Back to Journals » International Journal of General Medicine » Volume 18
Impact of Intraoperative Dexamethasone on Postoperative Complications and Long-Term Survival in Patients with Non-Small Cell Lung Cancer: A retrospective Propensity Score-Matched Study
Authors Zhu W, Zhu L, Wang X, Tan H
Received 11 March 2025
Accepted for publication 17 June 2025
Published 24 June 2025 Volume 2025:18 Pages 3347—3361
DOI https://doi.org/10.2147/IJGM.S524652
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Ching-Hsien Chen
Wenzhi Zhu,1,* Liping Zhu,2,* Xiaoyi Wang,3 Hongyu Tan1
1Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Department of Anesthesiology, Peking University Cancer Hospital & Institute, Beijing, 100142, People’s Republic of China; 2Department of Hospice Care, Peking University Cancer Hospital (Inner Mongolia Campus), Inner Mongolia, 010010, People’s Republic of China; 3Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Department of Medical Record Statistics, Peking University Cancer Hospital& Institute, Beijing, 100142, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hongyu Tan, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Department of Anesthesiology, Peking University Cancer Hospital & Institute, No. 52 Fucheng Road, Haidian District, Beijing, 100142, People’s Republic of China, Tel +86-13693564036, Email [email protected]
Objective: This study investigated the impact of intraoperative dexamethasone on postoperative complications and long-term survival in patients with non-small cell lung cancer (NSCLC) undergoing surgery.
Methods: Patients with NSCLC who underwent lung resection between January 1, 2006, and December 31, 2009, were included. Patients receiving dexamethasone formed the dexamethasone (DXM) group, while those who did not were assigned to the non-dexamethasone (non-DXM) group. Propensity score matching (PSM) was applied to minimize confounding bias. The primary endpoint was the incidence of postoperative complications.
Results: Of the 579 patients included, 224 received intraoperative DXM, while 355 did not. PSM produced a matched cohort of 400 patients (200 in each group). After matching, the DXM group had significantly lower incidences of postoperative pneumonia (P < 0.05), reduced intensive care unit (ICU) ICU occupancy, and shorter postoperative hospital stays (PHS) compared with the non-DXM group (P < 0.05). No significant differences were observed in overall survival (OS) or recurrence-free survival (RFS) between the groups.
Conclusion: Intraoperative DXM use reduced the incidence of postoperative pneumonia, ICU occupancy, and PHS. However, no clear association was found between intraoperative DXM use and long-term survival outcomes in NSCLC patients.
Keywords: dexamethasone, postoperative complications, survival, NSCLC
Introduction
Lung cancer remains the second most prevalent and the deadliest type of cancer worldwide.1 In 2024, it is estimated that 234,580 new cases (116,310 in males and 118,270 in females) of lung and bronchial cancer will be diagnosed, with 125,070 deaths (65,790 males and 59,280 females).2 Clinically, non-small cell lung cancer (NSCLC) is the predominant pathological type of lung cancer and constitutes 85% of all cases.3 Despite significant advances in NSCLC treatment such as targeted therapy or immunotherapy over the past decade, surgical resection remains the cornerstone for curative treatment in early-stage cases.4 Understanding the prognosis of lung cancer following surgery is critical for guiding clinical decisions and optimizing patient management.5
Although the existing data-driven prognostic prediction models displayed the associations between perioperative management and the postoperative outcomes for NSCLC patients, concerns have been raised regarding the effects of certain intraoperative drugs, such as dexamethasone, on patient prognosis.6,7 Dexamethasone is a synthetic steroid widely used in clinical practice for its anti-allergic and anti-emetic properties as an anesthetic adjunct. While its efficacy in mitigating anesthesia-related complications is well documented, its role in NSCLC perioperative care remains unclear, particularly regarding the balance between anti-inflammatory benefits and immunosuppressive risks specific to oncologic outcomes. In our previous study, we also found that perioperative glucocorticoids were associated with the delayed recurrence in patients with lung cancer.8 However, unfortunately, we did not conduct in-depth analysis and discussion on this aspect. Therefore, the purpose of this study was to retrospectively analyze the relationship between intraoperative dexamethasone use and postoperative complications as well as long-term survival in NSCLC patients and investigate the potential prognostic implication of intraoperative dexamethasone use.
Methods
Study Population
This retrospective cohort with propensity score-matching was approved by the Institutional Review Board of Peking University Cancer Hospital & Institute, Beijing (approval No. 2019YJZ22-GZ02). The requirement for informed consent was waived thanks to the retrospective design. This study adhered to the Declaration of Helsinki (as revised in 2013). The electronic medical records system of Peking University Cancer Hospital was used to screen eligible patients who were diagnosed by pathological examination and underwent surgical resection for NSCLC from January 1, 2006, to December 31, 2009. Exclusion criteria included: (1) combined with other primary malignant tumors; (2) recurrent lung tumor; (3) incomplete follow-up data or missing information.
Anesthesia, Surgery, and Perioperative Management
General anesthesia with double-lumen endobronchial tube intubation was performed for all patients. Induction agents included propofol and opioids (fentanyl or sufentanil), while maintenance utilized inhalational anesthetics (sevoflurane or isoflurane) combined with opioids. Epidural anesthesia was applied in some cases, depending on anesthesiologist preferences. Lung resections were conducted via posterolateral thoracotomy, tailored to tumor characteristics and surgical requirements. Postoperative analgesia was administrated with patient-controlled pumps delivering ropivacaine (epidural) or sufentanil (intravenous) according to the analgesic protocol chosen.
Data Collection
Data collected included demographics [age, gender and body mass index (BMI)], preoperative information [comorbidity, lab test, American Society of Anesthesiologists classification (ASA), tumor-node-metastasis (TNM) stage, smoking and drinking history], intraoperative details (anesthesia technique, fluid intake, transfusion, DXM administration, surgical procedure, mediastinal lymph node dissection, surgery duration and estimated blood loss), and postoperative information (pathology, differentiation, tumor size, complications, chemotherapy and radiotherapy).
Follow-Up and Endpoints
All patients were followed up by specially assigned personnel through telephone inquiry or outpatient review. Patients were followed up every 6 months within the first postoperative year, then annually. Recurrence and death dates were recorded. The termination of follow-up was death, loss of follow-up or completed follow-up of 10 years.
The primary endpoint was postoperative complications defined as postoperative pulmonary complications (PPCs) (eg, pneumonia, pleural effusion, pneumothorax, pulmonary embolism, atelectasis and respiratory failure) and non-PPCs (eg, new-onset arrhythmia, myocardial ischemia, heart failure, cerebral infarction and deep venous thrombosis of lower extremity). All postoperative complications were diagnosed according to the Society of Thoracic Surgeons and European Society of Thoracic Surgeons joint definitions.9
The secondary endpoint included intensive care unit (ICU) occupancy, duration of drainage catheter indwelling, postoperative hospital stay (PHS) which was defined as the length of hospital stay after surgery, recurrence-free survival (RFS) which was defined as the duration in years from surgery to recurrence or death, whichever happened first, and overall survival (OS) which is defined as the duration in years from surgery to death from any cause.
Statistical Analysis
Continuous data were presented as mean (±SD) or median (interquartile range [IQR]) on the basis of normal or abnormal distribution. Categorical data are presented as number (%). Continuous variables were compared using the independent samples t-test or Mann–Whitney U-test. Categorical variables were analyzed using Pearson’s chi-squared test or Fisher’s exact test as appropriate.
A propensity score matching (PSM) approach was employed to account for potential confounding factors between the patients with intraoperative DXM (DXM group) and patients without intraoperative DXM (non-DXM group). Baseline characteristics and perioperative data were analyzed, including age, gender, BMI, ASA classification, comorbidities, history of smoking and drinking, preoperative lab test, preoperative chemotherapy, TNM stage, pathological type, differentiation grade, maximum tumor size, surgical procedure, mediastinal lymph node dissection, duration of surgery, anesthesia technique, estimated blood loss, blood transfusion, fluid intake, postoperative radiotherapy and chemotherapy. Patients were matched in a 1:1 ratio using the nearest-neighbor matching with caliper widths equal to 0.02 of the standard deviation of the logit of the propensity score.
Univariate analyses were performed by the Kaplan–Meier survival analysis with Log rank tests. Variables with a p-value <0.2 in the univariate analysis were included in the Cox proportional hazard model for multivariable analysis to identify the final predictors for RFS or OS. In terms of continuous variables, the cut-off points were chosen according to clinical significance, mean or median values.
All statistical analyses were performed using IBM Statistics SPSS Version 26 (SPSS, Inc, Chicago, IL). A 2-tailed P-value of <0.05 was considered significant.
Results
In total, 622 patients, undergoing NSCLC resection, were recruited in this study between January 1, 2006, and December 31, 2009. After review, 43 patients were excluded, including 10 combined with other primary malignant tumors, 6 with recurrent lung tumor, 8 combined with infectious diseases and respiratory infections and 19 with incomplete data (3 no TNM stage, 2 no differentiation grade and 14 lost to follow-up) (Figure 1). Therefore, 579 patients were included in the final analysis. Among these patients, 224 received intraoperative DXM and 335 did not. Before matching, there were significant variations in COPD, ASA grade, TNM stage, anesthesia technique between the two groups (Table 1), and after matching, there were no significant differences in demographic characteristics or perioperative data between the two groups (Table 1).
 |
Table 1 Baseline and Perioperative Characteristics Before and After Propensity Score-Matching |
 |
Figure 1 Flowchart of the study. Abbreviations: NSCLC, non-small cell lung cancer; DXM, dexamethasone. |
After PSM, there was no significant difference in overall postoperative complications between DXM group and non-DXM group (33.0% vs 30.5%, P = 0.591) (Table 2). The incidence of pneumonia, among major PPCs, was significantly lower in the DXM group than that in non-DXM group (3.5% vs 8.5%, P = 0.035), while the occurrences of other postoperative complications did not differ significantly between the two groups (P > 0.05) (Table 2). Compared with the non-DXM group, the DXM group had lower ICU occupancy (15.5% vs 23.5%, P = 0.043) and shorter PSH [12.0 (9.0–14.0) days vs 12.5 (10.0–15.0) days, P = 0.038] (Table 3).
 |
Table 2 Occurrences of Postoperative Complications Requiring Treatment During Hospital Stay |
 |
Table 3 Other Postoperative Outcomes and Long-Term Outcomes |
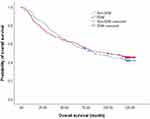
After matching, in the DXM group, the median duration of RFS was 63.4 months (IQR, 14.1–122.0), and the median duration of OS was 81.4 months (IQR, 26.4–122.2), and the 5-year RFS and OS rate were 50.9% (95% CI 44.0–57.9) and 61.5% (95% CI 54.7–68.2); in the non-DXM group, the median duration of RFS was 56.9 months (IQR, 13.9–121.6), and the median duration of OS was 78.4 months (IQR, 26.4–122.2), and the 5-year RFS and OS rate were 48.0% (95% CI 41.1–54.9) and 59.0% (95% CI 52.2–65.8), respectively (Tables 3 and 4).
 |
Table 4 The Survival Status of Patients After Surgery |
In the match cohort, 14 factors were included in multivariable Cox proportional hazard model for RFS, including 13 factors with P < 0.20 in univariable analyses and intraoperative DXM. Multivariable analysis identified 5 independent factors. Of them, preoperative Hemoglobin >136 g/L and mediastinal lymph node dissection were associated with delayed recurrence; postoperative complications, postoperative radiotherapy, and chemotherapy were associated with early recurrence (Tables 5 and 6). In the case of OS, after PSM, 13 factors were included in multivariable Cox proportional hazard model, including 12 factors with P <0.20 in univariable analyses and intraoperative DXM. Multivariable analysis identified 5 independent factors. Among them, preoperative Hemoglobin >136 g/L and mediastinal lymph node dissection were associated with prolonged survival; maximal tumor size >3.0cm, postoperative complications, postoperative radiotherapy and chemotherapy were associated with shortened survival (Tables 5 and 6).
 |
Table 5 Kaplan-Meier Univariable Analyses for Survival |
 |
Table 6 Multivariable Cox Proportional Hazard Model for Survival |
There were no significant differences in overall survival (OS) and recurrence-free survival (RFS) between the two groups. Intraoperative administration of dexamethasone was lack of association with RFS (HR, 0.789; 95% CI, 0.608–1.024; P = 0.075) and OS (HR, 0.885; 95% CI, 0.677–1.158; P = 0.374) (Table 6, Figures 2 and 3).
Discussion
Surgical trauma, including thoracic surgery, induces a stress response that leads to the activation of physiological responses, which promote wound healing and organ recovery, and participate in systemic inflammatory responses and angiogenesis10,11 In lung cancer surgery, systemic inflammation has two important aspects, namely, postoperative morbidity and control of tumor cell spread, which play a crucial role in postoperative tumor prognosis.12 Many factors, such as tissue injury, perioperative medications, and perioperative management (transfusion, fluid intake, and so forth), modulate the inflammatory response in lung cancer surgery.6 Prior study reported that glucocorticoids may attenuate surgical stress-induced inflammatory responses both directly by suppressing the release of proinflammatory cytokines and by inducing IL-10 synthesis.13 In this study, the intraoperative glucocorticoid used was dexamethasone, which was routinely administrated to prevent postoperative nausea and vomiting (PONV), usually at a dose of 5–10mg.
Postoperative complications are particularly common in patients with lung cancer, and the influence of postoperative complications after surgery is complicated.14 So far, postoperative complications have been reported to be associated with an exaggerated systemic inflammatory response following surgery.15 With regard to early postoperative complications, reduced levels and function of lymphocytes and NK cells can cause weakened cellular defense function, which may manifest in clinical practice as postoperative pneumonia, wound infection, or other inflammation.16 In the present matched cohort, there were no significant difference in total postoperative complications between the DXM group and non-DXM group. It seemed to imply a lack of connection between intraoperative dexamethasone and postoperative complications. However, in the matter of PPCs, the result showed the occurrence of postoperative pneumonia (POP) in the DXM group was lower than that in the non-DXM group (3.5% vs 8.5%, P = 0.035) and suggested that a low dose of dexamethasone during operation for prophylaxis of PONV might have the salutary effect on patients with NSCLC after surgery. According to previous studies, POP is one of prevalent postoperative inflammatory-related complications after lung cancer surgery, the incidence of which ranges from 2.1% to 40%.17,18 Dexamethasone is a synthetic glucocorticoid with potent anti-inflammatory effects in addition to its antiemesis.19 In a prospective double-blind trial, Corcoran et al found dexamethasone 4mg administered during surgery mitigate systematic inflammatory response after surgery, as detected using the C-reactive protein (CRP), which has been increasingly recognized as a reliable indicator of systemic inflammatory response and attenuated the changes in counts of all cells, apart from basophils and natural killer cells.20,21 Likewise, in another in-vivo experiment, Bain et al observed a significant decrease in classical monocytes, a major source of pro-inflammatory cytokines, within 2h of dexamethasone administration, and confirmed rapid effects of 8 mg dexamethasone on innate immune cells with the potential to alter the inflammatory response to surgery.22 To our best knowledge, no studies have specifically elucidated the effect of intraoperative dexamethasone on postoperative pneumonia after lung cancer. Based on our results, we speculated that the decrease in the occurrence of POP was partly attributed to the anti-inflammatory properties of dexamethasone in the DXM group. Moreover, POP has been reported to be associated with significant increases in intensive care unit stays, postoperative hospital stay, and hospitalization cost.23 In the current study, there were lower ICU occupancy (15.5% vs 23.5%, P = 0.043) and shorter PSH [12.0 days (IQR, 9.0–14.0) vs 12.5 days (IQR,10.0–15.0), P = 0.038] in the DXM group compared with the non-DXM group. We suspected that POP was responsible for these two outcomes in some degree. The reduced ICU occupancy and shortened PHS will greatly reduce the hospitalization cost and the financial burden of patients. It is of great clinical significance. Generally, postoperative complications after lung cancer resection remain a complicated challenge and mostly unpredictable. The link between intraoperative DXM use and POP deserves further study to develop more patient-friendly clinical management strategies.
Another concern of this study was the long-term survival status of patients with NSCLC. In the matched cohort, the median duration of RFS was 63.4 months (IQR, 14.1–122.0), and the median duration of OS was 81.4 months (IQR, 26.4–122.2) in the DXM group, while the median duration of RFS was 56.9 months (IQR, 13.9–121.6), and the median duration of OS was 78.4 months (IQR, 33.9–121.8) in the non-DXM group. Although there was a trend of prolonged RFS and OS in the DXM group, the difference was not significant between two groups after Kaplan–Meier analysis. Cox proportional hazard model revealed that intraoperative DXM was not the independent predictor for RFS (HR, 0.789; 95% CI, 0.608–1.024; P = 0.075) and OS (HR, 0.885; 95% CI, 0.677–1.158; P = 0.374). As far as the impact of corticosteroids on tumors are concerned, the available retrospective data have shown mixed results. Oliveira et al found there was no evidence for an association between perioperative systemic dexamethasone administration and ovarian cancer recurrence after primary cytoreductive surgery.24 Similarly, Newhook et al found intraoperative dexamethasone failed to confer any long-term survival benefit for patients with resected pancreatic ductal adenocarcinoma.25 Furthermore, Yu et al conducted a study on rectal cancer, indicating that patients who underwent radical surgical treatment gained a survival benefit by avoiding perioperative low-dose dexamethasone.26 The authors supposed that perioperative administration of dexamethasone might augment recurrence and mortality after tumor resection possibly by immunosuppression. On the contrary, a multicentric cohort study investigated the association between intraoperative dexamethasone and postoperative mortality in patients undergoing solid cancer resection and indicated dexamethasone decreased 1-year mortality and cancer recurrence.27 Another study by Zhang et al reported that perioperative use of low-dose glucocorticoids improved RFS in patients with pancreatic cancer and suggested dexamethasone may have prosurvival effects by its proapoptotic properties and suppress the perioperative stress response, which has detrimental effects on perioperative immune function and augments the risk of cancer recurrence.28 Nevertheless, in terms of lung cancer, Cata et al considered there was no association between dexamethasone and long-term survival after NSCLC surgery, in accord with our findings.29 Thus, the effects of DXM on long-term survival appear to vary by tumor type, but the potential mechanisms remain unclear and need to be further validated in prospective studies.
In the matched cohort, cox proportional hazards regression analysis showed preoperative Hemoglobin >136 g/L and mediastinal lymph node dissection improved RFS and OS. Hemoglobin represents the most widely utilized test parameter in clinical settings. Several studies have reported the prognostic value of hemoglobin level for cancers and demonstrated that higher pretreatment hemoglobin level is related with better long-term outcomes.30–32 Due to the heterogeneity of the study subjects, the preoperative hemoglobin levels analyzed were also different. Considering few patients with anemia due to adequate preoperative preparation in this study, the mean was chosen as the cutoff value for analyses. Our results are consistent with previous studies to some extent. As for mediastinal lymph node dissection, earlier studies have demonstrated that complete mediastinal lymph node dissection reduces the risk of postoperative recurrence and death,33,34 which is also reflected in our results.
In addition to the factors mentioned above for improving long-term prognosis, this study also found several adverse factors, including maximal tumor size >3.0cm, postoperative complications, postoperative radiotherapy and radiotherapy. A tumor size of 3cm in diameter has been regarded as the prognostic threshold in the staging of bronchogenic carcinoma since 1974, due to a significant survival difference between tumors ≤3 and >3 cm obtained on large databases by MD Anderson Cancer Center and Lung Cancer Study Group.35,36 Evidences from retrospective studies suggests tumor size ≤3cm was associated with a more favorable outcome in their patient population.36,37 In the present study, maximal tumor size >3.0cm was associated with prolonged OS (HR, 1.647; 95% CI, 1.252–2.166; P < 0.001). Recently, studies have shown that postoperative complications, including a severe inflammatory reaction, after various types of cancer surgery are associated with poor cancer-specific survival.38–40 The findings from Nojiri et al revealed that the presence of postoperative respiratory complications following lung cancer surgery was a significant predictor of cancer recurrence.38 Yamamichi et al reviewed data from 1129 patients with primary lung cancer and found postoperative complications are independent predictors of the overall and recurrence-free survival in lung cancer patients, especially advanced-stage cancer patients.39 Our results also showed that postoperative complications had a significant impact on postoperative outcomes and were associated with short RFS (HR, 1.341; 95% CI, 1.022–1.759; P = 0.034) and OS (HR, 1.336; 95% CI, 1.008–1.770; P = 0.044). In the postoperative complications, major infectious complications like pneumonia have been reported to be independent risk predictors of long-term survival in lung cancer patients.40 Therefore, in this sense, the patients who received DXM in this study had a lower incidence of postoperative pneumonia, indirectly indicating that intraoperative DXM use was beneficial to the long-term prognosis. Of note, in this cohort, postoperative radiotherapy and chemotherapy were associated with worsened outcomes. We considered that the possible reason was that the patients undergoing these therapies were at an advanced stage.
Limitation
There were several limitations in this study. First, it was a single-center, retrospective study, possibly resulting in unobserved confounding factors and selection bias. For example, there were variabilities in practices among surgeons from different institution. Furthermore, although PSM has balanced most measurable baseline variables, there may still be unmeasured confounding factors, such as anesthesiologists’ individualized decision-making preferences, tumor biological characteristics, and postoperative treatment regimens. Second, patients recruited in this study have undergone lung resection for more than 18 years. Some important clinical data such as preoperative lung function and intraoperative body temperature, which might have influence on the postoperative complications, have not been preserved, limited to the conditions during the cohort period. Therefore, the results of this cohort need to be interpreted with caution, and we will design prospective studies in the future to verify the findings. However, PSM was employed to balance the potential confounders and ensure the uniformity in perioperative characteristics.
Conclusion
In short, intraoperative use of dexamethasone decreased occurrence of postoperative pneumonia and ICU occupancy, and shortened the postoperative hospital stay in patients with NSCLC after lung resection. Given the frequency of administration of anti-emetic DXM to surgical patients, further prospective studies are needed to determine whether dexamethasone is associated with both short - and long-term outcomes.
Abbreviations
NSCLC, non-small cell lung cancer; DXM, dexamethasone; ICU, intensive care unit; PHS, postoperative hospital stay; OS, overall survival; RFS, recurrence-free survival; PONV, postoperative nausea and vomiting; PPCs, postoperative pulmonary complications; PSM, propensity score matching; BMI, body mass index; COPD, chronic obstructive pulmonary disease; ASA, American Society of Anesthesiologists; TNM, tumor-node-metastasis stage; WBC, white blood cell; PLT, platelets. CRP, C-reactive protein; POP, postoperative pneumonia.
Data Sharing Statement
The study datasets are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the Clinical Research Ethics Committee of the Peking University Cancer Hospital (Approval No.2019YJZ22-GZ02). The requirement for written informed consent was waived because of the study’s retrospective design.
Patient Confidentiality Statement
This retrospective study complies with institutional ethics and the Declaration of Helsinki. All patient-identifying information (names, hospital numbers, etc.) has been removed or anonymized in the manuscript and data. Presented data are aggregated to prevent individual identification. The Clinical Research Ethics Committee of the Peking University Cancer Hospital waived the informed consent requirement due to the study’s retrospective nature. This manuscript contains no information that compromises patient confidentiality. Authors are responsible for maintaining patient privacy.
Author Contributions
Wenzhi Zhu and Liping Zhu contributed equally and share first authorship. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hendriks LEL, Remon J, Faivre-Finn C, et al. Non-small-cell lung cancer. Nat Rev Dis Primers. 2024;10(1):71. doi:10.1038/s41572-024-00551-9
2. Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74(1):12–49. doi:10.3322/caac.21820
3. Miao D, Zhao J, Han Y, et al. Management of locally advanced non-small cell lung cancer: state of the art and future directions. Cancer Commun. 2024;44(1):23–46. doi:10.1002/cac2.12505
4. Roman M, Labbouz S, Valtzoglou V, et al. Lobectomy vs. segmentectomy. A propensity score matched comparison of outcomes. Eur J Surg Oncol. 2019;45(5):845–850. doi:10.1016/j.ejso.2018.10.534
5. Hu D, Li S, Huang Z, et al. Predicting postoperative non-small cell lung cancer prognosis via long short-term relational regularization. Artif Intell Med. 2020;107:101921. doi:10.1016/j.artmed.2020.101921
6. Choi H, Hwang W. Perioperative inflammatory response and cancer recurrence in lung cancer surgery: a narrative review. Front Surg. 2022;9:888630. doi:10.3389/fsurg.2022.888630
7. Huang WW, Zhu WZ, Mu DL, et al. Perioperative management may improve long-term survival in patients after lung cancer surgery: a retrospective cohort study. Anesth Analg. 2018;126(5):1666–1674. doi:10.1213/ANE.0000000000002886
8. Zhu W, Li S, Ji X, Tan H. Impact of anesthetic factors on prognosis of patients with non-small cell lung cancer after surgery. J Thorac Dis. 2023;15(9):4869–4884. doi:10.21037/jtd-22-1812
9. Seder CW, Salati M, Kozower BD, Cameron D, Pierre-Emmanuel F, Alessandro B. Variation in pulmonary resection practices between the society of thoracic surgeons and the European society of thoracic surgeons general thoracic surgery databases. Ann Thorac Surg. 2016;101(6):2077–2084. doi:10.1016/j.athoracsur.2015.12.073
10. Kinoshita T, Goto T. Links between inflammation and postoperative cancer recurrence. J Clin Med. 2021;10(2):228. doi:10.3390/jcm10020228
11. Zotova NV, Chereshnev VA, Gusev EY. Systemic inflammation: methodological approaches to identification of the common pathological process. PLoS One. 2016;11(5):e0155138. doi:10.1371/journal.pone.0155138
12. Takenaka K, Ogawa E, Wada H, et al. Systemic inflammatory response syndrome and surgical stress in thoracic surgery. J Crit Care. 2006;21(1):48–53. doi:10.1016/j.jcrc.2005.07.001
13. Li XX, Yu L, Yang JN, et al. Efficacy of preoperative single-dose dexamethasone in preventing postoperative pulmonary complications following minimally invasive esophagectomy: a retrospective propensity score-matched study. Perioper Med. 2024;13(1):46. doi:10.1186/s13741-024-00407-6
14. Koike Y, Aokage K, Osame K, et al. Risk factors of severe postoperative complication in lung cancer patients with diabetes mellitus. Ann Thorac Cardiovasc Surg. 2024;30(1):24. doi:10.5761/atcs.oa.24-00018
15. McSorley TT, Dolan RD, Roxburgh CS, et al. Possible dose dependent effect of perioperative dexamethasone and laparoscopic surgery on the postoperative systemic inflammatory response and complications following surgery for colon cancer. Eur J Surg Oncol. 2019;45(9):1613–1618. doi:10.1016/j.ejso.2019.05.020
16. Furák J, Németh T, Lantos J, et al. Perioperative systemic inflammation in lung cancer surgery. Front Surg. 2022;9:883322. doi:10.3389/fsurg.2022.883322
17. Yao L, Luo J, Liu L, et al. Risk factors for postoperative pneumonia and prognosis in lung cancer patients after surgery: a retrospective study. Medicine. 2021;100(13):e25295. doi:10.1097/MD.0000000000025295
18. Lee JY, Jin SM, Lee CH, et al. Risk factors of postoperative pneumonia after lung cancer surgery. J Korean Med Sci. 2011;26(8):979–984. doi:10.3346/jkms.2011.26.8.979
19. Chen H, Wang Y, Jiang K, et al. The effect of perioperative dexamethasone on postoperative complications after pancreaticoduodenectomy: a multicenter randomized controlled trial. Ann Surg. 2024;280(2):222–228. doi:10.1097/SLA.0000000000006240
20. watt DG, Horgan PG, McMillan DC. Routine clinical markers of the magnitude of the systemic inflammatory response after elective operation: a systematic review. Surgery. 2015;157(2):362–380. doi:10.1016/j.surg.2014.09.009
21. Corcoran T, Paech M, Law D, et al. Intraoperative dexamethasone alters immune cell populations in patients undergoing elective laparoscopic gynecological surgery. Br J Anaesth. 2017;119(2):221–230. doi:10.1093/bja/aex154
22. Bain CR, Draxler DF, Taylo R, et al. The early in-vivo effects of a single anti-emetic dose of dexamethasone on innate immune cell gene expression and activation in healthy volunteers. Anaesthesia. 2018;73(8):955–966. doi:10.1111/anae.14306
23. Zhou J, Wu D, Zheng Q, Wang T. A clinical prediction model for postoperative pneumonia after lung cancer surgery. J Surg Res. 2023;284:62–69. doi:10.1016/j.jss.2022.11.021
24. De Oliveira GS Jr, McCarthy R, Turan A, et al. Is dexamethasone associated with recurrence of ovarian cancer? Anesth Analg. 2014;118(6):1213–1218. doi:10.1213/ANE.0b013e3182a5d656
25. Newhook TE, Soliz JM, Prakash LR, et al. Impact of intraoperative dexamethasone on surgical and oncologic outcomes for patients with resected pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2021;28(3):1563–1569. doi:10.1245/s10434-020-09013-4
26. Yu HC, Luo YX, Peng H, et al. Avoiding perioperative dexamethasone may improve the outcome of patients with rectal cancer. Eur J Surg Oncol. 2015;41(5):667–673. doi:10.1016/j.ejso.2015.01.034
27. Blank M, Katsiampoura A, Wachtendorf LJ, et al. Association between intraoperative dexamethasone and postoperative mortality in patients undergoing oncologic surgery: a multicentric cohort study. Ann Surg. 2023;278(1):e105–e114. doi:10.1097/SLA.0000000000005526
28. Zhang YX, Mu DL, Jin KM, et al. Perioperative glucocorticoids are associated with improved recurrence-free survival after pancreatic cancer surgery: a retrospective cohort study with propensity score-matching. Ther Clin Risk Manag. 2021;22(17):87–101. doi:10.2147/TCRM.S287572
29. Cata JP, Jones J, Sepesi B, et al. Lack of association between dexamethasone and long-term survival after non-small cell lung cancer surgery. J Cardiothorac Vasc Anesth. 2016;30(4):930–935. doi:10.1053/j.jvca.2016.01.004
30. Huang YQ, Wei SQ, Jiang N, et al. The prognostic impact of decreased pretreatment haemoglobin level on the survival of patients with lung cancer: a systematic review and meta-analysis. BMC Cancer. 2018;18(1):1235. doi:10.1186/s12885-018-5136-5
31. Zhang YH, YQ L, Lu H, et al. Development of a survival prognostic model for non-small cell lung cancer. Front Oncol. 2020;10:362. doi:10.3389/fonc.2020.00362
32. Shen XB, Zhang YX, Wang W, et al. The Hemoglobin, Albumin, Lymphocyte, And Platelet (halp) score in patients with small cell lung cancer before first-line treatment with etoposide and progression-free survival. Med Sci Monit. 2019;25:5630–5639. doi:10.12659/MSM.917968
33. Zhong W, Yang X, Bai J, et al. Complete mediastinal lymphadenectomy: the core component of the multidisciplinary therapy in resectable non-small cell lung cancer. Eur J Cardiothorac Surg. 2008;34(1):187–195. doi:10.1016/j.ejcts
34. Lardinois D, Suter H, Hakki H, et al. Morbidity, survival, and site of recurrence after mediastinal lymph-node dissection versus systematic sampling after complete resection for non-small cell lung cancer. Ann Thorac Surg. 2005;80(1):
35. López-Encuentra A, Duque-Medina JL, Rami-Porta R, et al. Staging in lung cancer: is 3 cm a prognostic threshold in pathologic stage I non-small cell lung cancer? A multicenter study of 1,020 patients. Chest. 2002;121(5):1515–1520. doi:10.1378/chest.121.5.1515
36. Christian C, Erica S, Morandi U, et al. The prognostic impact of tumor size in resected stage I non-small cell lung cancer: evidence for a two thresholds tumor diameters classification. Lung Cancer. 2006;54(2):185–191. doi:10.1016/j.lungcan.2006.08.003
37. Rena O, Oliaro A, Cavallo A, et al. Stage I non-small cell lung carcinoma: really an early stage? Eur J Cardiothorac Surg. 2002;21(3):514–519. doi:10.1016/s1010-7940(01)01153-8
38. Nojiri T, Hamasaki T, Inoue M, et al. The presence of respiratory complications following lung cancer surgery was a significant predictor of cancer recurrence. Ann Surg Oncol. 2017;24(4):1135–1142. doi:10.1245/s10434-016-5655-8
39. Yamamichi T, Ichinose J, Omura K, et al. Impact of postoperative complications on the long-term outcome in lung cancer surgery. Surg Today. 2022;52(9):1254–1261. doi:10.1007/s00595-022-02452-4
40. Lugg ST, Agostini PJ, Tikka T, et al. Long-term impact of developing a postoperative pulmonary complication after lung surgery. Thorax. 2016;71(2):171–176. doi:10.1136/thoraxjnl-2015-207697
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Establishment and Validation of a Predictive Nomogram for Postoperative Survival of Stage I Non-Small Cell Lung Cancer
Wang ZH, Deng L
International Journal of General Medicine 2022, 15:7287-7298
Published Date: 14 September 2022
Overweight and Obesity are Associated with Poorer Survival Among Patients with Advanced Non-Small Cell Lung Cancer Receiving Platinum-Based Chemotherapy
Sutandyo N, Hanafi AR, Jayusman AM, Kurniawati SA, Hanif MA
International Journal of General Medicine 2023, 16:85-93
Published Date: 6 January 2023
Prognostic Value of miR-10a-3p in Non-Small Cell Lung Cancer Patients
Simiene J, Kunigenas L, Prokarenkaite R, Dabkeviciene D, Strainiene E, Stankevicius V, Cicenas S, Suziedelis K
OncoTargets and Therapy 2024, 17:1017-1032
Published Date: 14 November 2024