Back to Journals » Journal of Hepatocellular Carcinoma » Volume 12
Functional Liver Imaging Score to Predict Clinically Significant PHLF for Hepatocellular Carcinoma After Resection
Authors Zheng X, Zhang Y, Huang H, Luo N
Received 10 December 2024
Accepted for publication 3 July 2025
Published 18 July 2025 Volume 2025:12 Pages 1483—1493
DOI https://doi.org/10.2147/JHC.S511240
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr David Gerber
Xihua Zheng,* Yumin Zhang,* Huiying Huang, Ningbin Luo
Departments of Radiology, Guangxi Medical University Cancer Hospital, Nanning, Guangxi Zhuang Autonomous Region, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ningbin Luo, Departments of Radiology, Guangxi Medical University Cancer Hospital, Nanning, Guangxi Zhuang Autonomous Region, People’s Republic of China, Fax +860734-5312000, Email [email protected]
Purpose: To develop a model based on Functional Liver Imaging Score (FLIS) to estimate the risk of clinically significant post-hepatectomy liver failure (PHLF) for hepatocellular carcinoma (HCC) after resection.
Patients and Methods: This retrospective study analyzed 885 patients with HCC who undergoing liver resection at our medical center between January 2017 and December 2021. Patients were randomly (7:3) assigned to development (n=620) or internal validation (n=265) cohorts. Univariable and multivariable logistic regression analyses were performed to identify independent risk factors for clinically significant PHLF, defined as grade B or C PHLF by the International Study Group of Liver Surgery. Predictive performance was assessed by the area under receiver operator characteristic curves (AUC).
Results: Clinically significant PHLF occurred in 7.7% of the development cohort and 7.2% of the internal validation cohort. Multivariate analysis identified FLIS, major resection and ALBI score as independent predictors of clinically significant PHLF, and a model combining these three variables predicted failure in the development cohort (AUC 0.746, 95% CI 0.673– 0.820) and internal validation cohort (AUC 0.717, 95% CI 0.595– 0.838). The same model also predicted mortality within 90 days after surgery in the development cohort (AUC 0.704, 95% CI 0.575– 0.832) and internal validation cohort (AUC 0.717, 95% CI 0.586– 0.848). In both cohorts, overall survival rate was significantly lower among patients whom the model placed at high risk of clinically significant PHLF than among those at low risk.
Conclusion: The combination of FLIS and other easily acquired clinical data may reliably predict clinically significant PHLF and mortality in hepatocellular carcinoma.
Plain Language Summary: Functional liver imaging score derived from gadoxetic acid-enhanced MRI can effectively and conveniently evaluate liver function. In this study, functional liver imaging score, major resection and ALBI score were significantly associated with clinically significant post-hepatectomy liver failure for hepatocellular carcinoma after resection. A model combining these factors reliably predicted clinically significant post-hepatectomy liver failure and 90-day mortality in our cohort.
Keywords: hepatocellular carcinoma, hepatectomy, post-hepatectomy liver failure, functional liver imaging scores, magnetic resonance imaging, prognosis
Introduction
Primary liver cancer is the sixth most commonly diagnosed type of cancer and the third leading cause of cancer-related death worldwide, and 75–85% of cases are hepatocellular carcinoma.1 Selected patients can undergo potentially curative liver resection,2,3 but this should be performed with caution to avoid subsequent liver failure because of insufficient remnant liver.4 Such failure is one of the most frequent causes of higher medical expenses, longer hospitalization, and mortality after hepatic resection.4,5 In fact, it may explain nearly half of deaths within 90 days after resection.6,7 A reliable way to predict, before surgery, whether patients will subsequently experience liver failure serious enough to require intervention could improve the selection of patients for resection and their management before and after.
The occurrence of PHLF is closely related to residual liver volume and function.8 Model for End-stage Liver Disease (MELD) score, ICG-R15, Albumin-Bilirubin score (ALBI) is a common method for clinical assessment of liver function. However, they all have some defects, resulting in doubts about the accuracy and reliability of the models.9,10 The creatinine index in MELD score is not applicable to patients with early and middle stage liver cancer without affecting renal function.11,12 The limitation of ICG-R15 is that it may be affected by hepatic blood flow and biliary obstruction, which may reduce the credibility of ICG clearance tests.13 In recent years, ALBI score has been proposed as a more objective and accurate method for clinical assessment of liver function.14 However, the ALBI score consists of only two laboratory measures, serum albumin and total bilirubin, which may be influenced by non-hepatic factors, such as albumin levels which may be affected by nutritional status, inflammation or kidney disease, so its clinical application has some limitations.15 Therefore, there is urgently need for a simple, accurate and stable method to evaluate liver function and predict the risk of clinically significant post-hepatectomy liver failure (PHLF) before surgery, which can help patients develop personalized treatment plan, so as to avoid potential postoperative risks.
Gadoxetic acid-enhanced magnetic resonance imaging (MRI) has been widely used to detect liver lesions and evaluate liver function.16 Approximately 20 minutes following intravenous administration of Gd-EOB-DTPA, the liver parenchyma is enhanced to the maximum extent, and the biliary system is also developed due to the excretion of the contrast agent. This period is hepatobiliary phase (HBP), which can provide more information about the disease and liver function.17 A meta-analysis encompassing 15 studies demonstrated that quantitative parameters derived from Gd-EOB-DTPA enhanced MRI exhibit superior predictive performance for PHLF.18 Several studies have used Gd-EOB-DTPA enhanced MRI-derived liver function parameters to predict PHLF before surgery, such as relative hepatic parenchymal strengthening signal, liver uptake index, functional residual liver volume and other parameters or their derivatives.16,19 However, the application of these parameters may require complex, powerful calculations and is affected by the different MR devices, field strengths and sequences used, making their clinical application difficult to achieve. We wondered whether a previously reported functional liver imaging score (FLIS),20,21 which is based on hepatobiliary phase from gadoxetic acid-enhanced MRI, might help in such prediction. This score has already proven useful for assessing liver function, and one study suggested that it can predict PHLF,22 although that work did not focus on PHLF serious enough to require intervention.
Here we retrospectively analyzed data from patients at our medical center to determine whether the FLIS, together with other routine preoperative variables, could reliably predict clinically significant PHLF for hepatocellular carcinoma. We also asked whether the model could predict mortality and overall survival after resection.
Patients and Methods
Patients
Data were retrospectively reviewed for a consecutive series of patients with pathology-confirmed hepatocellular carcinoma who underwent MRI of the liver based on gadoxetic acid contrast at our hospital between January 2017 and December 2021, followed within one month by hepatectomy at our hospital. This study was approved by the Clinical Research Ethics Committee of our hospital (Approval numbers: KY2024871), which waived the requirement for informed consent. The procedures in this study were performed in compliance with the Helsinki Declaration.
Patients were excluded if their magnetic resonance imaging was inadequate to determine the FLIS; if they had a preoperative history of hepatectomy, transcatheter arterial chemoembolization, or radiofrequency ablation; if they had biliary obstruction or concurrent malignancy; or if they were lost to follow-up after surgery. Patients were followed up regularly, including telephone interviews every six months in order to assess survival and general health. Overall survival was calculated from the date of operation until the date of death or, if the patient was still alive, until the date of last follow-up.
Enrolled patients were randomly divided into development and internal validation cohorts in a 7:3 ratio.
MRI
All patients underwent abdominal MRI on a 1.5-T system (Magnetom Avanto, Siemens Healthcare), 1.5-T system (United Imaging Healthcare) or a 3.0-T system (Discovery MR 750, GE Healthcare). Detailed information and parameters of the magnetic resonance scanners are provided in Supplementary Table 1. All study participants were injected with gadoxetic acid intravenously at a rate of 1.0 mL/s, followed immediately by 20 mL of saline. At about 20 min after injection of gadoxetic acid, three-dimensional spoiled gradient echo T1-weighted imaging with fat suppression was performed in the hepatobiliary phase.
Two radiologists independently reviewed images and determined the FLIS as described (Figure 1). The score, which can range from 0 to 6 points, takes into account liver parenchymal enhancement, persistence of signal in the portal vein and biliary excretion of contrast agent. Disagreements between the two reviewers were resolved through discussion.
Study Outcomes and Other Definitions
The primary outcome of interest was clinically significant PHLF, which was defined as grade B or C liver failure on the scale from the International Study Group of Liver Surgery.23 Such liver failure was diagnosed as the (1) co-occurrence, on or after postoperative day 5, of an international normalized ratio >1.2 and a total bilirubin level that was above either 22 μmol/L or the preoperative value; that (2) required intervention, whether non-invasive or invasive. We did not include grade A PHLF in clinically significant PHLF because it does not require clinical intervention and is associated with low mortality.23,24
Other outcomes of interest were any-cause death within 90 days after surgery and overall survival during follow-up. Liver resection was defined as major if it involved at least three Couinaud segments.25 The MELD score is composed of three laboratory parameters: INR, creatinine, and total bilirubin. Its calculation formula is: MELD score = 11.2 × ln (INR) + 9.57 × ln (Cr, mg/dL) + 3.78 × ln (Tbil, mg/dL) + 6.43 × etiology (0 for cholestatic and alcoholic, 1 for liver cirrhosis due to virus and other causes).26 The ALBI score is composed of two laboratory parameters: total bilirubin and albumin. Its calculation formula is: ALBI score = 0.660 × log10[Tbil (µmol/L)] − 0.085 × [ALB (g/L)].27 Individuals who extracted clinicodemographic data and preoperative data for calculating scores were blinded to MRI findings.
Statistical Analysis
Data were analyzed statistically using SPSS 26.0 (IBM, Armonk, NY, USA), and results associated with p < 0.05 were considered statistically significant. Continuous data were expressed as mean ± standard deviation if normally distributed or as median (interquartile range) if skewed, while categorical data were expressed as n (%). Intergroup differences in continuous variables were assessed for significance using the two-tailed t test or Mann–Whitney U-test, while differences in categorical variables were assessed using the χ2 test or Fisher’s exact test. The missing data of ICG-R15 were imputed using the Markov chain Monte Carlo (MCMC) method with multiple imputations.28 The intraclass correlation coefficient (ICC) was used to evaluate the inter-observer agreement.29
Univariate logistic regression was used to identify factors associated with clinically significant PHLF, and those associated with p < 0.05 were input into a multivariate model. The ability of the model to predict patients who experienced clinically significant PHLF was assessed in terms of the area under receiver operator characteristic curves (AUC). Receiver operating characteristic curves (ROC) of models were compared using the DeLong test. The calibration of the logistic model was assessed using calibration curves. Clinical utility of the model was evaluated through decision curve analysis. The optimal cutoff of the model logit value was determined using the Youden Index. Overall survival between patients with a model logit value below or above the optimal cutoff was compared using the Kaplan-Meier method and Log rank test.
Results
Study Population
Of the 1379 patients whom we considered for enrollment, we excluded 364 because they had a history of hepatectomy, transcatheter arterial chemoembolization or radiofrequency ablation before the study; 58 because they had concurrent malignancy; 41 because the MRI data available were insufficient to calculate the FLIS; 22 because they were lost to follow-up; and 9 because they had biliary obstruction (Figure 2). In the end, 885 were included in the final analysis, 620 of whom were randomized into the development cohort and 265 into the internal validation cohort. The two cohorts did not differ significantly in any of the variables that we examined (Table 1), including preoperative FLIS, rate of clinically significant PHLF, or mortality within 90 days after surgery. Among the overall cohort, 132 patients (14.9%) exhibited missing ICG-R15 values. Following imputation, the median ICG-R15 value was 5.2% (Table 1).
 |
Table 1 Clinicodemographic Characteristics and Outcomes of Study Participants Before and After Randomization Into Development and Internal Validation Cohorts |
 |
Figure 2 Flowchart of patient enrollment and analysis. Abbreviations: HCC, hepatocellular carcinoma; MRI, magnetic resonance imaging. |
Inter-Observer Agreement Analysis
The interobserver agreement analysis for the FLIS and its three components demonstrated good consistency (ICC > 0.75). The interobserver agreement for FLIS was 0.914 (CI: 0.902–0.924). The interobserver agreement reached 0.888 (CI: 0.874–0.902) for liver parenchymal enhancement score, 0.920 (CI: 0.909–0.929) for portal vein signal score, and 0.826 (CI: 0.804–0.846) for biliary excretion of contrast agent score.
Comparison of the Predictive Efficacy Between the FLIS and Other Clinical Models for Clinically Significant PHLF
In the overall cohort, we conducted a comparative analysis of the predictive performance of the FLIS, ALBI score, ICG-R15, and MELD for clinically significant PHLF. The FLIS demonstrated significantly superior predictive performance compared to other clinical models, with AUC of 0.722 (95% CI: 0.691–0.751), which was significantly higher than the ALBI score (AUC = 0.609, 95% CI: 0.576–0.641; p = 0.028), ICG-R15 (AUC = 0.624, 95% CI: 0.591–0.656; p = 0.04), and MELD score (AUC = 0.558, 95% CI: 0.525–0.591; p < 0.001) (Supplemental Figure 1).
Univariate and Multivariate Analyses of Clinically Significant PHLF in the Development Cohort
Univariate analysis of data from the development cohort identified the following variables as associated with clinically significant PHLF (Table 2): major resection, ALBI score, FLIS and rate of indocyanine green 15-min retention (ICG-R15). All variables except ICG-R15 remained significant in multivariate logistic regression: major resection was associated with OR 2.236, 95% CI 1.201–4.166 (p = 0.011); ALBI score, OR 2.977, 95% CI 1.358–6.528 (p = 0.006); and FLIS, OR 0.680, 95% CI 0.541–0.885 (p = 0.001). The resulting multivariate regression model took the form:
Logit = 2.104 - (0.415 × FLIS) + (1.289 × ALBI score) + (0.760 × major resection).
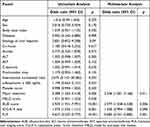 |
Table 2 Logistic Regression to Identify Predictors of Clinically Significant Liver Failure After Hepatectomy in the Development Cohort |
Predictive Performance of the Logistic Model for Postoperative Outcomes
This logistic regression model predicted clinically significant PHLF with an AUC of 0.746 (95% CI 0.673–0.820) in the development cohort and 0.717 (95% CI 0.595–0.838) in the internal validation cohort (Figure 3). The model also performed well in both cohorts in terms of calibration curves (Supplemental Figure 2) and decision curves (Supplemental Figure 3). According to the Youden index, model logit values ≥ −2.43 showed the best discrimination against data from the development cohort, with sensitivity of 70.8% and specificity of 43.5%. Next, we tested the ability of the model to predict mortality at 90 days after surgery and overall survival during follow-up. The model predicted mortality with AUC of 0.704 (95% CI 0.575–0.832) for the development cohort and 0.717 (95% CI 0.586–0.848) for the internal validation cohort (Figure 4A and B). When patients in either cohort were stratified into those whose logit values in the model were above or below the optimal cutoff of −2.43, those at higher risk of clinically significant PHLF showed significantly worse overall survival than those at lower risk (Figure 4C and D).
Discussion
Here we provide evidence that the combination of FLIS, major resection and ALBI score have the potential to predict clinically significant PHLF for hepatocellular carcinoma after resection. The same model also showed potential to predict 90 days mortality after surgery as well as overall survival. This model may improve the selection and management of patients for hepatectomy.
Our findings are consistent with previous studies suggesting that FLIS is associated with liver function.21,22 FLIS is a semi-quantitative scoring system based on three features derived hepatobiliary stage (liver parenchymal enhancement, biliary excretion of contrast agent, portal vein signal). The correlation between FLIS and liver function may be explained as follows: liver parenchymal enhancement can reflect the uptake and excretion capacity of hepatocytes to hepatobiliary specific contrast agents,30,31 biliary excretion of contrast agent often indicates the structural and functional integrity of the biliary tract,32,33 portal vein signals may indicate portal blood stasis or hepatic parenchymal fibrosis.34,35 The decrease of FLIS may indicate the impairment of liver function. A previous study involving 502 HCC patients demonstrated that the FLIS serves as an independent predictor for PHLF, and the study revealed that FLIS exhibited superior predictive performance compared to the MELD score, ALBI score, and ICG-R15.22 Indeed, our study further confirms that FLIS is an independent predictor of clinically significant PHLF and that the risk of clinically significant PHLF increases as FLIS decreases (OR: 0.680; 95% CI: 0.541–0.885; p = 0.001). Furthermore, the FLIS showed better predictive power compared with ALBI, ICG-R15, and MELD in predicting clinically significant PHLF in the overall cohort.
Several clinical models have shown potential for assessing liver function, such as models based on MELD score, ALBI score and ICG-R15, but their reliability and accuracy for predicting PHLF are controversial.36–38 The present study also failed to find significant correlations between clinically significant PHLF and either MELD score or ICG-R15, but the ALBI score was identified as an independent predictor of clinically significant PHLF. The advantage of the ALBI score may be directly related to its two indicators reflecting hepatocellular function. Declining albumin levels and elevated bilirubin are early markers of impaired hepatic synthetic function and cholestasis, which may align more closely with the progression of hepatocellular dysfunction in clinically significant PHLF.14,39 In contrast, the MELD score including creatinine is more oriented toward end-stage liver disease and renal function assessment,11,12 while ICG clearance focuses on hepatic hemodynamics.13 Our results suggest that among various clinical models reported to reflect liver function, the ALBI score may be the most suitable for predicting clinically significant PHLF, which should be explored further.
The inclusion of major resection in our model is not surprising, given that the procedure can improve prognosis of patients with large or multiple tumors,40 but it can also increase risk of subsequent liver failure because of insufficient residual liver function.41 Studies have demonstrated that patients undergoing major hepatectomy face a significantly elevated risk of PHLF relative to those undergoing minor hepatic resections.42,43 Therefore, developing a risk prediction model for clinically significant PHLF is critical, as it quantitatively assesses hepatic reserve to stratify high-risk patients and direct personalized surgical approaches.
In our study, the logistic regression model effectively stratified patients into high-risk and low-risk groups for clinically significant PHLF. Survival analysis demonstrated significantly shorter overall survival rate in high-risk patients compared to low-risk patients. This risk stratification system facilitates the identification of high-risk patient populations requiring specialized perioperative management, guiding the development of individualized clinical intervention strategies to optimize surgical decision-making processes, including determining appropriate liver resection extent and selecting optimal surgical techniques, ultimately improving patient’s survival outcomes.
Our data should be interpreted with caution in light of some limitations. One is the retrospective design of our study and the fact that our sample came from a single center. Another is the fact that the hepatocellular carcinoma in most of our sample was associated with chronic infection with hepatitis B virus, which is the case for patient populations in many parts of Asia but not in most western countries.44 The performance of our predictive model should be verified and extended in larger studies involving more medical centers and patients whose hepatocellular carcinoma is associated with alcoholic liver disease or chronic infection with hepatitis C virus. In addition, patients who had received preoperative treatment were excluded from our exclusion criteria. While this exclusion criterion ensured homogeneity in our study population, it may limit the generalizability of our findings, as many hepatocellular carcinoma patients in clinical practice often need to receive preoperative therapy. Future studies can validate the predictive power of this model in people who have received preoperative treatment.
Conclusion
Our study provides evidence that the combination of FLIS, major resection and ALBI score can preoperatively predict clinically significant liver failure after surgery as well as survival. Such prediction may help guide the selection and management of patients for hepatectomy to treat hepatocellular carcinoma.
Abbreviations
AUC, area under receiver operator characteristic; ALBI, albumin-bilirubin; FLIS, functional liver imaging score; HCC, hepatocellular carcinoma; ICG-R15, indocyanine green 15-min retention; MELD, model for end-stage liver disease; PHLF, post-hepatectomy liver failure.
Date Sharing Statement
The original anonymous dataset is available on request from the corresponding author at [email protected].
Compliance with Ethics Guidelines
This study was approved by the Institutional Review Board of Guangxi Medical University Cancer Hospital (Approval numbers: KY2024871), which waived the requirement for informed consent because participants provided written consent for their anonymized medical data to be analyzed and published for research purposes.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by grants of Guangxi Science and Technology Major Project (No. Guike AB24010038).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Gunasekaran G, Bekki Y, Lourdusamy V, Schwartz M. Surgical treatments of hepatobiliary cancers. Hepatology. 2021;73(S1):128–136. doi:10.1002/hep.31325
3. Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, Roberts LR. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol. 2019;16(10):589–604. doi:10.1038/s41575-019-0186-y
4. Asenbaum U, Kaczirek K, Ba-Ssalamah A, et al. Post-hepatectomy liver failure after major hepatic surgery: not only size matters. Eur Radiol. 2018;28(11):4748–4756. doi:10.1007/s00330-018-5487-y
5. Prodeau M, Drumez E, Duhamel A, et al. An ordinal model to predict the risk of symptomatic liver failure in patients with cirrhosis undergoing hepatectomy. J Hepatol. 2019;71(5):920–929. doi:10.1016/j.jhep.2019.06.003
6. Sparrelid E, Olthof PB, Dasari BVM, et al. Current evidence on posthepatectomy liver failure: comprehensive review. BJS Open. 2022;6(6):zrac142. doi:10.1093/bjsopen/zrac142
7. Jin S. Management of post-hepatectomy complications. WJG. 2013;19(44):7983. doi:10.3748/wjg.v19.i44.7983
8. Alizai PH, Haelsig A, Bruners P, et al. Impact of liver volume and liver function on posthepatectomy liver failure after portal vein embolization- A multivariable cohort analysis. Ann Med Surg. 2018;25:6–11. doi:10.1016/j.amsu.2017.12.003
9. Peng Y, Shen H, Tang H, et al. Nomogram based on CT–derived extracellular volume for the prediction of post-hepatectomy liver failure in patients with resectable hepatocellular carcinoma. Eur Radiol. 2022;32(12):8529–8539. doi:10.1007/s00330-022-08917-x
10. Takahashi K, Gosho M, Kim J, et al. Prediction of posthepatectomy liver failure with a combination of albumin-bilirubin score and liver resection percentage. J Am Coll Surg. 2022;234(2):155–165. doi:10.1097/XCS.0000000000000027
11. Kaiser T, Kinny-Köster B, Gnewuch C, et al. Limited comparability of creatinine assays in patients with liver cirrhosis and their impact on the MELD score. Pract Lab Med. 2017;8:41–48. doi:10.1016/j.plabm.2017.04.002
12. Trivedi HD. The evolution of the MELD score and its implications in liver transplant allocation: a beginner’s guide for trainees. ACG Case Rep J. 2022;9(5):e00763. doi:10.14309/crj.0000000000000763
13. Lam CM, Fan ST, Lo CM, Wong J. Major hepatectomy for hepatocellular carcinoma in patients with an unsatisfactory indocyanine green clearance test. J British Surg. 1999;86(8):1012–1017. doi:10.1046/j.1365-2168.1999.01204.x
14. Johnson PJ, Berhane S, Kagebayashi C, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach—the ALBI grade. JCO. 2015;33(6):550–558. doi:10.1200/JCO.2014.57.9151
15. Deng M, Ng SWY, Cheung ST, Chong CCN. Clinical application of albumin-bilirubin (ALBI) score: the current status. Surgeon. 2020;18(3):178–186. doi:10.1016/j.surge.2019.09.002
16. Costa AF, Tremblay St-Germain A, Abdolell M, Smoot RL, Cleary S, Jhaveri KS. Can contrast-enhanced MRI with gadoxetic acid predict liver failure and other complications after major hepatic resection? Clin Radiol. 2017;72(7):598–605. doi:10.1016/j.crad.2017.02.004
17. Tsuboyama T, Onishi H, Kim T, et al. Hepatocellular carcinoma: hepatocyte-selective enhancement at gadoxetic acid–enhanced MR imaging—correlation with expression of sinusoidal and canalicular transporters and bile accumulation. Radiology. 2010;255(3):824–833. doi:10.1148/radiol.10091557
18. Wang Q, Wang A, Sparrelid E, et al. Predictive value of gadoxetic acid–enhanced MRI for posthepatectomy liver failure: a systematic review. Eur Radiol. 2022;32(3):1792–1803. doi:10.1007/s00330-021-08297-8
19. Tsujita Y, Sofue K, Komatsu S, et al. Prediction of post-hepatectomy liver failure using gadoxetic acid-enhanced magnetic resonance imaging for hepatocellular carcinoma with portal vein invasion. Eur J Radiol. 2020;130:109189. doi:10.1016/j.ejrad.2020.109189
20. Bastati N, Beer L, Mandorfer M, et al. Does the functional liver imaging score derived from gadoxetic acid–enhanced mri predict outcomes in chronic liver disease? Radiology. 2020;294(1):98–107. doi:10.1148/radiol.2019190734
21. Bastati N, Beer L, Ba-Ssalamah A, et al. Gadoxetic acid-enhanced MRI-derived functional liver imaging score (FLIS) and spleen diameter predict outcomes in ACLD. J Hepatol. 2022;77(4):1005–1013. doi:10.1016/j.jhep.2022.04.032
22. Luo N, Huang X, Ji Y, et al. A functional liver imaging score for preoperative prediction of liver failure after hepatocellular carcinoma resection. Eur Radiol. 2022;32(8):5623–5632. doi:10.1007/s00330-022-08656-z
23. Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the international study group of liver surgery (ISGLS). Surgery. 2011;149(5):713–724. doi:10.1016/j.surg.2010.10.001
24. Reissfelder C, Rahbari NN, Koch M, et al. Postoperative course and clinical significance of biochemical blood tests following hepatic resection. Br J Surg. 2011;98(6):836–844. doi:10.1002/bjs.7459
25. Strasberg SM. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg. 2005;12(5):351–355. doi:10.1007/s00534-005-0999-7
26. Botta F. MELD scoring system is useful for predicting prognosis in patients with liver cirrhosis and is correlated with residual liver function: a European study. Gut. 2003;52(1):134–139. doi:10.1136/gut.52.1.134
27. Wang YY, Zhong JH, Su ZY, et al. Albumin–bilirubin versus Child–Pugh score as a predictor of outcome after liver resection for hepatocellular carcinoma. Br J Surg. 2016;103(6):725–734. doi:10.1002/bjs.10095
28. Meador KJ, Pennell PB, May RC, et al. Effects of periconceptional folate on cognition in children of women with epilepsy: NEAD study. Neurology. 2020;94(7). doi:10.1212/WNL.0000000000008757
29. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropractic Med. 2016;15(2):155–163. doi:10.1016/j.jcm.2016.02.012
30. Park SH, Kim H, Kim EK, et al. Aberrant expression of OATP1B3 in colorectal cancer liver metastases and its clinical implication on gadoxetic acid-enhanced MRI. Oncotarget. 2017;8(41):71012–71023. doi:10.18632/oncotarget.20295
31. Inokuchi Y, Fujikawa H, Uematsu M, Takashina T. Transitional phase Gd-EOB-DTPA-enhanced MRI: visual assessment of hepatic function and fibrosis based on uptake rate of Gd-EOB-DTPA. Eur J Radiol. 2022;156:110550. doi:10.1016/j.ejrad.2022.110550
32. Verloh N, Haimerl M, Rennert J, et al. Impact of liver cirrhosis on liver enhancement at Gd-EOB-DTPA enhanced MRI at 3Tesla. Eur J Radiol. 2013;82(10):1710–1715. doi:10.1016/j.ejrad.2013.05.033
33. Van Beers BE, Pastor CM, Hussain HK. Primovist, eovist: what to expect? J Hepatol. 2012;57(2):421–429. doi:10.1016/j.jhep.2012.01.031
34. Lee NK, Kim S, Kim GH, et al. Significance of the “Delayed hyperintense portal vein sign” in the hepatobiliary phase MRI obtained with Gd‐EOB‐DTPA. Magnetic Resonance Imaging. 2012;36(3):678–685. doi:10.1002/jmri.23700
35. Yang M, Zhang Y, Zhao W, Cheng W, Wang H, Guo S. Evaluation of liver function using liver parenchyma, spleen and portal vein signal intensities during the hepatobiliary phase in Gd-EOB-D TPA-enhanced MRI. BMC Med Imaging. 2020;20(1):119. doi:10.1186/s12880-020-00519-7
36. Wang Y, Zhao X, Ma L, et al. Comparison of the ability of Child‐Pugh score, MELD score, and ICG‐R15 to assess preoperative hepatic functional reserve in patients with hepatocellular carcinoma. J Surg Oncol. 2018;118(3):440–445. doi:10.1002/jso.25184
37. Zou H, Yang X, Li QL, Zhou QX, Xiong L, Wen Y. A comparative study of albumin-bilirubin score with child-Pugh score, model for end-stage liver disease score and indocyanine green R15 in predicting posthepatectomy liver failure for hepatocellular carcinoma patients. Dig Dis. 2018;36(3):236–243. doi:10.1159/000486590
38. Santol J, Kim S, Gregory LA, et al. An APRI+ALBI based multivariable model as preoperative predictor for posthepatectomy liver failure. Ann Surg. 2025;281:861–871. doi:10.1097/SLA.0000000000006127
39. Toyoda H, Johnson PJ. The ALBI score: from liver function in patients with HCC to a general measure of liver function. JHEP Rep. 2022;4(10):100557. doi:10.1016/j.jhepr.2022.100557
40. Dimitroulis D. Indications, limitations and maneuvers to enable extended hepatectomy: current trends. WJG. 2014;20(24):7887. doi:10.3748/wjg.v20.i24.7887
41. Søreide JA, Deshpande R. Post hepatectomy liver failure (PHLF) – recent advances in prevention and clinical management. Eur J Surg Oncol. 2021;47(2):216–224. doi:10.1016/j.ejso.2020.09.001
42. Reddy SK, Barbas AS, Turley RS, et al. A standard definition of major hepatectomy: resection of four or more liver segments. HPB. 2011;13(7):494–502. doi:10.1111/j.1477-2574.2011.00330.x
43. Bagante F, Ruzzenente A, Beal EW, et al. Complications after liver surgery: a benchmark analysis. HPB. 2019;21(9):1139–1149. doi:10.1016/j.hpb.2018.12.013
44. Kulik L, El-Serag HB. Epidemiology and management of hepatocellular carcinoma. Gastroenterology. 2019;156(2):477–491.e1. doi:10.1053/j.gastro.2018.08.065
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




