Back to Journals » ClinicoEconomics and Outcomes Research » Volume 17
Healthcare Resource Utilization and Cost Comparison Between Palbociclib, Abemaciclib, and Ribociclib Among Patients with HR+/HER2− Metastatic Breast Cancer
Authors Pluard TJ, Sandin R, Parikh RC , Ward MA, Stansfield L, Nham T, Esterberg E, Cha-Silva AS , Shah B
Received 13 September 2024
Accepted for publication 7 March 2025
Published 26 March 2025 Volume 2025:17 Pages 247—264
DOI https://doi.org/10.2147/CEOR.S496100
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Dean Smith
Timothy J Pluard,1 Rickard Sandin,2 Rohan C Parikh,3 Melea Anne Ward,4 Lindsay Stansfield,5 Tram Nham,3 Elizabeth Esterberg,3 Ashley S Cha-Silva,5 Bhavesh Shah6
1Saint Luke’s Cancer Institute, Kansas City, MO, USA; 2Pfizer AB, Stockholm, Sweden; 3RTI Health Solutions, Research Triangle Park, NC, USA; 4IPD Analytics, Aventura, FL, USA; 5Pfizer Inc, New York, NY, USA; 6Boston Medical Center, Boston, MA, USA
Correspondence: Bhavesh Shah, Boston Medical Center, 830 Harrison Avenue, Boston, MA, 02118, USA, Tel +1-617-638-6775, Email [email protected]
Purpose: To evaluate economic outcomes in patients with hormone receptor-positive/human epidermal growth factor receptor 2-negative (HR+/HER2−) metastatic breast cancer (mBC) treated with a first- or second-line cyclin-dependent kinase 4/6 inhibitor (CDK4/6i).
Methods: This retrospective analysis utilized Optum’s Clinformatics DataMart (January 1, 2014–September 30, 2021). Included patients had ≥ 1 pharmacy claim for palbociclib, abemaciclib, or ribociclib in first or second-line and ≥ 6 months of continuous health plan enrollment in preindex (index: date of first CDK4/6i claim) and follow-up periods. Mean all-cause per patient per month (PPPM) medical, healthcare resource utilization (HCRU) and costs, and outpatient pharmacy prescriptions costs were compared among CDK4/6is using stabilized inverse probability of treatment weighting (sIPTW).
Results: We identified 3,182 patients taking palbociclib, 286 taking abemaciclib, and 149 taking ribociclib, with median follow-ups of 20.8, 16.6, and 19.9 months, respectively. After sIPTW, palbociclib was associated with a lower risk of inpatient (IP) admissions versus abemaciclib (35.8% vs 41.6%; odds ratio: 1.31; P=0.034). No other significant differences were seen for HCRU. PPPM outpatient costs were significantly lower with palbociclib versus abemaciclib ($754; P=0.05). PPPM IP ($2,252 vs $6,286), medical ($6,948 vs $11,717), and total ($19,370 vs $23,639) costs were also lower with palbociclib versus abemaciclib, although not significant. There were no significant differences in PPPM HCRU or costs between palbociclib and ribociclib. In patients with Medicare, PPPM total medical costs were lower with palbociclib versus abemaciclib by $1,608 (P=0.04), while other costs were not significantly different. No significant differences in costs were seen with palbociclib versus ribociclib.
Conclusion: All-cause HCRU and costs were generally not different between the CDK4/6is but favored palbociclib for medical (including IP) costs versus abemaciclib. Due to limited patient numbers, uncertainty exists about abemaciclib and ribociclib cost estimations. Further studies of HCRU and costs are needed to support a cost-minimizing strategy for mBC.
Keywords: healthcare resource utilization, healthcare economics, CDK 4/6 inhibitors, HR+/HER2− metastatic breast cancer
Introduction
In 2023, an estimated 300,590 people were diagnosed with and 43,700 died from breast cancer (BC) in the United States (US).1 Furthermore, 6%–10% of new cases are metastatic BC (mBC), and 20%‒30% of patients with early-stage BC will eventually progress to mBC.2 Approximately 4% of women with a history of BC are living with metastatic disease, for whom the 5-year survival rate is less than 30%.3 The cost of treating mBC is substantial4 and is projected to increase from $75 billion in 2020 to $152.4 billion by 2030 owing to an increase in patient numbers.5
The majority of patients with mBC have the hormone receptor-positive/human epidermal growth factor receptor 2-negative (HR+/HER2−) subtype;3 guidelines recommend treating these patients with a cyclin-dependent kinase 4/6 inhibitor (CDK4/6i) in combination with endocrine therapy.6 Three CDK4/6is have been approved by the US Food and Drug Administration7–9 based on positive results from Phase 3 clinical trials, which reported progression-free survival (PFS) benefits with CDK4/6i treatment versus standard of care, with manageable tolerability profiles10–16 and maintaining patient quality of life (QoL).17–22 To date, no head-to-head randomized controlled trials have compared different CDK4/6is; however, indirect treatment comparisons23,24 and real-world evidence comparisons25,26 suggest no difference in efficacy, but differing safety profiles27,28 and impacts on health-related QoL.29 It is less clear how different CDK4/6is impact the economic burden of HR+/HER2– mBC.
Given the significant economic burden of mBC, healthcare providers and decision makers should consider healthcare resource utilization (HCRU) and costs alongside the efficacy and safety of proposed interventions. However, HCRU and cost data are usually not collected in clinical trials, and few studies evaluate these outcomes for CDK4/6i use in clinical practice. A recent article by Burne et al used data from the MarketScan Commercial and Medicare Supplemental database to compare HCRU and healthcare costs across all 3 CDK4/6is.30 Total healthcare costs, medical costs, and pharmacy costs were significantly lower with ribociclib versus abemaciclib, but similar to palbociclib. Although this study provides insights into HCRU and costs associated with CDK4/6i use, it does have important limitations, particularly with its short treatment period (driven by a high prevalence of patients with later-line therapies) that may restrict its generalizability. To better inform decision makers, studies are needed to better understand HCRU and costs during a longer treatment period associated with current CDK4/6i standard of care use in the first and second lines.
There is further value in understanding which types of HCRU and costs are most important and how these change over the phases of care: from the initial period when treatment is started to the continuation of treatment, and finally the last period before treatment discontinuation, particularly if differential CDK4/6i toxicity profiles may be driving cost variations. As most patients with HR+/HER2– mBC are aged ≥ 65 years and typically have complex needs (eg, because of comorbidity burden), it is important to evaluate HCRU and costs in these patients as well.
To address these evidence gaps, the aim of our study was to assess all-cause HCRU and costs among adult patients with HR+/HER2– mBC who received a CDK4/6i in the first or second line over a period that captures the full course of treatment in real-world clinical practice. The study used administrative claims data from Optum Clinformatics DataMart (CDM), which contains a large commercial and Medicare-insured population.
Methods
Data Source
This study was conducted using Optum CDM standard view with mortality plus race and ethnicity data from January 1, 2014 to September 30, 2021. This database has been used previously to conduct similar studies.31–34 Optum has administrative health insurance claims for members with medical and pharmacy coverage enrolled in commercial and Medicare Advantage health plans across all 50 states in the US. Longitudinal patient-level information is available on health plan enrollment, demographics, HCRU across different medical settings, and medication use. Optum data are deidentified and comply with the 1996 health Insurance Portability and Accountability Act.31–34
Study Design
This was an observational retrospective cohort study of patients identified from February 3, 2015 (date of first CDK4/6i treatment approval) to September 30, 2020 (Supplementary Figure S1). The study index date was defined as the date of the first observed claim for a CDK4/6i prescription during the patient selection window. The preindex period consisted of a 6-month period prior to the index date, and the follow-up period extended from the index date until the end of health or drug plan enrollment, death, or the end of study period. For the evaluation of study outcomes, all patients were followed from the study index date through discontinuation of CDK4/6i, disenrollment from health or drug plan, or the end of study period, whichever occurred first.
Sample Selection
Adult patients with HR+/HER2– mBC with ≥ 1 prescription claim for CDK4/6i therapy in the first- or second-line setting were included (Figure 1). Patients with mBC were classified as having de novo mBC if they had evidence of secondary malignancy within a 60-day period before or after the first medical encounter with a diagnosis of BC. Patients with evidence of secondary malignancy more than 60 days after the first medical encounter with a diagnosis of BC were classified as patients who progressed or recurred to mBC. Consistent with previous studies,30,35 HR+/HER2– status of patients was based on an observed claim for hormonal therapy or other therapy (ie, everolimus, olaparib, talazoparib) directed toward HR+/HER2–BC, or CDK4/6i and no receipt of any treatment indicated for HER2+ BC, any time after first evidence of BC.
Patients were required to have ≥ 6 months of continuous health plan enrollment in the preindex and follow-up periods,36 except for patients who died within the first 6 months after the study index date. Patients were excluded if they had evidence of cancers other than BC in the preindex period or were treated with multiple CDK4/6is during the follow-up period. Following identification of the study population, patients were categorized into 3 mutually exclusive cohorts based on the CDK4/6i they received on the index date: abemaciclib, ribociclib, or palbociclib.
Study Outcomes
Patient characteristics were assessed in the 6-month preindex period or at the study index date. Patient characteristics assessed included: age, gender, race, region, health plan type (commercial and Medicare), year of mBC diagnosis and initiation of CDK4/6i, National Cancer Institute’s Comorbidity Index (NCICI),37 type of mBC diagnosis (de novo or recurrent), and organ-level metastatic site.
HCRU and costs were assessed separately for each CDK4/6i cohort in aggregate and by care setting/resource. Per-patient-per-month (PPPM) HCRU and costs during CDK4/6i therapy were calculated by dividing the number of times the resource was utilized and the costs incurred by the total duration of CDK4/6i-based therapy. HCRU included all healthcare claims (inpatient [IP] admissions, total hospital days, emergency department [ED] visits, office visits, outpatient hospital, urgent care, outpatient pharmacy claims, and other outpatient/ancillary care) regardless of the diagnoses and procedures. Utilization of electrocardiogram (ECG) was also assessed. HCRU for IPs, total hospital days, hospital outpatient visits, and ED visits are only reported for patients who had ≥ 1 such visit. Healthcare costs were assessed from a payer perspective and included the estimated allowed amounts reported for each claim. Total medical costs for each patient comprised patient-level IP costs, ED costs, and all outpatient costs. Outpatient pharmacy costs were based on wholesale acquisition costs for CDK4/6i and endocrine partner, including dose adjustments and wastage.
A phase of care approach to assess costs during the initial (maximum of 3 months after initiation of CDK4/6i-based treatment), continuing (time period between initial period and terminal/discontinuation period), and final (maximum of 3 months before death or CDK4/6i-based treatment discontinuation) time periods, respectively, was used (Supplementary Figure S2), similar to that typically used to estimate direct medical costs among patients with cancer.38 A subgroup analysis restricted to patients aged ≥ 65 years enrolled in Medicare Advantage was conducted. All costs were converted to 2021 US dollars using the medical care component of the US Consumer Price Index.
Statistical Analysis
All study measures were summarized descriptively. Propensity score-based stabilized inverse probability treatment weighting (sIPTW) was used to balance cohort baseline characteristics. The multinomial logistic regression model included patient demographics (age at index, gender, race, and health plan type) and clinical characteristics (de novo mBC, bone-only disease at index treatment, brain/CNS metastasis at index treatment, visceral disease at index treatment, and NCICI score) that may influence the choice of treatment as independent variables. Similar to Burne et al,30 year of mBC diagnosis and CDK4/6i treatment start were not corrected for, as this would reduce sample size significantly due to the large imbalance in year of treatment introduction between the CDK4/6is and downweigh patients who were treated with palbociclib in the years 2015 and 2016. In line with Burne et al, baseline HCRU and costs were also not adjusted for; however, adjustment of other baseline characteristics such as age, would reduce potential cost differences at baseline between the treatments. Individual propensity score derived via multinomial logistic regression was used to compute individual sIPTW. A threshold for the standardized mean difference (SMD) of < 0.10 was used to indicate balanced cohorts. Factors with SMD of ≥ 0.10 were adjusted again in the outcome assessment regressions.
Regression analyses with sIPTW were used to compare HCRU and costs during the follow-up period. Logistic regression was used to evaluate the association between cohorts and HCRU. Incidence rate ratios (IRRs) for HCRU count outcomes were calculated using negative binomial regression. Generalized linear models with a log link function and gamma distribution for the error term were used for cost outcomes.39 Two-part models were used for predicting IP, ED, and outpatient costs. All models considered the palbociclib cohort as the reference category and were run separately for the overall population and ≥ 65 years of age subgroup. Comparative results are reported with P values, where P ≤ 0.05 was considered statistically significant.
Results
The final analytical sample included 3,617 patients who received first- or second-line CDK4/6i treatment (3,182 palbociclib [88%], 286 abemaciclib [8%], and 149 ribociclib [4%]) (Figure 1). A total of 179 patients with use of multiple CDK4/6is observed during the study follow-up were excluded. The median duration of follow-up for the palbociclib, abemaciclib, ribociclib cohorts was 20.8 (range: 0.3–79.4), 16.6 (range: 0.03–46.3), and 19.9 months (range: 0.9–52.9), respectively. Approximately 60% of patients received first-line CDK4/6i treatment (palbociclib: 64%; abemaciclib: 57%; ribociclib: 62%) and the remainder in the second line. The median time of initiation of index CDK4/6i from mBC diagnosis was 1.3 months for palbociclib, 2.1 months for abemaciclib, and 2.4 months for ribociclib. The Kaplan–Meier estimated median time to treatment discontinuation was 16.7 months (95% CI: 13.2–19.6) for abemaciclib, 16.1 months (95% CI: 15.0–17.1) for palbociclib, and 14.4 months (95% CI: 11.0–18.0) for ribociclib.
Demographics and Clinical Characteristics
Unadjusted and sIPTW-adjusted baseline demographic and clinical characteristics are presented in Table 1. Median age ranged from 69.0‒71.0 years, with 62.9%‒74.5% of patients aged ≥ 65 years, and 65.4%‒77.2% enrolled in Medicare. Approximately half of patients had de novo mBC, 36.5%–40.3% had visceral metastases, 27.6%–32.2% had bone-only metastases, and 5.4%–14.3% had brain/CNS metastases. Patient comorbidity burden was high, with an unadjusted NCICI ≥ 2 score ranging from 41.6%–48.3%. Of the patients enrolled in Medicare, 29.7% were enrolled in a health maintenance organization (HMO), 8.7% were enrolled in preferred provider organizations (PPOs), and 61.6% in others. Among commercially enrolled patients, 72.8% were enrolled in point-of-service, 13.3% in HMOs, 10.4% in exclusive provider organizations, 1.8% in indemnity plans, 1.3% in PPOs, and 0.5% in others.
 |
Table 1 Baseline Demographic and Clinical Characteristics of Patients with mBC Receiving First- or Second-Line Treatment with a CDK4/6i Before and After sIPTW Adjustment |
Before sIPTW, relative to the palbociclib cohort, the abemaciclib cohort included fewer patients aged 75–84 years (18.9% vs 24.7%, SMD = 0.14), fewer White (64.7% vs 69.7%, SMD = 0.11) and Hispanic patients (5.6% vs 9.2%, SMD = 0.14), more Asian patients (4.9% vs 3.0%, SMD = 0.10), fewer patients with bone-only metastases (27.6% vs 32.2%, SMD = 0.10), and more patients with brain metastases (14.3% vs 6.3%, SMD = 0.27).
Before sIPTW, relative to the palbociclib cohort, the ribociclib cohort had fewer patients aged 55–64 years (14.1% vs 20.8%, SMD = 0.18), more patients aged 65–74 years (39.6% vs 34.7%, SMD = 0.10) and 75–84 years (29.5% vs 24.7%, SMD = 0.11), more patients enrolled in Medicare (77.2% vs 67.0%, SMD = 0.23), fewer White patients (60.4% vs 69.7%, SMD = 0.20), more patients with de novo mBC (52.4% vs 46.9%, SMD = 0.11), and fewer patients with a NCICI score < 1 (31.5% vs 36.6%, SMD = 0.11) but more with a score > 2 (48.3% vs 41.8%, SMD = 0.13). After sIPTW adjustment, demographic and clinical characteristics of the 3 cohorts were well balanced (SMD < 0.10), and a double adjustment in regression was not needed. After sIPTW adjustment the median PPPM baseline costs were not different; $4,475 for ribociclib, $4,631 for palbociclib, and $4,928 for abemaciclib (absolute SMD: palbociclib vs ribociclib, 0.04; palbociclib vs abemaciclib, 0.09).
HCRU
During treatment, over a third of patients had an IP. The proportion of these patients was significantly higher with abemaciclib versus palbociclib (41.6% vs 35.8%; odds ratio: 1.31; P = 0.03). In addition, mean number of PPPM IPs were highest in the abemaciclib cohort (0.50), followed by the palbociclib (0.31) and ribociclib (0.28) cohorts (Table 2 and Supplementary Figure S3), with the estimated IRR trending toward being higher with abemaciclib versus palbociclib, but was not statistically significant (IRR: 1.32, P = 0.06).
Mean PPPM number of hospital days was highest with abemaciclib (2.85 days), followed by palbociclib (2.26 days) then ribociclib (2.24 days), and the estimated IRR trended toward a higher number with abemaciclib versus palbociclib, although this was not statistically significant (IRR: 1.43, P = 0.08). Mean PPPM number of and proportion of patients with ED visits, office visits, and prescriptions were similar across all 3 CDK4/6i cohorts.
Patients in the ribociclib cohort had a higher rate of ECG utilization compared with palbociclib, while no statistically significant differences were observed for any other HCRU outcomes (Table 2 and Supplementary Figure S3).
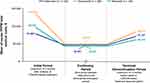
Healthcare Costs
After sIPTW adjustment, mean PPPM total costs were lowest in the palbociclib cohort ($19,370), followed by the ribociclib cohort ($20,951), then the abemaciclib ($23,639) cohort (Table 2 and Figure 2). This resulted in monthly incremental, but not statistically significant, mean total healthcare costs of $4,268 PPPM (P = 0.17) with abemaciclib and $1,580 (P = 0.40) with ribociclib versus palbociclib. Numerically, medical costs were higher with abemaciclib ($11,717; incremental costs vs palbociclib: $4,769; P = 0.09) and ribociclib ($8,407; incremental costs vs palbociclib: $1,459; P = 0.43) versus palbociclib ($6,948), but not statistically significant (Table 2 and Figure 3). In turn, these costs were driven by numerically higher PPPM IP costs with abemaciclib ($6,286; incremental cost vs palbociclib: $4,034, P = 0.14) and ribociclib ($4,362; incremental cost vs palbociclib: $2,110; P = 0.23) versus palbociclib ($2,252), although differences were not statistically significant.
Mean PPPM outpatient visit costs were significantly higher with abemaciclib versus palbociclib (incremental cost: $754, P = 0.05) but not for ED visits (incremental cost: –$19, P = 0.35). No differences were observed between ribociclib and palbociclib for ED visits (incremental cost: –$20, P = 0.65) or outpatient visits (incremental cost: –$631, P = 0.07). Finally, outpatient pharmacy costs (including dose adjustments and wastage) were not different across the 3 cohorts, ranging from $11,921 with abemaciclib (incremental cost vs palbociclib: –$501; P = 0.31) to $12,544 with ribociclib (incremental cost vs palbociclib: $122, P = 0.83).
When considering phase of care, PPPM costs were highest during the initial phase, followed by the terminal/discontinuation phase and then the continuing phase (Figure 4). During the initial period, mean PPPM total medical costs were highest with abemaciclib ($13,425), followed by ribociclib ($9,638) and palbociclib ($7,869). Compared with palbociclib, incremental initial period costs were higher (borderline significant) for abemaciclib (incremental cost: $5,556 [95% CI: -$71 to $11,183], P= 0.05) and not statistically different for ribociclib (incremental cost: $1,769 [95% CI: -$2,602 to $6,139], P = 0.43). During the continuing phase, mean PPPM total medical costs were similar across all cohorts, $4,247 for ribociclib (incremental cost compared to palbociclib: $-345 [95% CI: -$1,422 to $733], P= 0.53), $4,591 for palbociclib, and $4,924 for abemaciclib (incremental cost compared to palbociclib: $332 [95% CI: -$545 to $1,209], P = 0.46). Finally, during the terminal/discontinuation phase, abemaciclib had the highest mean PPPM total medical costs ($8,372; incremental cost compared to palbociclib: $1,265 [95% CI: -$1,022 to $3,552], P = 0.28) followed by palbociclib ($7107) and ribociclib ($6,125; incremental cost compared to palbociclib: -$982 [95% CI: -$2,921 to $957], P = 0.32).
HCRU and Costs Among Patients Aged ≥65 years and Enrolled in Medicare Advantage
HCRU and costs between cohorts, for patients aged ≥65 years and enrolled in Medicare were similar to the total population (Table 2; Supplementary Figures S4 and S5). No statistically significant differences were observed between CDK4/6is for HCRU outcomes, except for the mean PPPM number of prescriptions, which was significantly lower with abemaciclib (4.08; IRR: 0.88; P < 0.01) and ribociclib (3.98; IRR: 0.88; P = 0.03) versus palbociclib (4.52).
Mean PPPM total medical costs were significantly higher with abemaciclib versus palbociclib ($8,085 vs $6,255; incremental cost: $1,608; P = 0.04), while total healthcare cost was not different ($19,040 vs $18,192; incremental cost: $952; P = 0.37). There were no differences in PPPM total medical costs ($7,452 vs $6,255; incremental cost: $1,283; P = 0.49), or total healthcare cost ($18,095 vs $18,192; incremental cost: $411; P = 0.85) with ribociclib compared to palbociclib. Finally, outpatient pharmacy costs were numerically lower, but not statistically significant, with abemaciclib ($10,956) and ribociclib ($10,643) compared with palbociclib ($11,937; incremental cost vs ribociclib: ‒$921, P = 0.15 and incremental cost vs ribociclib: ‒$1,192, P = 0.09).
Discussion
With a median follow-up of over 20 months, our study provides a unique real-world HCRU and cost comparison of alternative CDK4/6i choices in patients with HR+/HER2– mBC. To the best of our knowledge, our study is the first to assess HCRU and costs of these treatments in the US in the approved 1st and 2nd line mBC indications and spanning a normal treatment period with different phases of treatment. Other than IP admissions, which were 30% more likely for patients taking abemaciclib (compared with palbociclib), we found that all-cause HCRU was generally not significant across the 3 CDK4/6is. Furthermore, no significant differences in total costs between the treatments were found; however, compared with palbociclib, there were higher PPPM outpatient medical visit costs and a trend for higher total medical costs, driven primarily by higher IP costs with abemaciclib. In addition, there was a strong trend for higher medical costs during the initial 3-month treatment period with abemaciclib. No differences in costs were seen between palbociclib and ribociclib across cost categories. Similar results were seen in the subgroup of patients aged ≥ 65 years and enrolled in Medicare Advantage. However, the comparison between the treatments in our study is associated with uncertainty due to a low number of patients taking abemaciclib and ribociclib (12% in total), and in the population of 65 and older (13%).
Our results are in line with those of Burne et al,30 in which higher total costs were seen with abemaciclib compared with palbociclib and ribociclib, but not between palbociclib and ribociclib. Although cost differences were not formally tested between abemaciclib and palbociclib in Burne et al,30 mean adjusted PPPM total costs were found to be $6,634 higher with abemaciclib (ribociclib vs abemaciclib [–$7,886]) versus palbociclib, compared with $4,268 higher (not significant) in our study. In both studies, cost differences were primarily derived from total medical costs, driven in turn by IP and outpatient costs. Although both studies found no significant difference between palbociclib and ribociclib in total costs, some differences in the direction and magnitude of the incremental costs exist. In Burne et al,30 mean PPPM total and medical cost were numerically lower with ribociclib compared with palbociclib ($859 and $841, respectively), while in our study, these costs were numerically higher ($1,580 and $1,459, respectively). IP costs were near identical between ribociclib and palbociclib in Burne et al30 but $2,110 higher PPPM for ribociclib in our study. Contrary to Burne et al, who found significant outpatient PPPM cost savings with ribociclib versus palbociclib ($1,245), no significant difference was seen in our study.
Such variations may come down to differences in study design. First, our study was restricted to patients receiving CDK4/6is as first- or second-line treatment, more reflective of current clinical practice,40,41 whereas almost half of patients in Burne et al received a CDK4/6i in the third or later line. Second, mean treatment duration was considerably longer in our study than in Burne et al (17.5–24.4 vs 3.9–8.8 months, respectively).30 Third, some parameters being weighted varied between studies, for example, menopausal status. Finally, patients in our study were considerably older than those in Burne et al (after reweighting: aged 69.0‒70.0 years compared with 58.5‒59.0 years, respectively); however, our median age is similar to that reported by SEER in which the median age for HR+/HER2‒ BC diagnosis was 64.0 years,42 with nearly half [48.6%] of patients with HR+/HER2– “distant” BC aged ≥ 65.0 years. Thus, considering these points together, our study is arguably the more representative of current CDK4/6i standard of care for patients with HR+/HER2– mBC.
Our results highlight the importance of accounting for all costs of care, including medical and pharmacy costs, as differences between CDK4/6is may be more pronounced depending on what is being considered. For instance, total PPPM costs were $23,639 with abemaciclib and $19,360 with palbociclib, with higher medical costs ($11,717 vs $6,948) versus outpatient pharmacy costs ($11,921 vs $12,422) driving most of the total cost difference, whereas the drug costs were only $501 PPPM lower with abemaciclib than palbociclib. This effect was more evident in the subgroup of patients aged ≥ 65 years enrolled in Medicare, whereby outpatient pharmacy costs trended lower with abemaciclib and ribociclib compared with palbociclib, but total medical costs were higher (statistically significant with abemaciclib). This real-world finding that differences in medical costs can be higher or outweigh any drug cost differences has implications for cost-effectiveness modeling and result interpretation.
Our study highlights differences in costs during different phases of care over the course of treatment. For instance, mean PPPM medical costs during the first 3 months were highest with abemaciclib ($13,425), followed by ribociclib ($9,638) and palbociclib ($7,869). There was a strong trend (incremental cost: $5,556 [95% CI: -$71 to $11,183]; P = 0.05) in higher cost with abemaciclib versus palbociclib during this initial treatment period, but not for ribociclib. On the other hand, medical costs during the treatment period in between the first and last periods (ie, the continuing period) were lower compared with the initial period and not significant ($4,247‒$4,924) across CDK4/6is. Finally, costs in the terminal/discontinuation period, while showing greater spread than the continuing period, were still not significantly different between the treatments (abemaciclib $8,372, palbociclib $7,107, and ribociclib $6,125).
There are several possible explanations for the medical cost differences between CDK4is and the cost patterns seen over time. CDK4/6is have different toxicity profiles,27,28 which may have contributed to the differences between treatments during the first 3 months. Compared with palbociclib, an indirect treatment comparison shows that abemaciclib is more associated with diarrhea, vomiting, and infections, but less associated with neutropenia. Treatment of gastrointestinal toxicity and infections is more costly compared with CDK4/6i-induced neutropenia, which is primarily managed by dose adjustments and interruption. Patients taking abemaciclib were also more likely to discontinue treatment due to adverse events (AEs) compared with palbociclib.27,28 In addition, an indirect comparison of patient-reported outcomes based on PALOMA 3 and MONARCH-2 found significantly different changes from baseline favoring palbociclib over abemaciclib in QoL, nausea/vomiting, appetite loss, diarrhea, and systemic therapy side effects.29 Differences in AE profiles were also seen between ribociclib and palbociclib, with more vomiting and infections with ribociclib but less neutropenia; there were more discontinuations with ribociclib in the second line, but no difference in the first line.27,28 Notably, in this study, AE costs were embedded in the aggregate medical costs of the Optum system and were not examined to identify HCRU and costs due to specific causes. Thus, future more detailed research is warranted to better understand the impact of the specific AE/tolerability profiles of CDK4/6is, particularly during the initial phase of treatment, on real-world HCRU and costs.
From the perspectives of payers and formulary decision-makers, our results indicate they should consider all types of healthcare costs as there may be differences across cost types, such as medical costs (likely explained in part by differences in tolerability), but not necessarily in overall costs. At this time, there is currently not enough information to prioritize between the CDK4/6i treatments from an overall cost perspective. Even from an effectiveness perspective, there is evidence to suggest that there may be no significant differences between the treatments in US clinical practice; a recently published (January 2025), large retrospective study using real-world data from the Flatiron Health electronic health record database (February 2015 through November 2023), reported that there were no significant differences in overall survival after sIPTW adjustment across >9,000 patients with HR+/HER2− mBC who were treated with first-line palbociclib, ribociclib, or abemaciclib in combination with an aromatase inhibitor, with similar findings observed across older patient subgroups.43 Taken together, all 3 agents may therefore provide the same pharmacoeconomic value. Nevertheless, given differences in tolerability profiles and monitoring requirements for these agents to accommodate the needs of comorbid and fragile patients with varying sensitivity to AEs (particularly in the Medicare eligible population treatments), the most conservative approach would be to have all 3 CDK4/6i options on the formulary. With continued emergence of real-world evidence on the comparative effectiveness of CDK4/6is, there are new opportunities for assessing their cost-effectiveness to more precisely determine their economic value and to help reduce the overall healthcare economic burden of mBC.
Study Limitations
This study is subject to the inherent limitations of using claims databases such as vulnerability to coding errors or underreporting of clinical conditions/events that do not trigger a billable event. Claims data reflect pharmacy fills of medication rather than actual use by patients. Treatments are not randomly assigned and therefore treatment selection may be confounded. Additionally, there is no information in claims data to directly identify mBC or HR+/ HER2– status; therefore, we used an algorithm based on treatments and procedures.30
Clinical characteristics not captured in the database, such as ECOG performance status or number of metastases, which may potentially affect CDK4/6i choice, could not be corrected by sIPTW. The year of initiation of CDK4/6i and baseline costs (which may include significant diagnostic costs) were not included as independent variables in the multinomial logistic regression computed to derive sIPTW weights. However, median PPPM total costs at baseline after sIPTW were almost identical between the treatments (a difference of less than $300; absolute SMD < 0.10) after sIPTW adjustment of other baseline characteristics. Patients with evidence of secondary malignancy within 60 days of initial BC diagnosis were considered to have de novo mBC, which may have resulted in misclassification of patients. However, such a criterion has been used previously,44 and the treatment-based cohorts were balanced for de novo mBC status after sIPTW adjustment. Patient frailty was not assessed, although it is a strong predictor of treatment toxicity,45 negatively impacts QoL,46 and is associated with a higher risk of unfavorable discharge, prolonged hospital stay, and greater hospital costs.47 Given the large proportion of frail patients with mBC,47 understanding whether frailty contributes to differences seen among CDK4/6i medical costs, including the potential for channeling bias,48 (drug tolerability driving prescription)27 is important. Although comorbidities were assessed using the NCICI score, individual comorbidities that may drive costs were not assessed due to low patient numbers in the abemaciclib and ribociclib cohorts. Finally, reasons behind CDK4/6i choice are not recorded in the Optum claims data. However, biases due to differences over time in available CDK4/6 treatments may have affected the choice of treatment in our study, which could not be controlled for.
In our study, similar to Burne et al, the majority (88%) of the patients were treated with palbociclib and included a low number of patients treated with abemaciclib (286 vs 100) or ribociclib (149 vs 102) compared with palbociclib (3,182 vs 4,118), consistent with their later approvals.8,9 Consequently, there is uncertainty about the HCRU and costs associated with abemaciclib and ribociclib in both studies. In our study, mean treatment duration was approximately 20 months, in line with PFS from recent US real-world studies.49–51 Therefore, considering the long-term use of branded CDK4/6is, choice of treatment could have a significant financial impact for payers, should total cost difference be close to our estimates (eg, an incremental PPPM cost of $4,268 for abemaciclib vs palbociclib), and significant. Approximately 164,000 women are living with mBC in the US,3 and their overall healthcare costs are high4 and expected to increase.5 Additional studies that include more patients taking abemaciclib and ribociclib are needed to better understand if there are cost differences between the CDK4/6is and to assess association with tolerability. Furthermore, patients with use of multiple CDK4/6is in this study were excluded, a patient group that may be of interest for future research.
Our findings may not be generalizable to the uninsured population or populations insured through other health plans; however, to address variability across health plans and provider contracts, Optum performs standardization of prices to increase database generalizability, and the prices used for the analysis reflect allowed payments. Similarly, two-thirds of our study population received their treatment via Medicare Advantage. Although enrollment in private Medicare Advantage plans increased from 28% in 2013 to 46% in 2022, and a Commonwealth Fund policy brief suggests that beneficiaries enrolled in Medicare and Medicare Advantage plans are similar after removing patients on special needs plans, our Medicare Advantage subgroup data may not be generalizable to patients receiving Medicare or who have a different Medicare plan type.52,53 Furthermore, rural populations are much less represented in the Optum database than urban populations. Due to unavailability of patient and provider ZIP Codes, the study was not able to adjust for patients’ geographic location (ie, rural/urban) or account for distance between patients and healthcare facilities.
Conclusions
This study compared HCRU and associated costs between palbociclib, abemaciclib, and ribociclib for treating patients with HR+/HER2– mBC in the first- and second-line settings. All-cause HCRU and costs were generally similar between the CDK4/6is, although compared with palbociclib, there were more IP admissions, higher outpatient medical costs, and a trend for higher total medical costs, driven primarily by higher IP costs with abemaciclib. In addition, there was a strong trend for higher medical costs during the initial treatment period with abemaciclib. There were no differences in costs between palbociclib and ribociclib. Further research with larger abemaciclib and ribociclib cohorts, overall and in important subgroups such as patients 65 years and older, and deeper exploration of types and underlying causes of costs is warranted to reduce uncertainty about the costs of abemaciclib and ribociclib and to refine the understanding of CDK4/6i-related costs in all phases of treatment, including those related to variations in the AE/tolerability profiles between the CDK4/6is. This may help reduce medical and IP costs, considering CDK4/6is are oral treatments, to support a cost-minimization strategy for mBC, which carries a high financial burden.
Abbreviations
AE, adverse event; BC, breast cancer; CDK4/6i, cyclin-dependent kinase 4/6 inhibitor; CDM, Clinformatics DataMart; CNS, central nervous system; ECG, electrocardiogram; ED, emergency department; HCRU, healthcare resource utilization; HR+/HER2– hormone receptor-positive/human epidermal growth factor receptor 2-negative; IP, inpatient; IRR, incidence rate ratio; mBC, metastatic breast cancer; NCICI, National Cancer Institute’s Comorbidity Index; PFS, progression-free survival; PPPM, per patient per month; QoL, quality of life; SD, standard deviation; sIPTW, stabilized inverse probability treatment weighting; SMD, standardized mean difference; US, United States.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Ethics Approval
This was a retrospective database study without prospectively enrolled participants. All database records are de-identified and fully compliant with US patient confidentiality requirements, including the Health Insurance Portability and Accountability Act of 1996. The data used for this study did not involve the interaction or interview with any subjects and the data does not include any individually identifiable data and, as such, is not research involving human subjects. Accordingly, ethical approval was not required for this study.
Acknowledgments
Medical writing support was provided by Helen Fishpool and Martin Dalziel of Oxford PharmaGenesis Inc., Newtown, PA, USA, and was funded by Pfizer Inc.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was sponsored by Pfizer Inc.
Disclosure
T. J. Pluard: Consulting or Advisory Role: Pfizer, MacroGenics, Genentech, Sermonix, Arvinas, Stemline, Scorpion, Jazz Pharmaceuticals, Merck, Seattle Genetics, Novartis, H3 Biomedicine, AstraZeneca/Daiichi Sankyo, Gilead Sciences; speakers’ bureau: Genentech/Roche, Novartis, Seattle Genetics, Gilead Sciences; Research Funding: Seattle Genetics (Inst), Zymeworks (Inst), HiberCell (Inst), Pfizer (Inst), H3 Biomedicine (Inst), DAEHWA Pharmaceutical (Inst), G1 Therapeutics (Inst), Olema Pharmaceuticals (Inst), Dantari (Inst), AstraZeneca/Daiichi Sankyo (Inst), Orinove (Inst), Sanofi (Inst). T. J. Pluard was a paid consultant to Pfizer Inc. in connection with the development of this manuscript. R. Sandin: Employee of and owns stock in Pfizer Inc. AB. R. C. Parikh: Employee of RTI Health Solutions, which received funding from Pfizer Inc. in connection with the development of this manuscript. M. Ward: Employee of IPD Analytics. L. Stansfield: Employee and stockholder of Pfizer Inc. T. Nham: Employee of RTI Health Solutions, which received funding from Pfizer Inc. in connection with the development of this manuscript. E. Esterberg: Employee of RTI Health Solutions, which received funding from Pfizer Inc. in connection with the development of this manuscript. A. S. Cha-Silva: Employee & stockholder of Pfizer Inc. B. Shah: Consultant or advisory role Pfizer Inc. The authors report no other conflicts of interest in this work.
References
1. American Cancer Society. Cancer facts and figures. Available from: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2023/2023-cancer-facts-and-figures.pdf.
2. Wang R, Zhu Y, Liu X, et al. The clinicopathological features and survival outcomes of patients with different metastatic sites in stage IV breast cancer. BMC Cancer. 2019;19(1):1091. doi:10.1186/s12885-019-6311-z
3. Giaquinto AN, Sung H, Miller KD, et al. Breast cancer statistics, 2022. Ca Cancer J Clin. 2022;72(6):524–541. doi:10.3322/caac.21754
4. McGarvey N, Gitlin M, Fadli E, Chung KC. Increased healthcare costs by later stage cancer diagnosis. BMC Health Serv Res. 2022;22(1):1155. doi:10.1186/s12913-022-08457-6
5. Gogate A, Wheeler SB, Reeder-Hayes KE, et al. Projecting the prevalence and costs of metastatic breast cancer from 2015 through 2030. JNCI Cancer Spectr. 2021;5.
6. Referenced with permission from the NCCN clinical practice guidelines in oncology (NCCN guidelines®) for guideline name V.3.2023. © National Comprehensive Cancer Network, Inc. 202X. All rights reserved. To view the most recent and complete version of the guideline, go online to NCCN.org.
7. FDA. IBRANCE® (palbociclib) Prescribing Information. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/207103s008lbl.pdf.
8. FDA. KISQALI® (ribociclib) Prescribing Information. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/209092s003lbl.pdf.
9. FDA. VERZENIO® (abemaciclib). Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/208716s006s007s008lbl.pdf.
10. Cristofanilli M, Turner NC, Bondarenko I, et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol. 2016;17(4):425–439. doi:10.1016/S1470-2045(15)00613-0
11. Hortobagyi GN, Stemmer SM, Burris HA, et al. Updated results from MONALEESA-2, a Phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Ann Oncol. 2018;29(7):1541–1547. doi:10.1093/annonc/mdy155
12. Johnston S, Martin M, Di Leo A, et al. MONARCH 3 final PFS: a randomized study of abemaciclib as initial therapy for advanced breast cancer. NPJ Breast Cancer. 2019;5(1):5. doi:10.1038/s41523-018-0097-z
13. Rugo HS, Finn RS, Dieras V, et al. Palbociclib plus letrozole as first-line therapy in estrogen receptor-positive/human epidermal growth factor receptor 2-negative advanced breast cancer with extended follow-up. Breast Cancer Res Treat. 2019;174(3):719–729. doi:10.1007/s10549-018-05125-4
14. Slamon DJ, Neven P, Chia S, et al. Phase III randomized study of ribociclib and fulvestrant in hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer: MONALEESA-3. J Clin Oncol. 2018;36(24):2465–2472. doi:10.1200/JCO.2018.78.9909
15. Sledge GW, Toi M, Neven P, et al. MONARCH 2: abemaciclib in combination with fulvestrant in women with HR+/HER2- advanced breast cancer who had progressed while receiving endocrine therapy. J Clin Oncol. 2017;35(25):2875–2884. doi:10.1200/JCO.2017.73.7585
16. Tripathy D, Im SA, Colleoni M, et al. Ribociclib plus endocrine therapy for premenopausal women with hormone-receptor-positive, advanced breast cancer (MONALEESA-7): a randomised phase 3 trial. Lancet Oncol. 2018;19(7):904–915. doi:10.1016/S1470-2045(18)30292-4
17. Rugo HS, Dieras V, Gelmon KA, et al. Impact of palbociclib plus letrozole on patient-reported health-related quality of life: results from the PALOMA-2 trial. Ann Oncol. 2018;29(4):888–894. doi:10.1093/annonc/mdy012
18. Harbeck N, Iyer S, Turner N, et al. Quality of life with palbociclib plus fulvestrant in previously treated hormone receptor-positive, HER2-negative metastatic breast cancer: patient-reported outcomes from the PALOMA-3 trial. Ann Oncol. 2016;27(6):1047–1054. doi:10.1093/annonc/mdw139
19. Fasching PA, Beck JT, Chan A, et al. Ribociclib plus fulvestrant for advanced breast cancer: health-related quality-of-life analyses from the MONALEESA-3 study. Breast. 2020;54:148–154. doi:10.1016/j.breast.2020.09.008
20. Harbeck N, Franke F, Villanueva-Vazquez R, et al. Health-related quality of life in premenopausal women with hormone-receptor-positive, HER2-negative advanced breast cancer treated with ribociclib plus endocrine therapy: results from a phase III randomized clinical trial (MONALEESA-7). Ther Adv Med Oncol. 2020;12:1758835920943065. doi:10.1177/1758835920943065
21. Kaufman PA, Toi M, Neven P, et al. Health-related quality of life in MONARCH 2: abemaciclib plus fulvestrant in hormone receptor-positive, HER2-negative advanced breast cancer after endocrine therapy. Oncologist. 2020;25(2):e243–e251. doi:10.1634/theoncologist.2019-0551
22. Goetz MP, Martin M, Tokunaga E, et al. Health-related quality of life in MONARCH 3: abemaciclib plus an aromatase inhibitor as initial therapy in HR+, HER2- advanced breast cancer. Oncologist. 2020;25(9):e1346–e1354. doi:10.1634/theoncologist.2020-0084
23. Kappel C, Elliott M, Kumar V, et al. Comparative overall survival of patients in trials of CKD4/6 inhibitors in combination with endocrine therapy in advanced breast cancer. J Clin Oncol. 2023;41(16_suppl):1056. doi:10.1200/JCO.2023.41.16_suppl.1056
24. Zhao JJ, Fong KY, Chan YH, et al. Indirect treatment comparison of first-line CDK4/6-inhibitors in post-menopausal patients with HR+/HER2- metastatic breast cancer. J Clin Oncol. 2023;41(16_suppl):1071. doi:10.1200/JCO.2023.41.16_suppl.1071
25. Cejuela M, Gil-Torralvo A, Castilla MA, et al. Abemaciclib, palbociclib, and ribociclib in real-world data: a direct comparison of first-line treatment for endocrine-receptor-positive metastatic breast cancer. Int J mol Sci. 2023;25(1):24. doi:10.3390/ijms25010024
26. Kahraman S, Erul E, Seyyar M, et al. Treatment efficacy of ribociclib or palbociclib plus letrozole in hormone receptor-positive/HER2-negative metastatic breast cancer. Future Oncol. 2023;19(10):727–736. doi:10.2217/fon-2022-1287
27. Mastrantoni L, Orlandi A, Palazzo A, et al. The likelihood of being helped or harmed as a patient-centred tool to assess cyclin dependent kinase 4/6 inhibitors clinical impact and safety in metastatic breast cancer: a systematic review and sensitivity-analysis. EClinicalMedicine. 2023;56:101824. doi:10.1016/j.eclinm.2023.101824
28. Desnoyers A, Nadler MB, Kumar V, Amir E, Saleh R. Comparison of treatment-related adverse events of different cyclin-dependent kinase 4/6 inhibitors in metastatic breast cancer: a network meta-analysis. Cancer Treat Rev. 2020;90:102086. doi:10.1016/j.ctrv.2020.102086
29. Law E, Gavanji R, Walsh S, et al. Palbociclib versus abemaciclib in HR+/HER2- advanced breast cancer: an indirect comparison of patient-reported end points. J Comp Eff Res. 2022;11(2):109–120. doi:10.2217/cer-2021-0221
30. Burne R, Balu S, Guérin A, et al. Comparison of healthcare resource utilization and costs of patients with HR+/HER2- advanced breast cancer treated with ribociclib versus other CDK4/6 inhibitors. J Med Econ. 2021;24(1):806–815. doi:10.1080/13696998.2021.1939705
31. Freeman L, Kee A, Tian M, Mehta R. Evaluating treatment patterns, relapses, healthcare resource utilization, and costs associated with disease-modifying treatments for multiple sclerosis in DMT-naïve patients. Clinicoecon Outcomes Res. 2021;13:65–75. doi:10.2147/CEOR.S288296
32. Hughes DR, Espinoza W, Fein S, Rula EY, McGinty G. Patient cost-sharing and utilization of breast cancer diagnostic imaging by patients undergoing subsequent testing after a screening mammogram. JAMA Network Open. 2023;6(3):e234893–e234893. doi:10.1001/jamanetworkopen.2023.4893
33. Reyes C, Engel-Nitz NM, DaCosta Byfield S, et al. Cost of disease progression in patients with metastatic breast, lung, and colorectal cancer. Oncologist. 2019;24(9):1209–1218. doi:10.1634/theoncologist.2018-0018
34. Ryan CJ, Ke X, Lafeuille MH, et al. Management of patients with metastatic castration-sensitive prostate cancer in the real-world setting in the United States. J Urol. 2021;206(6):1420–1429. doi:10.1097/JU.0000000000002121
35. Goyal RK, Cuyun CG, Nagar SP, et al. Treatment patterns, adverse events, and direct and indirect economic burden in a privately insured population of patients with HR+/HER2- metastatic breast cancer in the United States. Expert Rev Pharmacoecon Outcomes Res. 2021;21(4):699–710. doi:10.1080/14737167.2020.1804871
36. Vera-Llonch M, Weycker D, Glass A, et al. Healthcare costs in women with metastatic breast cancer receiving chemotherapy as their principal treatment modality. BMC Cancer. 2011;11(1):250. doi:10.1186/1471-2407-11-250
37. NCI Comorbidity Index Overview. Available from: https://healthcaredelivery.cancer.gov/seermedicare/considerations/comorbidity.html.
38. Yabroff KR, Davis WW, Lamont EB, et al. Patient time costs associated with cancer care. J Natl Cancer Inst. 2007;99(1):14–23. doi:10.1093/jnci/djk001
39. Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20(4):461–494. doi:10.1016/S0167-6296(01)00086-8
40. Grinshpun A, Tolaney SM, Burstein HJ, Jeselsohn R, Mayer EL. The dilemma of selecting a first line CDK4/6 inhibitor for hormone receptor-positive/HER2-negative metastatic breast cancer. NPJ Breast Cancer. 2023;9(1):15. doi:10.1038/s41523-023-00520-7
41. Hui R, de Boer R, Lim E, Yeo B, Lynch J. CDK4/6 inhibitor plus endocrine therapy for hormone receptor-positive, HER2-negative metastatic breast cancer: the new standard of care. Asia Pac J Clin Oncol. 2021;17 Suppl 1(S1):3–14. doi:10.1111/ajco.13555
42. SEER*explorer: an interactive website for SEER cancer statistics [Internet]. Surveillance Research Program, National Cancer Institute; 2023. [updated: 2023 Jun 8; cited 2023 Aug 7]. Available from: https://seer.cancer.gov/statistics-network/explorer/. Data source(s): SEER Incidence Data, November 2022 Submission (1975-2020), SEER 22 registries.
43. Rugo HS, Layman RM, Lynce F, et al. Comparative overall survival of CDK4/6 inhibitors plus an aromatase inhibitor in HR+/HER2- metastatic breast cancer in the US real-world setting. ESMO Open. 2025;10(1):104103. doi:10.1016/j.esmoop.2024.104103
44. Zeichner SB, Herna S, Mani A, et al. Survival of patients with de-novo metastatic breast cancer: analysis of data from a large breast cancer-specific private practice, a university-based cancer center and review of the literature. Breast Cancer Res Treat. 2015;153(3):617–624. doi:10.1007/s10549-015-3564-3
45. Dai S, Yang M, Song J, Dai S, Wu J. Impacts of frailty on prognosis in lung cancer patients: a systematic review and meta-analysis. Front Med Lausanne. 2021;8:715513. doi:10.3389/fmed.2021.715513
46. Williams GR, Deal AM, Sanoff HK, et al. Frailty and health-related quality of life in older women with breast cancer. Support Care Cancer. 2019;27(7):2693–2698. doi:10.1007/s00520-018-4558-6
47. Tsai HH, Yu JC, Hsu HM, et al. The impact of frailty on breast cancer outcomes: evidence from analysis of the Nationwide Inpatient Sample, 2005-2018. Am J Cancer Res. 2022;12(12):5589–5598.
48. Petri H, Urquhart J. Channeling bias in the interpretation of drug effects. Stat Med. 1991;10(4):577–581. doi:10.1002/sim.4780100409
49. DeMichele A, Cristofanilli M, Brufsky A, et al. Comparative effectiveness of first-line palbociclib plus letrozole versus letrozole alone for HR+/HER2- metastatic breast cancer in US real-world clinical practice. Breast Cancer Res. 2021;23(1):37. doi:10.1186/s13058-021-01409-8
50. Ha MJ, Singareeka raghavendra A, Kettner NM, et al. Palbociclib plus endocrine therapy significantly enhances overall survival of HR +/ HER2 − metastatic breast cancer patients compared to endocrine therapy alone in the second-line setting: a large institutional study. Int J Cancer. 2022;150(12):2025–2037. doi:10.1002/ijc.33959
51. Rugo HS, Brufsky A, Liu X, et al. Real-world study of overall survival with palbociclib plus aromatase inhibitor in HR+/HER2- metastatic breast cancer. NPJ Breast Cancer. 2022;8(1):114. doi:10.1038/s41523-022-00479-x
52. Centers for Medicare & Medicaid Services. Medicare monthly enrollment. 2023. Available from: https://data.cms.gov/summary-statistics-on-beneficiary-enrollment/medicare-and-medicaid-reports/medicare-monthly-enrollment.
53. Jacobson G, Cicchiello A, Sutton JP, Shah A. Medicare advantage vs. traditional medicare: how do beneficiaries’ characteristics and experiences differ?: the commonwealth fund. 2021. Available from: https://www.commonwealthfund.org/publications/issue-briefs/2021/oct/medicare-advantage-vs-traditional-medicare-beneficiaries-differ.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.