Back to Journals » Risk Management and Healthcare Policy » Volume 18
Impact of DRG Reform Policies on Hospitalization Costs of Stroke Patients in Western China: Wisdom from Traditional Chinese Medicine
Authors Wang J, Chen M , Yang J
Received 25 March 2025
Accepted for publication 4 July 2025
Published 11 July 2025 Volume 2025:18 Pages 2401—2411
DOI https://doi.org/10.2147/RMHP.S525667
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Haiyan Qu
Jiayi Wang,1 Mengen Chen,2 Jingyu Yang1,3
1School of Health Management, Gansu University of Chinese Medicine, Lanzhou, People’s Republic of China; 2School of Traditional Chinese Medicine, Beijing University of Chinese Medicine, Beijing, People’s Republic of China; 3School of Public Health, Lanzhou University, Lanzhou, People’s Republic of China
Correspondence: Jingyu Yang, School of Health Management, Gansu University of Chinese Medicine, 35 Dingxi East Road, Chengguan District, Lanzhou, Gansu, 730000, Email [email protected]
Background: Stroke presents a significant economic burden worldwide, with the impact being especially pronounced in developing countries. China is currently implementing Diagnosis-Related Group (DRG) reforms, attempting to use more traditional Chinese medicine (TCM) modalities to alleviate the economic burden on stroke patients.
Methods: This retrospective study extracted the medical records of stroke inpatients at Qingyang City Hospital of TCM from 2017 to 2022 from China’s Gansu National Health Big Data Platform. A single-group interrupted time series (ITS) design was employed to assess the impact of DRG reform on patients’ hospitalization costs and length of stay (LOS). Additionally, a two-group ITS was utilized to evaluate treatment costs and medicine costs.
Results: The single-group ITS analysis indicated that the average LOS decreased by 0.06 days per month following the reform (P < 0.05), while the average hospitalization cost declined by 48.92 yuan per month (P < 0.05). The two-group ITS results revealed a significant reduction in the average monthly cost of Western medicine by 22.67 yuan post-reform (P < 0.05), whereas the average monthly cost of Chinese medicine increased by 2.93 yuan, though this change was not statistically significant (P > 0.05). Additionally, the average monthly cost of Western medical treatment decreased by 11.24 yuan (P < 0.05). Acupuncture and massage treatment costs exhibited an initial sharp increase followed by a downward trend, with an average monthly decrease of 9.53 yuan (P < 0.05).
Conclusion: DRG reduced hospitalization costs and shortened the LOS of stroke patients, which may be related to the increased use of TCM in stroke treatment.
Keywords: DRG, stroke, Chinese medicine cost, acupuncture and massage treatment cost, ITS
Introduction
As the second leading cause of death and the third leading cause of disability worldwide at present, stroke is characterized by high morbidity, high disability, high mortality, and high recurrence.1,2 Globally, about 7.3 million people die each year from stroke-related diseases, and the prevalence of varying degrees of sequelae is as high as 70% to 80% among those who survive stroke.3,4 A study by the World Stroke Organization (WSO) estimated the global economic burden of stroke at over $721 billion, equivalent to 0.66% of the global GDP, with the majority of this burden concentrated in low- and lower-middle-income countries.5 Stroke is also the leading cause of death in China, accounting for about one-third of all global stroke-related deaths.6 Since 2004, China has allocated more than 10 billion yuan annually to the treatment of cerebral infarction. When combined with indirect economic losses, the total expenditure approaches 20 billion yuan.7 This burden is particularly acute in western China, where healthcare resources are relatively limited. As such, the management and control of stroke—recognized as a high-cost and high-burden condition—has become a critical focus of healthcare reform efforts in the country.
In the field of stroke prevention and treatment, current Western medical treatment is mostly based on symptomatic treatment and improvements in neurological symptoms.8 Standard therapies, including thrombolytic therapy, anticoagulation therapy, and neuroprotective drug therapy, which are crucial for the rescue of stroke patients in the acute phase, are available.9 However, owing to their narrow therapeutic window, strong adverse effects and single target of action, they are often limited in clinical applications.10,11 As an accessible and low-cost health resource, TCM has significant applications in stroke rehabilitation. In recent years, the proportion of stroke patients utilizing TCM has steadily increased.12,13 Evidence suggests that the integrated use of complementary and alternative therapies—such as TCM, acupuncture, and meridian massage—offers greater benefits than conventional Western medicine alone in improving post-stroke neurological deficits, mitigating the inflammatory response, and managing stroke-related complications.14,15
Disease burden is an important topic of concern for stroke patients. To control healthcare costs and improve healthcare quality management, China’s National Healthcare Security Bureau launched a nationwide DRG reform in 2019.16 The core of the DRG reform in TCM hospitals involves categorizing diseases based on similarities in clinical characteristics and resource utilization, establishing fixed payments for each group, standardizing pricing for identical conditions, and holding institutions accountable for financial outcomes.17 The primary objective of the reform is to promote the optimization of clinical pathways, incentivize the application of Chinese medicine techniques, and encourage the adoption of cost-effective treatment approaches. In this context, this study investigated the impact of DRG payment reform on changes in the hospitalization-related costs and cost structure of stroke patients in Qingyang City TCM Hospital in Gansu Province, seeking Chinese wisdom on TCM with respect to the economic burden associated with stroke patients.
Materials and Methods
Data Sources and Sample Selection
The data for this study were obtained from the Gansu Province National Health Big Data Platform (a governmental non-full disclosure database), which covers the case home page data of inpatients in Qingyang City TCM Hospital from January 2017 to June 2022. In accordance with the International Classification of Diseases, Tenth Edition (ICD-10) codes (I60, I61, I62, I63, I64) and TCM codes BNG080 (1995 edition) or A07.01.01 (2021 edition) as the primary diagnosis, 6965 patients with stroke were extracted from this study. The exclusion criteria included ① cases with mismatched disease codes and diagnostic information; ② cases with missing information on the front page of the cases or with logical errors; ③ cases with missing or zero hospitalization costs; and ④ cases with LOS less than 1 day or more than 90 days. After cleaning and screening according to the inclusion and exclusion criteria, as well as desensitizing the data, 6903 cases were ultimately included. Among them, the subtypes of stroke were classified as ischemic stroke (ICD-10:I63), hemorrhagic stroke (ICD-10:I60-I62), and undetermined stroke (ICD-10:I64).
The data collected included the following: (1) Socio-demographic information: gender, age, and marital status. (2) Medical information: type of stroke, ICD-10 code, TCM code, admission time, discharge time, LOS, use of TCM diagnostic and treatment equipment, use of TCM diagnostic and treatment techniques, and dialectical nursing based on TCM evidence. (3) Cost information: hospitalization cost; Western medicine cost (including drug cost and antibacterial drug cost); Chinese medicine cost (comprising herbal medicine cost, proprietary Chinese medicine cost, and Chinese medicine preparation cost); Western medical treatment cost (including non-surgical treatment item cost, clinical physiotherapy cost, surgical treatment cost, anesthesia cost, and surgery cost); acupuncture and massage treatment cost (including acupuncture and moxibustion cost, as well as Chinese massage treatment cost).
Research Methodology and Modeling
Single-Group ITS Analysis
ITS is a quasi-experimental research design that evaluates the effects of interventions.18 Trends in outcome indicators before and after intervention implementation were compared by collecting data related to outcome indicators at multiple time points.19 Currently, the ITSA has been widely used to study the effects of public policy interventions, and its main advantage lies in its ability to distinguish between the changes brought about by interventions and the changes in the things themselves.20 Among these, segmented regression, which is an effective method for assessing the effects of interventions and requires fewer time nodes, is the most commonly used model for the ITSA.21,22
In Qingyang City, the trial implementation of the CHS-DRG health insurance payment system commenced in October 2019, which was designated as the intervention point of this study. The Qingyang City Hospital of Traditional Chinese Medicine was the first pilot TCM hospital in China to participate in the DRG reform and is henceforth referred to as the “pilot TCM hospital” throughout the text. The period from January 2017 to September 2019 is defined as the pre-DRG reform phase, while the period from October 2019 to June 2022 is defined as the post-DRG reform phase. The time variable was selected as the independent variable, the statistics were conducted in months, and a single-group ITS was used to test the effect of DRG reform on the inpatient costs and inpatient days of stroke patients in TCM hospitals. The model application equation is as follows:
where  is the dependent variable, which is the evaluation indicator describing the effect of the reform;
is the dependent variable, which is the evaluation indicator describing the effect of the reform;  is the intercept, which indicates the level of Y at the starting stage;
is the intercept, which indicates the level of Y at the starting stage;  is the pre-reform slope, which indicates the monthly increase in hospitalization costs before the DRG reform;
is the pre-reform slope, which indicates the monthly increase in hospitalization costs before the DRG reform;  is the amount of instantaneous change, which is the difference in the level of the indicator before and after the reform;
is the amount of instantaneous change, which is the difference in the level of the indicator before and after the reform;  denotes the amount of change in the post-reform slope, which is the difference in the monthly increase in hospitalization costs before and after the reform; and
denotes the amount of change in the post-reform slope, which is the difference in the monthly increase in hospitalization costs before and after the reform; and  +
+ are the overall trend of the post-reform slope, denoting the monthly increase in hospitalization costs after the reform.
are the overall trend of the post-reform slope, denoting the monthly increase in hospitalization costs after the reform.  indicates a time series of 66 consecutive months from January 2017 to June 2022, coded by year and month as 2017m1, 2017m2 2017m3 … 2022m6.
indicates a time series of 66 consecutive months from January 2017 to June 2022, coded by year and month as 2017m1, 2017m2 2017m3 … 2022m6.  denotes the time dummy variable, which is assigned a value of “0” before the DRG reform and a value of “1” after the reform;
denotes the time dummy variable, which is assigned a value of “0” before the DRG reform and a value of “1” after the reform;  denotes the post-intervention time series; and
denotes the post-intervention time series; and  denotes random error.23,24
denotes random error.23,24
For the ITS analysis, this paper uses the Cumby-Huizinga method for the autocorrelation test and the Newey-West method for coefficient adjustment and calculation.25–27 For the data analysis process, Excel software was used to establish and maintain the database, the statistical analysis was completed with Stata 17.0 software, and a two-sided test with P < 0.05 was considered statistically significant.
Two-Group ITS Analysis
We used Western medicine costs and TCM costs as the control and experimental groups and Western medical treatment costs and acupuncture and massage treatment costs as the control and experimental groups, respectively. The impact of DRG reform on the changes in the structure of these four types of costs was explored by using a two-group ITS model. The model application equation is as follows:
where  represents the dependent variable, which is the primary outcome indicator of the study;
represents the dependent variable, which is the primary outcome indicator of the study;  represents the control group intercept, which is the constant term;
represents the control group intercept, which is the constant term;  represents the trend of change (slope) of the control group before the reform;
represents the trend of change (slope) of the control group before the reform;  denotes the change in the level of the control group at the time of the reform;
denotes the change in the level of the control group at the time of the reform;  denotes the difference in the slope of the control group between the post-reform and the pre-reform slopes;
denotes the difference in the slope of the control group between the post-reform and the pre-reform slopes;  refers to the difference in the level of the two groups before the reform;
refers to the difference in the level of the two groups before the reform;  is to the difference in the trend of change (slope) of the two groups before the reform; and
is to the difference in the trend of change (slope) of the two groups before the reform; and  indicates to the difference in the level of the two groups at the time of the reform change at the time of the reform, which is used to measure the short-term effect of the policy reform; and
indicates to the difference in the level of the two groups at the time of the reform change at the time of the reform, which is used to measure the short-term effect of the policy reform; and  denotes to the difference in the amount of change in the slopes of the two groups before and after the reform.
denotes to the difference in the amount of change in the slopes of the two groups before and after the reform.  indicates the sum of
indicates the sum of  and
and  , which reflects the long-run trend of change in the control group after the reform, and
, which reflects the long-run trend of change in the control group after the reform, and  is the sum of
is the sum of  ,
,  ,
,  , and
, and  , denoting the long-run trend of change in the experimental group after the reform. In addition, Z denotes a dummy variable for the experimental and control groups. The Chinese medicine cost as the experimental group is indicated by “1”, and the Western medicine cost as the control group is denoted by “0”; the acupuncture and massage treatment cost as the experimental group is denoted by “1”; and the Western medical treatment cost as the control group is denoted by “0”.
, denoting the long-run trend of change in the experimental group after the reform. In addition, Z denotes a dummy variable for the experimental and control groups. The Chinese medicine cost as the experimental group is indicated by “1”, and the Western medicine cost as the control group is denoted by “0”; the acupuncture and massage treatment cost as the experimental group is denoted by “1”; and the Western medical treatment cost as the control group is denoted by “0”.  and
and  are the same as those in regression model (1), and
are the same as those in regression model (1), and  is the random error. The test method is the same as above.
is the random error. The test method is the same as above.
Results
Descriptive Analysis
A total of 6,903 stroke inpatients were included in this study, with 2,583 admitted prior to the DRG reform and 4,320 admitted following its implementation. The socio-demographic characteristics and hospitalization information of patients before and after the policy intervention are presented in Table 1. The proportion of male patients exceeded that of female patients both before and after the reform, accounting for 56.83% and 55.90%, respectively. The average age of inpatients was 68 years prior to the reform and 70 years following the reform. Additionally, the proportion of married patients showed a decline after the implementation of the policy. There was no significant difference between stroke patients before and after DRG reform in terms of gender or hospitalization costs (P > 0.05). The differences in age, marital status, LOS, stroke type, use of TCM diagnostic and treatment equipment, use of TCM diagnostic and treatment technology, dialectical nursing based on TCM evidence, Western medical treatment cost, acupuncture and massage treatment cost, Western medicine cost, and Chinese medicine cost were statistically significant (P < 0.05).
 |
Table 1 General Information on Hospitalized Patients Before and After DRG Reform |
ITS results
Single-Group ITS
Cumby-Huisinga autocorrelation tests were performed on hospitalization-related costs and hospital days. The results revealed autocorrelation between three variables, namely, hospitalization costs, drug costs, and treatment costs, as shown in the Appendix, Table A1. The hospitalization costs showed first-order autocorrelation, the costs of medicines and treatments showed second-order autocorrelation, and no autocorrelation existed between the LOS. To ensure the robustness of the ITS, this study used the “lag(1)” and “lag(2)” commands to adjust for autocorrelation effects in the healthcare cost analysis.
We conducted a single-group time series analysis of hospitalization costs and LOS. The results of the study revealed that the hospitalization costs of the pilot TCM hospitals significantly increased before the DRG reform ( = 40.12, P<0.05) and that the change in the level of hospitalization costs during the reform period was not statistically significant (
= 40.12, P<0.05) and that the change in the level of hospitalization costs during the reform period was not statistically significant ( = 78.42, P>0.05). However, there was a significant downward trend after the reform, with an average monthly decrease of 48.92 CNY (
= 78.42, P>0.05). However, there was a significant downward trend after the reform, with an average monthly decrease of 48.92 CNY ( +
+ = –48.92, P<0.05). In terms of the LOS, there was a significant downward trend before the DRG reform (
= –48.92, P<0.05). In terms of the LOS, there was a significant downward trend before the DRG reform ( = –0.11, P < 0.05). There was no statistically significant change in the LOS during the reform period (
= –0.11, P < 0.05). There was no statistically significant change in the LOS during the reform period ( = –0.04, P > 0.05). However, there was a significant downward trend after the reform was implemented, with an average decrease of 0.06 days (
= –0.04, P > 0.05). However, there was a significant downward trend after the reform was implemented, with an average decrease of 0.06 days ( +
+ = 0.06, P < 0.05). The detailed results are shown in Table 2, and specific trend changes are shown in Figures 1 and 2.
= 0.06, P < 0.05). The detailed results are shown in Table 2, and specific trend changes are shown in Figures 1 and 2.
 |
Table 2 Results of Single-Group ITS Regression of Hospitalization Costs and LOS Before and After DRG Reform |
 |
Table 3 Results of Two-Group ITS Regression of the Medicine Costs Before and After DRG Reform |
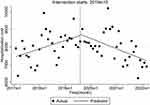 |
Figure 1 Changes in hospitalization costs before and after DRG reform for stroke patients. |
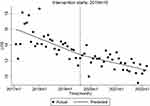 |
Figure 2 Changes in LOS before and after DRG reform for stroke patients. |
 |
Figure 3 Changes in Chinese medicine and Western medicine costs before and after DRG reform for stroke patients. |
Two-Group ITS
On the basis of the above analysis, we used two two-group ITS to study the structural changes in hospitalization costs for stroke patients after the DRG reform. Regarding patients’ drug costs, the Western medicine costs for stroke patients did not exhibit a significant change prior to the DRG reform ( = –26.76, P > 0.05). Although there was an increase in cost at the point of reform (
= –26.76, P > 0.05). Although there was an increase in cost at the point of reform ( = 252.19, P > 0.05), it was not statistically significant. Following the reform, a downward trend was observed, with an average monthly decrease of 22.67 yuan (
= 252.19, P > 0.05), it was not statistically significant. Following the reform, a downward trend was observed, with an average monthly decrease of 22.67 yuan ( = –22.67, P < 0.05). The Chinese medicine costs for stroke patients showed an insignificant trend before the reform (combined
= –22.67, P < 0.05). The Chinese medicine costs for stroke patients showed an insignificant trend before the reform (combined  ,
,  ), the cost change was insignificant at the time of the reform (combined
), the cost change was insignificant at the time of the reform (combined  ,
,  ), and the change was likewise insignificant after the reform (
), and the change was likewise insignificant after the reform ( = –2.93, P>0.05). The detailed results are shown in Table 3 and Figure 3. In terms of patients’ treatment costs, the change in Western medical treatment costs for stroke patients was not significant prior to the DRG reform (
= –2.93, P>0.05). The detailed results are shown in Table 3 and Figure 3. In terms of patients’ treatment costs, the change in Western medical treatment costs for stroke patients was not significant prior to the DRG reform ( = 22.87, P > 0.05). However, there was a significant decrease in the cost level at the time of the reform (
= 22.87, P > 0.05). However, there was a significant decrease in the cost level at the time of the reform ( = −754.04, P < 0.05), followed by a continued and significant downward trend post-reform, with an average monthly reduction of 11.24 yuan (
= −754.04, P < 0.05), followed by a continued and significant downward trend post-reform, with an average monthly reduction of 11.24 yuan ( = –11.24, P<0.05). Meanwhile, the acupuncture and massage treatment costs for stroke patients did not change significantly before the reform (combined
= –11.24, P<0.05). Meanwhile, the acupuncture and massage treatment costs for stroke patients did not change significantly before the reform (combined  and
and  ), the cost level increased significantly by about 390.32 yuan at the time of the reform (combined
), the cost level increased significantly by about 390.32 yuan at the time of the reform (combined  ,
,  ), and it showed a decreasing trend after the reform, with an average decrease of 9.53 yuan per month (
), and it showed a decreasing trend after the reform, with an average decrease of 9.53 yuan per month ( =–9.53, P < 0.05). The detailed results are shown in Table 4 and Figure 4.
=–9.53, P < 0.05). The detailed results are shown in Table 4 and Figure 4.
 |
Table 4 Results of Two-Group ITS Regression of the Treatment Costs Before and After DRG Reform |
 |
Figure 4 Changes in Chinese medical treatment and Western medical treatment costs before and after DRG reform for stroke patients. |
Discussion
Building on existing research, this study not only empirically demonstrates that the DRG reform in TCM hospitals reduces hospitalization costs and LOS for stroke patients but also elucidates the underlying factors contributing to these reductions. As the first tertiary TCM hospital in western China to implement the DRG payment reform, this study offers valuable insights for refining DRG payment strategies in the management of stroke diseases within the broader context of health insurance reform.
Descriptive statistics revealed that before the reform, more than 90% of stroke patients in the pilot TCM hospitals used TCM diagnostic and treatment equipment, TCM diagnostic and treatment techniques, and diagnostic and treatment methods on the basis of TCM evidence. The number of patients who used TCM diagnostic and treatment techniques and diagnostic and treatment methods on the basis of TCM evidence in the pilot TCM hospitals increased significantly after the DRG reform. As a late-onset disease, the average age of stroke patients changed from 68 to 70 years after DRG reform, and the age structure increased. DRG reform increased the attractiveness of TCM hospitals to ischemic stroke patients because of the more pronounced effect of TCM therapies on ischemic stroke.28–30
The single-group ITS analysis demonstrated that the DRG reform effectively reversed the long-term upward trend in inpatient costs for stroke patients in TCM hospitals, resulting in reduced hospitalization costs and shorter LOS. These outcomes underscore the significant impact of the reform. In particular, the instantaneous change in hospitalization costs was not significant at the time of policy implementation, but the increasing trend was reversed thereafter, showing a month-by-month decreasing trend. This may be due to the lag effect of the policy intervention, which is consistent with the findings of Zhu et al.31 Some scholars argue that DRG policies typically require sustained intervention, often necessitating a transition period during which the full effects of the reform may be delayed.1 Furthermore, the continuous decline in hospital days for stroke patients following the DRG reform suggests that the pilot TCM hospitals successfully reduced hospitalization durations by optimizing TCM diagnostic and treatment pathways, expediting patients’ functional recovery, and accelerating the overall rehabilitation process.
To further elucidate the factors contributing to the decline in hospitalization costs and LOS among stroke patients, the first two-group ITS analysis revealed that, within the treatment cost category, Western medical treatment costs exhibited a downward trend following the DRG reform. Additionally, acupuncture and massage treatment costs initially experienced a significant short-term increase, followed by a gradual decline. Both trends were statistically significant. The second two-group ITS equation demonstrated that in the drug cost group, Western medicine costs decreased significantly, and Chinese medicine costs increased slightly, although this change did not reach statistical significance. This suggests that the DRG reform has created effective incentives for healthcare providers. TCM hospitals have reduced Western medicine costs and Western medical treatment costs and increased the costs of Chinese medicines and acupuncture and massage treatments to control inpatient costs. Compared with Western hospitals, when treating stroke patients, TCM hospitals not only provide medication choices such as Chinese herbal tonics to activate blood circulation and remove blood stasis, dissolve phlegm and clear collaterals, and benefit qi and blood, as well as proprietary Chinese medicine injections but also equip them with a wide range of Chinese medicine equipment that is easy to operate, low cost and has remarkable curative effects.32,33 For example, meridians guide leveling therapeutic instruments, transcranial magnetic stimulation instruments, intermediate frequency electrotherapy instruments, Chinese medicine directional drug penetration therapeutic instruments, and acupuncture therapeutic equipment.34,35 These devices further enhance the effectiveness and cost-efficiency of TCM treatments. Several studies have indicated that integrating TCM in the treatment of circulatory system diseases, such as cerebral infarction, is more economical. Specifically, the hospitalization costs for patients not utilizing TCM were reported to be nearly twice as high as those for patients receiving TCM, a finding that aligns with the results of this study.36 In addition, as the DRG reform sets payment standards for each disease type, with overspending borne by hospitals and surpluses allocated to hospitals, hospitals need to control costs to generate more profit. The TCM hospitals prioritize the use of nonpharmacological therapies such as acupuncture, tuina, and moxibustion, which are less costly. These techniques, which depend on physicians’ clinical expertise rather than costly equipment, align with the TCM principles of “simplicity, convenience, affordability, and verifiability”.37 They not only contribute to controlling overall hospitalization costs but also maintain therapeutic efficacy. This illustrates how TCM hospitals, within the DRG framework, leverage their distinctive resources and technical strengths to achieve a dual objective of cost containment and improved service quality. Such dynamics further account for the observed reduction in hospitalization costs among stroke patients.
Limitations
Although this study has several limitations in exploring the impact of DRG reform policies on the hospitalization costs of stroke patients in western China, it provides some insights. Given that stroke patients in a pilot TCM hospital from January 2017 to June 2022 were selected as the study population, the number of study cases and time were limited. Future research could strengthen the robustness of findings by expanding the sample size and incorporating greater regional diversity. This study primarily examined the quantitative changes in Chinese and Western medicine costs, as well as treatment costs, in the hospitalization costs of stroke patients before and after the DRG reform. However, it did not explore the causal relationship between the use of Chinese medicines and the observed reduction in hospitalization costs—a gap that will be addressed in future investigations. Lastly, while this study sought to interpret specific cost changes from the perspective of TCM, it is important to note that the implementation of DRG systems in TCM hospitals remains in its early stages. Continued attention to major reforms in this area will be essential for providing a more comprehensive understanding of the impact of DRG policy changes.
Conclusion
DRG reform has prompted TCM hospitals to prioritize the use of lower-cost nonpharmacological therapies such as acupuncture, tuina, and TCM prescriptions as complementary to conventional treatment. The application of TCM therapies, capitalizing on their inherent advantages of “simplicity, convenience, affordability, and effectiveness” in stroke treatment, has contributed to a restructuring of hospitalization cost components. This shift has effectively curbed the rapid escalation of hospitalization costs for stroke patients, resulting in reduced costs and shorter hospital stays. Moving forward, it is essential to further enhance the value contribution of TCM within the DRG framework by refining the grouping and payment mechanisms to better reflect the distinct characteristics of TCM. For stroke patients across various subgroups, standardized clinical pathways and integrated treatment protocols combining Chinese and Western medicine should be developed to fully leverage TCM’s cost-efficiency and therapeutic potential in managing chronic conditions such as stroke.
Data Sharing Statement
The datasets utilized in this study are not currently available to the public due to internal hospital policies and confidentiality agreement restrictions. However, the data can be accessed from the corresponding author upon reasonable request for the purpose of study reproducibility.
Ethics Approval and Informed Consent
This study was approved by the Beijing University of Chinese Medicine Ethics Committee (BUCM-1002600). It utilized retrospective data for evaluation, ensuring no physical harm to the patients involved and avoiding any involvement with personal privacy or commercial interests. All patient information mentioned in this paper has been anonymized, excluding names and other sensitive or identifiable personal details. According to Article 32 of the Notice on the Issuance of Ethical Review Measures for Human Life Sciences and Medical Research issued by the National Health Commission of China and other departments on February 18, 2023, Ethical review may be exempted for life sciences and medical research involving human subjects that use human information data or biological samples, provided that no harm is caused to the human body and no sensitive personal information or commercial interests are involved. This exemption aims to reduce unnecessary burdens on researchers and promote the conduct of life sciences and medical research involving human subjects. The document also specifies that ethical review may be exempted from research using anonymized information data. Therefore, after deliberation by the Ethics Committee of Beijing University of Chinese Medicine, this study has been approved for conduct, and patient informed consent may be exempted. Our study complies with the Declaration of Helsinki.
Acknowledgments
The authors sincerely thank the Gansu Provincial Health and Wellness Commission for data support.
Funding
This study was supported by the General project of the Education Department of Gansu Province, China (Grant No. 2025CXZX-951).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wu Y, Han X, Qiu J. Impacts of the zero-markup drug policy on hospitalization expenses of patients with stroke in Western China: an interrupted time series analysis. Risk Manag Healthc Policy. 2024;Volume 17:777–788. doi:10.2147/RMHP.S456977
2. Wang L, Peng B, Zhang H, et al. Brief report on stroke prevention and treatment in China, 2020. Chin J Cerebrovasc Dis. 2022;19(02):136–144.
3. Rodgers H, Bosomworth H, Krebs HI, et al. Robot assisted training for the upper limb after stroke (RATULS): a multicentre randomised controlled trial. Lancet. 2019;394(10192):51–62. doi:10.1016/S0140-6736(19)31055-4
4. Feigin VL, Stark BA, Johnson CO, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 2021;20(10):795–820. doi:10.1016/S1474-4422(21)00252-0
5. Feigin VL, Brainin M, Norrving B, et al. World Stroke Organization (WSO): global stroke fact sheet 2022. Int J Stroke. 2022;17(1):18–29. doi:10.1177/17474930211065917
6. Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2019;394(10204):1145–1158. doi:10.1016/S0140-6736(19)30427-1
7. Hu D, Dong J, Zhu J, et al. Analysis of the Composition and Influencing Factors of Hospitalization Costs for Cerebral Infarction in a Tertiary Hospital, 2007-2011. Chin J Health Statistics. 2014;31(4):707–709.
8. Chen B, Jin W. A comprehensive review of stroke-related signaling pathways and treatment in western medicine and traditional Chinese medicine. Front Neurosci. 2023;17:1200061. doi:10.3389/fnins.2023.1200061
9. Safouris A, Magoufis G, Tsivgoulis G. Emerging agents for the treatment and prevention of stroke: progress in clinical trials. Expert Opin Investig Drugs. 2021;30(10):1025–1035. doi:10.1080/13543784.2021.1985463
10. Yang L, Qian J, Yang B, He Q, Wang J, Weng Q. Challenges and improvements of novel therapies for ischemic stroke. Front Pharmacol. 2021;12:721156. doi:10.3389/fphar.2021.721156
11. Wu Q, Yan R, Sun J. Probing the drug delivery strategies in ischemic stroke therapy. Drug Deliv. 2020;27(1):1644–1655. doi:10.1080/10717544.2020.1850918
12. Chang -C-C, Chen T-L, Chiu HE, et al. Outcomes after stroke in patients receiving adjuvant therapy with traditional Chinese medicine: a nationwide matched interventional cohort study. J Ethnopharmacol. 2016;177:46–52. doi:10.1016/j.jep.2015.11.028
13. Zhang H, Jin B, You X, et al. Pharmacodynamic advantages and characteristics of traditional Chinese medicine in prevention and treatment of ischemic stroke. Chin Herbal Med. 2023;15(4):496–508. doi:10.1016/j.chmed.2023.09.003
14. Su Q, Wang L, Yu H, Li H, Zou D, Ni X. Chinese herbal medicine and acupuncture for insomnia in stroke patients: a systematic review and meta-analysis of randomised controlled trials. Sleep Med. 2024;120:65–84. doi:10.1016/j.sleep.2024.05.006
15. Chen W-S, Hsu H-C, Chuang Y-W, et al. Predictors for the use of traditional Chinese medicine among inpatients with first-time stroke: a population-based study. BMC Complement Med Ther. 2020;20:1–12. doi:10.1186/s12906-020-03037-9
16. National Healthcare Security Administration. Notice regarding the publication of the list of national pilot cities for DRG payment. June 5, 2019. Available from: https://www.nhsa.gov.cn/art/2019/6/5/art_37_1362.html.
17. Qian M, Zhang X, Chen Y, Xu S, Ying X. The pilot of a new patient classification-based payment system in China: the impact on costs, length of stay and quality. Soc Sci Med. 2021;289:114415. doi:10.1016/j.socscimed.2021.114415
18. Linden A, Adams JL. Applying a propensity score-based weighting model to interrupted time series data: improving causal inference in programme evaluation. J Eval Clin Pract. 2011;17(6):1231–1238. doi:10.1111/j.1365-2753.2010.01504.x
19. Li L, Cuerden MS, Liu B, Shariff S, Jain AK, Mazumdar M. Three statistical approaches for assessment of intervention effects: a primer for practitioners. Risk Manag Healthc Policy. 2021;2021:757–770. doi:10.2147/RMHP.S275831
20. Taljaard M, McKenzie JE, Ramsay CR, Grimshaw JM. The use of segmented regression in analysing interrupted time series studies: an example in pre-hospital ambulance care. Implement Sci. 2014;9:1–4. doi:10.1186/1748-5908-9-77
21. Nistal-Nuño B. Segmented regression analysis of interrupted time series data to assess outcomes of a South American road traffic alcohol policy change. Public Health. 2017;150:51–59. doi:10.1016/j.puhe.2017.04.025
22. Jandoc R, Burden AM, Mamdani M, Lévesque LE, Cadarette SM. Interrupted time series analysis in drug utilization research is increasing: systematic review and recommendations. J Clin Epidemiol. 2015;68(8):950–956. doi:10.1016/j.jclinepi.2014.12.018
23. Sun J, Huang J, Liu H, Liang D, Luo Y. Research on the effect of the DRG payment reform on the structure of average hospitalization expenses in county public hospitals. Chin Hospital Manage. 2024;44(12):38–41.
24. Wang F, Tang S, Zhao K, Xiao Y, Li X. Applying interrupted time series to evaluate the effect of medicine price reform in a county-level public hospital. Chin J Health Statistics. 2016;33(01):78–80.
25. Linden A. A comprehensive set of postestimation measures to enrich interrupted time-series analysis. Stata J. 2017;17(1):73–88. doi:10.1177/1536867X1701700105
26. Baum C, Schaffer M. ACTEST: stata module to perform Cumby-Huizinga general test for autocorrelation in time series.
27. Linden A. Conducting interrupted time-series analysis for single-and multiple-group comparisons. Stata J. 2015;15(2):480–500. doi:10.1177/1536867X1501500208
28. Hao D-L, Li J-M, Xie R, et al. The role of traditional herbal medicine for ischemic stroke: from bench to clinic—A critical review. Phytomedicine. 2023;109:154609. doi:10.1016/j.phymed.2022.154609
29. J-g L, L-q W, X-y Y, et al. Chinese herbal medicine Dengzhan Xixin injection for acute ischemic stroke: a systematic review and meta-analysis of randomised controlled trials. Complement Ther Med. 2017;34:74–85. doi:10.1016/j.ctim.2017.08.004
30. Zhao A, Sun Q, Zhang J, et al. Substance basis and pharmacological mechanism of heat-clearing herbs in the treatment of ischaemic encephalopathy: a systematic review and network pharmacology. Ann Med. 2024;56(1):2308077. doi:10.1080/07853890.2024.2308077
31. Zhu Z, Wang J, Sun Y, Zhang J, Han P, Yang L. The impact of zero markup drug policy on patients’ healthcare utilization and expense: an interrupted time series study. Front Med Lausanne. 2022;9:928690. doi:10.3389/fmed.2022.928690
32. Fan G, Liu M, Liu J, Huang Y, Mu W. Traditional Chinese medicines treat ischemic stroke and their main bioactive constituents and mechanisms. Phytother Res. 2024;38(1):411–453. doi:10.1002/ptr.8033
33. Gong X, Sucher N. Stroke therapy in traditional Chinese medicine (TCM): prospects for drug discovery and development. Phytomedicine. 2002;9(5):478–484. doi:10.1078/09447110260571760
34. Li S. Study on the early curative effect of comprehensive rehabilitation technology combined with meridiantao therapy device in the treatment of hemiplegia after stroke. Chin Med Device Information. 2024;30(12):87–89. doi:10.15971/j.cnki.cmdi.2024.12.050
35. Wu Y. Advances in the clinical application and mechanism of action of repetitive transcranial magnetic stimulation in stroke rehabilitation. Chin J Rehabil Med. 2023;38(02):147–150.
36. Lu Y, Li L, Bian Y. How to reduce health expenses by using Traditional Chinese Medicine (TCM) Based on the analysis of inpatients’ TCM expenses and typical diseases in Ningxia Province. Chin J Health Policy. 2017;10(07):53–58. doi:10.15971/j.cnki.cmdi.2024.12.050
37. Fan X, Meng F, Wang D, et al. Correction to: perceptions of traditional Chinese medicine for chronic disease care and prevention: a cross-sectional study of Chinese hospital-based health care professionals. BMC Complement Altern Med. 2019;19(1):26. doi:10.1186/s12906-019-2434-7
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



