Back to Journals » Clinical Interventions in Aging » Volume 20
Falls, Sleep Disorders and Cognitive Frailty in Hospitalized Older Adults with Hypertension:A Cross-Sectional Study
Authors Li X , Li H , Gan S , Zhang Y, Yin D , Zhu B , Wang S, Liu Y
Received 7 December 2024
Accepted for publication 4 June 2025
Published 17 June 2025 Volume 2025:20 Pages 859—872
DOI https://doi.org/10.2147/CIA.S510228
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Maddalena Illario
Xiaoyan Li,1 Huizhen Li,2 Shibao Gan,3 Youran Zhang,1 Dianhe Yin,1 Baihui Zhu,1 Shiyi Wang,1 Yuru Liu1
1Department of Geriatrics, Huaihe Hospital of Henan University, Kaifeng, Henan Province, People’s Republic of China; 2Department of Pulmonary Medicine, Kaifeng People’s Hospital, Kaifeng, Henan Province, People’s Republic of China; 3Department of Gastroenterology, Huaihe Hospital of Henan University, Kaifeng, Henan Province, People’s Republic of China
Correspondence: Yuru Liu, Department of Geriatrics,Huaihe Hospital of Henan University, No. 115, Ximen Street, Longting District, Kaifeng, Henan Province, People’s Republic of China, Tel +86 136 9390 9362, Email [email protected]
Purpose: Falls and fall-related injuries are highly prevalent among older adults. Falls negatively impact functional independence and quality of life, and are associated with increased morbidity, mortality, and healthcare costs. Sleep disorders in the older adults are a common phenomenon, with sleep quality gradually deteriorating as age increases. Cognitive frailty(CF) refers to the presence of both physical frailty(PF) and mild cognitive impairment(MCI) without simultaneous diagnosis of Alzheimer’s disease(AD) or other dementia. Epidemiological studies have confirmed the association between falls and sleep disorders, as well as CF. However, no studies have yet investigated the relationship between falls, sleep disorders and CF in hospitalized older adults with hypertension. Our study is to explore the relationship between falls and both sleep disorders and CF in hospitalized older adults with hypertension, providing a basis for fall prevention.
Patients and Methods: Demographic characteristics were collected from hypertensive patients aged 65 and above who were hospitalized in the Department of Geriatrics at Huaihe Hospital of Henan University, from July 2022 to June 2024. These patients were assessed for history of falls, sleep quality, CF, depression and nutritional status. Logistic regression analysis was used to examine the correlation between falls and both sleep disorders and CF.
Results: A total of 266 older adults with hypertension were surveyed in this study, of whom 108 reported having fallen once or more in the past year. Both sleep disorders and CF were significantly associated with an increased risk of falls (sleep disorders: OR=2.625, 95% CI 1.214– 5.678, P=0.014; CF: OR=5.920, 95% CI 2.632– 13.314, P< 0.001). Other significant risk factors included: Age (OR=1.119, 95% CI 1.055– 1.188, P< 0.001), Comorbidities (OR=2.855, 95% CI 1.353– 6.024, P=0.006), Polypharmacy (OR=4.126, 95% CI 1.937– 8.793, P< 0.001), Compared to hospitalized older adults with hypertension with good nutritional status, those with malnutrition had a 4.698-fold higher risk of falls (95% CI 1.724– 12.800, P=0.002).
Conclusion: The incidence of falls was higher among hospitalized older adults with hypertension. Both sleep disorders and CF were strongly associated with falls in this patient population.
Keywords: falls, sleep disorders, CF, hospitalization, older adults, hypertension
Introduction
Falls refer to an event that causes a person to inadvertently rest on the ground, floor or other lower level. According to the International Classification of Diseases,10th Revision (ICD-10), falls are categorized into two types (World Health Organization, 2008): (1) falls from one surface to another, (2) falls within the same surface. Research has shown that the fall incidence rate among elderly people in the United Kingdom is 30%.1 In the United States, 27.5% of community-dwelling adults 65 years or older reported at least 1 fall in the past year (714 falls per 1000 older adults) and 10.2% reported a fall-related injury (170 fall-related injuries per 1000 older adults) in 2018.2 In 2019, in mainland China, the incidence rate of falls among people aged 60 years and older was 3799.4 (95% uncertainty interval [UI] 3062.4–4645.0) new falls per 100000 population, and 39.2 deaths (21.8–48.8) per 100000 population and 1238.9 DALYs (920.5–1553.2) per 100000 population were due to falls.3 Each year, one-third of adults aged 65 and older, and half of those over 80, experience falls.4 Studies have found that elderly individuals with hypertension have an increased risk of falling.5 Falls not only impact the quality of life of elderly individuals but also extend their hospitalization time, imposing a heavy economic burden on their families. In the United States, medical expenses related to falls are estimated to approach $50 billion annually.6 Scholars have conducted extensive research on the risk factors for falls, including gender, age, muscle weakness, gait and balance disorders, vision impairment, foot or ankle joint diseases, history of falls, fear of falling, polypharmacy and more.4 Early identification of fall-related risk factors can help identify individuals who may benefit from appropriate interventions and prevent future injuries.
As people age, their physiological functions gradually decline, including changes in circadian rhythms and sleep structure, which ultimately lead to a decrease in sleep quality and the onset of sleep disorders.7 A multinational study on health aging and retirement conducted in 16 European countries among individuals aged 50 and above revealed that sleep problems are highly prevalent among older Europeans, with the prevalence ranging from 16.6% in Denmark and Italy to 31.2% in Poland.8 In addition, the US National Health and Aging Trends Study (NHATS) found that 28% of participants aged 65 and older reported poor sleep quality.9 A sleep survey in Japan among individuals with diabetes aged over 65 found a prevalence of sleep disorders of 44.8%.10 Multiple studies have shown that sleep disorders are associated with falls in the elderly and are a significant risk factor for falls.11 A study evaluating sleep quality among Chinese elderly people using the Pittsburgh Sleep Quality Index (PSQI) found that poor sleep quality was associated with an increased risk of falls and recurrent falls.12 Additionally, several components of the sleep quality assessment (sleep quality factor, sleep latency factor, sleep efficiency factor and sleep disturbance factor) were consistently associated with falls and recurrent falls.13 The Brassington study found that after controlling for other risk factors, difficulties falling asleep, waking up during the night, and early morning awakenings with an inability to fall back asleep were all linked to both the occurrence and frequency of falls in the elderly.14
With the aging population, diseases related to aging, such as frailty and cognitive decline, have significantly increased. In recent years, it has been observed that frailty and cognitive impairment are common among older adults, and their interaction forms a vicious cycle, ultimately contributing to the onset of CF.15 In 2013, a consensus expert group from the International Academy on Nutrition and Aging (IANA) and the International Association of Gerontology and Geriatrics (IAGG) first defined CF as: (1) the simultaneous presence of PF and MCI (Clinical Dementia Rating [CDR] = 0.5); (2) excluding diagnosed AD or other dementias.16 Research has shown that cognitive impairment and frailty increase the risk of falls,17–20 and CF better predicts falls and other adverse outcomes in older adults, such as disability, functional impairment, and death.21–24 Studies have indicated that CF is independently associated with falls among elderly individuals in both urban and rural communities in China.25
Although the correlation between sleep disorders, CF, and falls has been reported, similar studies have not been conducted in hospitalized older adults with hypertension. It is well known that hypertension, sleep disorders, cognitive impairment, and frailty are common among the elderly, and the prevalence of these conditions increases with age.26–28 Hypertension and sleep quality are interrelated: hypertension can make individuals more susceptible to insomnia, and excessive focus on their physical condition may lead to anxiety and depression, which affect blood pressure control. This, in turn, increases vascular stress, endothelial injury, and the production of active substances, ultimately contributing to the development of sleep disorders.29 Furthermore, hypertension is a common risk factor for frailty and cognitive decline.30,31 Therefore, we believe it is necessary to focus our research on the specific group of hospitalized older adults with hypertension. Our goal is to explore whether the occurrence of falls in this group is associated with sleep disorders and CF, and whether this association is stronger than in older adults without a diagnosis of hypertension. This study aims to understand the relationship between falls and both sleep disorders and CF in hospitalized older adults with hypertension in China, providing a basis for fall prevention in this population.
Materials and Methods
Clinical Data
This study focused on hospitalized older adults with hypertension treated at the Department of Geriatrics, Huaihe Hospital of Henan University from July 2022 to June 2024. The inclusion criteria were: (1) age≥65 years; (2) having received antihypertensive treatment or a history of hypertension; (3) stable condition and able to cooperate with the completion of relevant assessments. Exclusion Criteria: (1) Patients with severe hearing or visual impairment, dementia, or psychiatric disorders (eg, schizophrenia, bipolar disorder) that would impair normal communication and cooperation; (2) Patients in the terminal stages of diseases (eg, end-stage malignant tumors).
Methods
Collection of General Demographic Data
A self-designed questionnaire was used to collect data from all enrolled patients. This included information on gender, age, smoking history (defined as smoking more than 20 cigarettes per day for more than 6 months), alcohol consumption history (defined as drinking more than 20 g per day for more than 6 months), and education level (categorized as illiterate, primary school, junior middle school, senior high school and above). Height and weight were measured, and Body Mass Index (BMI) was calculated. A detailed inquiry about past medical history was conducted, including grading the severity of hypertension and stratifying the duration of hypertension (≤10 years, >10 years). The presence of comorbidities (defined as the coexistence of two or more chronic diseases) was assessed,32 along with the patient’s medication use, to determine if polypharmacy was present.Polypharmacy was defined as concurrent use of ≥5 medications (including both prescribed and over-the-counter drugs) for ≥28 days prior to admission, excluding topical agents, short-term medications (eg, antibiotics for <7 days), and PRN drugs. Two pharmacists independently cross-verified medications using Electronic Health Records, brought containers, and family interviews.
Falls
In this study, a fall is defined as “an unintentional descent to the ground or a lower level, not caused by a sustained, violent blow, loss of consciousness, stroke-related paralysis, or a sudden seizure”.33
The definition of a fall was communicated to the study participants. Falls were measured based on the participants’ responses to the question, “In the past 12 months, have you experienced any falls?” If the response was “Yes”, the participant was considered to have had a fall. Similarly, if the response was “No”, the participant was considered not to have experienced any falls.To minimize recall bias, particularly among participants with cognitive impairment, all reported fall events were cross-verified through a three-tiered approach: (1) medical record review screening for fall-related ICD-10 codes (W00-W19) or documented injuries consistent with fall mechanisms (eg, fractures, contusions) in emergency department and outpatient records; (2) caregiver verification through standardized questionnaires for community-dwelling participants’ family members and real-time documentation via hospital incident reporting systems for inpatients; (3) application of strict inclusion criteria requiring either ≥1 independent verification source (medical records or caregiver reports) or self-reports with detailed circumstantial descriptions (time/location/injury) confirmed by research staff.
Sleep Quality
The PSQI was used for assessment,34 consisting of 7 dimensions: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Each dimension is scored on a scale of 0 to 3, with the total PSQI score ranging from 0 to 21. A higher score indicates poorer sleep quality. A total score ≤5 indicates no sleep disorder, while a score >5 suggests the presence of sleep disorder.
Cognitive Frailty
CF refers to PF and MCI (excluding dementia) in older adult individuals. We used the Frailty Phenotype(FP) and Mini Mental State Examination(MMSE) to measure CF.35,36 The FP is used to evaluate PF and includes five physiological indicators: involuntary weight loss, fatigue, reduction in grip strength, reduction in walking speed and reduction in physical activity. The total score ranges from 0 to 5. A score of 0 indicates no frailty, a score of 1 or 2 indicates the prophase of frailty, and a score from 3 to 5 indicates frailty. The MMSE is used to evaluate the cognitive function of individuals. The score ranges between 0 and 30. The higher the score is, the better the cognitive function. The MMSE scoring standard is based on the patient’s educational level: illiterate≤17 points, elementary school education≤20 points, and secondary school or higher≤24 points, with scores below these thresholds indicating cognitive impairment.37 It should be emphasized that an unauthorized version of the Chinese MMSE was used by the study team without permission, however this has now been rectified with PAR.T he MMSE is a copyrighted instrument and may not be used or reproduced in whole or in part, in any form or language, or by any means without written permission of PAR (www.parinc.com).
Depression
The Geriatric Depression Scale (GDS-15) was used for depression evaluation.38 This scale assesses the participant’s emotional status over the past week with 15 questions. Participants answer “Yes” or “No” to each question. A score of 1 point is given for depressive symptoms, with a maximum score of 15. A total score of ≥5 points indicates the presence of depression.
Nutritional Status
The Mini Nutritional Assessment (MNA) was used to evaluate the nutritional status.39 The MNA includes 18 items, with a total score of 30 points. The scoring criteria are as follows: MNA > 24 points: indicates good nutritional status, 17 ≤ MNA ≤ 23.5 points: suggests potential risk of malnutrition, MNA < 17 points: indicates malnutrition.
Sample Size Calculation
The sample size was estimated a priori using G*Power 3.1 for binary logistic regression. Based on literature reporting a 30% fall incidence among older hypertensive patients without sleep disorders,1 138 participants were required to detect an OR=2.5 for the sleep disorder-fall association (α=0.05, power=0.80). Accounting for 15% variance explained by covariates (age, sex, polypharmacy, etc). and 20% attrition, we planned to recruit 173 participants. The final sample size was expanded to 250 to ensure adequate power for cognitive frailty analyses (target OR=4.0) and subgroup explorations.
Statistical Methods
This study used SPSS 29.0 software for statistical description and inference. For continuous data, normality was tested using the Kolmogorov–Smirnov test, and homogeneity of variance was tested using Levene’s test. Data following a normal distribution or approximately normal distribution were expressed as mean±standard deviation (SD), with comparisons between two groups performed using the t-test. For data that did not follow a normal distribution, the median (interquartile range) was used, and comparisons between two groups were made using the Wilcoxon rank-sum test. Categorical data were expressed as frequency and percentage, and comparisons were conducted using the chi-square test. Multicollinearity was evaluated by calculating variance inflation factors (VIFs), where VIF values exceeding 5 were considered indicative of substantial multicollinearity. To address highly correlated variables, we either excluded one of the redundant variables or created composite variables through appropriate transformations. Variables demonstrating statistically significant differences in univariate analyses were included in the binary logistic regression model, with statistically significant predictors subsequently identified through forward stepwise selection based on the likelihood ratio (LR) criterion. The significance level was set at α= 0.05, and a P < 0.05 was considered statistically significant.
Results
The final sample of 266 participants surpassed the a priori estimated requirement (n=250), achieving >99% statistical power for the primary exposures (sleep disorders and cognitive frailty) at α=0.05. Among the 266 hospitalized elderly hypertensive patients, 108 experienced falls within the past 12 months, with a fall incidence rate of 40.6%. Of the 108 falls analyzed, 46% (n=50) were confirmed by medical records, 32% (n=34) by caregiver reports, and 22% (n=24) by self-report only. Other statistical data, including gender, age, BMI, smoking history, alcohol consumption history, education level, duration and classification of hypertension, comorbidities, polypharmacy, as well as sleep quality, CF, depression and nutritional status, are shown in Table 1. The results of univariate analysis of falls in hospitalized older adults with hypertension are as follows (Table 1): The fall incidence rate differed significantly in terms of age, BMI, comorbidities, polypharmacy, sleep disorders, CF, cognitive impairment, frailty, depression, and nutritional status (P<0.05). However, there were no statistically significant differences in fall incidence rate regarding gender, smoking history, alcohol consumption history, education level, hypertension duration or hypertension classification (P > 0.05).
 |
Table 1 General Demographic Data and Univariate Analyses |
Multicollinearity diagnosis was performed for factors showing statistical significance in univariate analyses (including age, BMI, comorbidities, polypharmacy, sleep disorders, CF, cognitive impairment, frailty, depression, and nutritional status) (Table 2). The results revealed significant multicollinearity among CF (VIF=5.118), frailty (VIF=6.400), and cognitive impairment (VIF=6.120). Given that CF exhibited relatively lower VIF values and encompasses both cognitive and physical functional dimensions, we retained CF while excluding the other two variables from subsequent analyses.
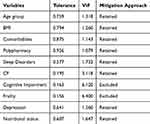 |
Table 2 Multicollinearity Diagnosis |
The occurrence of falls was used as the dependent variable, and factors with statistical significance and collinearity diagnosis VIF < 5 in univariate analysis (age, BMI, comorbidity, polypharmacy, sleep disorders, CF, depression, nutritional status) were analyzed using forward logistic regression. The inclusion criterion was 0.05, and the exclusion criterion was 0.10. The results show (Table 3): Age was associated with falls in older adults with hypertension (95% CI 1.055–1.188, P < 0.001). The fall risk in hospitalized older adults with hypertension with comorbidities was 2.855 times higher than those without comorbidities (95% CI 1.353–6.024, P = 0.006). Polypharmacy was associated with 4.126-times greater fall risk (95% CI 1.937–8.793, p<0.001). Patients with poor sleep quality had 2.625-times increased fall risk relative to those with good sleep quality (95% CI 1.214–5.678, p=0.014).CF conferred a 5.920-fold elevated risk of falls (95% CI 2.632–13.314, p<0.001). Malnourished patients demonstrated 4.698-times higher fall risk than well-nourished patients (95% CI 1.724–12.800, p=0.002).
 |
Table 3 Forward Logistics Regression Analysis |
Discussion
This study explores the relationship between falls and both sleep disorders and CF in hospitalized older adults with hypertension, as well as the factors influencing falls. Previous studies have found that sleep disorders and CF are associated with falls. However, no relevant studies have specifically focused on older adults with hypertension. Our research results indicate that there is a significant correlation between falls and both sleep disorders and CF in hospitalized older adults with hypertension.
In our study, the prevalence of falls was 40.6%, which is higher than the results of several other studies (13.1% to 25.4%).40–43 This may be related to the fact that our study was conducted in an elderly hypertensive population. International studies also show that falls are a major issue among the older adults, with more than 30% of community residents aged 65 and older experiencing at least one fall within a year, and elderly individuals with hypertension having the highest incidence.44 Previous studies have shown that a history of falls, fear of falling, use of antihypertensive medications, and poor medication adherence are all significant factors contributing to the high incidence of falls in this population.45 Furthermore, these patients experience vascular sclerosis and reduced sensitivity of pressure receptors, making them more vulnerable to factors such as emotions, infections, fatigue, and other fall-inducing conditions, which ultimately lead to falls.
Our study found that sleep disorders are associated with falls in hospitalized older adults with hypertension. In longitudinal studies, poor sleep quality has been shown to be a significant factor influencing falls.46 Research by Kanda et al indicated that sleep deprivation is associated with white matter lesions, which are known to be an important risk factor for falls in the elderly.47,48 Shortened sleep duration, due to insomnia, fragmented sleep, and poor sleep quality, may result in poor physical performance, thereby increasing the risk of falls.49,50 Individuals with insomnia may have poorer balance control, alertness, attention, and slower response times,51 all of which can increase the risk of falls. Avidan et al found that insomnia could predict subsequent falls.52 Unresolved insomnia or insomnia unresponsive to hypnotic treatments resulted in a significantly higher risk of falls, with a greater number of falls occurring compared to participants without insomnia. A study in Boston, after adjusting for multiple covariates, found that the likelihood of falls increased by 32% in adults with insomnia, and insomnia was significantly associated with fall risk in individuals aged 60 and older, as well as in women, but not in adults younger than 60 or in men, this study also found that insomnia was not associated with recurrent falls.53 Other studies have shown that the use of pharmacological treatments for sleep, such as sedative-hypnotics, increases the risk of falls.54 Older adults who take sleep medications are at a higher risk of falls compared to those who do not use sleep medications,55 with the exposure rate to sleep medications among US participants as high as 20.9%. Chen et al found that elderly individuals who used doctor-recommended sleep medications had a higher risk of falls, regardless of the severity of their insomnia symptoms.56 The potential mechanisms behind fall risk associated with sedative-hypnotics seem to involve daytime sedation, dizziness, psychomotor impairment, loss of balance, and residual effects of the medication on the following day. Both sleep disturbances themselves and the medications used to treat them may contribute to falls.57 However, sleep medications may alleviate insomnia symptoms in elderly individuals and potentially reduce the risk of subsequent falls. Thus, further research is needed to explore the impact of sleep medications on the occurrence of falls. Recent studies also show that sleep problems can affect psychological states, which in turn influence the occurrence of falls. Poor psychological states have been shown to affect fall risk, and psychological state partially mediates the relationship between self-reported sleep quality and falls.58 Poor sleep quality may impair emotional regulation, increasing the risk of depression and anxiety. These mood disorders can further compromise patients’ attention, reaction time, and executive function, thereby elevating the risk of falls. Depression is associated with hyperactivity of the hypothalamic-pituitary-adrenal (HPA) axis, which may lead to muscle atrophy and impaired balance. Depressed patients may also reduce physical activity, accelerating muscle loss and functional decline. Anxiety, on the other hand, may trigger overly cautious or exaggerated gait patterns, further increasing the likelihood of falls.59 It is important to note that our study did not examine the relationship between various dimensions of sleep and falls. Therefore, further studies are needed to clarify the correlation between different aspects of sleep and fall risk in the older adults with hypertension.
In our study, the risk of falls in hospitalized older adults with hypertension with CF was 5.920 times higher than in those without CF (OR=5.920, 95% CI 2.632–13.314,P<0.001). This suggests that a thorough assessment for CF should be conducted in older adults with hypertension to prevent falls. A cross-sectional study categorized 1,192 individuals aged 70 and older into three groups: MCI, frailty, and CF. Through interviews regarding falls in the past year, the study found that the CF group had significantly more falls than the other two groups.43 This result aligns with Ma et al,25 and similarly, our study found that CF is a Key risk factor for falls in older adults with hypertension. Tsutsumimoto et al collected data from 10,202 community-dwelling elderly individuals and found that CF was not only associated with falls but also with fall-related fractures, the risk of fall-related fractures in individuals with CF (OR = 1.92, 95% CI 1.20,3.08, P = 0.007) was higher than in those with only cognitive decline or frailty.40 Frailty is considered a precursor to disability in older adults, increasing the likelihood of falls, disability, and other common clinical events, which significantly reduce the quality of life and increase mortality.60 Literature also shows that frailty is an independent risk factor for falls, with the risk of falls correlating positively with the severity of frailty. Frail elderly individuals have a significantly higher risk of falls compared to non-frail individuals, and the frequency of falls is generally higher, particularly among those aged 75 and older.61 Frailty increases the risk of falls, and the adverse consequences of falls, such as soft tissue injuries and fractures, further exacerbate frailty. Studies have reported that elderly individuals with cognitive impairment have a 70–80% higher probability of falling within a year compared to their cognitively normal peers of the same age.62 Research suggests that cognitive decline leads to various symptoms, including impairments in processing speed, attention, planning ability, reaction time, memory, and executive function, all of which can further impair balance, walking rhythm, slow down gait speed, and increase gait variability. Moreover, central nervous system dysfunction can lead to decreased muscle strength, further triggering falls.63 A study examining the relationship between MCI and falls found that individuals with MCI had a significantly higher risk of falling,17 as cognitive decline impairs elderly individuals’ ability to process and respond to external information effectively. Thus, CF and the associated cognitive decline should be considered important factors in fall prevention strategies for elderly hypertensive patients, emphasizing the need for early identification and intervention to reduce fall risks.
In the demographic data of this study, age was found to be closely associated with falls in older adults with hypertension (OR=1.119, 95% CI 1.055–1.188,P<0.001), which is consistent with findings from several other studies.64,65 These studies generally included elderly participants without distinguishing whether they were diagnosed with hypertension. Aging is associated with the varying degradation rates of organs, tissues, muscles, cells, and other bodily components. The incidence of falls is notably high in elderly individuals, especially among the older age groups. Relevant studies suggest that in elderly women, a decline in estrogen levels results in reduced osteoblast and osteoclast activity, leading to a significant decrease in bone density. This, coupled with poor physical function and an increased prevalence of osteoporosis, makes older women more susceptible to falls. Furthermore, elderly women are often more engaged in household chores and activities such as square dancing, and they may be more prone to negative emotions and reduced attention, further increasing their fall risk.66 However, Zhao et al reported in a study of community-dwelling elderly individuals that men were more likely to fall than women.67 Previous studies have found that after adjusting for malnutrition, both age and male gender were independently associated with inpatient falls.68 In our study, we found no significant gender difference in fall risk among older adults with hypertension. This suggests that, in the context of hypertension, gender may not be a differentiating factor for fall risk, which warrants further investigation.
Chronic diseases are recognized as significant risk factors for falls in the elderly, and the more chronic diseases an elderly person has, the higher their incidence of falls.69 This finding aligns with our study results. Lee et al observed that among 11,000 elderly individuals, those with chronic diseases had a significantly higher fall incidence compared to those without chronic diseases.70 In another study of 12,669 Medicare-enrolled community-dwelling elderly individuals in the US, Shumway-Cook et al found that the number of comorbidities was associated with an increased likelihood of falls, particularly among those who had fallen one or two times or more in the previous year.71 Several acute or chronic conditions, such as osteoporosis, diabetes, urinary incontinence, and cardiovascular diseases, are well-established fall risk factors.72 For example, elderly individuals with cardiovascular disease may experience ischemia in the heart or brain, which can trigger chest pain, dizziness, or syncope, ultimately leading to falls. In a national longitudinal study by Ye Tian et al involving 11,618 participants, it was found that the risk of falls during the follow-up period significantly increased with the number of chronic diseases at baseline.73 There was a clear dose-response relationship between the number of chronic diseases at baseline and the occurrence of falls during follow-up. Specifically, elderly individuals with two or more chronic diseases at baseline had a significantly higher risk of falling during the follow-up period. Furthermore, participants who had a history of falls at baseline were at a notably higher risk of developing multiple chronic diseases compared to those without a fall history.
Our study also indicates that polypharmacy is associated with falls in older adults with hypertension. A case-control study on elderly individuals aged 70 years and above found that for each additional medication taken, the risk of falls increased by 1.02 times.67 The medications that most significantly impact fall risk include psychotropic drugs, cardiovascular medications, antidiabetic drugs, and analgesics.74–76 There is no universally accepted definition of polypharmacy, but the most common criterion is the use of five or more medications.77 Studies have shown that using≥5 medications is associated with an increased risk of falls, disability, and mortality in elderly individuals.78 Polypharmacy may increase the risk of falls through drug-drug or drug-disease interactions, leading to adverse side effects.79 The American Geriatrics Society (AGS) fall prevention guidelines recommend reducing the number of medications for patients taking more than four drugs as an effective strategy to prevent falls.80 Furthermore, polypharmacy due to comorbidities is widespread in the elderly population. Some studies suggest that polypharmacy in older adults is primarily a result of multiple chronic health conditions, which may lead to complex pathophysiological changes in the body.81 However, there is also research that takes a different stance. For example, KOJIMA et al argued that polypharmacy, rather than multimorbidity itself, is the factor most strongly associated with increased fall risk in elderly outpatients.82 Other studies suggest that chronic conditions, such as depression, hypertension, and chronic obstructive pulmonary disease (COPD), do not significantly influence the relationship between polypharmacy and falls.83 Therefore, prospective and interventional studies are needed to clarify the causal relationship between polypharmacy, comorbidities, and falls.
Previous research has consistently shown that malnutrition is a significant risk factor for falls.84 Trevisan et al reported in a systematic review that malnutrition increased the fall rate among community-dwelling elderly individuals by approximately 1.5 times.85 In addition, a nationwide survey in Taiwan (the Taiwan Longitudinal Survey on Aging) found that, among 97.5% of elderly individuals capable of walking, malnutrition risk was associated with an increased likelihood of falls.86 Yuria Ishida et al further highlighted that the fall risk during hospitalization was 2.7 times higher for malnourished patients compared to those who were not malnourished.68 Eckert et al used screening data from elderly individuals receiving supportive home care services and identified a significant association between malnutrition risk and fall risk.87 After adjusting for demographic factors and other fall risk factors, they found that a higher risk of malnutrition was significantly associated with an increased likelihood of falls compared to those at low risk of malnutrition. Some scholars believe that malnutrition increases fall risk through associated conditions such as sarcopenia and frailty,88 as well as the role of nutrition in maintaining muscle and bone health.89 Our study also confirms that malnourished older adults with hypertension demonstrated 4.698-times higher fall risk than well-nourished patients (95% CI 1.724,12.800, p=0.002).
Strengths and Limitations of This Study
This study has certain limitations. First, the data were collected cross-sectionally, which only allows for the study of influencing factors, but not causal inference. We plan to conduct further follow-up on this cohort and examine longitudinal data in the future. Second, due to issues with database accessibility, this study was unable to collect data on home environmental factors, which limited the analysis of home-related risk factors for falls among the elderly. Additionally, we did not include epidemiological data on falls, such as the location, time, consequences, and disease burden of falls.Third, this study did not investigate the relationship between various dimensions of sleep and falls.Fourth, the rough diagnosis of MCI is one of the limitations of this study. We used the MMSE to diagnose MCI without assessing the independence of daily living activities. A more comprehensive neuropsychological evaluation may aid in the diagnosis of MCI. Fifth, this study did not systematically collect patients’ medication usage data (including polypharmacy status, specific drug categories, and duration of use). We recommend that future research incorporate medication burden assessment to improve risk prediction models. Sixth,venth, the findings of this study are primarily applicable to hospitalized older adults with hypertension with similar high-risk characteristics (eg, multimorbidity and polypharmacy), and thus may not be directly generalizable to healthier aging populations. Future studies should validate these results in patient groups with fewer comorbidities and limited medication use. Therefore, future research should use more comprehensive and high-quality databases to conduct longitudinal studies, enhance the explanatory power of causal inference, and carry out relevant epidemiological investigations, predictive studies, and intervention research. This will provide a strong reference for the development of effective strategies and interventions for preventing and controlling falls in the elderly.
Conclusion
In conclusion, our research results indicate that both sleep disorders and CF were strongly associated with falls in hospitalized older adults with hypertension in China. Old age, comorbidities, polypharmacy and poor nutritional status play important roles in the risk of falls in this patient population. These findings provide valuable guidance for decision-making in fall prevention. Based on the identification of CF (OR=5.92) and sleep disorders (OR=2.625) as key modifiable risk factors, we recommend implementing the following preventive strategies: conducting CF assessments for all hospitalized older adults with hypertension, screening for sleep problems using the PSQI, and providing early multidisciplinary team management for those who test positive.
Ethics Approval and Consent to Participate
This study strictly adhered to the ethical principles of the Declaration of Helsinki and was approved by the Ethics Committee of Huaihe Hospital of Henan University. Written informed consent was obtained from all participants, and all assessments, including the MMSE, were conducted only after completion of the informed consent procedures. We hereby confirm that no identifiable participant information (such as medical images, facial characteristics, or names) was disclosed in this study.
Acknowledgments
We thank all participants for the time dedicated to the study.
Disclosure
The authors declare that there are no competing interests associated with the manuscript.
References
1. Ganz DA, Latham NK. Fall prevention in community-dwelling older adults. Reply. N Engl J Med. 2020;382(26):2581–2582. doi:10.1056/NEJMcp1903252
2. Nicholson WK, Silverstein M, Wong JB, et al. Interventions to prevent falls in community-dwelling older adults: US Preventive Services Task Force recommendation statement. JAMA. 2024;332(1):51–57. doi:10.1001/jama.2024.8481
3. Ye P, Er Y, Wang H, et al. Burden of falls among people aged 60 years and older in mainland China, 1990-2019: findings from the Global Burden of Disease Study 2019. Lancet Public Health. 2021;6(12):e907–e918. doi:10.1016/S2468-2667(21)00231-0
4. Guirguis-Blake JM, Perdue LA, Coppola EL, Bean SI. Interventions to prevent falls in older adults: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2024;332(1):58–69. doi:10.1001/jama.2024.4166
5. Xu Q, Ou X, Li J. The risk of falls among the aging population: a systematic review and meta-analysis. Front Public Health. 2022;10:902599. doi:10.3389/fpubh.2022.902599
6. Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc. 2018;66(4):693–698. doi:10.1111/jgs.15304
7. Jaqua EE, Hanna M, Labib W, Moore C, Matossian V. Common sleep disorders affecting older adults. Perm J. 2023;27(1):122–132. doi:10.7812/TPP/22.114
8. van de Straat V, Bracke P. How well does Europe sleep? A cross-national study of sleep problems in European older adults. Int J Public Health. 2015;60(6):643–650. doi:10.1007/s00038-015-0682-y
9. Endeshaw YW, Yoo W. Association between social and physical activities and insomnia symptoms among community-dwelling older adults. J Aging Health. 2016;28(6):1073–1089. doi:10.1177/0898264315618921
10. Ida S, Kaneko R, Nagata H, et al. Association between sarcopenia and sleep disorder in older patients with diabetes. Geriatr Gerontol Int. 2019;19(5):399–403. doi:10.1111/ggi.13627
11. Min Y, Slattum PW. Poor sleep and risk of falls in community-dwelling older adults: a systematic review. J Appl Gerontol. 2018;37(9):1059–1084. doi:10.1177/0733464816681149
12. Ma T, Shi G, Zhu Y, et al. Sleep disturbances and risk of falls in an old Chinese population-Rugao Longevity and Ageing Study. Arch Gerontol Geriatr. 2017;73:8–14. doi:10.1016/j.archger.2017.07.003
13. Knechel NA, Chang PS. The relationships between sleep disturbance and falls: a systematic review. J Sleep Res. 2022;31(5):e13580. doi:10.1111/jsr.13580
14. Essien SK, Feng CX, Sun W, Farag M, Li L, Gao Y. Sleep duration and sleep disturbances in association with falls among the middle-aged and older adults in China: a population-based nationwide study. BMC Geriatr. 2018;18(1):196. doi:10.1186/s12877-018-0889-x
15. Chen C, Li X, Wang J, et al. Longitudinal changes of cognition and frailty with all-cause and cause-specific mortality in Chinese older adults: an 11-Year Cohort Study. Innov Aging. 2023;7(9):igad114. doi:10.1093/geroni/igad114
16. Kelaiditi E, Cesari M, Canevelli M, et al. Cognitive frailty: rational and definition from an (I.A.N.A./I.A.G.G.) international consensus group. J Nutr Health Aging. 2013;17(9):726–734. doi:10.1007/s12603-013-0367-2
17. Quach LT, Ward RE, Pedersen MM, et al. The association between social engagement, mild cognitive impairment, and falls among older primary care patients. Arch Phys Med Rehabil. 2019;100(8):1499–1505. doi:10.1016/j.apmr.2019.01.020
18. Chittrakul J, Siviroj P, Sungkarat S, Sapbamrer R. Physical frailty and fall risk in community-dwelling older adults: a cross-sectional study. J Aging Res. 2020;2020:3964973. doi:10.1155/2020/3964973
19. Hu K, Zhou Q, Jiang Y, et al. Association between frailty and mortality, falls, and hospitalization among patients with hypertension: a systematic review and meta-analysis. Biomed Res Int. 2021;2021:2690296. doi:10.1155/2021/2690296
20. Song Y, Deng Y, Li J, et al. Associations of falls and severe falls with blood pressure and frailty among Chinese community-dwelling oldest olds: the Chinese Longitudinal Health and Longevity Study. Aging. 2021;13(12):16527–16540. doi:10.18632/aging.203174
21. Aprahamian I, Suemoto CK, Aliberti MJR, et al. Frailty and cognitive status evaluation can better predict mortality in older adults? Arch Gerontol Geriatr. 2018;77:51–56. doi:10.1016/j.archger.2018.04.005
22. Hao Q, Dong B, Yang M, Dong B, Wei Y. Frailty and cognitive impairment in predicting mortality among oldest-old people. Front Aging Neurosci. 2018;10:295. doi:10.3389/fnagi.2018.00295
23. Bu Z, Huang A, Xue M, Li Q, Bai Y, Xu G. Cognitive frailty as a predictor of adverse outcomes among older adults: a systematic review and meta-analysis. Brain Behav. 2021;11(1):e01926. doi:10.1002/brb3.1926
24. Zhang XM, Jiao J, Zhu C, et al. Cognitive frailty and 30-day mortality in a national cohort of older Chinese inpatients. Clin Interv Aging. 2021;16:389–401. doi:10.2147/CIA.S294106
25. Ma L, Zhang L, Zhang Y, Li Y, Tang Z, Chan P. Cognitive frailty in China: results from China Comprehensive Geriatric Assessment Study. Front Med. 2017;4:174. doi:10.3389/fmed.2017.00174
26. Yaremchuk K. Sleep disorders in the elderly. Clin Geriatr Med. 2018;34(2):205–216. doi:10.1016/j.cger.2018.01.008
27. Sugimoto T, Arai H, Sakurai T. An update on cognitive frailty: its definition, impact, associated factors and underlying mechanisms, and interventions. Geriatr Gerontol Int. 2022;22(2):99–109. doi:10.1111/ggi.14322
28. Zhang M, Shi Y, Zhou B, et al. Prevalence, awareness, treatment, and control of hypertension in China, 2004-18: findings from six rounds of a national survey. BMJ. 2023;380:e071952.
29. Liu C, Ye Z, Chen L, et al. Interaction effects between sleep-related disorders and depression on hypertension among adults: a cross-sectional study. BMC Psychiatry. 2024;24(1):482. doi:10.1186/s12888-024-05931-9
30. Fougère B, Delrieu J, Del Campo N, Soriano G, Sourdet S, Vellas B. Cognitive frailty: mechanisms, tools to measure, prevention and controversy. Clin Geriatr Med. 2017;33(3):339–355. doi:10.1016/j.cger.2017.03.001
31. Ungvari Z, Toth P, Tarantini S, et al. Hypertension-induced cognitive impairment: from pathophysiology to public health. Nat Rev Nephrol. 2021;17(10):639–654. doi:10.1038/s41581-021-00430-6
32. Xu X, Mishra GD, Jones M. Evidence on multimorbidity from definition to intervention: an overview of systematic reviews. Ageing Res Rev. 2017;37:53–68. doi:10.1016/j.arr.2017.05.003
33. The prevention of falls in later life. A report of the Kellogg International Work Group on the Prevention of Falls by the Elderly. Dan Med Bull. 1987;34(Suppl 4):1–24.
34. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
35. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol a Biol Sci Med Sci. 2001;56(3):M146–156. doi:10.1093/gerona/56.3.M146
36. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi:10.1016/0022-3956(75)90026-6
37. Pu L, Pan D, Wang H, et al. A predictive model for the risk of cognitive impairment in community middle-aged and older adults. Asian J Psychiatr. 2023;79:103380. doi:10.1016/j.ajp.2022.103380
38. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17(1):37–49. doi:10.1016/0022-3956(82)90033-4
39. Guigoz Y, Vellas B, Garry PJ. Assessing the nutritional status of the elderly: the mini nutritional assessment as part of the geriatric evaluation. Nutr Rev. 1996;54(1 Pt 2):S59–65. doi:10.1111/j.1753-4887.1996.tb03793.x
40. Tsutsumimoto K, Doi T, Makizako H, et al. Cognitive frailty is associated with fall-related fracture among older people. J Nutr Health Aging. 2018;22(10):1216–1220. doi:10.1007/s12603-018-1131-4
41. Kim H, Awata S, Watanabe Y, et al. Cognitive frailty in community-dwelling older Japanese people: prevalence and its association with falls. Geriatr Gerontol Int. 2019;19(7):647–653. doi:10.1111/ggi.13685
42. Brigola AG, Ottaviani AC, Alexandre TDS, Luchesi BM, Pavarini SCI. Cumulative effects of cognitive impairment and frailty on functional decline, falls and hospitalization: a four-year follow-up study with older adults. Arch Gerontol Geriatr. 2020;87:104005. doi:10.1016/j.archger.2019.104005
43. Zhao D, Li J, Fu P, et al. What role does activity engagement play in the Association between cognitive frailty and falls among older adults? Evidence from Rural Shandong, China. Gerontology. 2020;66(6):593–602. doi:10.1159/000510639
44. Graafmans WC, Ooms ME, Hofstee HM, Bezemer PD, Bouter LM, Lips P. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol. 1996;143(11):1129–1136. doi:10.1093/oxfordjournals.aje.a008690
45. Sirkin AJ, Rosner NG. Hypertensive management in the elderly patient at risk for falls. J Am Acad Nurse Pract. 2009;21(7):402–408. doi:10.1111/j.1745-7599.2009.00418.x
46. Takada S, Yamamoto Y, Shimizu S, et al. Association between subjective sleep quality and future risk of falls in older people: results from LOHAS. J Gerontol a Biol Sci Med Sci. 2018;73(9):1205–1211. doi:10.1093/gerona/glx123
47. Kanda A, Matsui T, Ebihara S, Arai H, Sasaki H. Periventricular white matter lesions and sleep alteration in older people. J Am Geriatr Soc. 2003;51(3):432–433. doi:10.1046/j.1532-5415.2003.51125.x
48. Srikanth V, Beare R, Blizzard L, et al. Cerebral white matter lesions, gait, and the risk of incident falls: a prospective population-based study. Stroke. 2009;40(1):175–180. doi:10.1161/STROKEAHA.108.524355
49. Eshkoor SA, Hamid TA, Nudin SS, Mun CY. The effects of sleep quality, physical activity, and environmental quality on the risk of falls in dementia. Am J Alzheimers Dis Other Demen. 2013;28(4):403–407. doi:10.1177/1533317513488921
50. Helbig AK, Döring A, Heier M, et al. Association between sleep disturbances and falls among the elderly: results from the German Cooperative Health Research in the Region of Augsburg-Age study. Sleep Med. 2013;14(12):1356–1363. doi:10.1016/j.sleep.2013.09.004
51. Robillard R, Prince F, Filipini D, Carrier J. Aging worsens the effects of sleep deprivation on postural control. PLoS One. 2011;6(12):e28731. doi:10.1371/journal.pone.0028731
52. Avidan AY, Fries BE, James ML, Szafara KL, Wright GT, Chervin RD. Insomnia and hypnotic use, recorded in the minimum data set, as predictors of falls and Hip fractures in Michigan nursing homes. J Am Geriatr Soc. 2005;53(6):955–962. doi:10.1111/j.1532-5415.2005.53304.x
53. Zhang Y, Cifuentes M, Gao X, Amaral G, Tucker KL. Age- and gender-specific associations between insomnia and falls in Boston Puerto Rican adults. Qual Life Res. 2017;26(1):25–34. doi:10.1007/s11136-016-1374-7
54. Brassington GS, King AC, Bliwise DL. Sleep problems as a risk factor for falls in a sample of community-dwelling adults aged 64-99 years. J Am Geriatr Soc. 2000;48(10):1234–1240. doi:10.1111/j.1532-5415.2000.tb02596.x
55. Min Y, Kirkwood CK, Mays DP, Slattum PW. The effect of sleep medication use and poor sleep quality on risk of falls in community-dwelling older adults in the US: a Prospective Cohort Study. Drugs Aging. 2016;33(2):151–158. doi:10.1007/s40266-015-0339-9
56. Chen TY, Lee S, Buxton OM. A greater extent of insomnia symptoms and physician-recommended sleep medication use predict fall risk in community-dwelling older adults. Sleep. 2017;40(11). doi:10.1093/sleep/zsx142
57. Johnell K, Jonasdottir Bergman G, Fastbom J, Danielsson B, Borg N, Salmi P. Psychotropic drugs and the risk of fall injuries, hospitalisations and mortality among older adults. Int J Geriatr Psychiatry. 2017;32(4):414–420. doi:10.1002/gps.4483
58. Liu JH, Ma QH, Sun HP, Xu Y, Pan CW. Depressive symptom as a mediator of the influence of self-reported sleep quality on falls: a mediation analysis. Aging Mental Health. 2021;25(4):728–733. doi:10.1080/13607863.2020.1711860
59. Kim JH, Song JH, Wee JH, Lee JW, Choi HG. Depressive symptoms, subjective cognitive decline, and subjective sleep quality are associated with slips and falls: data from the community health survey in Korean Adults. Gerontology. 2022;68(5):518–528. doi:10.1159/000518007
60. Kojima G, Iliffe S, Jivraj S, Walters K. Association between frailty and quality of life among community-dwelling older people: a systematic review and meta-analysis. J Epidemiol Community Health. 2016;70(7):716–721. doi:10.1136/jech-2015-206717
61. de Vries OJ, Peeters GM, Lips P, Deeg DJ. Does frailty predict increased risk of falls and fractures? A prospective population-based study. Osteoporos Int. 2013;24(9):2397–2403. doi:10.1007/s00198-013-2303-z
62. Booth V, Hood V, Kearney F. Interventions incorporating physical and cognitive elements to reduce falls risk in cognitively impaired older adults: a systematic review. JBI Database Syst Rev Implement Rep. 2016;14(5):110–135. doi:10.11124/JBISRIR-2016-002499
63. Bowen ME, Crenshaw J, Stanhope SJ. Balance ability and cognitive impairment influence sustained walking in an assisted living facility. Arch Gerontol Geriatr. 2018;77:133–141. doi:10.1016/j.archger.2018.05.004
64. Pirrie M, Saini G, Angeles R, Marzanek F, Parascandalo J, Agarwal G. Risk of falls and fear of falling in older adults residing in public housing in Ontario, Canada: findings from a multisite observational study. BMC Geriatr. 2020;20(1):11. doi:10.1186/s12877-019-1399-1
65. Susilowati IH, Nugraha S, Sabarinah S, Peltzer K, Pengpid S, Hasiholan BP. Prevalence and risk factors associated with falls among community-dwelling and institutionalized older adults in Indonesia. Malays Fam Physician. 2020;15(1):30–38. doi:10.1016/S0140-6736(15)60692-4
66. Delbaere K, Crombez G, Vanderstraeten G, Willems T, Cambier D. Fear-related avoidance of activities, falls and physical frailty. A prospective community-based cohort study. Age Ageing. 2004;33(4):368–373. doi:10.1093/ageing/afh106
67. Zhao YL, Alderden J, Lind B, Stibrany J. Risk factors for falls in homebound community-dwelling older adults. Public Health Nurs. 2019;36(6):772–778. doi:10.1111/phn.12651
68. Ishida Y, Maeda K, Nonogaki T, et al. Malnutrition at admission predicts in-hospital falls in hospitalized older adults. Nutrients. 2020;12(2):541. doi:10.3390/nu12020541
69. LeCuyer M, Lockwood B, Locklin M. Development of a fall prevention program in the ambulatory surgery setting. J Perianesth Nurs. 2017;32(5):472–479. doi:10.1016/j.jopan.2016.01.003
70. Lee PG, Cigolle C, Blaum C. The co-occurrence of chronic diseases and geriatric syndromes: the health and retirement study. J Am Geriatr Soc. 2009;57(3):511–516. doi:10.1111/j.1532-5415.2008.02150.x
71. Shumway-Cook A, Ciol MA, Hoffman J, Dudgeon BJ, Yorkston K, Chan L. Falls in the medicare population: incidence, associated factors, and impact on health care. Phys Ther. 2009;89(4):324–332. doi:10.2522/ptj.20070107
72. Ye P, Liu Y, Zhang J, et al. Falls prevention interventions for community-dwelling older people living in mainland China: a narrative systematic review. BMC Health Serv Res. 2020;20(1):808. doi:10.1186/s12913-020-05645-0
73. Tian Y, Zhou X, Jiang Y, et al. Bidirectional association between falls and multimorbidity in middle-aged and elderly Chinese adults: a national longitudinal study. Sci Rep. 2024;14(1):9109. doi:10.1038/s41598-024-59865-z
74. Hart LA, Phelan EA, Yi JY, Marcum ZA, Gray SL. Use of fall risk-increasing drugs around a fall-related injury in older adults: a systematic review. J Am Geriatr Soc. 2020;68(6):1334–1343. doi:10.1111/jgs.16369
75. American Geriatrics Society. 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–694. doi:10.1111/jgs.15767
76. Seppala LJ, Wermelink A, de Vries M, et al. Fall-risk-increasing drugs: a systematic review and meta-analysis: II. Psychotropics. J Am Med Dir Assoc. 2018;19(4):
77. Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230. doi:10.1186/s12877-017-0621-2
78. Montero-Odasso M, Sarquis-Adamson Y, Song HY, Bray NW, Pieruccini-Faria F, Speechley M. Polypharmacy, gait performance, and falls in community-dwelling older adults. Results from the Gait and Brain Study. J Am Geriatr Soc. 2019;67(6):1182–1188. doi:10.1111/jgs.15774
79. Zia A, Kamaruzzaman SB, Tan MP. Polypharmacy and falls in older people: balancing evidence-based medicine against falls risk. Postgrad Med. 2015;127(3):330–337. doi:10.1080/00325481.2014.996112
80. Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc. 2001;49(5):664–672.
81. Lawlor DA, Patel R, Ebrahim S. Association between falls in elderly women and chronic diseases and drug use: cross sectional study. BMJ. 2003;327(7417):712–717. doi:10.1136/bmj.327.7417.712
82. Kojima T, Akishita M, Nakamura T, et al. Association of polypharmacy with fall risk among geriatric outpatients. Geriatr Gerontol Int. 2011;11(4):438–444. doi:10.1111/j.1447-0594.2011.00703.x
83. Helgadóttir B, Laflamme L, Monárrez-Espino J, Möller J. Medication and fall injury in the elderly population; do individual demographics, health status and lifestyle matter? BMC Geriatr. 2014;14:92. doi:10.1186/1471-2318-14-92
84. Adly NN, Abd-El-Gawad WM, Abou-Hashem RM. Relationship between malnutrition and different fall risk assessment tools in a geriatric in-patient unit. Aging Clin Exp Res. 2020;32(7):1279–1287. doi:10.1007/s40520-019-01309-0
85. Trevisan C, Crippa A, Ek S, et al. Nutritional status, body mass index, and the risk of falls in community-dwelling older adults: a systematic review and meta-analysis. J Am Med Dir Assoc. 2019;20(5):569–582.e567. doi:10.1016/j.jamda.2018.10.027
86. Tsai AC, Lai MY. Mini nutritional assessment and short-form mini nutritional assessment can predict the future risk of falling in older adults - results of a national cohort study. Clin Nutr. 2014;33(5):844–849. doi:10.1016/j.clnu.2013.10.010
87. Eckert C, Gell NM, Wingood M, et al. Malnutrition risk, rurality, and falls among community-dwelling older adults. J Nutr Health Aging. 2021;25(5):624–627. doi:10.1007/s12603-021-1592-8
88. Lorenzo-López L, Maseda A, de Labra C, Regueiro-Folgueira L, Rodríguez-Villamil JL, Millán-Calenti JC. Nutritional determinants of frailty in older adults: a systematic review. BMC Geriatr. 2017;17(1):108. doi:10.1186/s12877-017-0496-2
89. Sim M, Blekkenhorst LC, Lewis JR, et al. Vegetable and fruit intake and injurious falls risk in older women: a prospective cohort study. Br J Nutr. 2018;120(8):925–934. doi:10.1017/S0007114518002155
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Association Between Sleep Quality and Hypertension in Chinese Adults: A Cross-Sectional Analysis in the Tianning Cohort
Chen S, Song X, Shi H, Li J, Ma S, Chen L, Lu Y, Hong C, Zhu H, Sun H, Zhang M
Nature and Science of Sleep 2022, 14:2097-2105
Published Date: 28 November 2022
Determinants of Adherence to Antihypertensives Among Elderly: A Multifactorial Concern
Sheilini M, Hande HM, Devi ES, Kamath A, Nayak BS, Morisky DE, George A
Patient Preference and Adherence 2022, 16:3185-3193
Published Date: 7 December 2022
Systemic Inflammation Response Index as a Predictor of Stroke Risk in Elderly Patients with Hypertension: A Cohort Study
Cai X, Song S, Hu J, Wang L, Shen D, Zhu Q, Yang W, Luo Q, Hong J, Li N
Journal of Inflammation Research 2023, 16:4821-4832
Published Date: 24 October 2023
Adherence Behaviors and Related Factors Among Elderly Hypertensive Patients in China: Evidence from the China Health and Retirement Longitudinal Study
Liu F, Chang H, Liu X
Patient Preference and Adherence 2023, 17:3539-3553
Published Date: 23 December 2023
Home Environmental Factors Associated with Falls Among Elderly in Ubon Ratchathani, Thailand
Boonkhao L, Puangjan K, Ouengprasert I, Laosupap K, Bootsorn A, Junsiri S, Thongdamrongtham S, Chaikhan S, Pramaya P, Rattanachaikunsopon P
Journal of Multidisciplinary Healthcare 2024, 17:1363-1373
Published Date: 26 March 2024

