Back to Journals » Nature and Science of Sleep » Volume 17
Impact of Circadian Rhythm and Sleep Architecture Changes on Prognosis in Patients with Acute Hemorrhagic Stroke
Authors Yuan X , Fu Y, Ou Y, Xue J, Yang N, Liu H, Wang T, Wang J, Yan C, Zhang P
Received 15 April 2025
Accepted for publication 29 June 2025
Published 18 July 2025 Volume 2025:17 Pages 1655—1668
DOI https://doi.org/10.2147/NSS.S533202
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Marco Veneruso
Xiaodong Yuan,1,2,* Yongshan Fu,1,2,* Ya Ou,1,2 Jing Xue,1,2 Na Yang,1,2 Hongrui Liu,1,2 Tiantian Wang,1,2 Jing Wang,1,2 Cuiping Yan,1,2 Pingshu Zhang1,2
1Department of Neurology, Kailuan General Hospital, North China University of Technology, Tangshan, Hebei, People’s Republic of China; 2Key Laboratory of Neurobiological Function in Hebei Province, Tangshan, Hebei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Pingshu Zhang, Email [email protected]
Objective: Research is limited on whether circadian rhythm and sleep architecture alterations during acute intracerebral hemorrhage (ICH) influence patient outcomes. This study aims to characterize these changes and explore their association with clinical prognosis, offering new insights for diagnosis and treatment.
Methods: We enrolled 100 acute hemorrhagic stroke patients who underwent continuous, contactless sleep monitoring via a smart mattress for 3– 5 consecutive days. Prognosis was evaluated at discharge using the modified Rankin Scale (mRS), and patients were classified into favorable or unfavorable outcome groups. Circadian rhythm parameters (IS, IV, RA) and sleep metrics (eg, total sleep time, sleep latency, REM latency) during day and night were compared between groups. Multivariate logistic regression identified independent prognostic factors, and ROC analysis evaluated their predictive value.
Results: Group comparisons revealed statistically significant differences in RA and nighttime sleep latency between the favorable and unfavorable prognosis groups (P < 0.05). Binary logistic regression analysis identified nighttime sleep latency as an independent predictor of functional outcome (95% CI: 1.066 ~ 1.128, P < 0.05), which remained significant after adjusting for potential confounders (95% CI: 1.016 ~ 1.148, P < 0.05). The mean nighttime sleep latency was 18.14 minutes in the favorable group and 12.30 minutes in the unfavorable group. The area under the ROC curve (AUC) for nighttime sleep latency was 0.642 (95% CI: 0.526– 0.757, P = 0.028), with an optimal cutoff value of 10.95 minutes, yielding a sensitivity of 72.2% and specificity of 53.6%.
Conclusion: Hemorrhagic stroke patients show disrupted circadian stability, with greater RA reductions in those with worse outcomes. Nighttime sleep latency independently predicts poor prognosis with moderate accuracy. Circadian rhythm stability may serve as a prognostic marker in hemorrhagic stroke to avoid implying causality.
Keywords: stroke, stroke prognosis, circadian rhythm, intracerebral hemorrhage, nighttime sleep latency
Introduction
Stroke is the second leading cause of death globally and can be broadly classified into ischemic stroke (IS) and hemorrhagic stroke. Intracerebral hemorrhage (ICH), a major subtype of hemorrhagic stroke, accounts for approximately 27.9% of all new stroke cases. Although less common than IS, ICH is associated with significantly higher mortality and more severe long-term disability.1
The circadian rhythm system regulates a wide array of vital physiological functions, including cortical arousal, sympathetic nervous tone, cardiovascular dynamics, coagulation, immune activity, glucose homeostasis, and metabolism.2–4 These circadian-driven physiological oscillations are closely linked to stroke pathophysiology. For instance, the morning surge in sympathetic activity increases the risk of plaque rupture and thromboembolic events, thereby elevating the incidence of acute ischemic stroke.5 Conversely, a failure of nocturnal blood pressure dipping has been identified as a risk factor for stroke.6 Additionally, stroke-related hormonal fluctuations also play crucial roles in determining prognosis. Elevated cortisol levels post-stroke have been shown to exacerbate neuronal injury in ischemic brain regions, impair recovery, and worsen functional outcomes.7 In contrast, increased levels of orexins—particularly orexin-A—have demonstrated neuroprotective effects in both cerebral ischemia and ischemia-reperfusion injury (IRI) models.8
Sleep-wake cycles are essential physiological processes fundamental to maintaining overall health across the human lifespan. Sleep is intimately involved in regulating metabolism,9 neural plasticity,10 inflammatory responses,11 and apoptosis.12 Changes in these processes during sleep are closely associated with the onset, progression, and prognosis of stroke.
The relationship between sleep and stroke can be viewed from three perspectives: (1) sleep and sleep disorders as risk factors for stroke; (2) stroke as a risk factor for the development or exacerbation of sleep disorders; and (3) the impact of transient sleep disturbances on stroke outcomes. Among these, the third aspect—how short-term sleep alterations influence stroke prognosis—remains relatively underexplored.13
A recent study14 reported that, in the acute phase of ischemic stroke, patients exhibit prolonged rapid eye movement (REM) sleep latency and significantly reduced REM sleep duration. These alterations were found to be associated with unfavorable outcomes. Moreover, the study suggested that acute ischemic stroke may disrupt circadian sleep-wake organization, which could further contribute to poor prognosis.
However, evidence regarding the role of circadian rhythm disturbances and sleep architecture alterations in the acute phase of intracerebral hemorrhage (ICH) is limited. The present study aims to investigate the characteristics of circadian rhythmicity and sleep structure in patients with acute ICH and to explore their associations with clinical outcomes. These findings may offer novel insights into clinical assessment and management strategies for patients with hemorrhagic stroke.
Materials and Methods
Study Population
As a retrospective study, we analyzed patients diagnosed with intracerebral hemorrhage (ICH) who were treated at the Department of Neurology, Kailuan General Hospital and its Linxi Branch, both affiliated with North China University of Science and Technology, between January 2020 and December 2024. A total of 148 patients were initially screened (104 males, 70.2%; 44 females, 29.7%). After applying the inclusion and exclusion criteria, 100 patients were ultimately enrolled in the study (72 males, 72%; 28 females, 28%).
Patients were categorized into two groups based on their modified Rankin Scale (mRS) score at discharge, using a cutoff score of 2. Those with mRS ≤2 were assigned to the favorable outcome group (n = 72), and those with mRS >2 were assigned to the unfavorable outcome group (n = 28).
This study was approved by the Ethics Committee of Kailuan General Hospital, North China University of Science and Technology (Approval No. 2023027), and written informed consent was obtained from all participants.
Inclusion Criteria
(1) Age between 18 and 75 years, meeting the diagnostic criteria outlined in the 2019 Chinese Guidelines for the Diagnosis and Treatment of Intracerebral Hemorrhage, with confirmation of hemorrhagic lesions via cranial CT; (2) No disturbance of consciousness; (3) Sleep monitoring duration of ≥3 days, with a total daily recording time (day and night) of ≥8 hours.
Exclusion Criteria
(1) Patients with traumatic brain hemorrhage, post-thrombolysis hemorrhage, or subarachnoid hemorrhage; (2) History of psychiatric disorders or cognitive impairment; (3) Severe functional impairment of major organs, including the heart, lungs, and liver; (4) Use of sedative or sleep-promoting medications.
Clinical Data Collection
Baseline clinical information was collected for all patients, including sex, age, body mass index (BMI), and medical history (hypertension, diabetes mellitus, hyperhomocysteinemia, and hyperlipidemia), as well as smoking and alcohol consumption history.
Neuroimaging data were obtained from the first non-contrast head CT scan performed upon hospital admission (typically within 1 hour). Hematoma volume was calculated using the ABC/2 formula15 and the location of intracerebral hemorrhage was recorded accordingly.
Sleep Monitoring
Sleep monitoring was conducted using the SC-500 sleep monitoring system (Nanjing Bochuang Haiyun Electronic Technology Co., Ltd). Sleep parameters were recorded across two time periods: daytime (06:00–18:00) and nighttime (18:00–06:00 the following day). The recorded parameters included total recording time, total sleep time (TST), sleep onset latency (SOL), rapid eye movement (REM) wake after sleep onset (WASO), light sleep duration, deep sleep duration, non-rapid eye movement (NREM) sleep duration, and REM sleep duration. All sleep indices were reported as the mean values relative to the total recording time.
Circadian Rhythm Assessment Criteria
Circadian rhythm variations were evaluated using three key parameters: interdaily stability (IS), intradaily variability (IV), and relative amplitude (RA).16
- Interdaily Stability (IS): IS assesses the stability of 24-hour circadian activity variations and the balance between rest-activity rhythms and the circadian cycle. The IS value ranges from 0 to 1, with values closer to 1 indicating a more stable circadian rhythm.
- Intradaily Variability (IV): IV quantifies the fragmentation of circadian activity variability by analyzing the frequency and intensity of activity within a given time unit. It measures the transitions between rest and activity periods over time. The IV value ranges from 0 to 1, with higher values indicating greater rhythm fragmentation.
- Relative Amplitude (RA): RA is calculated using data from the most active 10-hour period (M10) and the least active 5-hour period (L5) within a 24-hour cycle.
All of the above indices were derived from heart rate measurements recorded during sleep monitoring. The specific calculation formulas are as follows:
 : Total monitoring duration (hours);
: Total monitoring duration (hours);  : 24 h;
: 24 h;  ; Average heart rate in the h hour of daily monitoring;
; Average heart rate in the h hour of daily monitoring;  :Average hourly heart rate during the monitoring period.
:Average hourly heart rate during the monitoring period.  :Average heart rate in the i hour of the monitoring period;
:Average heart rate in the i hour of the monitoring period; : Total heart rate during the most active 10-hour period;
: Total heart rate during the most active 10-hour period; : Total heart rate during the least active 5-hour period.
: Total heart rate during the least active 5-hour period.
Neurological Functional Prognosis Assessment
Neurological prognosis was evaluated using the Modified Rankin Scale (mRS). The mRS scoring criteria are as follows:
- 0 points: No symptoms.
- 1 point: Mild symptoms that do not affect daily life.
- 2 points: Mild disability but able to independently perform daily activities.
- 3 points: Moderate disability, requiring partial assistance for daily activities.
- 4 points: Severe disability, requiring assistance for daily activities.
- 5 points: Profound disability, fully dependent on assistance for daily life.
Patients were categorized into two groups based on their mRS scores at discharge:
Good prognosis group: mRS score ≤ 2
Poor prognosis group: mRS score > 2
Statistical Analysis
Statistical analyses were performed using SPSS 26.0 software. Continuous variables following a normal distribution were expressed as mean ± standard deviation (x±s) and compared between groups using an independent sample t-test. Non-normally distributed continuous variables were presented as median (P25, P75) and analyzed using the Mann–Whitney U-test. Categorical variables were expressed as counts (%) and compared using the Chi-square χ2 test.
Multivariate logistic regression analysis was conducted to identify significant predictors. Receiver operating characteristic (ROC) curve analysis was used to evaluate the predictive value of relevant factors identified through multivariate logistic regression. A p-value < 0.05 was considered statistically significant. As this was an exploratory analysis, no correction for multiple comparisons was applied.
Results
Comparison of General Characteristics Between the Two Groups
A total of 100 patients with intracerebral hemorrhage were ultimately included in this study, comprising 72 in the favorable outcome group and 28 in the poor outcome group. All continuous variables (age and BMI) met the assumptions for independent samples t-test, as assessed by the Shapiro–Wilk test for normality (P > 0.05) and Levene’s test for homogeneity of variances (P > 0.05). There were no statistically significant differences between the two groups in terms of age, sex, BMI, or past medical history (P > 0.05) (Table 1).
 |
Table 1 Comparison of General Characteristics |
Distribution of Hemorrhagic Brain Regions in the Two Groups
Among the 100 patients (72 with favorable outcomes and 28 with poor outcomes), chi-square tests for the distribution of brain regions met the condition of expected frequencies >5 (except for small sample regions such as the pons and frontal lobe, for which Fisher’s exact test was applied). The results showed no statistically significant differences in the distribution of brain regions between the two groups (P > 0.05) (Table 2).
 |
Table 2 Distribution Results of Hemorrhagic Brain Regions in Patients with Hemorrhagic Stroke |
Comparison of Hematoma Volume Between the Two Groups
The median hematoma volume in the poor outcome group was 5.33 mL, which was significantly higher than that in the favorable outcome group (2.92 mL) (P = 0.030), indicating a statistically significant difference (Table 3).
 |
Table 3 Comparison of Hemorrhage Volume Between Groups |
Comparison of Circadian Rhythm and Sleep Structure Parameters Between the Two Groups
Among the 100 patients, the poor outcome group showed a significantly lower Relative Amplitude (RA) (P = 0.014) and a significantly shorter nighttime sleep latency (P = 0.029), while no significant differences were found between the groups for the other indicators (P > 0.05) (Table 4).
 |
Table 4 Comparative Analysis of Circadian Rhythms and Sleep Architecture Parameters Between Groups |
Circadian Rhythm Changes in the Two Groups
A line chart was used to depict the 72-hour average heart rate variations in both groups (Figure 1). The results showed that in the good prognosis group, the heart rate curve exhibited a distinct circadian rhythm pattern, characterized by higher values during the daytime and lower values during the nighttime. In contrast, the poor prognosis group displayed a blunted circadian rhythm, with a flattened heart rate curve and less pronounced day-night fluctuations.
 |
Figure 1 Circadian rhythm variation diagram. |
Comparison of Hematoma Volume Between the Two Groups Based on Brain Regions
After stratifying patients by brain region, hematoma volume was compared between the favorable and poor outcome groups within each region. Among the 46 patients with basal ganglia hemorrhage (12 in the poor outcome group and 34 in the favorable outcome group), the hematoma volume was significantly different between the two groups (P < 0.05). No statistically significant differences were observed between the two groups in other brain regions (P > 0.05) (Table 5).
 |
Table 5 Intergroup Comparison of Cerebral Hemorrhage Volume by Brain Regions |
Multivariate Analysis of Prognostic Factors in Patients with Hemorrhagic Stroke
Multivariate Analysis of Circadian Rhythm and Sleep Structure Parameters in Relation to Hemorrhagic Stroke Prognosis
A binary logistic regression analysis was conducted using nighttime sleep latency and relative amplitude (RA) as independent variables, with prognosis outcome (good or poor) as the dependent variable. The results indicated that nighttime sleep latency was an independent risk factor for poor prognosis in patients with hemorrhagic stroke (P < 0.05). (Table 6).
 |
Table 6 Multivariable Analysis of Prognostic Factors in Hemorrhagic Stroke Patients |
Multivariate Regression Analysis of Nighttime Sleep Latency in Relation to Hemorrhage Location and Volume
Given the potential influence of hematoma volume and hemorrhage location on the prognosis of hemorrhagic stroke patients, a regression analysis was performed to control for these confounding factors by including both hematoma volume and hemorrhage location alongside nighttime sleep latency as independent variables.
After adjusting for confounding factors, the results demonstrated that nighttime sleep latency remained an independent risk factor for poor prognosis (P < 0.05) (Table 7).
 |
Table 7 Logistic Regression Analysis of Combined Effects: Nighttime Sleep Latency, Hemorrhage Volume and Location |
Box Plot of Nighttime Sleep Latency in Hemorrhagic Stroke Patients
The nighttime sleep latency was 18.14 minutes in the good prognosis group and 12.30 minutes in the poor prognosis group. The good prognosis group exhibited a longer nighttime sleep latency compared to the poor prognosis group (Figure 2).
 |
Figure 2 Box plot of nighttime sleep onset latency in patients with hemorrhagic stroke. |
Predictive Value of Nighttime Sleep Latency for Prognosis in Hemorrhagic Stroke Patients
The area under the ROC curve (AUC) for nighttime sleep latency in predicting prognosis was 0.642 (95% CI: 0.526–0.757, P = 0.028). The cutoff value for nighttime sleep latency was 10.95 minutes, with a sensitivity of 72.20% and a specificity of 53.6% (Figure 3).
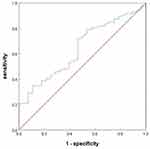 |
Figure 3 ROC curve of nighttime sleep onset latency for predicting outcomes in patients with hemorrhagic stroke. |
Discussion
This study found that hematoma volume in hemorrhagic stroke patients was larger in the poor prognosis group compared to the good prognosis group, consistent with previous studies.17,18 Regarding circadian rhythm parameters, the relative amplitude (RA) was lower in the poor prognosis group than in the good prognosis group. Among sleep structure parameters, nighttime sleep latency was shorter in the poor prognosis group.
After controlling for potential confounding factors, our findings suggest that nighttime sleep latency in the acute phase of hemorrhagic stroke remains a positive factor for prognosis. A moderate prolongation of nighttime sleep latency during the acute phase may facilitate recovery in hemorrhagic stroke patients. Furthermore, ROC curve analysis demonstrated that nighttime sleep latency has a certain predictive value for the prognosis of acute hemorrhagic stroke.
The homeostasis of circadian rhythms is closely associated with whole-brain neuronal activity, cortical functional plasticity regulation, and various physiological processes, including cell maintenance, synaptic scaling, firing rate homeostasis, and memory consolidation, all of which are achieved through sleep.19
In mammals, the synthesis of pineal melatonin is regulated by the suprachiasmatic nucleus (SCN) of the hypothalamus, which functions as the master circadian clock. This process is synchronized with the external light/dark cycle via intrinsically photosensitive retinal ganglion cells (ipRGCs), which transmit environmental light cues to the SCN, restricting melatonin production to nighttime.20
Stroke directly disrupts circadian rhythms, and environmental factors such as continuous incandescent lighting and noise in hospital wards can further disturb melatonin secretion. Since melatonin plays a crucial role in immune regulation, antioxidation, neurotransmission, and synaptic plasticity, such disturbances may negatively impact recovery.21,22
Studies have shown that stable circadian sleep rhythms enhance post-stroke motor learning and play a significant role in neuroplasticity and functional recovery.14 In our study, IS and IV—both indicators of circadian rhythm integrity—did not show significant differences between the poor prognosis group and the good prognosis group. However, the IS values in these groups were 0.30 and 0.32, respectively, suggesting that circadian rhythm stability was markedly reduced in this population, as higher IS values (closer to 1) indicate a more stable circadian rhythm.
Similarly, regarding RA, the poor prognosis group exhibited a lower RA value compared to the good prognosis group, indicating that patients with poor prognosis in this hemorrhagic stroke cohort had blunted circadian fluctuations. This finding aligns with our 72-hour average heart rate circadian rhythm plots, where we visually observed that in the good prognosis group, heart rate demonstrated a more pronounced diurnal rise (7:00–17:00) and nocturnal decline (18:00–6:00), with a more distinct nadir at 3:00, compared to the poor prognosis group.
Heart rate itself exhibits 24-hour oscillations, which are generally attributed to well-characterized circadian fluctuations in autonomic nervous system activity, neurotransmitters, and hormones.23 Disruptions in these fundamental circadian regulatory mechanisms can lead to pathological consequences.24 While both groups exhibited flattened circadian rhythm curves, the good prognosis group still retained greater heart rate variability across the day-night cycle compared to the poor prognosis group. This suggests that hemorrhagic stroke contributes to circadian rhythm disruption, while also implying that preserving near-normal circadian rhythmicity post-stroke may facilitate recovery.
Patients with hemorrhagic stroke who sleep for more than 12 hours per day can be diagnosed with hypersomnia, also known as excessive sleepiness, which is one of the most common sleep disorders associated with hemorrhagic stroke.25
In this cohort of hemorrhagic stroke patients, the total daytime sleep duration was 7.60 hours in the poor prognosis group and 8.06 hours in the good prognosis group. The total nighttime sleep duration was 9.84 hours in the poor prognosis group and 9.76 hours in the good prognosis group. The 24-hour sleep duration in both groups exceeded 12 hours per day, meeting the criteria for hypersomnia.
The primary cause of excessive sleep in these patients is brain edema induced by hemorrhage, which disrupts the specific ascending projection system, thereby interrupting arousal signals to the brain and impairing the “wakefulness center” in the hypothalamus. Furthermore, neuronal death leads to a reduction in the synthesis of key wakefulness-related neurotransmitters, including dopamine, norepinephrine, and acetylcholine.26
Studies have confirmed that orexin plays a crucial role in the central nervous system by maintaining wakefulness.27 Orexinergic neurons receive extensive afferent projections from the cortex and limbic system, including the prefrontal cortex, bed nucleus of the stria terminalis, and amygdala, as well as from brainstem regions, such as the dorsal raphe nucleus and rostral ventrolateral medulla.28–30 Efferent fibers from orexinergic neurons project to multiple brain regions involved in arousal regulation, including the ventral tegmental area, nucleus accumbens, basal forebrain, locus coeruleus, dorsal raphe nucleus, amygdala, and reticular formation.31–33
In our cohort of hemorrhagic stroke patients, the hematoma volume in the basal ganglia was larger in the poor prognosis group than in the good prognosis group. This suggests that as the hematoma expands, the corresponding neural network structures may undergo more severe suppression, potentially contributing to excessive sleepiness in ICH patients.
Nocturnal SOL refers to the time required to transition from attempting to fall asleep to actual sleep onset. It is an important parameter for assessing sleep quality and sleep disorders. The normal SOL typically ranges from 10 to 20 minutes, whereas an SOL exceeding 30 minutes is indicative of insomnia.
Our study found that during the acute phase of hemorrhagic stroke, the mean nocturnal SOL was 12.30 minutes in the poor prognosis group, compared to 18.14 minutes in the good prognosis group (Figure 3). When the nocturnal SOL was 10.95 minutes, the sensitivity for predicting hemorrhagic stroke prognosis was 72.20%, with a specificity of 53.6%.
Our findings suggest that a moderate prolongation of nocturnal SOL serves as an independent protective factor for the prognosis of hemorrhagic stroke patients. These patients exhibit significantly increased 24-hour sleep duration, and maintaining a relatively prolonged wakefulness period during the transition between daytime and nighttime sleep—rather than immediately re-entering sleep—may confer potential prognostic benefits.
Previous studies have indicated that orexin exerts neuroprotective effects by regulating the OX1 receptor (OX1R)-mediated MAPK/ERK/mTOR signaling pathway, which inhibits excessive autophagy.34 Additionally, orexin has been shown to protect neurons from oxidative stress-induced damage.35 Thus, we hypothesize that in hemorrhagic stroke patients, the sleep-wake cycle is influenced by both melatonin and orexin, while intracerebral hemorrhage itself may alter their secretion. Based on this interaction, we propose that a moderate prolongation of nocturnal SOL (rather than excessive wakefulness) during the acute phase of hemorrhagic stroke may contribute to better functional recovery and improved prognosis.
A moderate prolongation of nocturnal SOL in hemorrhagic stroke patients may also be associated with the activation and inhibition of the ascending reticular activating system (RAS). The reticular formation is a collection of neuronal networks extending from the rostral midbrain to the rostral medulla, named for its loosely arranged, net-like structure. This formation comprises various nuclei clusters, which mediate multiple physiological functions, among which the RAS plays a critical role in wakefulness and consciousness. The RAS is primarily located in the central and dorsal brainstem, spanning the caudal midbrain to the pontomesencephalic region.36
In our study population, both the poor prognosis group (17.4 h/day) and the good prognosis group (17.8 h/day) exhibited excessive sleep duration, indicative of a hypersomnolence state. Given that the poor prognosis group had a shorter nocturnal SOL compared to the good prognosis group, We propose an exploratory hypothesis: nocturnal SOL may reflect a potential association with ascending reticular activating system integrity in hemorrhagic stroke patients. Specifically, patients with a moderately prolonged nocturnal SOL may have a relatively preserved RAS function, which, in turn, may facilitate their daily functional recovery to some extent.
Moreover, the shortened sleep onset latency (SOL) observed in patients with poor prognosis may be associated with post-stroke fatigue (PSF). Previous studies have demonstrated significant correlations between PSF and various abnormal sleep parameters, including poor sleep quality, increased daytime sleepiness, prolonged and more frequent daytime naps, and elevated frequency of nocturnal awakenings.37 Although direct evidence linking SOL to PSF is currently lacking, mechanistic studies suggest that impaired activity of orexin (hypocretin) neurons—a key driver of PSF38—may also underlie SOL reduction. Given that orexin plays a central role in maintaining wakefulness within the central nervous system,27 damage to the hypothalamic orexinergic pathways following hemorrhagic stroke may contribute to both the development of PSF and the pathological shortening of SOL through a dual-pathway mechanism.
Summary
Patients with hemorrhagic stroke exhibit poor stability in their circadian rhythms, with a more pronounced reduction in RA in cases of poor prognosis. Nocturnal SOL is an independent risk factor for hemorrhagic stroke prognosis and has certain predictive value. Maintaining a relatively intact circadian rhythm may be beneficial for patient recovery.
Limitation
Our study identified nocturnal SOL as an independent risk factor for hemorrhagic stroke prognosis, which may be associated with circadian rhythm disruption and altered hormonal secretion following stroke. However, this hypothesis requires further validation through additional studies, such as investigations into acute-phase changes in hormonal markers like melatonin and orexin in patients with ICH.
Although we controlled for key confounding factors such as hematoma volume and location, it is important to acknowledge that sleep disturbances are highly prevalent after ICH and can contribute to autonomic dysfunction,39 catecholamine imbalance,40 and cortisol dysregulation.41 These factors, in turn, may influence stroke onset, progression, and prognosis. Therefore, our findings may still be affected by confounding factors such as obstructive sleep apnea (OSA) and other sleep disorders. Further studies are warranted to elucidate these potential influences and strengthen the validity of our conclusions.
Finally, the relatively small sample size in this study may limit the statistical power and generalizability of the results. A small sample size could reduce the statistical efficiency of subgroup analyses and may amplify the influence of individual variability on overall outcomes. Therefore, future studies with larger sample sizes and multicenter, prospective cohorts are warranted to further validate our findings.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The authors affirm that this present study follows the ethical principles outlined in the Declaration of Helsinki. Ethical approval for this study was granted by the Ethics Review Committee of Kailuan General Hospital affiliated to North China University of Science and Technology (2023027) and confirmation that informed consent was obtained from the study participants.
Authorship Contribution Statement
Xiaodong Yuan and Yongshan are co-first authors. Xiaodong Yuan, Yongshan Fu: writing - original draft, methodology, conceptualization, formal analysis, investigation, and writing-review and editing. Ya Ou, Jing Xue, Hongrui Liu: formal analysis, project administration, investigation writing-review and editing. Tiantian Wang, Jing Wang: conceptualization, methodology, resources writing-review and editing. Cuiping Yan, Na Yang: investigation, visualization writing-review and editing. Pingshu Zhang: methodology, conceptualization, writing - review and editing, and supervision. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by the 2024 Tangshan Municipal Science and Technology Program under project numbers 24150217C and 24120202B, respectively.
Disclosure
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
1. Feigin VL, Stark BA, Johnson CO. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 2021;20:795–820. doi:10.1016/s1474-4422(21)00252-0
2. Zaki NFW, Spence DW, Subramanian P, et al. Basic chronobiology: what do sleep physicians need to know? Sleep Sci. 2020;13:256–266. doi:10.5935/1984-0063.20200026
3. Nishimon S, Nishino N, Nishino S. Advances in the pharmacological management of non-24-h sleep-wake disorder. Exp Opinion Pharmacother. 2021;22:1039–1049. doi:10.1080/14656566.2021.1876665
4. Coiffard B, Diallo AB, Mezouar S, Leone M, Mege JL. A tangled threesome: circadian rhythm, body temperature variations, and the immune system. Biology. 2021;10:65. doi:10.3390/biology10010065
5. Kawano Y. Diurnal blood pressure variation and related behavioral factors. Hypertens Res. 2011;34:281–285. doi:10.1038/hr.2010.241
6. Pandian JD, Wong AA, Lincoln DJ, et al. Circadian blood pressure variation after acute stroke. J Clin Neurosci. 2006;13:558–562. doi:10.1016/j.jocn.2005.09.003
7. Liu JA, Walton JC, DeVries AC, Nelson RJ. Disruptions of circadian rhythms and thrombolytic therapy during ischemic stroke intervention. Front Neurosci. 2021;15:675732. doi:10.3389/fnins.2021.675732
8. Wang C, Wang Q, Ji B, et al. The orexin/receptor system: molecular mechanism and therapeutic potential for neurological diseases. Front Mol Neurosci. 2018;11:220. doi:10.3389/fnmol.2018.00220
9. Lack LC, Gradisar M, Van Someren EJ, Wright HR, Lushington K. The relationship between insomnia and body temperatures. Sleep Med Rev. 2008;12:307–317. doi:10.1016/j.smrv.2008.02.003
10. Duss SB, Seiler A, Schmidt MH, et al. The role of sleep in recovery following ischemic stroke: a review of human and animal data. Neurobiol Sleep Circadian Rhythms. 2017;2:94–105. doi:10.1016/j.nbscr.2016.11.003
11. Li X, et al. Sleep deprivation promotes endothelial inflammation and atherogenesis by reducing exosomal miR-182-5p. Arteriosclerosis Thrombosis Vasc Biol. 2023;43:995–1014. doi:10.1161/atvbaha.123.319026
12. Matsumoto Y, Mishima K, Satoh K, et al. Total sleep deprivation induces an acute and transient increase in NK cell activity in healthy young volunteers. Sleep. 2001;24:804–809.
13. Miano S, et al. SAS CARE 1: sleep architecture changes in a cohort of patients with Ischemic Stroke/TIA. Sleep Medicine. 2022;98:106–113. doi:10.1016/j.sleep.2022.06.002
14. Pace M, Camilo MR, Seiler A, et al. Rapid eye movements sleep as a predictor of functional outcome after stroke: a translational study. Sleep. 2018;41. doi:10.1093/sleep/zsy138
15. Teo KC, Fong S-M, Leung WCY, et al. Location-specific hematoma volume cutoff and clinical outcomes in intracerebral hemorrhage. Stroke. 2023;54:1548–1557. doi:10.1161/strokeaha.122.041246
16. Gonçalves BS, Adamowicz T, Louzada FM, Moreno CR, Araujo JF. A fresh look at the use of nonparametric analysis in actimetry. Sleep Med Rev. 2015;20:84–91. doi:10.1016/j.smrv.2014.06.002
17. Hemphill JC, Greenberg SM, Anderson CS, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:2032–2060. doi:10.1161/str.0000000000000069
18. Lo WD, Hajek C, Pappa C, Wang W, Zumberge N. Outcomes in children with hemorrhagic stroke. JAMA Neurol. 2013;70:66–71. doi:10.1001/jamaneurol.2013.577
19. Thomas CW, Blanco-Duque C, Bréant BJ, et al. Psilocin acutely alters sleep-wake architecture and cortical brain activity in laboratory mice. Transl Psychiatry. 2022;12:77. doi:10.1038/s41398-022-01846-9
20. Canteras NS, Ribeiro-Barbosa ER, Goto M, Cipolla-Neto J, Swanson LW. The retinohypothalamic tract: comparison of axonal projection patterns from four major targets. Brain Res Rev. 2011;65:150–183. doi:10.1016/j.brainresrev.2010.09.006
21. Cipolla-Neto J, Amaral FGD. Melatonin as a Hormone: new Physiological and Clinical Insights. Endocrine Reviews. 2018;39:990–1028. doi:10.1210/er.2018-00084
22. Claustrat B, Leston J. Melatonin: physiological effects in humans. Neuro-Chirurgie. 2015;61:77–84. doi:10.1016/j.neuchi.2015.03.002
23. Zhang J, Chatham JC, Young ME. Circadian regulation of cardiac physiology: rhythms that keep the heart beating. Ann Rev Physiology. 2020;82:79–101. doi:10.1146/annurev-physiol-020518-114349
24. Smolensky MH, Hermida RC, Reinberg A, Sackett-Lundeen L, Portaluppi F. Circadian disruption: new clinical perspective of disease pathology and basis for chronotherapeutic intervention. Chronobiol. Int. 2016;33:1101–1119. doi:10.1080/07420528.2016.1184678
25. Ferre A, Ribó M, Rodríguez-Luna D, et al. Strokes and their relationship with sleep and sleep disorders. Neurologia. 2013;28:103–118. doi:10.1016/j.nrl.2010.09.016
26. Hepburn M, Bollu PC, French B, Sahota P. Sleep medicine: stroke and sleep. Missouri Med. 2018;115:527–532.
27. Li SB, de Lecea L. The hypocretin (orexin) system: from a neural circuitry perspective. Neuropharmacology. 2020;167(107993):107993. doi:10.1016/j.neuropharm.2020.107993
28. Sakurai T, Nagata R, Yamanaka A, et al. Input of orexin/hypocretin neurons revealed by a genetically encoded tracer in mice. Neuron. 2005;46:297–308. doi:10.1016/j.neuron.2005.03.010
29. Jalewa J, Joshi A, McGinnity TM, et al. Neural circuit interactions between the dorsal raphe nucleus and the lateral hypothalamus: an experimental and computational study. PLoS One. 2014;9:e88003. doi:10.1371/journal.pone.0088003
30. Bochorishvili G, Nguyen T, Coates MB, et al. The orexinergic neurons receive synaptic input from C1 cells in rats. J Comparative Neurol. 2014;522:3834–3846. doi:10.1002/cne.23643
31. Dehkordi O, Rose JE, GarcAA-a MID, et al. neuroanatomical relationships between orexin/hypocretin-containing neurons/nerve fibers and nicotine-induced c-fos-activated cells of the reward-addiction neurocircuitry. J Alcoholism Drug Dependence. 2017;5. doi:10.4172/2329-6488.1000273
32. Hasegawa E, Maejima T, Yoshida T, et al. Serotonin neurons in the dorsal raphe mediate the anticataplectic action of orexin neurons by reducing amygdala activity. Proc Natl Acad Sci USA. 2017;114:E3526–e3535. doi:10.1073/pnas.1614552114
33. Arendt DH, Hassell J, Li H, et al. Anxiolytic function of the orexin 2/hypocretin A receptor in the basolateral amygdala. Psychoneuroendocrinology. 2014;40:17–26. doi:10.1016/j.psyneuen.2013.10.010
34. Xu D, et al. Orexin-A protects against cerebral ischemia-reperfusion injury by inhibiting excessive autophagy through OX1R-mediated MAPK/ERK/mTOR pathway. Cell. Signalling. 2021;79:109839. doi:10.1016/j.cellsig.2020.109839
35. Oliver PL, et al. Oxr1 is essential for protection against oxidative stress-induced neurodegeneration. PLoS Genetics. 2011;7:e1002338. doi:10.1371/journal.pgen.1002338
36. Taran S, et al. The reticular activating system: a narrative review of discovery, evolving understanding, and relevance to current formulations of brain death. Canad J Anaesthes J Canad D’anesthesie. 2023;70:788–795. doi:10.1007/s12630-023-02421-6
37. Ho LYW, Lai CKY, Ng SSM. Contribution of sleep quality to fatigue following a stroke: a cross-sectional study. BMC Neurol. 2021;21:151. doi:10.1186/s12883-021-02174-z
38. Kuppuswamy A, et al. Mechanisms of post-stroke fatigue: a follow-up from the third stroke recovery and rehabilitation roundtable. Neurorehabil Neural Repair. 2024;38:52–61. doi:10.1177/15459683231219266
39. Meerlo P, Sgoifo A, Suchecki D. Restricted and disrupted sleep: effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Med Rev. 2008;12:197–210. doi:10.1016/j.smrv.2007.07.007
40. Zhang J, Ma RCW, Kong AP, et al. Relationship of sleep quantity and quality with 24-hour urinary catecholamines and salivary awakening cortisol in healthy middle-aged adults. Sleep. 2011;34:225–233. doi:10.1093/sleep/34.2.225
41. Kumari M, Badrick E, Ferrie J, et al. Self-reported sleep duration and sleep disturbance are independently associated with cortisol secretion in the Whitehall II study. J Clin Endocrinol Metab. 2009;94:4801–4809. doi:10.1210/jc.2009-0555
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


