Back to Journals » Journal of Inflammation Research » Volume 17
Improved Fatigue Management in Primary Sjögren’s Syndrome: A Retrospective Analysis of the Efficacy of Methotrexate in Chinese Patients
Received 25 June 2024
Accepted for publication 17 October 2024
Published 21 October 2024 Volume 2024:17 Pages 7551—7560
DOI https://doi.org/10.2147/JIR.S475605
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Meiju Zhou, Xiaona Dai, Fang Yuan
Department of Rheumatology and Immunology, Zhejiang Hospital, Hangzhou, People’s Republic of China
Correspondence: Fang Yuan, Department of Rheumatology and Immunology, Zhejiang Hospital, No. 1229 Gudun Road, Hangzhou, 310030, People’s Republic of China, Email [email protected]
Objective: To assess the efficacy of methotrexate (MTX) and hydroxychloroquine (HCQ) in improving fatigue symptoms in patients with primary Sjögren’s syndrome (pSS).
Methods: A single-center retrospective study was conducted on pSS patients experiencing fatigue symptoms. All patients received either MTX, HCQ, or a combination of MTX + HCQ for a period of six months. Clinical efficacy was measured using the European League Against Rheumatism (EULAR) Sjögren’s Syndrome Disease Activity Index (ESSDAI), EULAR Sjögren’s Syndrome Patient Reported Index (ESSPRI), Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F), fatigue severity scale (FSS), and visual analog scale (VAS) score. These measures were assessed at baseline and at 1, 2, 3, and 6 months.
Results: A total of 86 pSS patients with fatigue symptoms were enrolled (27 received MTX, 29 received HCQ, and 30 received MTX + HCQ). Patients receiving MTX and MTX + HCQ showed significant improvements at 6th month in ESSDAI, ESSPRI, FSS, FACIT-F, and VAS scores (all P < 0.01) compared with baseline. Repeated-measures analysis of variance revealed that patients treated with MTX and MTX + HCQ experienced significant improvements in ESSDAI, FSS, FACIT-F, and VAS scores (all P < 0.01) from baseline to the 6th month. The HCQ group did not show significant improvement in FSS, FACIT-F, and VAS scores (all P > 0.05), although their ESSDAI and ESSPRI scores did improve significantly (all P < 0.01). Patients in the MTX group showed the most improvement in mean changes of ESSDAI score, FSS score, FACIT-F score, and VAS score from baseline to the 6th month. And patients received MTX treatment significantly had more fatigue remission numbers (all P < 0.05).
Conclusion: In clinical practice, methotrexate is more effective than hydroxychloroquine in improving fatigue symptoms, as measured by patient-reported fatigue scales (FSS, FACIT-F, and VAS scores) in patients with pSS.
Keywords: primary Sjögren’s syndrome, fatigue, methotrexate, hydroxychloroquine
Introduction
Primary Sjögren’s syndrome (pSS) is a multisystemic autoimmune disease, second only to rheumatoid arthritis in frequency.1 Typical symptoms of pSS include oral and ocular dryness, fatigue, and pain. These symptoms are characterized by hypofunction of the salivary and lacrimal glands, and possible systemic multi-organ manifestations that primarily affect women.2,3 Current evidence suggests that approximately 75% of pSS patients produce autoantibodies of the Sjögren’s Syndrome A (SSA/Ro) and -B (SSB/La) type.4 The majority of pSS patients experience persistent pain, fatigue, and ocular and/or oral dryness.5
Fatigue is a complex and disabling symptom affecting between 22 and 30% of the general population, resulting in reduced quality of life.6 Nearly 70% of patients with pSS report profound, debilitating fatigue as the single symptom with the most significant negative impact on their quality of life.7 The prevalence of fatigue in pSS patients is reported to range from 67%8 to 85%.9 It is now understood that pSS-related fatigue differs from general fatigue in that it is constant, unrelenting, and volatile. Patients with pSS describe fatigue as “an ever-present, fluctuating, and non-relievable lack of vitality beyond one’s own control”.10 This symptom is reported as the most challenging to manage.11 This underscores the importance of identifying effective treatment strategies to improve fatigue in patients with pSS.12
However, the mechanisms that lead to and regulate fatigue are debated. The etiology of fatigue is very complex and unclear, and may be multifactorial, including biological and psychosocial elements contributing to the perception of fatigue. Fatigue symptoms are frequently observed in immune-mediated inflammatory conditions and consistently follow autoimmune diseases, tumors, and infections. This is part of a constellation of symptoms termed “sickness behavior”.6,13 As reported by S.V. Arnett et al, proinflammatory cytokines may play a critical role as the biological basis of fatigue.13 Evidence suggests that genetic and molecular mechanisms are activated during inflammation and cellular stress conditions, and signaled via neuro-immune and oxidative / nitrosative stress pathways.14
Currently, treatment for pSS focuses on relieving symptoms and altering the course of the disease. For glandular symptoms, artificial tears are reasonably effective for xerophthalmia. However, symptomatic treatments like sprays, lozenges, pastilles, and artificial saliva have limited efficacy in relieving xerostomia.15 Similarly, glucocorticoids and immunosuppressants, such as methotrexate (MTX), leflunomide (LEF), and hydroxychloroquine (HCQ), as well as biological agents, have not been shown to improve dryness symptoms in patients with pSS.2,16,17 Evidence supporting the use of disease-modifying anti-rheumatic drugs for pSS is also limited.
Otherwise, pain, depression, and daytime sleepiness scores were closely associated with both physical and mental fatigue in pSS patients, which was observed even after adjustment for comorbidities associated with fatigue or medications associated with drowsiness.18
While immunosuppressants like MTX, cyclophosphamide, corticosteroids, and others are often used to manage organ involvement in Sjögren’s syndrome, they can also be effective in addressing extra-glandular manifestations of the disease. However, their use comes with some uncertainty regarding efficacy and the potential for adverse effects.19
There is currently no effective treatment for fatigue symptoms in pSS. While evidence from small, uncontrolled, open-label studies suggests rituximab may improve patient-reported dryness, pain, fatigue, global assessment, stimulated salivary flow, and physician global assessment,20–22 a larger, multicenter, randomized, double-blind, placebo-controlled trial by Simon J Bowman et al found rituximab to be ineffective in pSS patients.2
However, no large, systemic, randomized controlled studies have been conducted on the effect of MTX on fatigue in pSS patients. Previous study showed improvement of MTX for the main subjective symptoms (dry mouth and eyes) as well as in the frequency of parotid gland enlargement, dry cough and purpura, however, no improvement in the objective parameters of dry eyes and dry mouth were observed. But regrettably, fatigue symptom was not observed.16
Systematic review showed that there is no significant difference between HCQ and placebo in the treatment of dry mouth, dry eye, and fatigue in pSS, and the effectiveness of HCQ was lower than placebo.23
This single-center, retrospective clinical study aimed to evaluate the efficacy of MTX in improving fatigue symptoms in pSS patients. All participants were diagnosed with pSS.
Method
Inclusion and Exclusion Criteria
Participants were enrolled from the Department of Rheumatology and Immunology, Zhejiang Hospital between January 2019 and December 2023.
Inclusion criteria: All patients fulfilled the 2016 classification criteria for pSS,24 and were followed up for at least 6 months. During the follow-up period, none of the patients received corticosteroids or immunosuppressants other than methotrexate and hydroxychloroquine.
Exclusion criteria: We excluded patients with a history of other rheumatic diseases, tumors, infectious diseases, malnutrition, chronic kidney disease, graft-versus-host disease, head or neck radiation therapy, or psychiatric disorders.
Study Design
Patients
All patients received MTX or HCQ treatment for at least 6 months, and oral MTX 10 mg/week, oral HCQ 400 mg/day. Efficacy endpoints were assessed at 6 months. Efficacy and safety were evaluated at baseline and at 1, 2, 3, and 6 months. Demographic, clinical, and laboratory data were collected from the electronic hospital information system. The study was approved by the Ethics Committee of Zhejiang Hospital (2020101K) and followed the tenets of the Declaration of Helsinki. Written informed consent was obtained from all subjects before participation in the study.
Efficacy Evaluations
Clinical efficacy measures included the European League Against Rheumatism (EULAR) Sjögren’s Syndrome Disease Activity Index (ESSDAI),25 EULAR Sjögren’s Syndrome Patient Reported Index (ESSPRI),26 Functional Assessment of Chronic Illness Therapy–Fatigue (FACIT-F),27 fatigue severity scale (FSS),28 and visual analog scale (VAS).29 The ESSDAI scores were assessed by rheumatologists, and ESSPRI scores, FACIT-F scores, FSS scores, VAS scores were conducted by patients.
Statistical Analysis
Data were analyzed using SPSS version 23.0 for Windows. All analyses were two-sided, with P < 0.05 considered statistically significant. Continuous variables were presented as mean ± standard deviation (SD). One-way analysis of variance (ANOVA) with Scheffé or LSD post-hoc tests were used to evaluate differences between groups for continuous variables. Repeated-measures ANOVA was used for within-group comparisons over time. Qualitative variables were expressed as frequencies (%). The chi-square test with Bonferroni correction was used to evaluate the significance of associations between categorical variables.
Results
Participant Characteristics
A total of 114 patients were assessed for eligibility. After screening clinical information and follow-up, 28 patients were excluded. Two patients were ineligible due to discontinued treatment, and 20 patients were lost to follow-up. One patient was diagnosed with a tumor, one with chronic kidney disease, and four developed infections. Therefore, 86 patients were included in the final analysis. The patient selection process of this study is shown in Figure 1.
 |
Figure 1 Flow diagram depicting the selection process of study participants. |
Table 1 presents the baseline characteristics of the 86 pSS patients. Among these patients, 27 (31.4%) received MTX, 29 (33.7%) received HCQ, and 30 (34.9%) received both MTX and HCQ. There were no significant differences in gender, age, ESSDAI score, ESSPRI score, FSS score, FACIT-F score, VAS score, or presence of extra-glandular involvement between the MTX, HCQ, and MTX + HCQ groups at baseline (all P > 0.05).
 |
Table 1 Baseline Characteristics of Subjects |
Table 2 shows the serological parameters of pSS patients at baseline. There were significant differences in the proportions of patients with hyper-immunoglobulin G (IgG), hypocomplementemia C3, hypocomplementemia C4, leukopenia, anemia, and thrombocytopenia among the three groups at baseline (all P < 0.01). Interestingly, ANOVA analysis revealed significant differences in the levels of IgG, complement C3, complement C4, white blood cells, hemoglobin, and platelets among the three groups (all P < 0.05). However, no significant differences were found in autoantibodies among the three groups at baseline (all P > 0.05).
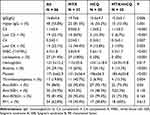 |
Table 2 Baseline Serological Parameters of pSS Patients |
Clinical Efficacy Measures
A repeated-measures ANOVA analysis was conducted to assess the differences in outcomes among the MTX, HCQ, and MTX + HCQ groups from baseline to the 6th month. The MTX and MTX + HCQ groups showed significant improvements of ESSDAI score, FSS score, FACIT-F score and VAS score from baseline to the 6th month (all P < 0.05). In contrast, the HCQ group did not exhibit significant improvement during the follow-up period (baseline to 6th month) (P > 0.05) (Figure 2).
The ESSDAI score (5.1 ± 1.0, 4.6 ± 1.0, 4.8 ± 0.8 vs 0.9 ± 0.9, 2.4 ± 1.2, 1.2 ± 0.8, respectively; P < 0.01), ESSPRI score (6.6 ± 1.2, 6.5 ± 1.1, 6.4 ± 1.3 vs 3.5 ± 1.0, 4.0 ± 1.0, 3.9 ± 1.4, respectively; P < 0.01), FSS score (46.2 ± 9.2, 42.3 ± 4.7, 44.1 ± 7.9 vs 31.6 ± 6.6, 43.9 ± 4.2, 35.4 ± 5.7, respectively; P < 0.01), FACIT-F score (25.7 ± 4.6, 26.8 ± 2.5, 25.0 ± 4.6 vs 38.9 ± 5.1, 28.7 ± 5.7, 35.2 ± 6.6, respectively; P < 0.01), and VAS score (3.5 ± 1.1, 3.4 ± 0.9, 3.5 ± 0.9 vs 1.2 ± 0.9, 3.1 ± 1.1, 2.2 ± 1.0, respectively; P < 0.01) all showed significant improvement for the MTX, HCQ, and MTX + HCQ groups from baseline to the 6th month Scores in the MTX group showed the most significant improvement, while the HCQ group showed the least (Figure 3).
Several patient-reported outcome instruments were used in the study to assess changes in fatigue and disease activity. Patients in the MTX group showed the most improvement in mean changes of ESSDAI score, FSS score, FACIT-F score, and VAS score from baseline to the 6th month (Figure 4). However, there was no significant difference in ESSPRI scores across the three groups (Table 3).
 |
Table 3 Clinical Efficacy Measures |
 |
Figure 4 Improvement of ESSDAI score (A), ESSPRI score (B), FSS score (C), FACIT-F score (D) and VAS score (E) of the MTX, HCQ and MTX+HCQ group. |
At 6 months, the MTX, HCQ, and MTX+HCQ groups showed significant differences in fatigue remission rates according to FSS score (63%, 3.4%, 13.3%, P < 0.01), FACIT-F score (96.3%, 13.8%, 24.8%, P < 0.01), and VAS score (25.6%, 3.4%, 30%, P = 0.04), respectively (Table 3).
Discussion
Fatigue is a complex and subjective experience, often described as a constant feeling of tiredness, lack of energy, endurance, or vitality that interferes with daily activities. The estimated prevalence of fatigue in pSS patients varies considerably, and there is a lack of standardized instruments specifically designed to measure fatigue in rheumatic diseases. Severe fatigue symptoms are present in 41% to 57% of patients with various inflammatory rheumatic diseases, including rheumatoid arthritis, systemic lupus erythematosus, ankylosing spondylitis, Sjögren’s syndrome, psoriatic arthritis, and scleroderma. Notably, severe fatigue is least prevalent in patients with osteoarthritis (35%) and most prevalent in patients with fibromyalgia (82%).30 Studies have identified depression, ESSDAI, and ESSPRI as independent risk factors for fatigue in pSS patients.31 Unfortunately, there is currently no specific and highly effective treatment to completely relieve fatigue symptoms in pSS patients. Based on our clinical experience, we designed this study to explore the efficacy of MTX and HCQ in managing fatigue symptoms in patients with pSS.
The purpose of this study is to evaluate the efficacy of MTX and HCQ for fatigue symptom in pSS patients. In this study, we enrolled 86 patients with pSS who were experiencing fatigue. We found that MTX was more effective than HCQ in improving fatigue symptoms. Hydroxychloroquine may still be considered in certain situations for managing fatigue in pSS. Some reports suggest that HCQ improves fatigue in about one-third of patients treated with the medication.32
Although, hydroxychloroquine is one of the most frequently prescribed DMARDs for fatigue symptom in pSS patients. However, evidence regarding its efficacy is limited. Previous study involving a significant number of randomized or non-randomized controlled experiments have reported hydroxychloroquine to exhibit placebo-like effects in the treatment of pSS.17 Nevertheless, we conducted this substantial workload study and similarly, we did not observe significant improvement in fatigue among patients receiving HCQ. While the overall quality of evidence is considered very low, some experts recommend considering HCQ for pSS patients with fatigue due to its favorable safety profile and established use in clinical practice.33
Otherwise, we found MTX presented compelling evidence for a robust therapeutic effect for fatigue in pSS patients, compared with hydroxychloroquine. But considering the potential confounding factors inherent in retrospective studies, the reliability of the conclusion warrants further scrutiny. On the other hand, possibly due to its relatively short duration, we could not get an accurate conclusion. MTX was already recommended for treating inflammatory musculoskeletal pain in pSS, but there was no existing evidence or recommendation for its use in managing fatigue.34
James Posada et al7 found that RSLV-132 improved severe fatigue in patients with pSS. This improvement was determined by independent patient-reported measures of fatigue, including the ESSPRI, FACIT-F, Profile of Fatigue (ProF), and Digit Symbol Substitution Test (DSST). They also found a significant correlation between this improvement and increased expression of selected interferon-inducible genes.7 In contrast, a multicenter, randomized, double-blind, placebo-controlled trial conducted by Simon J Bowman et al2 recruited 133 pSS patients with fatigue and found that Rituximab was neither clinically nor cost-effective for this patient population. However, a pilot RCT study by another group enrolled 17 pSS patients and reported a significant reduction in fatigue among those randomized to rituximab compared to placebo. This study did not find a significant difference in the proportion of patients achieving either a 20% or 30% reduction in fatigue from baseline at 6 months.35
It is widely thought that physicotherapeutics play an important role in managing fatigue. Jessica Tarn et al36 recruited 15 pSS patients who used a noninvasive vagus nerve stimulation device twice daily for a 26-day period. This study found a reduction in clinical symptoms of fatigue and sleepiness, suggesting that the vagus nerve may be involved in regulating fatigue and immune responses in pSS. However, a larger placebo-controlled follow-up study is required to confirm these findings. According to the Treatment Guidelines for Rheumatologic Manifestations of Sjögren’s Syndrome, experts recommend self-care measures and exercise advice as ways to reduce fatigue.33
Herein, we selected three fatigue scales that are currently or have recently been used in rheumatology populations and are considered easy for patients to complete. However, it is important to note that the FSS, developed by Krupp et al in 1989, was originally designed to evaluate fatigue in Parkinson’s disease and may not be entirely suitable for pSS patients,28 despite being simple and easy to understand. Additionally, while all three scales are patient-reported measures of fatigue, self-assessment may not always accurately reflect the true level of fatigue experienced. Due to the subjective of the several assessment scales, the results of the questionnaire may be not very accuracy.
The PROMIS (Patient Reported Outcomes Measurement Information System) scales are available in both a fixed short form as well as a computer-adaptive testing format and have shown robust psychometric properties, and the PROMIS fatigue instruments have been shown to be reliable, well correlated with, and responsive to change in rheumatoid arthritis disease activity.37,38 But there were not objective assessment tools available. More scientific approach needed to be used to evaluate fatigue severity and degree.
There are no established pharmacological treatment options for fatigue in pSS. So far, exercise and neuromodulation techniques have shown positive effects on fatigue in pSS.39 Patients with Sjögren’s syndrome may have complex comorbidities and be taking medications that contribute to fatigue. And MTX can cause fatigue symptom.40 These factors may account for a relatively small proportion of the variation observed in fatigue symptoms among the study participants.18
The biological mechanisms and pathology involved in pSS fatigue are still not fully understood. In terms of physiology, fatigue is multidimensional and associated with neurocognitive, neuroendocrine, environmental and behavioral components. Fatigue in pSS is multifactorial and clinically related to sleep, mood and physical, and psychological disorders.18 Additionally, pSS patients developed with low quality of sleep, and this may correlate with fatigue.41 Sleep quality definitely associated with fatigue symptom, and future studies could address whether such factors could be useful as surrogate markers for fatigue in pSS. But regrettably, in this study, we did not study the correlations between sleep, psychiatric disorders and fatigue.
Several limitations in this study should be acknowledged. First, the retrospective design relies on data obtained from medical records, which can be susceptible to recall bias. Second, a prospective long - time follow-up study with a larger sample size is required to confirm the findings. Finally, differences in education level among participants may have contributed to the heterogeneity observed in fatigue scores, as educational background can influence how patients understand and respond to assessment questions. Well-designed, randomized, controlled trials are needed to provide higher-quality evidence to confirm our findings, and future studies should focus on some extra-glandular measures, such as fatigue symptom to further explore the therapeutic effect of MTX in pSS.
Conclusion
This retrospective study investigated the efficacy of MTX in managing fatigue symptoms in patients with pSS. Utilizing a limited sample size, the study employed patient-reported fatigue measures to assess the comparative effects of MTX and HCQ. The findings demonstrate that MTX treatment resulted in significantly greater improvements in fatigue symptoms compared to HCQ, and it’s the first study to explore the efficacy of MTX and HCQ for fatigue in pSS patients.
Data Sharing Statement
All data generated or analyzed during this study are included in this article. For further information, please contact the corresponding author, Fang Yuan.
Ethics Approval and Consent to Participate
The study was approved by the Ethics Committee of Zhejiang Hospital (2020101K) and followed the tenets of the Declaration of Helsinki. Written informed consent was obtained from all subjects before participation in the study.
Acknowledgments
We thank all patients for their understanding and cooperation during this study and their contributions to the research. We acknowledge Zhejiang hospital for financial support for this study.
In addition, Meiju Zhou wants to thank Qizuan Chen, in particular, the patience, care and encouragement during the research.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception and design, data acquisition, or data analysis and interpretation, participated in the drafting of the article or critically revising it for important intellectual content, agreed to submit to the current journal, gave final approval for the version to be published, and agreed to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors have declared no conflicts of interest.
References
1. Fox RI, Stern M, Michelson P. Update in Sjögren syndrome. Curr Opin Rheumatol. 2000;12(5):391–398. doi:10.1097/00002281-200009000-00007
2. Bowman SJ, Everett CC, O’Dwyer JL, et al. Randomized controlled trial of rituximab and cost-effectiveness analysis in treating fatigue and oral dryness in primary Sjögren’s syndrome. Arthritis Rheumatol. 2017;69(7):1440–1450. doi:10.1002/art.40093
3. Zhou M, Yuan F. Hypocomplementemia in primary Sjögren’s syndrome: a retrospective study of 120 treatment-naive Chinese patients. Int J Gen Med. 2022;15:359–366. doi:10.2147/IJGM.S346188
4. Omdal R, Mellgren SI, Norheim KB. Pain and fatigue in primary Sjögren’s syndrome. Rheumatology. 2021;60(7):3099–3106. doi:10.1093/rheumatology/kez027
5. Seror R, Theander E, Brun JG, et al. Validation of EULAR primary Sjögren’s syndrome disease activity (ESSDAI) and patient indexes (ESSPRI). Ann Rheum Dis. 2015;74(5):859–866. doi:10.1136/annrheumdis-2013-204615
6. Davies K, Mirza K, Tarn J, et al. Fatigue in primary Sjögren’s syndrome (pSS) is associated with lower levels of proinflammatory cytokines: a validation study. Rheumatol Int. 2019;39(11):1867–1873. doi:10.1007/s00296-019-04354-0
7. Posada J, Valadkhan S, Burge D, et al. Improvement of severe fatigue following nuclease therapy in patients with primary Sjögren’s syndrome: a randomized clinical trial. Arthritis Rheumatol. 2021;73(1):143–150. doi:10.1002/art.41489
8. Segal B, Thomas W, Rogers T, et al. Prevalence, severity, and predictors of fatigue in subjects with primary Sjögren’s syndrome. Arthritis Rheum. 2008;59(12):1780–1787. doi:10.1002/art.24311
9. Mandl T, Jãrgensen TS, Skougaard M, et al. Work disability in newly diagnosed patients with primary Sjögren syndrome. J Rheumatol. 2017;44(2):209–215. doi:10.3899/jrheum.160932
10. Mengshoel AM, Norheim KB, Omdal R. Primary Sjögren’s syndrome: fatigue is an ever-present, fluctuating, and uncontrollable lack of energy. Arthritis Care Res. 2014;66(8):1227–1232. doi:10.1002/acr.22263
11. Pinto A, Piva SR, Vieira A, et al. Transcranial direct current stimulation for fatigue in patients with Sjögren’s syndrome: a randomized, double-blind pilot study. Brain Stimul. 2021;14(1):141–151. doi:10.1016/j.brs.2020.12.004
12. Hackett KL, Deane KHO, Newton JL, et al. Mixed-methods study identifying key intervention targets to improve participation in daily living activities in primary Sjögren’s syndrome patients. Arthritis Care Res. 2018;70(7):1064–1073. doi:10.1002/acr.23536
13. Arnett SV, Clark IA. Inflammatory fatigue and sickness behaviour - lessons for the diagnosis and management of chronic fatigue syndrome. J Affect Disord. 2012;141(2–3):130–142. doi:10.1016/j.jad.2012.04.004
14. Maes M. Inflammatory and oxidative and nitrosative stress pathways underpinning chronic fatigue, somatization and psychosomatic symptoms. Curr Opin Psychiatry. 2009;22(1):75–83. doi:10.1097/yco.0b013e32831a4728
15. Papas AS, Sherrer YS, Charney M, et al. Successful treatment of dry mouth and dry eye symptoms in Sjögren’s syndrome patients with oral pilocarpine: a randomized, placebo-controlled, dose-adjustment study. J Clin Rheumatol. 2004;10(4):169–177. doi:10.1097/01.rhu.0000135553.08057.21
16. Skopouli FN, Jagiello P, Tsifetaki N, et al. Methotrexate in primary Sjögren’s syndrome. Clin Exp Rheumatol. 1996;14(5):555–558.
17. Gottenberg JE, Ravaud P, Puéchal X, et al. Effects of hydroxychloroquine on symptomatic improvement in primary Sjögren syndrome: the JOQUER randomized clinical trial. JAMA. 2014;312(3):249–258. doi:10.1001/jama.2014.7682
18. Hackett KL, Davies K, Tarn J, et al. Pain and depression are associated with both physical and mental fatigue independently of comorbidities and medications in primary Sjögren’s syndrome. RMD Open. 2019;5(1):e000885. doi:10.1136/rmdopen-2018-000885
19. Liu X, Li X, Li X, et al. The efficacy and safety of total glucosides of peony in the treatment of primary Sjögren’s syndrome: a multi-center, randomized, double-blinded, placebo-controlled clinical trial. Clin Rheumatol. 2019;38(3):657–664. doi:10.1007/s10067-018-4315-8
20. Devauchelle-Pensec V, Pennec Y, Morvan J, et al. Improvement of Sjögren’s syndrome after two infusions of rituximab (anti-CD20). Arthritis Rheum. 2007;57(2):310–317. doi:10.1002/art.22536
21. Pijpe J, van Imhoff GW, Spijkervet FK, et al. Rituximab treatment in patients with primary Sjögren’s syndrome: an open-label phase II study. Arthritis Rheum. 2005;52(9):2740–2750. doi:10.1002/art.21260
22. St Clair EW, Levesque MC, Prak ET, et al. Rituximab therapy for primary Sjögren’s syndrome: an open-label clinical trial and mechanistic analysis. Arthritis Rheum Apr. 2013;65(4):1097–1106. doi:10.1002/art.37850
23. Wang SQ, Zhang LW, Wei P, et al. Is hydroxychloroquine effective in treating primary Sjögren’s syndrome: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2017;18(1):186. doi:10.1186/s12891-017-1543-z
24. Shiboski CH, Shiboski SC, Seror R, et al. 2016 American college of rheumatology/European league against rheumatism classification criteria for primary Sjögren’s syndrome: a consensus and data-driven methodology involving three international patient cohorts. Ann Rheum Dis Jan. 2017;76(1):9–16. doi:10.1136/annrheumdis-2016-210571
25. Seror R, Ravaud P, Bowman SJ, et al. EULAR Sjögren’s syndrome disease activity index: development of a consensus systemic disease activity index for primary Sjögren’s syndrome. Ann Rheum Dis. 2010;69(6):1103–1109. doi:10.1136/ard.2009.110619
26. Seror R, Ravaud P, Mariette X, et al. EULAR Sjögren’s syndrome patient reported index (ESSPRI): development of a consensus patient index for primary Sjögren’s syndrome. Ann Rheum Dis. 2011;70(6):968–972. doi:10.1136/ard.2010.143743
27. Cella D, Yount S, Sorensen M, et al. Validation of the functional assessment of chronic illness therapy fatigue scale relative to other instrumentation in patients with rheumatoid arthritis. J Rheumatol. 2005;32(5):811–819.
28. Krupp LB, LaRocca NG, Muir-Nash J, et al. The fatigue severity scale. application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46(10):1121–1123. doi:10.1001/archneur.1989.00520460115022
29. Hewlett S, Dures E, Almeida C. Measures of fatigue: Bristol rheumatoid arthritis fatigue multi-dimensional questionnaire (BRAF MDQ), Bristol rheumatoid arthritis fatigue numerical rating scales (BRAF NRS) for severity, effect, and coping, chalder fatigue questionnaire (CFQ), checklist individual strength (CIS20R and CIS8R), fatigue severity scale (FSS), functional assessment chronic illness therapy (fatigue) (FACIT-F), multi-dimensional assessment of fatigue (MAF), multi-dimensional fatigue inventory (MFI), pediatric quality of life (Pedsql) multi-dimensional fatigue scale, profile of fatigue (ProF), short form 36 vitality subscale (sf-36 vt), and visual analog scales (VAS). Arthritis Care Res. 2011;63(Suppl11):S263–286. doi:10.1002/acr.20579
30. Overman CL, Kool MB, Da Silva JA, et al. The prevalence of severe fatigue in rheumatic diseases: an international study. Clin Rheumatol. 2016;35(2):409–415. doi:10.1007/s10067-015-3035-6
31. Zhao R, Dong C, Gu Z, et al. Development and validation of a nomogram for predicting fatigue in patients with primary Sjögren’s syndrome. Clin Rheumatol. 2024;43(2):717–724. doi:10.1007/s10067-023-06853-9
32. Fox RI, Dixon R, Guarrasi V, et al. Treatment of primary Sjögren’s syndrome with hydroxychloroquine: a retrospective, open-label study. Lupus. 1996;5(Suppl 1):S31–36. doi:10.1177/0961203396005001081
33. Carsons SE, Vivino FB, Parke A, et al. Treatment guidelines for rheumatologic manifestations of Sjögren’s syndrome: use of biologic agents, management of fatigue, and inflammatory musculoskeletal pain. Arthritis Care Res. 2017;69(4):517–527. doi:10.1002/acr.22968
34. Ramos-Casals M, Brito-Zerón P, Bombardieri S, et al. EULAR recommendations for the management of Sjögren’s syndrome with topical and systemic therapies. Ann Rheum Dis. 2020;79(1):3–18. doi:10.1136/annrheumdis-2019-216114
35. Dass S, Bowman SJ, Vital EM, et al. Reduction of fatigue in Sjögren syndrome with rituximab: results of a randomised, double-blind, placebo-controlled pilot study. Ann Rheum Dis. 2008;67(11):1541–1544. doi:10.1136/ard.2007.083865
36. Tarn J, Legg S, Mitchell S, et al. The effects of noninvasive vagus nerve stimulation on fatigue and immune responses in patients with primary Sjögren’s syndrome. Neuromodulation. 2019;22(5):580–585. doi:10.1111/ner.12879
37. Cook KF, Jensen SE, Schalet BD, et al. PROMIS measures of pain, fatigue, negative affect, physical function, and social function demonstrated clinical validity across a range of chronic conditions. J Clin Epidemiol. 2016;73:89–102. doi:10.1016/j.jclinepi.2015.08.038
38. Bingham Iii CO, Gutierrez AK, Butanis A, et al. PROMIS fatigue short forms are reliable and valid in adults with rheumatoid arthritis. J Patient Rep Outcomes. 2019;3(1):14. doi:10.1186/s41687-019-0105-6
39. Mæland E, Miyamoto ST, Hammenfors D, et al. Understanding fatigue in Sjögren’s syndrome: outcome measures, biomarkers and possible interventions. Front Immunol. 2021;12:703079. doi:10.3389/fimmu.2021.703079
40. Nowell WB, Karis E, Gavigan K, et al. Patient-reported nausea and fatigue related to methotrexate: a prospective, self-controlled study in the Arthritispower(®) registry. Rheumatol Ther. 2022;9(1):207–221. doi:10.1007/s40744-021-00398-6
41. Sandikci SC, Gultuna S, Ozisler C, et al. The role of orexin in fatigue and sleep quality in patients with primary Sjögren’s syndrome. Z Rheumatol. 2024;83(Suppl 1):242–247. doi:10.1007/s00393-023-01462-y
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



