Back to Journals » Clinical Ophthalmology » Volume 18
Intraocular Pressure and Cup-to-Disc Ratio Asymmetry in Diagnosing Iris Melanoma
Authors Kong AW , Au A, Song W, Oh AJ, McCannel TA
Received 13 September 2023
Accepted for publication 5 January 2024
Published 16 October 2024 Volume 2024:18 Pages 2907—2915
DOI https://doi.org/10.2147/OPTH.S440072
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Alan W Kong, Adrian Au, Weilin Song, Angela J Oh, Tara A McCannel
Department of Ophthalmology, Stein Eye Institute, University of California Los Angeles, Los Angeles, CA, USA
Correspondence: Tara A McCannel, Department of Ophthalmology, University of California Los Angeles, 100 Stein Plaza, Los Angeles, CA, 90095, USA, Email [email protected]
Purpose: Distinguishing an iris melanoma from an iris nevus can be challenging as few clinical features other than documented growth are helpful in making the diagnosis. In this study, we compared the presenting intraocular pressure (IOP) and cup-to-disc ratio (CDR) between affected and unaffected eyes in patients with iris melanoma and iris nevus.
Patients and methods: This was a single-institution retrospective case series of patients treated for iris melanoma and iris nevus from January 2013 to October 2022. Thirty-nine subjects with iris melanoma and forty age-matched patients with iris nevus were included. We analyzed the difference in IOP, CDR, and diagnosis of glaucoma between affected and unaffected eyes in patients with iris melanoma and control iris nevus cohort.
Results: The average IOP for eyes with iris melanoma and iris nevus was 18.8± 6.1 mmHg and 14.6± 3.5 mmHg (P< 0.001), respectively. The average CDR was 0.36± 0.27 and 0.24± 0.14 (P=0.02), respectively. The average IOP of the contralateral unaffected eye in iris melanoma patients was 16.3± 3.5 mmHg, significantly less than the affected eye (P=0.03). The average CDR of the contralateral unaffected eye in iris melanoma was 0.25± 0.15, which was trending towards being less than the affected eye (P=0.05). There was no difference in the average IOP (P=0.89) or average CDR (P=0.49) between the affected and unaffected eye in patients with iris nevus.
Conclusion: We demonstrate that patients with iris melanoma are more likely to have greater IOP and CDR in the affected eye compared to the unaffected eye, and a diagnosis of unilateral glaucoma than eyes with iris nevus. Patients with iris melanoma had greater IOP asymmetry between the affected and unaffected eye. Therefore, IOP and CDR asymmetry may suggest a diagnosis of iris melanoma.
Keywords: iris melanoma, iris nevus, secondary glaucoma, intraocular pressure, cup to disc ratio
Introduction
Uveal melanoma is the most common primary intraocular malignancy, with iris melanoma representing approximately 2–4% of these intraocular cancers.1–3 Early detection and intervention remain key for the best overall vision and survival. Although clinical evaluation with slit-lamp biomicroscopy and ultrasound biomicroscopy (UBM) may aid in the diagnosis of iris melanoma, there are currently no well-established criteria for ruling in the diagnosis of iris melanoma other than documented growth.4,5 Factors that may suggest the diagnosis of iris melanoma include younger age, blood in the anterior chamber, diffuse configuration, presence of ectropion, and feathery margins (ABCDEF guide).6,7 Other clinical features that have been reported in iris melanoma include heterochromia and corectopia.8 Several studies and case reports have also shown an association between iris melanoma and elevated intraocular pressure (IOP), most commonly believed to be due to tumor infiltration of the trabecular meshwork.9–12 In fact, one study found that 15% of patients with iris melanoma had secondary melanoma-related glaucoma.13
While iris melanoma is known to interfere with the trabecular meshwork and may be associated with an increased risk of secondary glaucoma, little has been reported on the indirect findings of the long-standing effects of disrupted aqueous humor drainage from the tumor itself. Namely, the observations of IOP asymmetry and the effects of elevated IOP causing compression of the optic nerve resulting cup-to-disc asymmetry. In this study, we compared the presenting IOP and cup-to-disc ratio (CDR) between eyes with iris melanoma and iris nevus, and we compared the IOP and CDR differences between the affected and unaffected eyes for both iris melanoma and iris nevus.
Methods
This retrospective consecutive case series was conducted at the University of California, Los Angeles (UCLA) Stein Eye Institute, Los Angeles, CA, after obtaining approval from the UCLA Institutional Review Board (IRB). All study-related proceedings were performed in accordance with good clinical practice, the Declaration of Helsinki, and the Health Insurance Portability and Accountability Act (HIPAA). Patients with iris melanoma were identified through a review of patient who received episcleral plaque brachytherapy at the Ocular Oncology Center at UCLA Stein Eye Institute from January 2013 to December 2021. Patients were included if they had a diagnosis of iris melanoma that was confirmed through the progression in size on at least two visits either at the Ocular Oncology Center or by the referring specialist. Age-matched controls of patients with iris nevus were identified by reviewing consecutive patients who presented at the Ocular Oncology Center with iris nevus from January 2013 to October 2022. The diagnosis of iris nevus was confirmed if the patient had at least two clinical evaluations at least two years apart with no transformation to iris melanoma. Patients were excluded if they had bilateral iris nevus documented.
Electronic health records were reviewed for patient variables collected at the initial visit. These include age, sex, visual acuity, IOP, CDR, number of glaucoma medications, and number of glaucoma surgeries. IOPs were measured using Tonopen tonometry (Ametek Reichert Technology, Depew, NY). All CDR ratios were determined by a single provider (TAM). Baseline diagnosis of primary open-angle glaucoma or secondary glaucoma was noted by the referring physician. Baseline ultrasound biomicroscopy (Sonomed Escalon, New Hyde Park, New York) at presentation was also recorded. Patients with color fundus photography prior to treatment of iris melanoma or baseline fundus imaging for patients with iris nevus were utilized for calculation of the CDR.
Vertical CDR measurements were calculated from the fundus images. The images of patients with iris melanoma and iris nevus were randomized and analyzed by a grader (AWK) who was blinded to the diagnosis. The vertical CDR was calculated using JAVA-based ImageJ software (https://imagej.net/ij/index.html). Measurements were made using the straight-line measurement function to record the distance in pixels, similar to previous studies that compared CDR.14,15 The cup border was based on the pallor of the rim. The vertical CDR was defined as the ratio of the longest vertical line across the cup to the longest vertical line across the disc.
Baseline demographic data was compared using Student’s t-test for continuous variables and Fischer’s exact test for categorical variables. In addition, multivariate linear regressions were used to compare the differences in IOP and CDR asymmetry between the affected and unaffected eyes with iris melanoma while controlling for ciliary body involvement and tumor size. Receiver operating characteristic (ROC) curve analysis was performed to evaluate the diagnostic significance of using absolute IOP and CDR as well as IOP and CDR asymmetry between iris melanoma and iris nevus. A comparison of the area under ROC curves between two variables was calculated with DeLong’s test. The maximum Youden J cutoff was calculated to determine the optimum sensitivity and specificity of the ROC curves. An intraclass correlation analysis using two-way random effect models was completed to compare the agreement between the recorded CDR and the measured vertical CDR from fundus images. Significance was defined as P< 0.05. Data analyses were performed with R software version 4.2.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Demographics (Table 1)
Thirty-nine patients with iris melanoma were identified with forty age-matched patients with unilateral iris nevus. Demographics and baseline ocular characteristics of both groups are listed in Table 1. Patients with iris melanoma compared to iris nevus tended to have greater tumor heights and were more likely to have ciliary body involvement (Table 1). Furthermore, following the American Joint Committee on Cancer, 15 (38.5%) patients were classified as T1 stage at the time of presentation with 7 of 15 patients (46.7%) presenting with T1c stage compared to 8 patients (53.3%) with T1a or T1b stage. There were 24 patients (61.5%) with T2 stage at the time of presentation with 13 of 24 (54.2%) with T2c stage compared to 11 patients (45.8%) with T2a or T2b stage.
 |
Table 1 Demographics |
Among the 39 patients with iris melanoma, 12 patients had a diagnosis of secondary glaucoma and only one had a diagnosis of primary open-angle glaucoma. Of those with secondary glaucoma, 11 were reported to have glaucoma secondary to the tumor, and one individual had uveitic glaucoma. All 12 individuals with a diagnosis of secondary glaucoma had been started on IOP lowering medications prior to the first evaluation visit of their iris lesion.
Differences Between Patients with Iris Melanoma versus Iris Nevus (Table 2)
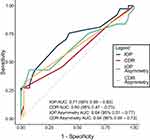
Differences in characteristics in the eyes between patients with an iris melanoma and an iris nevus are listed in Table 2. The eyes with iris melanoma had an average IOP of 18.8±6.1 mmHg, while the average IOP of eyes with iris nevus was 14.6±3.5 mmHg (P<0.001 and Figure 1A). The area under the ROC curve using the IOP was 0.71 (95% CI 0.59–0.83, P=0.001, Figure 2). The Youden J cutoff has a sensitivity of 76% and a specificity of 58%. Eyes with iris melanoma also exhibited larger CDRs (P=0.02 and Figure 1B), greater number of IOP lowering medications (P=0.04), but the area under the ROC curve using CDR was 0.60 (95% CI 0.47–0.73, P=0.07, Figure 2), which was not significant. Moreover, the Youden J cutoff has a sensitivity of 27% and a specificity of 97%. Eyes with iris melanoma were more likely to have a diagnosis of secondary glaucoma at the time of presentation (P<0.001). When comparing the subset of patients without a diagnosis of secondary glaucoma, eyes with iris melanoma had an average IOP of 17.2±4.45 mmHg, which was significantly greater than the eyes with an iris nevus (P=0.02). However, the average CDR for eyes with an iris melanoma and without a diagnosis of secondary glaucoma was 0.25±0.17, which was not significant (P=0.74).
 |
Table 2 Differences Between Affected Eyes of Patients with Iris Melanoma and Iris Nevus |
Differences Between Affected and Unaffected Eyes in Patients with Iris Melanoma versus Nevus (Table 3)
The average IOP in the eye with the iris melanoma was 18.8±6.1 mmHg, which was significantly greater than the contralateral, unaffected eye of 16.3±3.5 mmHg (P=0.03 and Figure 3A). There was no significant difference in IOP between the affected and unaffected eyes in patients with an iris nevus (P=0.89 and Figure 3B). Furthermore, the magnitude of the difference between the affected and unaffected eyes with iris melanoma was significantly larger than with an iris nevus (P=0.03). The ROC curve for using IOP asymmetry (Figure 2) had an area under the curve of 0.64 (95% CI 0.51–0.77, P=0.02). The Youden J cutoff has a sensitivity of 36% and a specificity of 93%. When comparing the recorded CDR within individuals, the average CDR for the eye with the iris melanoma was trending towards being significantly larger than the contralateral eye (P=0.05 and Figure 3C). Eyes with an iris nevus had no significant difference in CDR when compared to the contralateral eye (P=0.49 and Figure 3D). The ROC curve for CDR asymmetry (Figure 2) had an area under the curve of 0.64 (95% CI 0.54–0.73, P=0.03), and the Youden J cutoff has a sensitivity of 33% and a specificity of 95%. The difference in IOP and CDR was attenuated when analyzing those without an initial diagnosis of iris melanoma, however. The average IOP of eyes with an iris melanoma and without a diagnosis of secondary glaucoma was 17.2±4.5 mmHg compared to the contralateral eye with an average of 16.2±3.4 mmHg (P=0.40). The average CDR with an iris melanoma and without a diagnosis of secondary glaucoma was 0.25±0.17, and the average CDR for the contralateral eye was 0.22±0.10 (P=0.41).
 |
Table 3 Differences Between Unaffected and Affected Eyes with Iris Melanoma and Iris Nevus |
In addition, a multivariate analysis comparing IOP differences between the affected and unaffected eyes with both ciliary body involvement and tumor height showed that neither variable was predictive of an increased difference in IOP between eyes (−0.95±2.33 mmHg, P=0.68 for ciliary body; −0.08±0.59 mmHg, P=0.90 for tumor height). The same was true for CDR differences (−0.01±0.09, P=0.90 for ciliary body; −0.002±0.022 CDR units, P=0.91 for tumor height).
Agreement Between Measurements of CDR Using Subjective and Objective Approaches
To reduce the risk and bias for subjective CDR measurements in clinic, we performed a secondary objective analysis of the optic disc to confirm reliability and reproducibility of CDR. In total, 14 of the 39 patients (36%) with an iris melanoma had color fundus photography prior to treatment of the iris melanoma. For patients with an iris nevus, 10 of the 40 (25%) patients had baseline color fundus photography. After recalculating the CDR using ImageJ, the recalculated CDR was 0.43±0.13, which was not significantly different from the recorded CDR in the patient chart for this subset of patients of 0.32±0.23 (P=0.08). The average difference between the recalculated CDR (0.09± 0.17) and the recorded CDR (0.04±0.20) also did not significantly differ between the affected eye and the contralateral eye (P = 0.34). Moreover, using two-way random effect models to measure agreement between CDR raters, the intraclass correlation coefficient was 0.55 (95% confidence interval 0.058 to 0.783).
Discussion
In this cohort of patients with iris melanoma and iris nevus, we found that eyes with an iris melanoma had greater IOP and larger CDR compared to eyes with an iris nevus. In addition, patients with iris melanoma were more likely to have a diagnosis of secondary glaucoma at the time of presentation as well. In a subset of patients without secondary glaucoma at presentation, eyes with iris melanoma still exhibited greater IOP than eyes with iris nevus, but CDR was not significantly different. Furthermore, when comparing the IOP and CDR within individuals, patients with iris melanoma were more likely to have greater IOP and CDR asymmetry between the affected and unaffected eye at the time of presentation to an ocular oncology center. The area under the ROC curves for absolute IOP values, IOP differences, and CDR differences to diagnose iris melanoma from iris nevus were all significant, with the ROC curve for absolute IOP demonstrating the best diagnostic utility. Therefore, IOP and CDR asymmetry are two easily identifiable parameters in the clinical evaluation that may indicate a high likelihood of the diagnosis of iris melanoma.
While the rate of transformation from iris nevus to iris melanoma is relatively low, with only 2% becoming malignant over a mean follow-up period of 68 months,6 there is great interest in identifying clinical features and risk factors that predict transformation to malignancy as early treatment may result in improved outcomes. Currently, there are no well-established practice guidelines for diagnosing iris melanoma, and the best diagnostic sign of transformation is documented growth.4,5 Previous studies have identified several clinical features suggestive of an iris melanoma, but asymmetries in IOP or CDR between the affected and unaffected eyes were not assessed.6 In addition, prior studies have demonstrated that iris melanoma is associated with elevated IOPs,9–12 and eyes with iris melanoma also showed greater IOP than eyes with iris nevus in this study. However, these previous studies focused on defining elevated IOP as a binary event where the IOP was greater than a specific threshold that ranged from 21 to 23 mmHg. Thus, while elevated IOP is a helpful indicator of an iris melanoma, diagnostically, this study also suggests that it may be advantageous to recognize increasing IOP asymmetry between eyes within the same patient. Nevertheless, the area under the ROC curves for either IOP or CDR asymmetry remains relatively poor at discriminating (area under the ROC curve < 0.70) between iris melanoma and iris nevus. Future studies with larger datasets may further characterize the effectiveness of using IOP and CDR asymmetry.
In a subset analysis of patients without a diagnosis of secondary glaucoma at the time of presentation, eyes with iris melanoma still had greater IOP than eyes with iris nevus. However, CDR differences were attenuated. The IOP and CDR asymmetry were also decreased in patients without the diagnosis of secondary glaucoma. This suggests that the IOP elevation seen with iris melanoma may be subtle and further work is required to distinguish whether these IOP changes occur before the development of glaucoma. Future studies can also measure structural and functional changes by measuring retinal nerve fiber layer (RNFL) thickness and visual field changes to identify if there are early glaucomatous changes in patients presenting with iris melanoma. After all, it is possible that the greater asymmetry in IOP and CDR are proxies for early, undiagnosed secondary glaucoma that warrants further diagnostic testing. This is suggested by our finding of an existing diagnosis of glaucoma at the initial presentation in 30.8% of iris melanomas.
In this cohort, patients with iris melanoma were more likely to have ciliary body involvement, and the tumor height was greater than the iris nevus height. However, in this study, neither ciliary body involvement nor the tumor height was predictive of the difference of IOP or CDR between the affected and unaffected eyes in this cohort. In a prospective study of patients with all forms of uveal melanoma, both larger tumors and ciliary body involvement, as well as retinal detachments, were predictive of initial secondary glaucoma.16 While angle involvement and tumor invasion into the angle are some of the primary mechanisms that we believe result in elevated IOP,9,16 these results suggest that ciliary body involvement and tumor size alone may not fully explain the asymmetries seen in IOP or CDR. Additional work can be done to better characterize the tumor features that do predict subtle IOP changes that may further improve the detection of malignant transformations.
One limitation of this study was that many of the patients were followed by an outside provider before being referred. As a result, we only have the IOP and CDR of patients at the time of presentation to the ocular oncology center, and we do not have the visual field or other diagnostic data to confirm the diagnosis of secondary glaucoma that was given to several patients prior to their presentation, which limits our ability to comment on the severity of the glaucoma and initial IOP changes. The IOP was also measured using Tonopen tonometry in this cohort. While Tonopen tonometry has reasonable repeatability, rebound and applanation tonometry have better repeatability and were found to be better at measuring the true IOP.17 Further work with standardized IOP measurements using applanation tonometry may allow for more precise readings of the IOP asymmetry to evaluate this same question. Another limitation is that CDR may be a subjective measurement that could be influenced by the provider’s a priori knowledge. Nevertheless, in this study, we randomized the fundus images and recalculated the vertical CDR. In doing so, we found that the recorded CDR did not significantly differ from the recalculated CDRs. For this population of patients, anterior segment optical coherence tomography (OCT) was not done to evaluate the iris melanoma or nevus. Anterior segment OCT can be a useful tool in diagnosing iris melanocytic tumors,18–21 and in one case series, anterior segment OCT was helpful in identifying iris nevus where UBM visualization was not satisfactory.19 Future studies can also incorporate anterior segment OCT for additional evaluation of malignant transformations. The tumor base diameter was also unable to be retrospectively collected for this dataset, which would also be another useful tumor characteristic that could be used in further analysis of IOP and CDR differences.
In summary, eyes with iris melanoma have larger IOP and CDR compared to the contralateral, unaffected eye, which was not observed in patients with iris nevus. Moreover, eyes with iris melanoma and without secondary glaucoma exhibited greater IOP than eyes with an iris nevus, suggesting that eyes with iris melanoma may have changes prior to the development of glaucomatous changes to the optic nerve. Early detection and treatment can ultimately lower the need for enucleation or metastatic disease. IOP and CDR asymmetry are two easily identifiable parameters in the clinical evaluation that can indicate a high likelihood of the diagnosis of iris melanoma.
Acknowledgments
None of the authors have competing interests to disclose. Funding was provided by an unrestricted grant to the Stein Eye Institute from the Research to Prevent Blindness (RPB), and the George E. and Ruth Moss Trust. The abstract of this paper was presented at the Association for Research in Vision and Ophthalmology as an abstract presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in Investigative Ophthalmology and Visual Sciences, Volume 64, Issue 8.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Shields CL, Shields JA, Materin M, Gershenbaum E, Singh AD, Smith A. Iris melanoma: risk factors for metastasis in 169 consecutive patients. Ophthalmology. 2001;108(1):172–178. doi:10.1016/S0161-6420(00)00449-8
2. Jensen OA. Malignant melanomas of the human uvea. Recent follow-up of cases in Denmark, 1943–1952. Acta Ophthalmol. 1970;48(6):1113–1128. doi:10.1111/j.1755-3768.1970.tb06592.x
3. Shields CL, Furuta M, Thangappan A, et al. Metastasis of uveal melanoma millimeter-by-millimeter in 8033 consecutive eyes. Arch Ophthalmol Chic IL 1960. 2009;127(8):989–998. doi:10.1001/archophthalmol.2009.208
4. Kaliki S, Shields CL. Uveal melanoma: relatively rare but deadly cancer. Eye. 2017;31(2):241–257. doi:10.1038/eye.2016.275
5. Oxenreiter MM, Lane AM, Jain P, Kim IK, Gragoudas ES. Conservative management of suspicious melanocytic lesions of the iris. Graefes Arch Clin Exp Ophthalmol. 2019;257(6):1319–1324. doi:10.1007/s00417-019-04296-0
6. Shields CL, Kaliki S, Hutchinson A, et al. Iris nevus growth into melanoma: analysis of 1611 consecutive eyes: the ABCDEF guide. Ophthalmology. 2013;120(4):766–772. doi:10.1016/j.ophtha.2012.09.042
7. Shields CL, Kels JG, Shields JA. Melanoma of the eye: revealing hidden secrets, one at a time. Clin Dermatol. 2015;33(2):183–196. doi:10.1016/j.clindermatol.2014.10.010
8. Shields CL, Kaliki S, Shah SU, Luo W, Furuta M, Shields JA. Iris melanoma: features and prognosis in 317 children and adults. J AAPOS off Publ Am Assoc Pediatr Ophthalmol Strabismus. 2012;16(1):10–16. doi:10.1016/j.jaapos.2011.10.012
9. Shields CL, Shields JA, Shields MB, Augsburger JJ. Prevalence and mechanisms of secondary intraocular pressure elevation in eyes with intraocular tumors. Ophthalmology. 1987;94(7):839–846. doi:10.1016/s0161-6420(87)33537-7
10. Conway RM, Chua WC, Qureshi C, Billson FA. Primary iris melanoma: diagnostic features and outcome of conservative surgical treatment. Br J Ophthalmol. 2001;85(7):848–854. doi:10.1136/bjo.85.7.848
11. Shields CL, Materin MA, Shields JA, Gershenbaum E, Singh AD, Smith A. Factors associated with elevated intraocular pressure in eyes with iris melanoma. Br J Ophthalmol. 2001;85(6):666–669. doi:10.1136/bjo.85.6.666
12. Demirci H, Shields CL, Shields JA, Eagle RC, Honavar SG. Diffuse iris melanoma: a report of 25 cases. Ophthalmology. 2002;109(8):1553–1560. doi:10.1016/s0161-6420(02)01104-1
13. Shukla AG, Vaidya S, Yaghy A, et al. Iris melanoma: factors predictive of post-management secondary glaucoma in 271 cases at a Single Ocular Oncology Centre. Eye Lond Engl. 2022. doi:10.1038/s41433-022-02051-0
14. McClelland JF, O’Donoghue L, McIntyre M, Saunders KJ. Cup-to-disc and arteriole-to-venule ratios in children aged 6–7 and 12–13 years. Ophthalmic Physiol Opt J Br Coll Ophthalmic Opt Optom. 2012;32(1):31–38. doi:10.1111/j.1475-1313.2011.00878.x
15. Chan PP, Chiu V, Wong MO. Variability of vertical cup to disc ratio measurement and the effects of glaucoma 5-year risk estimation in untreated ocular hypertensive eyes. Br J Ophthalmol. 2019;103(3):361–368. doi:10.1136/bjophthalmol-2017-311841
16. Stadigh AE, Puska PM, Kivelä TT. Incidence and risk factors for secondary glaucoma in eyes with uveal melanoma. Ophthalmol Glaucoma. 2023;6(1):29–41. doi:10.1016/j.ogla.2022.08.002
17. Ertel MK, Seibold LK, Patnaik JL, Kahook MY. Comparison of intraocular pressure readings with Perkins, Tonopen, iCare 200, and iCare Home to manometry in cadaveric eyes. Int J Ophthalmol. 2022;15(12):2022–2027. doi:10.18240/ijo.2022.12.19
18. Razzaq L, Emmanouilidis-van der Spek K, Luyten GPM, de Keizer RJW. Anterior segment imaging for iris melanocytic tumors. Eur J Ophthalmol. 2011;21(5):608–614. doi:10.5301/EJO.2011.6214
19. Konopińska J, Lisowski Ł, Wasiluk E, Mariak Z, Obuchowska I. The effectiveness of ultrasound biomicroscopic and anterior segment optical coherence tomography in the assessment of anterior segment tumors: long-term follow-up. J Ophthalmol. 2020;2020:9053737. doi:10.1155/2020/9053737
20. Mirzayev I, Gündüz AK, Gündüz ÖÖ. Anterior segment optical coherence tomography in iris and ciliary body tumors: a systematic review. Expert Rev Ophthalmol. 2023;18(3):193–204. doi:10.1080/17469899.2023.2224565
21. Mirzayev I, Gündüz AK, Aydın EP, Gündüz ÖÖ. Clinical applications of anterior segment swept-source optical coherence tomography: a systematic review. Photodiagnosis Photodyn Ther. 2023;42:103334. doi:10.1016/j.pdpdt.2023.103334
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Risk Factors and Management of Intraocular Pressure Elevation After Vitrectomy Combined with Silicone Oil Tamponade
Ge L, Su N, Fan W, Yuan S
International Journal of General Medicine 2024, 17:447-456
Published Date: 3 February 2024