Back to Journals » Patient Preference and Adherence » Volume 18
Imatinib Adherence and Persistence in Patients with Chronic Myeloid Leukemia in Belgium: Evidence from Real-World Data
Authors Michiels S , Tricas-Sauras S, Salaroli A, Bron D, Lewalle P, Vanschoenbeek K, Poirel HA, Kirakoya-Samadoulougou F
Received 7 April 2024
Accepted for publication 4 September 2024
Published 25 September 2024 Volume 2024:18 Pages 1991—2006
DOI https://doi.org/10.2147/PPA.S472478
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Sandra Michiels,1– 3 Sandra Tricas-Sauras,2 Adriano Salaroli,3 Dominique Bron,3 Philippe Lewalle,3 Katrijn Vanschoenbeek,4 Hélène A Poirel,4 Fati Kirakoya-Samadoulougou1
1Center for Research in Epidemiology, Biostatistics and Clinical Research, School of Public Health, Université Libre de Bruxelles, Brussels, Belgium; 2Center for Research in Social Approaches to Health, School of Public Health, Université Libre de Bruxelles, Brussels, Belgium; 3Department of Hematology/Oncology, Institut Jules Bordet, Hôpital Universitaire de Bruxelles, Université Libre de Bruxelles, Brussels, Belgium; 4Belgian Cancer Registry, Brussels, Belgium
Correspondence: Sandra Michiels, Email [email protected]; [email protected]
Purpose: Imatinib adherence and persistence are key components of the successful treatment of Chronic Myeloid Leukemia (CML). In Belgium, there is no study assessing these behaviors at a national level. Our study aimed to provide the first nationwide measure and to identify associated pharmacy-based predictors (age, gender, comorbidities). We also assessed mortality and transplantation incidence according to adherence status.
Methods: Based on medico-administrative database linkage, we identified a retrospective Belgian cohort of 1194 patients diagnosed with CML between 2004 and 2016 and treated with imatinib. Adherence was measured over 24 months, considering the proportion of days covered (PDC). Persistence was measured as the time until discontinuation (gap of ≥ 90 days). Multivariable Poisson regression models with robust standard error were conducted to identify predictors associated with adherence (≥ 90% PDC). To identify factors associated with persistence, a multivariable Cox regression was performed.
Results: At six months, 60.3% of patients were adherent, declining to 41.5% at 12 months, and to 30.1% at two-year follow-up (n=998). Adherence was greater at a younger age (eg 31– 40 years vs ≥ 75 years, adjusted prevalence ratio (aPR) 1.73; 95% confidence interval (CI): 1.09– 2.77) and among patients with no comorbidity (0 vs ≥ 2 comorbidities (aPR 1.56; 95% CI: 1.11– 2.19). The median persistence was 334.5 days (Q1:200–Q3:505.5); persistence at 24 months was 83.6% (n=998). Only age was associated with higher risk of discontinuation, with adjusted hazard ratio (aHR) of 6.05 for patients ≥ 75 years (95% CI: 5.52– 6.58). Transplants and deaths mainly occurred in patients defined as non-adherent at 24 months.
Conclusion: This Belgian nationwide representative study revealed a critical low level of imatinib adherence, which decreased over time even though persistence was high at six months. We pinpointed pharmacy-based predictors that were easily identifiable by health care stakeholders in order to undertake interventions to improve adherence.
Plain Language Summary: The introduction of imatinib, a new oral anticancer medication, has transformed chronic myeloid leukemia (CML) from a fatal disease to a chronic disease. However, the success of imatinib partly depends on how long a patient continues to take it (persistence) and the extent to which they take imatinib as prescribed (adherence). Over a 24-month follow-up period, this study aimed to provide an assessment of imatinib adherence and persistence for the first time and to identify associated risk factors. Using pharmacy dispensing data, our study revealed that whilst very few CML patients discontinued imatinib, a considerable proportion struggled to adhere to imatinib recommendations, with a decreasing rate of adherence and persistence over time. We have identified some demographic and clinical characteristics associated with higher risk of poor adherence and early discontinuation. The current study’s findings will help healthcare professionals to screen adherence behaviors prospectively and design specific interventions to maintain long-term optimal adherence to imatinib.
Keywords: adherence, persistence, imatinib, chronic myeloid leukemia, pharmacy refills data, Belgium
Introduction
Chronic myeloid leukemia (CML) is a myeloproliferative neoplasm accounting for around 15% of newly diagnosed adult leukaemia.1
Over the past 30 years, the incidence of CML has increased dramatically, reaching 1/100,000 in the global population in 2018.2 Simultaneously, innovative research and molecular biology have considerably increased survivorship by enabling the accelerating expansion of oral anticancer drugs.3
In 1998, the introduction of imatinib (Glivec®), the first tyrosine kinase BCR-ABL inhibitor (TKI), ushered in a new era of CML treatment, moving it from a fatal disease to a chronic condition.4 Only 10 years after its introduction, the five-year survival rate doubled from 33% to 70%;5 20 years later, the mortality rate dropped from 10–20% to 1–2%.6,7
Because of its high efficacy and low toxicity, imatinib has become the first-line standard treatment for CML patients. Oral therapy seems to be preferred by cancer patients due to convenience, ease of administration, outpatient use, and improved quality of life.8
In return, the time period over which a patient continues to take imatinib (persistence) and the extent to which they take imatinib as prescribed (adherence) control the success of the treatment. Poor adherence is associated with incomplete cytogenetic9 and molecular responses10 and with a suboptimal treatment response.11 Even more challenging, reducing the intake of imatinib from 100% to 90% of the prescribed dose reduces the likelihood of the various treatment responses by 2.35–1.95 times, indicating no margin for non-adherence.12
Published studies note that a substantial proportion of CML patients struggle to adhere to their medications as prescribed.13 Across studies, there is a wide range of adherence of CML patients, ranging from 20% to 53%12 and declining over time.13 Variables previously associated with (non)adherence are: longer time since diagnosis of CML or since start of imatinib,10,14 the wish to avoid side effects,15 multiple medications,16 demographic variable of living arrangement,10 social activities disturbing daily routines, and physician’s communication.17
In Belgium, around 160 patients are newly diagnosed with CML every year, with a median age of 64 and respective incidence of 1.5/100,000 for men and 1.2/100,000 for women.18 The five-year relative survival is very high in children and young adults, with more than 90% of positive outcomes, but drops after the age of 50 years in both sexes.18
So far, in Belgium, the extent to which CML patients adhere to and persist with imatinib has been ignored. Only one Belgian study in 2009 explored adherence in CML patients. The ADAGIO study10 was a 90-day prospective study demonstrating that non-adherence was more prevalent than patients, physicians, or family members believed and that there was a significantly higher mean percentage of imatinib not being taken in patients with a suboptimal response. Unfortunately, the ADAGIO study was conducted in a small sample of 169 CML patients and suffered from a severe lack of patient diversity, making it quite challenging to generalize the results to the wider Belgian population.
Using real-world data of pharmacy refills, our study aimed to assess imatinib adherence and persistence in CML patients over a 24-month follow-up (F/U) period and to identify pharmacy-based predictors of adherence and persistence. We also assessed mortality and transplantation incidences according to adherence status.
Material and Methods
Data Source
Pharmacy refill data were extracted from the Belgian Cancer Registry (BCR), a national organization collecting information about all new cancer diagnoses in Belgium and their F/U regarding vital status. The Inter-Mutualist Agency (IMA), which gathers the patient data of the seven Belgian mutual insurance companies, annually shares the health care claims data of cancer patients with the BCR.19 In Belgium, health insurance is mandatory, so 98% of residents are captured.20
The BCR captured 1) all diagnosed CML patients in Belgium between 2004 and 2016; 2) the surgical procedures and drugs delivered to these patients in Belgian hospitals and their pharmacies from one year before to five years after the CML incidence date; and 3) drugs delivered for the same period by Belgian community pharmacies.
We linked the three datasets to constitute a CML cohort with the following variables: gender, age at diagnosis, year of CML diagnosis, number of comorbidities, imatinib refills dates and corresponding supplied days, hematopoietic stem cell transplantation (HSCT) procedures, subsequent TKI first refill date and survival status.
Study Design and Sample Selection
In this retrospective study, we first identified 1876 patients diagnosed with CML between 1 January 2004 and 1 July 2016. The selected CML diagnoses were 9863/3 and 9875/3 according to the third edition of the International Classification of Diseases for Oncology (ICD-03). Children under 18 years of age were excluded (n=24). Among the 1852 remaining adults, we selected the 1237 new patients with at least one dose of imatinib dispensed and then kept only the 1194 with at least two consecutive imatinib deliveries to measure persistence. A total of 196 patients discontinued imatinib before the end of two years’ F/U and were excluded from the measure of adherence (Figure 1).
 |
Figure 1 Sample selection and patients’ attrition. |
Baseline Comorbidities
According to the rules established by the Belgian Cancer Registry and the Belgian Health Care Knowledge Centre (KCE),21,22 the number and types of baseline comorbidities were identified based on the medication used during the one year pre-imatinib initiation period.
Based on Anatomical Therapeutic Chemical (ATC) codes, we calculated the volume and frequency of relevant delivered drugs to identify three major comorbidities: chronic cardiovascular diseases, diabetes mellitus, and chronic respiratory diseases.
Chronic respiratory diseases include chronic obstructive pulmonary disease (COPD), asthma, pulmonary fibrosis, and diseases treated by drugs with ATC code R3 (drugs for obstructive airway diseases).
Chronic cardiovascular diseases refer to diseases treated with drugs with the following ATC codes: C01 (cardiac therapy), C02 (antihypertensives), C03 (diuretics), CO4 (peripheral vasodilators), C07 (beta blocking agents), C08 (calcium channel blockers), C09 (agents acting on the renin–angiotensin system), and B01 (antithrombotic agents, excluding B01 AB (heparin)).
Diabetes mellitus was captured based on consumption of drugs with ATC code A10, used in diabetes.
Previous tumor history, obtained from the BCR, was retained as a fourth comorbidity.
Outcome Measures
New taxonomy describing and defining adherence to medications distinguishes three elements in the process by which patients take their medication as prescribed: initiation, implementation, and discontinuation.23,24
Initiation begins when the first dose of the prescribed medication is taken. The process continues with implementation, defined as the extent to which a patient’s actual dosing corresponds to the prescribed dosing regimen from initiation to discontinuation. Discontinuation marks the end of therapy, when the next dose to be taken is omitted and no more doses are taken thereafter.23
Adherence
In the current study, we aimed to measure implementation (henceforth named adherence) of imatinib by calculating the proportion of days covered (PDC) over a fixed observation period of 24 months after initiation. As recommended by the International Society of Pharmacoeconomics and Outcomes Research, adherence should be measured by calculating the medication possession ratio25 (MPR) or the PDC. Since then, the PDC has been agreed to be more accurate than the MPR.26 Based on pharmacy refills, we used the PDC calculated as the number of days with drug on hand divided by the number of days in the specified time interval.25
In Belgium, every medicine and para-pharmaceutical package dispensed in a pharmacy has a unique identification number (CNK) providing information about the dosage and quantity of pills delivered. For each pharmacy refill we calculated the number of days supplied by dividing the total dosage delivered by the defined daily dose (DDD) for imatinib in chronic phase (CP) CML.
The DDD corresponds to the assumed average maintenance dose per day for a drug used for its main indication in adults and is recommended when the actual prescribed dose is not available.27 According to both the international treatment guidelines28 and the World Health Organization (WHO),24 the DDD for imatinib in CP CML is 400 mg once a day. Though CML is a triphasic disease, more than 95% of cases of CML are diagnosed in the chronic phase.29
Using SAS program, all imatinib refill dates and corresponding supplied days were transposed to a single observation per patient showing the medication fill pattern and supplied days of each fill. Next, using arrays and DO loops procedures, we found the days of medication coverage for each patient and calculated the proportion of covered days in the review period. Specifically, the PDC looks at each day in the interval to see if the patient had the prescribed imatinib on-hand. At last, we followed the method described by Leslie30 to account for early refill and adjust the overlapping days supplied by shifting the fill date forward to the day after the end of supply of the previous fill.31
Adherence was analyzed as both a continuous (mean PDC) and a binary outcome (optimal vs suboptimal adherence). Consistent with previous research demonstrating that 90% adherence to imatinib is needed to achieve a major molecular response,11,32,33 a threshold of 90% PDC was considered to designate optimal adherence.
Adherence was measured over time, at six months, one year, 18 months, and two years after imatinib initiation.
To clearly separate the assessment of adherence from that of persistence and avoid any ambiguity associated with a low adherence score, eligible patients for adherence measurement were alive and still covered by imatinib (persistent) at the end of the two-year F/U.34
Reason for missing dose was unknown. However, we know treatments interruptions attributed to hematologic intolerances result in interruptions of multiple consecutive days and mainly occurred in the first year, much less in the second year.35 We measured and compared over time the number of patients experiencing one or multiple episodes of interruptions lasting 30, 60, or 90 days.
Discontinuation and Persistence
Persistence was measured as the duration in days between imatinib initiation and discontinuation. We considered discontinuation to have occurred when a gap in the possession of imatinib of 90 days or longer was observed, with no further refills for imatinib during the remainder of the observation period.
The reason for discontinuation was unknown. However, as death may be a primary reason for treatment discontinuation, we first used a Cox proportional hazards model to account for death as a competing risk. Persistence was assessed by censoring the first occurrence of discontinuation, whether death or a 90-day gap in possession of imatinib. We assessed both the median time of persistence and the proportion of patients remaining on imatinib (“persistent”) during 6, 12, 18, and 24 months post-initiation.
We identified involuntary discontinuations corresponding to the patient’s date of death. Next, among alive discontinued patients and those experiencing discontinuation before death, we checked for subsequent TKI delivery (dasatinib, nilotinib or ponatinib) to assess voluntary discontinuations that may be refractory disease- or toxicity-related.
Other Outcomes
In a last set of outcomes, we assessed the incidence of HSCT and mortality over a five-year extended F/U. Based on the patient’s adherence status at 24 months, we compared the distribution of cases in both adherent and non-adherent groups.
Statistical Analysis
Descriptive statistics were performed using means and standard deviations (SD) for continuous variables and percentages for categorical variables. Statistical t-tests and Kruskal–Wallis tests were conducted to examine differences in adherence and persistence, respectively, among the selected characteristics (gender, age, total number of individual comorbidities).
Multivariable Poisson regression with robust standard error and Cox proportional hazards models were conducted to identify predictors associated with adherence (≥90% PDC); estimates are presented as adjusted prevalence ratios (aPR) and adjusted hazard ratios (aHR) with 95% confidence intervals (95% CI).
All statistical analyses were conducted using SAS Enterprise Guide version 7.1.
Sensitivity Analysis
Several sensitivity analyses were performed for both primary outcomes. Firstly, we compared two periods of diagnosis (2004–2009 vs 2010–2016) corresponding to before and after the introduction in Belgium of second-generation (2nd) TKIs. It is safe to assume that since a switch to 2nd generation TKI has been recommended in case of imatinib intolerance, the found missed doses linked to treatment interruptions and consequently, the calculated adherence rates, should be lower.
Then, for adherence, we conducted different analyses defining optimal adherence as 80–85% PDC. For persistence, we repeated our analysis to limit the assessment of discontinuation to patients not persistent for a reason other than death. We also conducted analysis considering a 30- or 60-day gap for discontinuation definition.
Results
Study Population
Overall, most patients (70%) were aged over 50 years, more than half were male, and more than half of patients were diagnosed after 2009 (Table 1).
 |
Table 1 Characteristics of Patients Treated by Imatinib for Chronic Myeloïd Leukemia (CML), Belgium, 2004–2016 |
Half of the patients have no comorbidity, more than 30% have one, and 18% have at least two comorbidities. Chronic cardiovascular diseases were the most frequent comorbidity. Imatinib was by far the TKI most frequently delivered (95.4%) as the first-line treatment, followed by nilotinib (2.8%) and dasatinib (1.8%).
Adherence
Mean PDC was 0.87 (SD 0.16) in the first six months and decreased over time, falling to 0.80 after one year, to 0.76 after 18 months, and to 0.72 when measured after two years (Supplementary Table S1).
Globally, the proportion of patients with optimal adherence was fairly low. Optimal adherence was seen in 60.3% of patients within the first six months after initiation. This proportion dropped sharply, by 19%, in the next six months to achieve 41.5% at one year, and then gradually declined to 35.2% after 18 months and 30.1% after 24 months (Supplementary Figure S1).
Being younger than 75 years and not having any comorbidity is associated with higher adherence. Compared to the group aged ≥75 years, adherent proportion was 1.87 times higher in the group aged 51–64 and 1.73 times higher in the group aged 31–40 (P<0.01). The proportion of adherent patients was higher among patients without comorbidities (aPR 1.56, 95% CI: 1.11–2.19) and those with one comorbidity (aPR 1.36, 95% CI: 0.97–1.96) compared to patients with at least two comorbidities (Table 2).
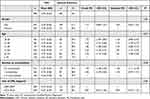 |
Table 2 Demographic and Clinical Characteristics Associated with Two Years Optimal Adherence (PDC ≥ 90%) to Imatinib in CML, Belgium, 2004–2016 |
Discontinuation and Persistence
The proportion of patients persistent within the first 6 months was high (96.7%) and decreased slightly to achieve 91.4% at 1 year, 86.6% at 18 months and 83.6% at 2 years (Table 3).
 |
Table 3 Proportion of CML Patients Persistent to Imatinib, Belgium, 2004–2016 |
Within two years, 196 patients (17.4%) experienced discontinuation, with a median time of 334.5 days [Q1:200–Q3:505.5] (Figure 2).
Among them, 111 patients (9.3%) died before the end of the study period F/U. We found that about 99 deaths occurred while the patient was still covered by imatinib, ie half of all discontinuations are involuntary and explained by death. On the other hand, 12 patients died after having experienced a 90-days gap discontinuation.
In all, 97 discontinuations were voluntary. Of these, only a quarter of patients (n=26) have been delivered with subsequent second or third-generation TKI. The median time between imatinib discontinuation and subsequent TKI delivery was 312.5 days [range: 22–2539]. Only a quarter had a delivery less than 100 days after imatinib discontinuation. This suggests that the vast majority of voluntary discontinuations – 4.5% of sample – cannot be explained by a treatment switch.
The Cox proportional hazard model did not confirm any statistical association between discontinuation and gender, individual number of comorbidities, or year of diagnosis but identified older age as a predictor associated with non-persistence. Compared to the group aged 18–30 years, the risk of non-persistence was considerably higher in the group aged 75 and older (aHR 6.05, 95% CI (5.52–6.58), P<0.0001) (Table 4).
 |
Table 4 Demographic and Clinical Characteristics Associated with Non Persistence to Imatinib in CML Patients, Belgium, 2004–2016 |
Other Outcomes
Of the 998 patients eligible for the measure of two-year F/U adherence, 19 (1.9%) received an HSCT within five years of the initiation of imatinib. The median time to HSCT was 25 months [range: 6.3–58.63]. In total, 15 (1.6%) patients had a transplant within three years, 16 (1.9%) within four years and 19 (2.2%) within five years. Before transplantation, the large majority of patients (84.2%) were treated by one (57.9%) or at least two (26.3%) subsequent TKIs.
A comparison of HSCT distribution showed that transplants mainly occurred in patients defined as suboptimally adherent at 24 months (100% of HSCT performed within three years’ F/U and 89% of those performed within five years’ F/U). Similarly, we found that the large majority of deaths concerned non-adherent patients: 76.7% of deaths (n=23) at three years F/U, 77.2% (n=44) at four years, and 72.9% (n=35) at five years (Figure 3).
The comparison of the 30-, 60- or 90-consecutive day’s interruptions showed that shorter is the interruption, higher is the proportion of the 1194 experiencing it (Supplementary Figure S2). After one year, respectively, 250 (20.9%) and 41 (3.4%) patients experienced one interruption of 30-days and 90-days. Most patients experienced only one episode of interruption within two years, but whatever the interruption length, the repetition of episodes increased over time. On average, the number of episodes lasting 30 days was similar in the two diagnosis periods of 2004–2009 and 2010–2016.
Sensitive Analyses
The comparison of the two periods of diagnosis did not show any statistically significant difference between PDC rates. The PDC was not lower for the period 2004–2009 (77%) but higher than for the period 2010–2016 (67%) (Table 2).
The sensitive analyses considering a lower threshold of 85% or 80% to define optimal adherence showed a similar decrease over time in the proportion of patients with optimal adherence. Albeit necessarily higher (69.9% and 78.4%, respectively, at six months), these proportions drop over time to 47.3% and 58.4% at two years (Supplementary Figure S1).
All analyses comparing age groups and total number of comorbidities were consistent with our main analysis. The proportion of patients showing optimal adherence (PDC≥85%) was 2.05 times higher in the group aged 51–64 and 1.89 times higher in the group aged 31–40 (P<0.001), and higher in the group with no comorbidities (aPR 1.27, 95% CI (1.02–1.60)) (Supplementary Table S2). A similar significant association with age was observed with a threshold of 80%, but not with comorbidity status (Supplementary Table S3).
Concerning persistence, while limiting the measure of non-persistence to patients who discontinued imatinib for a reason other than death, we found a higher rate of persistent patients (99.2% at six months F/U), also decreasing over time (91.9% at two years F/U) (Supplementary Table S4). Similar to our main analysis including death as a competing risk, the Cox regression model confirmed in this population a higher risk of imatinib discontinuation (≥90-day gap in possession) in patients older than 75 years (aHR 6.80, 95% CI (6.05–7.55), P<0.001) (Supplementary Table S5).
All analyses using 30- and 60-day gap definitions for discontinuation confirmed the much lower proportions of persistent patients over time. Consistently, the Cox regression model assessing predicting factors confirmed a higher risk of discontinuation in patients older than 75 years (Supplementary Table S6 and S7).
Discussion
Adherence to treatment and persistence are key factors of treatment success. However, the current study has revealed that a critical proportion of CML patients in Belgium have not adhered to imatinib recommendations, with a decreasing rate of adherence and persistence over time.
Using real-world data on pharmacy refills, we were able to identify demographic and comorbidity status predictive of poor adherence and persistence.
Our findings concerning imatinib adherence rates are supported by those of another claim-based study using the same adherence definition over the same follow-up period, which found 44% of adherent patients after one year and 38% after two years.36 Studies reporting higher proportions of adherent patients have used a lower threshold of 80%37–39 or 85%40–42 to categorize adherence, as we found in our sensitive analyses. It is worth noting that a lower threshold necessarily results in a higher proportion of adherent patients.43 Since the threshold used should be the lowest level at which the desired therapeutic effect is maintained,44 a minimum threshold of 90% should be used for imatinib in CML.11,32
The length of the observation period is equally important to consider. As adherence to long-term oral therapy declines over time,45–47 a shorter observation period may overestimate adherence to treatment. Prospective studies able to provide more comprehensive clinical data and to explore the reasons for non-adherence cannot, in contrast, afford to monitor adherence over a long period48 and may therefore provide higher rates of adherence. Based on 3 months pills count, the previous Belgian ADAGIO study10 found 90.9% of adherence. By assessing adherence over for distinct F/U period, our study showed that adherence drops off as early as 6 months and continues to decline for up to two years.
The above adherence rates calculated from the PDC and a DDD of 400mg were put into perspective with the rest of the data and the context to check their reliability. First, in CML, according to international guidelines, it was not recommended to increase the dosage of imatinib to 600 or 800 mg outside of clinical studies whose patients are not included in our cohort.49 On the other hand, toxicity-related dose reduction only concerns a very small proportion of patients29 and has certainly been further limited by the arrival of second generation TKIs.49 Since then, in case of imatinib intolerance, suboptimal response or failure, a switch to dasatinib or nilotinib was recommended.
The comparison of the PDC between these two periods did not show any statistical difference in the number of days not covered by imatinib. Moreover, the diagnosis period of 2010–2016 showed more days of interruptions. The assessment of episodes of 30-days interruption showed that the number of patients experiencing one unique episode stabilized within the first year F/U. They may therefore correspond to toxicity-related treatment interruptions. One single episode of 30 days kept, however, the patient in the category defined as optimally adherent (PDC ≥90%). In contrast, the patients multiplying the episodes increased over time and are more inconsistent with drug-related toxicity.
It is therefore reasonable to consider that high rates of non-adherence found in the following study were not biased by toxicity-related treatment interruptions.
Among baseline characteristics, our study, in accordance with the previous small-scale Belgian ADAGIO study,10 did not identify gender as a predictor for poor adherence.
In turn, we found a significant association between adherence and age. Age has often been identified as a risk factor associated with poor adherence, but, rather inconsistently, sometimes in relation to younger age9 and sometimes older age.42,50 The current study showed that patients aged over 75 years are less likely to be adherent compared to the younger 31–40 or 51–64 age groups. However, it should be noted that the 18–30 group was also found to be struggling with imatinib adherence regardless of the threshold of 80%, 85%, or 90% PDC used to define optimal adherence.
It is all the more striking that current evidence suggests that the biology of CML is not affected by the patient’s age and that older individuals may benefit from TKI treatment to the same extent as younger patients.51 In the case of TKI failure or resistance, HSCT is currently the only cure for CML. Unfortunately, transplant is not always an available option, considering older age or comorbidity. In any case, HSCT is a costly and risky procedure with a high mortality rate and lifelong complications. This should justify all efforts to improve high adherence regardless of age category.
Our results regarding the distribution of HSCT events support this view. Though HSCT indications and causes of death were unknown, we observed that the majority of these events concerned patients with suboptimal adherence (PDC<90%) at two years. These results are consistent with those of other retrospective studies showing a higher risk of treatment failure and mortality in patients with suboptimal adherence.10,11,52
If improving high adherence should be a priority regardless of age, the type of intervention required to achieve it will necessarily vary. Although the main reasons for non-adherence reported by young adults and the elderly are partly comparable,53 their reality differs and may affect adherence behaviors differently. Elderly patients are more prone to multimorbidity and therefore complex regimens with multiple prescribing physicians, but also to cognitive impairment or difficulty with drug storage and formulation, which are all additional factors associated with poor adherence.54 Young adults (18–30 years) are most concerned about entering university or the job market and about starting a family. Generally, they are less able to recognize or more unwilling to consider the long-term implications of optimal adherence though, conversely, they feel directly impacted by the adverse effect of treatment that may negatively affect their social and active life.
Alongside age, our study revealed that having one or two comorbidities was a predictive factor of lower adherence. Supporting this, patients receiving multiple medications for coexisting conditions have been demonstrated less adherent to anticancer medications13,55–58 First of all, increasing the number of dose to be taken simply increases the risk of forgetfulness.59 Next, the size and number of pills may increase discomfort and make it difficult to swallow. Some patients may also choose to receive less effective anticancer treatment because they fear potential interactions and side-effects.55 However, many other factors are involved and comorbidities-related medications do not justify the barriers in adherence alone. Non-adherence may be increased due to physical impairments, a daily routine complexified by multiple foreign caregivers for chronic conditions, but also, patients with multiple chronic conditions may have a different perspective on health outcomes such as longer survival, prevention of disease-specific events, or tolerable risks of adverse drug reactions.60
The current study assessing persistence revealed that around 17% of patients discontinue imatinib within two years. Our results are quite similar to what Klil-Drori et al61 observed when they reported that 88.2% of CML patients remained persistent at three years F/U, though they used a 45-day gap definition. However, our sensitive analysis using a 60- and 30-day gap found yet lower proportions (82.3% and 56.6%, respectively) of still persistent patients at two years F/U, which is closer to what M. Pajiep and colleagues observed in France in their population-based study.62
The number of consecutive imatinib-free days varies across studies from 3063 to 45,61 60,41,64 or 90 days64 and cross-validation is made difficult. However, we think there is a risk in choosing a too short timeframe for the definition of discontinuation. When we compared the number of 30-, 60-, or 90-day gaps, we illustrated how the shorter the gap, the higher the number and the more frequent the episodes. After initiation, imatinib may have to be temporarily suspended until side effects or toxicities disappear. By choosing too short a duration, there is a risk of excluding several discontinued patients from the adherence measure and therefore confusing non-adherence behaviors with non-persistence. This is all the more essential as reasons for these two behaviors differ and they require different interventions.
We found that half of non-persistence concerned involuntary discontinuation due to the patient’s death and the other half concerned voluntary discontinuation. Patients who discontinue treatment due to death may have substantially different profiles, including more severe disease or more comorbid conditions than those who intentionally discontinue treatment (eg treatment failure or switch).53 This is 4.5% of patients discontinuing before 2 years who will not reach deep molecular response required to allow treatment discontinuation and potentially a treatment-free remission status.65
The analysis of predictive variables revealed no significant association other than age. Patients ≥75 years old had a higher risk of discontinuation. Using a competing risk approach for death, higher estimates may be expected on the assumption that non-persistence was predominantly driven by patient deaths. However, our sensitive analysis showed that the statistical association between age ≥75 and intentional discontinuation remained. Multiple explanations are possible. Due to increased fragility of older patients, discontinuation may be a medical decision related to drug toxicity. It is also possible, however, that older patients’ perspectives on the quality and length of life in case of adverse effects affect their continuation of imatinib.66
CML is most frequently diagnosed among people aged 65–74, and approximately half of newly diagnosed patients are 65 years or older. The changing demographic may contribute to an increasing number of patients over 65 years with cancer diagnoses.67 The higher prevalence of comorbidity in this population68 exacerbates their risk of non-adherence.
The results of the current study demonstrate that, in Belgium, although imatinib is reimbursed for CML treatment, a very large proportion of patients still do not adhere to their treatment. This argues for urgent prospective interventions to screen and improve CML patients’ adherence. Interventions are diverse and should be specific to patients’ difficulties. It is important to remember that patients might not be adequately informed or knowledgeable about their therapeutic regimen. As they may change their dosages according to their comprehension, it is critical to ensure that they are aware of the importance of taking their medications exactly as directed.69
Older patients tend to have more regular contact with their doctor. Patients with multiple comorbidities and cognitive impairment54 may therefore benefit from medication reviews aimed at simplifying regimens and educating patients about their treatment. Younger individuals, generally more likely to consult the internet to understand their condition and medications, need more time with the healthcare professional to discuss their condition fully and be convinced of the benefits of adhering to their regimen. For the long term, it may be necessary to support motivation, possibly through digital channels.
New treatment guidelines provide hope for treatment discontinuation and treatment-free remission but deep molecular response must be maintained during at least 5 years.70 However, not all patients will be eligible,71 and the others will have to maintain a deep molecular response for 5 years. Imatinib therefore remains a long-term or lifelong treatment for which optimal adherence (PDC ≥90%) should be ensured.
Strengths and Limitations
This study provides the first nationwide Belgian retrospective measure of imatinib adherence and persistence in adult patients with CML. Based on pharmacy refill data and calculated for the whole CML patient population treated in Belgium between 2004 and 2018, our study provides strong objective results that are reliably transposable and relevant for the international context.
By measuring outcomes at four time points over a longer two-year observation period, we were able to disclose the changing nature of adherence behaviors. To date, there is still no gold standard for measuring adherence to treatment.72 Each method has advantages and disadvantages. The results of the current study must be interpreted in the context of the strengths and limitations of the method used.
First, pharmacy dispensing does not necessarily mean that the patient has consumed the medication or taken it as prescribed. However, if the PDC cannot claim to measure the uptake of medication itself, on the other hand, it does identify with certainty the days on which the patient had no medication available, which necessarily says something about non-adherence. The limitation of this method is therefore not to underestimate but to overestimate adherence. Considering the low proportion of patient found being optimally adherent (PDC≥90%) within 12 (41.5%) or 24 (30.1%) months, the risk would be to have still overestimated adherence rates.
Secondly, while non-adherence can manifest in various ways within implementation phase, the PDC only provide an aggregate summary of imatinib availability and is unable to differentiate between a patient who was poorly adherent because he skipped imatinib every other day or one who was fully adherent for one month before interrupting treatment for two weeks. Additional approaches such as group-based trajectory models are therefore warranted to identify the heterogeneity of poor adherence behaviors and related associated factors.
Thirdly, our observation was limited to two a 2 years F/U period. According to new CML treatment guidelines, it would be beneficial to extend the F/U period to 5 years.
Finally, medication adherence is a complex and dynamic behavior influenced by multiple interacting factors. Administrative data are collected for financial and administrative rather than research purposes. As such, they do not provide insights into clinical variables such as reasons for interruptions, treatment-related toxicities or adverse effects, or several other personal and contextual reasons for nonadherence. Regarding patient demographic factors, our study was restricted by the limited available data, so multiple unobserved confounders may remain, such as living arrangement, migration background, or educational level.
Conclusion
Based on real-world pharmacy refill data, our study provides the first nationwide measures of adherence to and persistence with imatinib. Our findings revealed that a considerable proportion of CML patients struggle to adhere to imatinib recommendations, with a decreasing rate of adherence and persistence over time.
The proportion of optimal adherence at two years F/U was low, with a higher risk of poor adherence in patients older than 75 years and those with one or two comorbidities. The proportion of discontinued patients was significantly higher among the elderly.
Our study results argue for prospective screening whatever patients’ age but suggest specific population interventions. Further research describing different types of poor adherence/persistence and reasons for it is warranted to improve the efficacy of interventions and guarantee the efficacy of treatment.
Abbreviations
aHR, Adjusted hazard ratio; aPR, Adjusted prevalence ratio; ATC, Anatomical therapeutic chemical; BCR, Belgian Cancer Registry; CML, Chronic myeloid leukemia; COPD, Chronic obstructive pulmonary disease; CP, Chronic phase; DDD, Defined daily dose; F/U, Follow-up; HR, Hazard ratio; HSCT, Hematopoietic stem cell transplantation; ICD-03, International Classification of Diseases for Oncology, Third Edition; KCE, Belgian Health Care Knowledge Centre; MPR, Medication possession ratio; PDC, Proportion of days covered; PR, Prevalence ratio; SD, Standard deviation; SE, Standard error; TKI, Tyrosine kinase BCR-ABL inhibitor; WHO, World Health Organization.
Ethics Statement
The current study was the subject of an agreement between the Belgian Cancer Registry and the Université Libre de Bruxelles (ULB), all parties expressly undertaking to comply with the conditions of the law of 30 July 2018 on the protection of individuals with regard to the processing of personal data, as well as the General Data Protection Regulation EU 2016/679.
Acknowledgments
We thank Geert Silversmith from the Belgian Cancer Registry and Nicolas Dubois for providing precious help regarding data management issues.
Funding
This work was supported by the Association Jules Bordet, the Centre for Research in Epidemiology, Biostatistics, and Clinical Research of the School of Public Health (Université Libre de Bruxelles).
Disclosure
The authors have no conflicts of interest in this work.
References
1. O’Brien S, Berman E, Borghaei H, et al. NCCN clinical practice guidelines in oncology: chronic myelogenous leukemia. J Natl Compr Cancer Netw JNCCN. 2009;7(9):984–1023. doi:10.6004/jnccn.2009.0065
2. Hu Y, Li Q, Hou M, Peng J, Yang X, Xu S. Magnitude and Temporal Trend of the Chronic Myeloid Leukemia: on the Basis of the Global Burden of Disease Study 2019. JCO Glob Oncol. 2021;7:1429–1441. doi:10.1200/GO.21.00194
3. Weingart SN, Brown E, Bach PB, et al. NCCN Task Force Report: oral chemotherapy. J Natl Compr Cancer Netw JNCCN. 2008;6(3):S1–14.
4. Apperley JF. Chronic myeloid leukaemia. Lancet Lond Engl. 2015;385(9976):1447–1459. doi:10.1016/S0140-6736(13)62120-0
5. National Cancer Institute. Chronic Myeloid Leukemia - Cancer Stat Facts. SEER. https://seer.cancer.gov/statfacts/html/cmyl.html.
6. Jabbour E, Kantarjian H. Chronic myeloid leukemia: 2018 update on diagnosis, therapy and monitoring. Am J Hematol. 2018;93(3):442–459. doi:10.1002/ajh.25011
7. American Cancer Society. Cancer Facts & Figures 2019. CA:A Canc J Clini. 2023.
8. Ciruelos EM, Díaz MN, Isla MD, et al. Patient preference for oral chemotherapy in the treatment of metastatic breast and lung cancer. Eur J Cancer Care. 2019;28(6):e13164. doi:10.1111/ecc.13164
9. Marin D, Bazeos A, Mahon FX, et al. Adherence is the critical factor for achieving molecular responses in patients with chronic myeloid leukemia who achieve complete cytogenetic responses on imatinib. J Am Soc Clin Oncol. 2010;28(14):2381–2388. doi:10.1200/JCO.2009.26.3087
10. Noens L, van Lierde MA, De Bock R, et al. Prevalence, determinants, and outcomes of nonadherence to imatinib therapy in patients with chronic myeloid leukemia: the ADAGIO study. Blood. 2009;113(22):5401–5411. doi:10.1182/blood-2008-12-196543
11. Obeng-Kusi M, MacDonald K, van Lierde MA, Lee CS, De Geest S, Abraham I. No margin for non-adherence: probabilistic Kaplan-Meier modeling of imatinib non-adherence and treatment response in CML (ADAGIO study). Leuk Res. 2021;111:106734. doi:10.1016/j.leukres.2021.106734
12. Greer JA, Amoyal N, Nisotel L, et al. A Systematic Review of Adherence to Oral Antineoplastic Therapies. oncologist. 2016;21(3):354–376. doi:10.1634/theoncologist.2015-0405
13. Hall AE, Paul C, Bryant J, et al. To adhere or not to adhere: rates and reasons of medication adherence in hematological cancer patients. Crit Rev Oncol Hematol. 2016;97:247–262. doi:10.1016/j.critrevonc.2015.08.025
14. Hochhaus A, Baccarani M, Silver RT, et al. European LeukemiaNet 2020 recommendations for treating chronic myeloid leukemia. Leukemia. 2020;34(4):966–984. doi:10.1038/s41375-020-0776-2
15. Pandey D, Chugh P, Chaudhry S. Non-adherence to Imatinib despite availability: analysis from a resource limited setting. Authorea Preprin. doi:10.22541/au.171834908.81536930/v1
16. Gugliotta G, Castagnetti F, Fogli M, Cavo M, Baccarani M, Rosti G. Impact of comorbidities on the treatment of chronic myeloid leukemia with tyrosine-kinase inhibitors. Expert Rev Hematol. 2013;6(5):563–574. doi:10.1586/17474086.2013.837279
17. Geissler J, Sharf G, Bombaci F, et al. Factors influencing adherence in CML and ways to improvement: results of a patient-driven survey of 2546 patients in 63 countries. J Cancer Res Clin Oncol. 2017;143(7):1167–1176. doi:10.1007/s00432-017-2372-z
18. Tambuyzer T, Henau K, Van Gool B, et al. Haematological malignancies in Belgium 2004-2018. Belgian Cancer Registry. 2021.
19. de Santé D. IMA-AIM Agence Intermutualiste.
20. KCE. Financial accessibililty. For a Healthy Belgium.
21. Jegou D, Dubois C, Schillemans V, et al. Use of health insurance data to identify and quantify the prevalence of main comorbidities in lung cancer patients. Lung Cancer. 2018;125:238–244. doi:10.1016/j.lungcan.2018.10.002
22. Vrijens F Quality indicators for the management of lung cancer; 2016.
23. Vrijens B, De Geest S, Hughes DA, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705. doi:10.1111/j.1365-2125.2012.04167.x
24. De Geest S, Zullig LL, Dunbar-Jacob J, et al. ESPACOMP Medication Adherence Reporting Guideline (EMERGE). Ann Intern Med. 2018;169(1):30. doi:10.7326/M18-0543
25. Steiner JF, Prochazka AV. The assessment of refill compliance using pharmacy records. Methods, validation, and applications. J Clin Epidemiol. 1997;105–106.
26. Forbes CA, Deshpande S, Sorio-Vilela F, et al. A systematic literature review comparing methods for the measurement of patient persistence and adherence. Curr Med Res Opin. 2018;34(9):1613–1625. doi:10.1080/03007995.2018.1477747
27. 2023_guidelines_web.pdf. https://www.whocc.no/filearchive/publications/2023_guidelines_web.pdf.
28. Benghiat FS, Beguin Y, Dessars B, et al. Practical management of chronic myeloid leukaemia in Belgium. Belg J Hematol. 2015;6(1):16–32.
29. Geelen IGP, Thielen N, Janssen JJWM, et al. Treatment outcome in a population-based, “real-world” cohort of patients with chronic myeloid leukemia. Haematologica. 2017;102(11):1842–1849. doi:10.3324/haematol.2017.174953
30. Leslie SR, Gwadry-Sridhar F, Thiebaud P, Patel BV. Calculating medication compliance, adherence and persistence in administrative pharmacy claims databases. Pharm Program. 2008;1(1):13.
31. Traubenberg S, Zhongwen H, Wang S Measuring Medication Adherence with Simple Drug Use and Medication Switching. SAS Global Forum 2013. Pharma and Health Care. https://support.sas.com/resources/papers/proceedings13/168-2013.pdf.
32. Santoleri F, Ranucci E, Barba GL, et al. Adherence, persistence and efficacy of dasatinib and nilotinib in the treatment of patients resistant or intolerant to imatinib with chronic myeloid leukemia in chronic phase: an Italian multicenter study over two years in real life. Curr Med Res Opin. 2021. doi:10.1080/03007995.2021.1876006
33. Horizons-Hemato-Mars-2015-35-36-Charbonnier.pdf.
34. DeClercq J, Choi L. Statistical considerations for medication adherence research. Curr Med Res Opin. 2020;36(9):1549–1557. doi:10.1080/03007995.2020.1793312
35. Hehlmann R, Cortes JE, Zyczynski T, et al. Tyrosine kinase inhibitor interruptions, discontinuations and switching in patients with chronic‐phase chronic myeloid leukemia in routine clinical practice: SIMPLICITY. Am J Hematol. 2019;94(1):46–54. doi:10.1002/ajh.25306
36. Halpern R, Barghout V, Williams D. Compliance with Imatinib Mesylate Associated with Lower Health Resource Utilization and Costs for Patients with CML and GIST. Blood. 2007;110(11):5159. doi:10.1182/blood.V110.11.5159.5159
37. Winn AN, Keating NL, Dusetzina SB. Factors Associated With Tyrosine Kinase Inhibitor Initiation and Adherence Among Medicare Beneficiaries With Chronic Myeloid Leukemia. J Clin Oncol. 2016;34(36):4323–4328. doi:10.1200/JCO.2016.67.4184
38. Shen C, Zhao B, Liu L, Shih YCT. Adherence to tyrosine kinase inhibitors among Medicare Part D beneficiaries with chronic myeloid leukemia. Cancer. 2018;124(2):364–373. doi:10.1002/cncr.31050
39. Doshi JA, Jahnke J, Raman S, et al. Treatment utilization patterns of newly initiated oral anticancer agents in a national sample of Medicare beneficiaries. J Manag Care Spec Pharm. 2021;27(10):1457–1468. doi:10.18553/jmcp.2021.27.10.1457
40. Ward MA, Fang G, Richards KL, et al. Comparative evaluation of patients newly initiating first-generation versus second-generation tyrosine kinase inhibitors for chronic myeloid leukemia and medication adherence, health services utilization, and healthcare costs. Curr Med Res Opin. 2015;31(2):289–297. doi:10.1185/03007995.2014.991440
41. Trivedi D, Landsman-Blumberg P, Darkow T, Smith D, McMorrow D, Mullins CD. Adherence and persistence among chronic myeloid leukemia patients during second-line tyrosine kinase inhibitor treatment. J Manag Care Spec Pharm. 2014;20(10):1006–1015. doi:10.18553/jmcp.2014.20.10.1006
42. Charles M, Bollu V, Hornyak E, Coombs J, Blanchette C, DeAngelo D. Predictors of Treatment Non-Adherence in Patients Treated with Imatinib Mesylate for Chronic Myeloid Leukemia. Blood. 2009;114. doi:10.1182/blood.V114.22.2209.2209
43. Efficace F, Baccarani M, Rosti G, et al. Investigating factors associated with adherence behaviour in patients with chronic myeloid leukemia: an observational patient-centered outcome study. Br J Cancer. 2012;107(6):904–909. doi:10.1038/bjc.2012.348
44. Stauffer ME, Hutson P, Kaufman AS, Morrison A. The Adherence Rate Threshold is Drug Specific. Drugs RD. 2017;17(4):645–653. doi:10.1007/s40268-017-0216-6
45. Makubate B, Donnan PT, Dewar JA, Thompson AM, McCowan C. Cohort study of adherence to adjuvant endocrine therapy, breast cancer recurrence and mortality. Br J Cancer. 2013;108(7):1515–1524. doi:10.1038/bjc.2013.116
46. Weaver KE, Camacho F, Hwang W, Anderson R, Kimmick G. Adherence to adjuvant hormonal therapy and its relationship to breast cancer recurrence and survival among low-income women. Am J Clin Oncol. 2013;36(2):181–187. doi:10.1097/COC.0b013e3182436ec1
47. Lee HS, Lee JY, Ah YM, et al. Low adherence to upfront and extended adjuvant letrozole therapy among early breast cancer patients in a clinical practice setting. Oncology. 2014;86(5–6):340–349. doi:10.1159/000360702
48. Shah KK, Touchette DR, Marrs JC. Research and scholarly methods: measuring medication adherence. JACCP J Am Coll Clin Pharm. 2023;6(4):416–426. doi:10.1002/jac5.1771
49. Baccarani M, Cortes J, Pane F, et al. Chronic myeloid leukemia: an update of concepts and management recommendations of European LeukemiaNet. J Clin Oncol off. 2009;27(35):6041–6051. doi:10.1200/JCO.2009.25.0779
50. Larizza MA, Dooley MJ, Stewart K, Kong DC. Factors Influencing Adherence to Molecular Therapies in Haematology-Oncology Outpatients. J Pharm Pract Res. 2006;36(2):115–118. doi:10.1002/j.2055-2335.2006.tb00584.x
51. Balducci L, Dolan D. Chronic Myelogenous Leukemia (CML) in the elderly. Mediterr J Hematol Infect Dis. 2014;6(1):e2014037. doi:10.4084/MJHID.2014.037
52. Ganesan P, Sagar TG, Dubashi B, et al. Nonadherence to Imatinib adversely affects event free survival in chronic phase chronic myeloid leukemia. Am J Hematol. 2011;86(6):471–474. doi:10.1002/ajh.22019
53. Ge L, Heng BH, Yap CW. Understanding reasons and determinants of medication non-adherence in community-dwelling adults: a cross-sectional study comparing young and older age groups. BMC Health Serv Res. 2023;23:905. doi:10.1186/s12913-023-09904-8
54. Smaje A, Weston-Clark M, Raj R, Orlu M, Davis D, Rawle M. Factors associated with medication adherence in older patients: a systematic review. Aging Med Milton NSW. 2018;1(3):254–266. doi:10.1002/agm2.12045
55. Kemp A, Preen DB, Saunders C, et al. Early discontinuation of endocrine therapy for breast cancer: who is at risk in clinical practice? SpringerPlus. 2014;3(1):282. doi:10.1186/2193-1801-3-282
56. Sarfati D, Hill S, Blakely T, et al. The effect of comorbidity on the use of adjuvant chemotherapy and survival from colon cancer: a retrospective cohort study. BMC Cancer. 2009;9(1):116. doi:10.1186/1471-2407-9-116
57. Drzayich Antol D, Waldman Casebeer A, Khoury R, et al. The relationship between comorbidity medication adherence and health related quality of life among patients with cancer. J Patient-Rep Outcomes. 2018;2(1):29. doi:10.1186/s41687-018-0057-2
58. Mulu Fentie A, Tadesse F, Engidawork E, Gebremedhin A. Prevalence and determinants of non-adherence to Imatinib in the first 3-months treatment among newly diagnosed Ethiopian’s with chronic myeloid leukemia. PLoS One. 2019;14(3):e0213557. doi:10.1371/journal.pone.0213557
59. Jimmy B. Patient Medication Adherence: measures in Daily Practice. Oman Med J. 2011;26(3):155–159. doi:10.5001/omj.2011.38
60. Corsonello A, Pedone C, Garasto S, et al. The impact of comorbidity on medication adherence and therapeutic goals. BMC. 2009.
61. Klil-Drori AJ, Yin H, Azoulay L, et al. Persistence with generic imatinib for chronic myeloid leukemia: a matched cohort study. Haematologica. 2019;104(7):e293–e295. doi:10.3324/haematol.2018.211235
62. Pajiep M, Conte C, Huguet F, Gauthier M, Despas F, Lapeyre-Mestre M. Patterns of Tyrosine Kinase Inhibitor Utilization in Newly Treated Patients With Chronic Myeloid Leukemia: an Exhaustive Population-Based Study in France. Front Oncol. 2021;11:675609. doi:10.3389/fonc.2021.675609
63. Yood MU, Oliveria SA, Hirji I, Cziraky M, Davis C. Adherence to Treatment In Patients with Chronic Myelogenous Leukemia During a 10-Year Time Period: a Medical Record Review. Blood. 2010;116(21):1235. doi:10.1182/blood.V116.21.1235.1235
64. Cole AL, Jazowski SA, Dusetzina SB. Initiation of generic imatinib may improve medication adherence for patients with chronic myeloid leukemia. Pharmacoepidemiol Drug Saf. 2019;28(11):1529–1533. doi:10.1002/pds.4893
65. Senapati J, Sasaki K, Issa GC, et al. Management of chronic myeloid leukemia in 2023 – common ground and common sense. Blood Cancer J. 2023;13(1):1–12. doi:10.1038/s41408-023-00823-9
66. Alefan Q, Yao S, Taylor JG, et al. Factors associated with early nonpersistence among patients experiencing side effects from a new medication. J Am Pharm Assoc JAPhA. 2022;62(3):717–726.e5. doi:10.1016/j.japh.2021.12.001
67. Williams GR, Mackenzie A, Magnuson A, et al. Comorbidity in older adults with cancer. J Geriatr Oncol. 2016;7(4):249–257. doi:10.1016/j.jgo.2015.12.002
68. Jørgensen TL, Hallas J, Friis S, Herrstedt J. Comorbidity in elderly cancer patients in relation to overall and cancer-specific mortality. Br J Cancer. 2012;106(7):1353–1360. doi:10.1038/bjc.2012.46
69. R V, Chacko AM, Abdulla N, et al. Medication Adherence in Cancer Patients: a Comprehensive Review. Cureus. 2024;16(1). doi:10.7759/cureus.52721
70. Özdemir Z N, Kılıçaslan NA, Yılmaz M, Eşkazan AE. Guidelines for the treatment of chronic myeloid leukemia from the NCCN and ELN: differences and similarities. Int J Hematol. 2023;117(1):3–15. doi:10.1007/s12185-022-03446-1
71. Atallah E, Schiffer CA. Discontinuation of tyrosine kinase inhibitors in chronic myeloid leukemia: when and for whom? Haematologica. 2020;105(12):2738–2745. doi:10.3324/haematol.2019.242891
72. Lam WY, Fresco P. Medication Adherence Measures: an Overview. BioMed Res Int. 2015;2015:217047. doi:10.1155/2015/217047
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



