies (p=0.007) may support significant IOP reductions of up to 14.4% and 17.6%, respectively, in clinical practice.35 In addition, in the same study, participants treated with three individual active agents at baseline significantly reduced their IOP with PF tafluprost/timolol FC therapy (14.3%; p=0.005).35 Case series data from Ansari et al have also highlighted the IOP-lowering benefits that may accompany the simplification of treatment when a patient with OAG/OHT fails to tolerate administration of multiple individual topical agents or maximal therapy.33 In those cases presented, combination treatment regimens comprising PGA, beta-blocker, CAI and alpha-2 agonist agents (including preserved formulations) had resulted in patients showing OSD signs and symptoms, elevated IOP values (≥23 mmHg) and wide fluctuations in pressure (ranging between 11–20 mmHg).33 However, treatment to address tolerability issues and simplification of the therapeutic regimen using the PF tafluprost/timolol FC helped to improve overall treatment outcomes and achieve lower, stable IOP (≤18 mmHg) outcomes.33
Real-Life Studies: Tolerability and Safety Outcomes with PF Tafluprost/Timolol FC
Indicators of Tolerability
Tolerability is a critical factor in glaucoma management that can impact treatment adherence and, therefore, therapeutic outcomes.2,53,54,56,58,59 Toxicities that affect the ocular surface, causing discomfort and affecting QoL, can result in poor compliance with the treatment regimen.2,53,54,56,58,59 Adherence is particularly important for chronic conditions such as glaucoma that require long-term perseverance with medications.2,53,56,59 Improvements in IOP-lowering efficacy demonstrated in observational studies and clinical case series have typically been accompanied by enhanced tolerability outcomes compared with prior therapy, regardless of the previous treatment used.25,31–35 Improvements in IOP may, in part, be due to better treatment adherence and/or compliance, as highlighted by Ansari et al in their case series.33 Patients who admitted to poor adherence with prior treatment, due to tolerability issues, reported better compliance when their treatment was switched to PF tafluprost/timolol FC therapy and seemed to tolerate topical therapy more effectively after the switch.33 Observational data from Germany provide further supportive evidence concerning the tolerability profile of the PF tafluprost/timolol FC in real-life studies.35 Of the 1157 people assessed for safety outcomes, just one (0.1%) terminated PF tafluprost/timolol FC treatment due to poor compliance.35 Twelve of the 577 patients included in VISIONARY study discontinued treatment as a result of poor local tolerance.25
Assessment of the signs and symptoms of OSD and ocular health can provide a good indication of a patient’s tolerance to their ongoing topical glaucoma treatment regimen. Real-life study evidence published to date suggests that a switch to PF tafluprost/timolol FC therapy from other topical treatments may result in improvements in the indicators of ocular surface health.24,25,32,34,35 Figure 3 provides a summary of the change in conjunctival hyperemia severity reported in the VISIONARY, Pillunat et al and HERO studies for patients stepping up from PGA monotherapy to PF tafluprost/timolol FC therapy.24,25,35 The VISIONARY study showed that severity of conjunctival hyperemia was significantly lowered at all study visits following a switch from monotherapy to PF tafluprost/timolol FC treatment (p<0.0001 at each visit).25 Reduction in conjunctival hyperemia was statistically significant at all study visits for participants treated with each of the baseline PGA monotherapies; latanoprost (p<0.0001), tafluprost (p=0.029), bimatoprost (p<0.0001), and travoprost (p<0.0001).25 When exploring data for the prior latanoprost subgroup in more detail, preserved latanoprost users experienced significant lowering in conjunctival hyperemia severity at each study visit following a switch to PF tafluprost/timolol FC therapy (p<0.001) while, in contrast, reductions in conjunctival hyperemia did not reach statistical significance in the prior PF-latanoprost subgroup (p=0.148).32 Despite subjective symptoms being generally absent or of mild severity at baseline in the VISIONARY study, severity scores of ocular health indicators were significantly reduced at Month 6, including symptoms of dry eye, irritation, itching, and foreign body sensation (p<0.001 for each parameter).25 Significant improvements were observed across the VISIONARY study population concerning the severity of corneal fluorescein staining (CFS; Oxford Grade Scale; p<0.0001). Improvements in CFS grade for patients previously treated with PGA monotherapies were largely driven by those seen in the prior bimatoprost subgroup, in which CFS score was significantly reduced at Month 6 (p=0.0013).32 The Bourne et al study also suggested that bimatoprost may be associated with some ocular surface tolerability issues.34 Patients receiving either preserved or PF formulations of bimatoprost/timolol FC who presented with signs and symptoms of OSD experienced benefit from switching to PF tafluprost/timolol FC.34 After a change to the PF tafluprost/timolol FC, patients treated with bimatoprost/timolol FC at screening showed significant improvements in conjunctival hyperemia and the severity of their worst ocular symptom (p<0.001).34 Signs and symptoms were improved early after the switch, from Week 2, and were sustained through Weeks 6 and 12.34 These results indicate that the PGA agent used may contribute to tolerability outcomes in addition to the presence of preservative agent.34
 |
Figure 3 The change from baseline in the severity of conjunctival hyperemia for OAG/OHT patients previously treated with PGA monotherapy who were switched to PF tafluprost/timolol FC therapy. Results from (A) the VISIONARY study, (B) Pillunat et al, (C) the HERO study.24,25,32,35,50 VISIONARY study: Change from baseline in conjunctival hyperemia severity at the final visit according to prior PGA monotherapy used: preserved latanoprost p<0.001, PF latanoprost p=0.148, tafluprost p=0.029, bimatoprost p<0.0001, and travoprost p<0.0001. N=416. Pillunat et al: Change from baseline in conjunctival hyperemia severity at the final visit: p<0.001. N=338. HERO study: Change from baseline in conjunctival hyperemia severity at the final visit: p<0.001. N=38. Abbreviations: FC, fixed-dose combination; IOP, intraocular pressure; OAG, open-angle glaucoma; OHT, ocular hypertension; PF, preservative-free, PGA, prostaglandin analogue. |
Pillunat et al reported significant reductions in conjunctival hyperemia and conjunctival staining among patients switching to PF tafluprost/timolol FC from all prior medications (p<0.01) as well as those subgroups previously treated with PGA monotherapy (p<0.001) and PGA/timolol FC therapies (p<0.01).35 The severity grade of lid-parallel conjunctival folds (LIPCOF) was significantly lowered among patients on all prior medications (p<0.001) and in those subgroups previously treated with a PGA monotherapy (p<0.05) or PGA/timolol FC therapies (p<0.001).35
Oddone et al reported that hyperemia and corneal staining were significantly reduced at Month 3 during their 24-hour IOP study comparing PF tafluprost/timolol FC treatment outcomes with those of baseline preserved latanoprost monotherapy.24,50 Overall, 52.6% of participants had a 2-grade reduction in corneal staining score (Oxford Grade Scale), with the percentage of patients showing none/minimal corneal staining increasing from 68.4% at baseline to 92.1% at Month 3 (p<0.03).24,50 Hyperemia severity was improved from baseline in 63.3% of participants at Month 3 (p<0.001).24,50 Of the 11 (28.9%) patients who had blepharitis at baseline, 4 (10.5%) had recovered at Month 3 after initiating PF tafluprost/timolol FC therapy.24,50 HERO study participants reported significant lowering of mean 5-item dry eye questionnaire (DEQ-5) scores compared with baseline (DEQ-5 score: 8.29) after 3 months of PF tafluprost/timolol FC therapy (DEQ-5 score: 6.13; p=0.002) as result of reduced ocular symptoms.24,50
The reductions in severity of conjunctival hyperemia and other indicators of ocular surface health demonstrated in real-life studies support the findings of randomized studies examining treatment outcomes with the PF tafluprost/timolol FC.19,24,25,34–36,42
Safety Outcomes
Overall, the PF tafluprost/timolol FC has demonstrated a favorable safety profile in a real-life setting and the majority of outcomes reflect those from published randomized trials.18,19,22,24–36,42,43,45 Treatment-related adverse events (AEs) reported during the VISIONARY study were mild to moderate in severity, and the majority had resolved or were resolving at the end of the study period.25 Unsurprisingly, as the study treatment was a topical medication, 50 (72.5%) of the 69 treatment-related AEs were ocular events, with the most common being eye pain (23 events).25 AEs reported in the Pillunat et al study were also typically local ocular events (affecting 2.5% of the study population), the most common of which being burning (0.5%) and hyperemia (0.3%).35 During the HERO study (Oddone et al, 2024), the only reported AE comprised one non-serious case of new onset moderate blepharitis, which was considered likely to be related to the study treatment.24,50
Compliance with Treatment and Patient-Reported Tolerability in Real-Life Studies
As discussed by Ansari et al in their OAG and OHT patient case series publication, improvements in IOP-lowering outcomes may typically be accompanied by enhanced patient-reported compliance or adherence with the PF tafluprost/timolol FC treatment regimen.33 The VISIONARY study demonstrated physician-reported improvements in treatment compliance at Month 6, following a switch to PF tafluprost/timolol FC, compared with prior PGA or beta-blocker monotherapy.25,32 Enhancements in compliance were accompanied by reassuring patient-reported tolerability outcomes, with the majority indicating tolerability with PF tafluprost/timolol FC therapy to be good or very good in the VISIONARY study (91.4% at Month 6), regardless of the prior monotherapy used.25,32 Patients included in the Pillunat et al study also reported tolerability to be good/very good (90.6%) at the final visit.35
Achieving a Balance of Powerful IOP-Lowering Efficacy and Long-Term Tolerability and Safety
Real-life studies have shown that patients with OAG and OHT who require a switch to PGA/timolol FC for further IOP reduction or due to tolerability issues with prior treatment can achieve additional and clinically significant IOP reductions and, at the same time, substantial improvements in ocular tolerance when changing from their existing topical glaucoma therapy to the PF tafluprost/timolol FC.24,25,31–33,35,50 Real-life clinical studies to date have typically examined PF tafluprost/timolol FC treatment outcomes following a switch from PGA or beta-blocker monotherapy or fixed/unfixed combination therapies, including PGA/beta-blocker and CAI/beta-blocker therapies.24,25,31–33,35,37,50
While the limitations of observational studies should be considered, the evidence base regarding the treatment of OAG/OHT with the PF tafluprost/timolol FC has evolved and expanded rapidly during recent years, and efficacy and safety data from real-life studies reflect the published outcomes from randomized trials.18,19,22,24–35,42,43,45–49 Real-life studies have generally reported relatively few treatment-related AEs with PF tafluprost-timolol FC, with most being ocular events of mild to moderate intensity, and a minority have led to discontinuation of treatment.24,25,35,50 This is also mirrored by the patient-reported tolerability data.24,25,32–34,50 These insights should provide additional confidence for clinicians regarding the treatment outcomes that they may expect when initiating PF tafluprost/timolol FC use in their own clinics, whether they are aiming to intensify or simplify the OAG/OHT therapeutic regimen or address ongoing tolerability issues with existing topical medications.
Acknowledgments
Medical writing services were provided on behalf of the authors by Rebecca Down at Copperfox Communications Limited.
Funding
Funding for medical writing services and publication fees was provided by Santen SA, Geneva, Switzerland.
Disclosure
Gábor Holló has received consultancy and lecturing fees from Santen and consultancy fees from Thea. The author reports no other conflicts of interest in this work.
References
1. Chun YS, Sung KR, Park CK, et al. Factors influencing vision‐related quality of life according to glaucoma severity. Acta Ophthalmol. 2019;97(2). doi:10.1111/aos.13918
2. Quaranta L, Riva I, Gerardi C, Oddone F, Floriani I, Konstas AGP. Quality of life in glaucoma: a review of the literature. Adv Ther. 2016;33(6):959–981. doi:10.1007/s12325-016-0333-6
3. Janz NK, Wren PA, Lichter PR, et al. The collaborative initial glaucoma treatment study: interim quality of life findings after initial medical or surgical treatment of glaucoma. Ophthalmology. 2001;108(11):1954–1965. doi:10.1016/s0161-6420(01)00874-0
4. European Glaucoma Society. Terminology and guidelines for glaucoma, 5th edition. Br J Ophthalmol. 2021;105:1–169. doi:10.1136/bjophthalmol-2021-egsguidelines
5. Collaborative Normal-Tension Glaucoma Study Group. The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Am J Ophthalmol. 1998;126(4):498–505. doi:10.1016/s0002-9394(98)00272-4.
6. International Council of Ophthalmology. Guidelines for glaucoma care; 2016. Available from: https://icoph.org/eye-care-delivery/glaucoma/.
7. The AGIS Investigators. The advanced glaucoma intervention study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130(4):429–440. doi:10.1016/s0002-9394(00)00538-9.
8. Holló G, Hommer A. Delivery of glaucoma care committee of the European glaucoma society. The status of glaucoma diagnostics and care in Europe in 2015: a European survey. Eur J Ophthalmol. 2016;26(3):216–220. doi:10.5301/ejo.5000699
9. Aptel F, Cucherat M, Denis P. Efficacy and tolerability of prostaglandin-timolol fixed combinations: a meta-analysis of randomized clinical trials. Eur J Ophthalmol. 2012;22(1):5–18. doi:10.5301/ejo.5000009
10. Holló G, Topouzis F, Fechtner RD. Fixed-combination intraocular pressure-lowering therapy for glaucoma and ocular hypertension: advantages in clinical practice. Expert Opin Pharmacother. 2014;15(12):1737–1747. doi:10.1517/14656566.2014.936850
11. Quaranta L, Biagioli E, Riva I, et al. Prostaglandin analogs and timolol-fixed versus unfixed combinations or monotherapy for open-angle glaucoma: a systematic review and meta-analysis. J Ocul Pharmacol Ther. 2013;29(4):382–389. doi:10.1089/jop.2012.0186
12. Pisella PJ, Pouliquen P, Baudouin C. Prevalence of ocular symptoms and signs with preserved and preservative free glaucoma medication. Br J Ophthalmol. 2002;86(4):418–423. doi:10.1136/bjo.86.4.418
13. Aguayo Bonniard A, Yeung JY, Chan CC, Birt CM. Ocular surface toxicity from glaucoma topical medications and associated preservatives such as benzalkonium chloride (BAK). Expert Opin Drug Metab Toxicol. 2016;12(11):1279–1289. doi:10.1080/17425255.2016.1209481
14. Holló G, Katsanos A, Boboridis KG, Irkec M, Konstas AGP. Preservative-free prostaglandin analogs and prostaglandin/timolol fixed combinations in the treatment of glaucoma: efficacy, safety and potential advantages. Drugs. 2018;78(1):39–64. doi:10.1007/s40265-017-0843-9
15. Figus M, Agnifili L, Lanzini M, et al. Topical preservative-free ophthalmic treatments: an unmet clinical need. Expert Opin Drug Deliv. 2021;18(6):655–672. doi:10.1080/17425247.2021.1860014
16. Holló G, Katsanos A, Boboridis K G, Irkec M, Konstas AG. Letter to the editor: “topical preservative-free ophthalmic treatments an unmet clinical need”. Expert Opin Drug Deliv. 2021;18(4):527–529. doi:10.1080/17425247.2021.1898866
17. Tabet R, Stewart WC, Feldman R, Konstas AGP. A review of additivity to prostaglandin analogs: fixed and unfixed combinations. Surv Ophthalmol. 2008;53 Suppl1:S85–92. doi:10.1016/j.survophthal.2008.08.011
18. Hoy SM. Tafluprost/timolol: a review in open-angle glaucoma or ocular hypertension. Drugs. 2015;75(15):1807–1813. doi:10.1007/s40265-015-0476-9
19. Holló G, Katsanos A. Safety and tolerability of the tafluprost/timolol fixed combination for the treatment of glaucoma. Expert Opin Drug Saf. 2015;14(4):609–617. doi:10.1517/14740338.2015.1010507
20. Holló G, Hommer A, Antón López A, Ropo A. Efficacy, safety, and tolerability of preservative-free fixed combination of tafluprost 0.0015%/timolol 0.5% versus concomitant use of the ingredients. J Ocul Pharmacol Ther. 2014;30(6):468–475. doi:10.1089/jop.2013.0229
21. Lorenz K, Pfeiffer N. Efficacy and safety of tafluprost 0.0015% and timolol maleate 0.5% fixed combination in patients with ocular hypertension or open-angle glaucoma. Expert Opin Pharmacother. 2014;15(15):2255–2262. doi:10.1517/14656566.2014.955471
22. Pfeiffer N, Traverso CE, Lorenz K, et al. A 6-month study comparing efficacy, safety, and tolerability of the preservative-free fixed combination of tafluprost 0.0015% and timolol 0.5% versus each of its individual preservative-free components. Adv Ther. 2014;31(12):1228–1246. doi:10.1007/s12325-014-0163-3
23. Suzuki K, Otsuka N, Hizaki H, Hashimoto M, Kuwayama Y, Tafluprost/Timolol Versus Latanoprost/Timolol (TTVLT) Study Group. Multicenter, randomized, controlled study comparing tafluprost/timolol fixed combination with latanoprost/timolol fixed combination in primary open-angle glaucoma and ocular hypertension. Adv Ther. 2018;35(6):796–808. doi:10.1007/s12325-018-0718-9
24. Oddone F, Tanga L, Giammaria S, et al. 24-hour evaluation of the effectiveness and tolerability of preservative-free tafluprost-timolol fixed combination in glaucoma or ocular hypertensive patients previously treated with preserved latanoprost. Clin Ophthalmol. 2024;18:1751–1760. doi:10.2147/OPTH.S462672
25. Oddone F, Tanga L, Kóthy P, Holló G, VISIONARY Study Group. Treatment of open-angle glaucoma and ocular hypertension with preservative-free tafluprost/timolol fixed-dose combination therapy: the VISIONARY study. Adv Ther. 2020;37(4):1436–1451. doi:10.1007/s12325-020-01239-8
26. Ansari E, Pavicic-Astalos J, Ayan F, et al. Treatment of open-angle glaucoma and ocular hypertension with preservative-free tafluprost/timolol fixed-dose combination therapy: UK and Ireland results from the VISIONARY study. Adv Ther. 2021;38(6):2990–3002. doi:10.1007/s12325-021-01725-7
27. Garcia-Medina JJ, Benitez-Del-Castillo J, Rodríguez-Agirretxe I, Lopez-Lopez F, Moreno-Valladares A, VISIONARY Study Group (Spain). Treatment of open-angle glaucoma and ocular hypertension with preservative-free tafluprost/timolol fixed-dose combination therapy: results from the VISIONARY study population in Spain. J Ocul Pharmacol Ther. 2022;38(3):252–260. doi:10.1089/jop.2021.0099
28. Oddone F, Scorcia V, Iester M, et al. Treatment of open-angle glaucoma and ocular hypertension with the fixed-dose combination of preservative-free tafluprost/timolol: clinical outcomes from ophthalmology clinics in Italy. Clin Ophthalmol. 2022;16:1707–1719. doi:10.2147/OPTH.S364880
29. Karlova EV, Petrov SY, Germanova VN. Preservative-free fixed combination in the treatment of open-angle glaucoma and ocular hypertension: the VISIONARY study (EUPAS22204). Vestn Oftalmol. 2020;136(4):76–84. doi:10.17116/oftalma202013604176
30. Holló G, Kóthy P, the Hungarian VISIONARY investigators. The Hungarian VISIONARY study: Hungarian results in the European multicenter preservative-free tafluprost/timolol fixed combination investigation. Ophthalmologica Hungarica. 2020;57:196–201.
31. Holló G, Kirwan J, Lopez-Lopez F, et al. A comparison of country-level data from the VISIONARY study examining treatment outcomes with preservative-free tafluprost/timolol fixed-dose combination therapy. Curr Med Res Opin. 2022;38(7):1189–1201. doi:10.1080/03007995.2022.2083324
32. Oddone F, Kirwan J, Lopez-Lopez F, et al. Switching to preservative-free tafluprost/timolol fixed-dose combination in the treatment of open-angle glaucoma or ocular hypertension: subanalysis of data from the VISIONARY study according to baseline monotherapy treatment. Adv Ther. 2022;39(8):3501–3521. doi:10.1007/s12325-022-02166-6
33. Ansari E, Chappiti S, Pavicic-Astalos J, et al. Treatment of open-angle glaucoma and ocular hypertension with preservative-free tafluprost/timolol fixed-dose combination therapy: 6 case reports and clinical outcomes. BMC Ophthalmol. 2022;22(1):152. doi:10.1186/s12886-022-02361-7
34. Bourne RRA, Kaarniranta K, Lorenz K, Traverso CE, Vuorinen J, Ropo A. Changes in ocular signs and symptoms in patients switching from bimatoprost-timolol to tafluprost-timolol eye drops: an open-label phase IV study. BMJ Open. 2019;9(4):e024129. doi:10.1136/bmjopen-2018-024129
35. Pillunat LE, Erb C, Ropo A, Kimmich F, Pfeiffer N. Preservative-free fixed combination of tafluprost 0.0015% and timolol 0.5% in patients with open-angle glaucoma and ocular hypertension: results of an open-label observational study. Clin Ophthalmol. 2017;11:1051–1064. doi:10.2147/OPTH.S128453
36. Oddone F. Reviewing the evidence surrounding preservative-free tafluprost/timolol fixed-dose combination therapy in open-angle glaucoma and ocular hypertension management: a focus on efficacy, safety, and tolerability. Expert Opin Drug Saf. 2022;21(10):1259–1268. doi:10.1080/14740338.2022.2135701
37. Takagi Y, Osaki H, Yamashita T, Kai Y. Prospective observational post-marketing study of tafluprost 0.0015%/timolol 0.5% combination ophthalmic solution for glaucoma and ocular hypertension: short-term efficacy and safety. Ophthalmol Ther. 2016;5(2):191–206. doi:10.1007/s40123-016-0057-3
38. Inoue K, Kawashima T, Katakura S, et al. Switching from concomitant therapy to tafluprost/timolol fixed combination. Clin Ophthalmol. 2018;12:549–554. doi:10.2147/OPTH.S150595
39. Kitamura K, Chiba T, Mabuchi F, et al. Efficacy and safety of switching prostaglandin analog monotherapy to tafluprost/timolol fixed-combination therapy. J Ophthalmol. 2018;2018:1–9. doi:10.1155/2018/8456764
40. Fuwa M, Ueda K, Akaishi T, et al. Advantages of efficacy and safety of fixed-dose tafluprost/timolol combination over fixed-dose latanoprost/timolol combination. PLoS One. 2016;11(7):e0158797. doi:10.1371/journal.pone.0158797
41. Okumichi H, Kiuchi Y, Baba T, et al. The signs of ocular-surface disorders after switching from latanoprost to tafluprost/timolol fixed combination: a prospective study. Clin Ophthalmol. 2017;11:1175–1181. doi:10.2147/OPTH.S136418
42. Holló G, Vuorinen J, Tuominen J, Huttunen T, Ropo A, Pfeiffer N. Fixed-dose combination of tafluprost and timolol in the treatment of open-angle glaucoma and ocular hypertension: comparison with other fixed-combination products. Adv Ther. 2014;31(9):932–944. doi:10.1007/s12325-014-0151-7
43. Konstas AG, Katsanos A, Athanasopoulos GP, et al. Preservative-free tafluprost/timolol fixed combination: comparative 24-h efficacy administered morning or evening in open-angle glaucoma patients. Expert Opin Pharmacother. 2018;19(18):1981–1988. doi:10.1080/14656566.2018.1534958
44. Rolle T, Spinetta R, Nuzzi R. Long term safety and tolerability of tafluprost 0.0015% vs timolol 0.1% preservative-free in ocular hypertensive and in primary open-angle glaucoma patients: a cross sectional study. BMC Ophthalmol. 2017;17(1):136. doi:10.1186/s12886-017-0534-z
45. Kaarniranta K, Ikäheimo K, Mannermaa E, Ropo A. Pharmacokinetics, efficacy, and safety of the preservative-free fixed combination of tafluprost 0.0015% and timolol 0.5% in healthy volunteers: a Phase I comparison vs. the corresponding preservative-free monotherapies. Clin Pharmacokinet. 2016;55(4):485–494. doi:10.1007/s40262-015-0331-x
46. Schad F, Thronicke A. Real-world evidence—current developments and perspectives. Int J Environ Res Public Health. 2022;19(16):10159. doi:10.3390/ijerph191610159
47. Dang A. Real-world evidence: a primer. Pharmaceut Med. 2023;37(1):25–36. doi:10.1007/s40290-022-00456-6
48. Fernainy P, Cohen AA, Murray E, Losina E, Lamontagne F, Sourial N. Rethinking the pros and cons of randomized controlled trials and observational studies in the era of big data and advanced methods: a panel discussion. BMC Proc. 2024;18(Suppl 16):18. doi:10.1186/s12919-023-00285-8
49. Tapply I, Broadway DC. Improving adherence to topical medication in patients with glaucoma. Patient Prefer Adherence. 2021;15:1477–1489. doi:10.2147/PPA.S264926
50. Tanga L, Oddone F, Carnevale C, et al. 24-hour efficacy and tolerability of the fixed combination tafluprost/timolol without preservatives in glaucoma or ocular hypertensive patients. Prospective multicenter study lasting 3 months (HERO study) [Italian].
51. Jaenen N, Baudouin C, Pouliquen P, Manni G, Figueiredo A, Zeyen T. Ocular symptoms and signs with preserved and preservative-free glaucoma medications. Eur J Ophthalmol. 2007;17(3):341–349. doi:10.1177/112067210701700311
52. Boimer C, Birt CM. Preservative exposure and surgical outcomes in glaucoma patients: the PESO study. J Glaucoma. 2013;22(9):730–735. doi:10.1097/IJG.0b013e31825af67d
53. Aptel F, Denis P. Balancing efficacy and tolerability of prostaglandin analogues and prostaglandin-timolol fixed combinations in primary open-angle glaucoma. Curr Med Res Opin. 2011;27(10):1949–1958. doi:10.1185/03007995.2011.613923
54. Pérez-Bartolomé F, Martínez-de-la-Casa JM, Arriola-Villalobos P, Fernández-Pérez C, Polo V, García-Feijoó J. Ocular surface disease in patients under topical treatment for glaucoma. Eur J Ophthalmol. 2017;27(6):694–704. doi:10.5301/ejo.5000977
55. Dubrulle P, Labbé A, Brasnu E, et al. Influence of treating ocular surface disease on intraocular pressure in glaucoma patients intolerant to their topical treatments: a report of 10 cases. J Glaucoma. 2018;27(12):1105–1111. doi:10.1097/IJG.0000000000001041
56. Mylla Boso AL, Gasperi E, Fernandes L, Costa VP, Alves M. Impact of ocular surface disease treatment in patients with glaucoma. Clin Ophthalmol. 2020;14:103–111. doi:10.2147/OPTH.S229815
57. Konstas AG, Boboridis KG, Athanasopoulos GP, et al. Changing from preserved, to preservative-free cyclosporine 0.1% enhanced triple glaucoma therapy: impact on ocular surface disease-A randomized controlled trial. Eye. 2023;37(17):3666–3674. doi:10.1038/s41433-023-02578-w
58. Rossi GCM, Pasinetti GM, Scudeller L, Radaelli R, Bianchi PE. Do adherence rates and glaucomatous visual field progression correlate? Eur J Ophthalmol. 2011;21(4):410–414. doi:10.5301/EJO.2010.6112
59. Nijm LM, De Benito-Llopis L, Rossi GC, Vajaranant TS, Coroneo MT. Understanding the dual dilemma of dry eye and glaucoma: an international review. Asia Pac J Ophthalmol. 2020;9(6):481–490. doi:10.1097/APO.0000000000000327
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

