Back to Journals » Journal of Inflammation Research » Volume 17
Intraperitoneal MASP-1 Levels are Associated with Peritoneal Solute Transport Rate in Peritoneal Dialysis Patients: A Retrospective Cohort Study
Authors Li J , Xiong Y , Chen M, Xu D, Zhou L, Shen L, Lu G
Received 20 August 2024
Accepted for publication 18 October 2024
Published 29 October 2024 Volume 2024:17 Pages 7807—7817
DOI https://doi.org/10.2147/JIR.S486011
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Adam Bachstetter
Jianzhong Li,1,* Yan Xiong,2,* Mingyu Chen,1,* Deyu Xu,1 Ling Zhou,1 Lei Shen,1 Guoyuan Lu1
1Department of Nephrology, The First Affiliated Hospital of Soochow University, Suzhou, Jiangsu, 215006, People’s Republic of China; 2Department of Nephrology, Kunshan First People’s Hospital Affiliated to Jiangsu University, Kunshan, Jiangsu, 215300, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jianzhong Li; Guoyuan Lu, Department of Nephrology, The First Affiliated Hospital of Soochow University, Suzhou, Jiangsu, 215006, People’s Republic of China, Email [email protected]; [email protected]
Purpose: A major limitation of long-term peritoneal dialysis (PD) is peritoneal membrane dysfunction characterized by faster peritoneal solute-transport rate (PSTR). This study aimed to identify efficient complement factors in peritoneal effluents of continuous ambulatory peritoneal dialysis (CAPD) patients that can predict the PSTR.
Methods: A multiplex suspension protein array was used to screened related complement pathways in overnight peritoneal effluents among 58 CAPD patients. Then the related complement factors in lectin and classical pathways in effluents were analyzed using ELISA kits among another cohort of 129 CAPD patients. Logistic regression modeling was fitted to predict the PSTR of PD patients.
Results: The multiplex suspension protein array showed complement factors including C2, C4b, C5, C5a, Factor D, Factor I, and MBL were detected in effluents of CAPD patients, and the effluent C2 Appearance rate (Ar) and C4b Ar levels were significantly correlated with D/P Cr and D/D0 glucose. The levels of effluents MASP-1 Ar, M-Ficolin Ar, C2 Ar and C4b Ar, which belong to the lectin pathway were also positively correlated with D/P Cr according the ELISA results and these parameters were expressed higher in the high and high-average (H/HA) groups according to the PET results. Moreover, effluent Masp-1 was independently associated with increased PSTR and adverse events related peritoneal transport function failure.
Conclusion: This study suggested that the lectin pathway may be involved in local complement activation and peritoneal injury of PD patients, intraperitoneal level of Masp-1 was an independent predictor of increased PSTR in PD patients.
Keywords: peritoneal dialysis, complement, lectin pathway, Masp-1, peritoneal solute-transport rate
Introduction
Peritoneal dialysis (PD) is an effective renal replacement therapy for patients with end-stage renal disease1,2. The structural and functional completeness of peritoneal membrane is essential for PD efficiency, which deteriorates with long-term PD. The damaged peritoneum is characterized by phenotypic changes in mesothelial cells and deposition of extracellular matrix and collagen, eventually leading to peritoneal fibrosis and functional failure of PD. Exposure to bio-incompatible dialysis solutions, angiogenesis in peritoneum, and chronic inflammation have been identified to cause the progression of peritoneal fibrosis in patients undergoing PD.3,4
Clinically, the peritoneal equilibration test (PET) is applied to assess the function of peritoneal membrane by observing solute clearance and daily ultrafiltration. The PET includes three parameters, namely, 4h dialysate/plasma creatinine, 4h to 0h dialysate glucose, and 4h ultrafiltration volume.5
As shown by data from a large contemporary cohort study, a faster solute-transfer rate is closely associated with higher all-cause mortality and hospitalization rates.5 The peritoneal solute transport rate (PSTR) is an indicator commonly derived from the PET (D/P Cr) and reflects the efficiency of solute transport across the peritoneal membrane in patients undergoing peritoneal dialysis,6 and it is recognized as a predictor for local chronic inflammation in peritoneal cavity and the progression of peritoneum injury. Evidence has shown that the local production of several inflammatory cytokines including interleukin (IL) 6 (IL-6), tumor necrosis factor α, IL-1, and interferon-g (IFN-g) are strongly correlated with PSTR.7–9 The PET is also time consuming, and the patients always need to be hospitalized. Therefore, the search for a biomarker in effluent that is both readily accessible and effective in reflecting the PSTR is of great value and can significantly improve operational efficiency.
The complement cascade is involved in the innate immune system, and it has three activating routes, the classical, the alternative, and the lectin pathway.10,11 In vitro studies have shown that peritoneal mesothelial cells can synthesize and secrete various complement factors, including C3, C4, and C5.12 Proteomic and ELISA analyses have revealed that C3, C4, Factor B, Factor D, Factor H, and Factor I are present in the peritoneal dialysate of PD patients.13–15 Proteomic analysis of PD fluid has also revealed high transporter status presenting as high expression of C3 in effluents of PD patients, whereas C4 expression is lower in low transporters.16 These results indicate that the complement cascade is activated in the peritoneal cavity of PD patients, and complement factors in effluents may be related to PSTR. Moreover, it is not known which complement pathway initiates and modulates the involvement of peritoneal membrane injury in PD patients.
Therefore, this study aimed to determine the predictive value of complement components in effluents for increased PSTR.
Patients and Methods
Patients
Stable CAPD patients at the PD unit of the First Hospital Affiliated of Soochow University were followed-up regularly from June 2018 to June 2022. All these patients were indwelling Tenckhoff double-polyester-sheathed PD catheters and initiated PD with a 1.5% or 2.5% dextrose PD fluid (Dianeal®, Baxter). Exclusion criteria included patients who suffered peritonitis, abdominal trauma, or other acute inflammatory diseases over the past six months, as well as active autoimmune diseases, and cancer. All patients were asked to undergo PD using 1.5% or 2.5% dextrose PD solution with a 10 h dwell time. Then, we collected a 10 mL effluent sample, simultaneously, venous blood samples were also collected. After the dialysis fluid had drained completely, a standard PET was performed. A total of 58 samples obtained from the peritoneal dialysis effluent (June 2018 to Feb 2019) were selected for the multiplex suspension protein array experiment. In the ELISA experiment, we selected the effluent samples from the CAPD patients between Feb 2019 and June 2022 who was regularly followed up for 24 months. A total of 129 patients were included in the experiment. This study was performed with the written informed consent of all patients, and the procedures were approved by the Ethics Committee of The First Affiliated Hospital Affiliated of Soochow University (NO. 2952023). All participants signed an informed consent form. Our study was complied with the Declaration of Helsinki.
Peritoneal Equilibration Test
A 4h PET was used to evaluate the peritoneal membrane-transport parameters as previously described.17 D/P Cr, D/D0 glucose, and 4 h ultrafiltration capacity were calculated. The CAPD patients were grouped according to the following PET results: high transport (D/P Cr = 0.82–1.03), high-average transport (D/P Cr = 0.65–0.81), low-average transport (D/P Cr = 0.50–0.64), and low transport (D/P Cr = 0.34–0.49).
Clinical Definitions
Hypertension was defined as a systolic blood pressure >140 mmHg, a diastolic blood pressure >90 mmHg, a documented history of hypertension, and/or the use of antihypertensive medications. Diabetes mellitus was defined by an HbA1c level > 6.5%, a history of diabetes, and/or the use of oral hypoglycemic agents or insulin. Adverse events in the study were defined: Retrospective analysis during the 24 months after specimen collection, we assessed the incidence of cardiovascular causes of death, PD withdrawal, and newly developed heart failure.
ELISA and Multiplex Suspension Protein Array for Complement Factors
All patients in the study were required to undergo PD using 1.5% or 2.5% dextrose PD solution with a 10 h dwell time. We collected peritoneal fluid samples from the overnight effluent in the PD center, venous blood samples were also collected. The samples were immediately stored at −80°C. Effluent C1q (Invitrogen), MASP-1 (CUSABIO), MASP-2 (CUSABIO), M-Ficolin (Abcam), H-Ficolin (Reddot Biotech), L-Ficolin (CUSABIO), C2 (Reddot Biotech), C4b (CUSABIO) levels were quantified with ELISA kits according to the manufacturer’s instructions. For the Multiplex suspension protein array test, the abundance of complement factors in effluents were measured using a Luminex Platform (Bio-Plex, Bio-Rad) and the Milliplex human complement panel (Millipore) according to the manufacturer’s procedure. Appearance rate (Ar) = concentration of complement factors in the peritoneal effluent × volume of the effluent (mL) / dwell time (min).
Statistical Analysis
Quantitative variables were expressed as the mean±standard deviation. We compared the baseline characteristics of the study population between the high and high-average (H/HA) and low and low-average (L/LA) transport groups by using Student’s-test for normally distributed data or nonparametric Mann–Whitney U-test for non-normally distributed variables, and χ2 testing for categorical variables. The relationships between clinical variables and D/P Cr level were analyzed by Pearson/Spearman correlation coefficient test for normally or non-normally distributed data. Multivariate logistic regression modelling was applied to identify independent significant factors influencing PSTR obtained by PET results and adverse events related peritoneal transport function failure. These statistical analyses were performed using SPSS version 25.0 software (IBM Corp, USA).
Results
Effluent Complement Factors Assessed by a Multiplex Suspension Protein Array
First, a multiplex suspension protein array (C2, C4b, C5, C5a, C9, Factor D, Factor I, and MBL) was used to detect related complement factors in overnight peritoneal effluents among 58 CAPD patients with routine follow-up, the mean age of the cohort was 49.59 years, 40% were male, and the median PD duration was 37.49±34.64 months. The patients’ clinical characteristics were summarized in Table 1. Except for complement C9, other complement factors in this array can be detected, including C2, C4b, C5, C5a, Factor D, Factor I, and MBL (Table 2). We then compared the correlation of these complement factors in effluents with the PET results. Through Pearson/Spearman correlation coefficient test, the effluent C2 appearance rate (Ar) levels were found to be significantly correlated with D/P Cr (p<0.0001, r=0.53) and D/D0 glucose (P<0.0001 r=−0.54), and the effluent C4b Ar levels were significantly correlated with D/P Cr (p=0.01, r =0.33) and D/D0 glucose (P=0.001 r=−0.41) (Table 2). No apparent correlation was observed for serum samples between the PET results and C2 or C4b levels (Supplementary Table 1). During to complement C2 and C4b belong to lectin or classical pathway, the above results suggest these two complement pathways may be involved in local complement activation and peritoneal injury of PD patients.
 |
Table 1 Clinical Characteristics of Enrolled CAPD Patients (N= 58) |
 |
Table 2 Detection of Effluent Complement Factors by a Multiplex Suspension Protein Array and Compared the Association of Effluent Complement Factors and PET Results |
Lectin and Classical Pathways in Effluents of CAPD Patients
We further quantified complement cascades of lectin and classical pathways in effluents by ELISA kits. In the assessment cohort of 129 patients with CAPD, we measured c1q, MASP-1, MASP-2, M-Ficolin, H-Ficolin, L-Ficolin, C2, C4b. Consistent with the results of multiplex suspension protein array, levels of C2 Ar and C4b Ar were associated with higher D/P Cr (p=0.003, r=0.258 and p=0.011 r=0.224, respectively). Additionally, higher effluents MASP-1 Ar, M-Ficolin Ar levels were also positively correlated with D/P Cr (p<0.001, r=0.303 and p=0.004, r=0.251, respectively) (Figure 1). Considering the potential impact of glucose exposure on complement activation, we observed the correlation between complement concentration and glucose exposure in the overnight peritoneal dialysis fluid, the results suggest that only effluent L-flicolin Ar is positively correlated with glucose exposure, the other complement components were not significantly correlated with glucose exposure (Supplementary Table 2). The above findings showed that lectin pathway may play a role in local complement activation and peritoneal injury of PD patients. The patients were then divided into two subgroups, ie, L/LA (low/low-average transport) or H/HA (high/high-average transport) group based on D/P Cr obtained by PET. The H/HA group displayed considerably higher levels of effluent Masp-1 Ar (6.65 ± 2.87 vs 5.00 ± 2.56 μg/min; p=0.002); M-Ficolin Ar (4.42 ± 1.66 vs 3.45 ± 1.67 μg/min; p=0.002); C2 Ar (0.99 ± 0.44 vs 0.80 ± 0.42 μg/mL; p=0.025), C4b Ar (0.44 ± 0.17 vs 0.36 ± 0.19 μg/mL; p=0.017) than the L/LA group. The H/HA group presented longer PD durations (35.66 ± 29.77 vs 24.52 ± 17.04 months; p=0.008), with lower serum albumin (31.47 ± 4.98 vs 34.32 ± 3.33 g/L; p<0.001), lower serum hemoglobin (96.21 ± 12.46 vs 102.91 ± 13.52 g/L; p=0.008), lower serum phosphate levels (1.48 ± 0.29 vs 1.65 ± 0.36 mmol/L; p=0.005) (Table 3).
 |
Table 3 Clinical Characteristics and Effluent Complement Biomarkers with CAPD Patients Stratified by L/LA and H/HA According to the PET Results |
 |
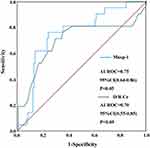
Figure 1 Associations of effluent complement biomarkers and D/P Cr according to the PET results. The unit of all the Ar of complement factors is μg/min. |
Predictive Value of Masp-1 for Peritoneal Transport Status
To evaluate whether these complement factors were independent predictive factors of peritoneal membrane transport function, we performed multivariate logistic regression analysis. Effluent Masp-1 was an independent predictor of PSTR even after adjustment for Age, Sex, Uric acid, Creatinine, Calcium, Phosphate, Albumin, Hemoglobin, PTH, Hypertension, Diabetic mellitus, hs-CRP, 4h ultrafiltration volume, PD vintage, Renal Kt/V urea, Peritoneal Kt/V urea, Total Kt/V urea, History of peritonitis, Glucose exposure (odds ratio [OR]:0.76; 95% CI:0.61 ~ 0.95; P=0.016) (Table 4). These patients underwent follow-up for 24 months, we traced the adverse events related peritoneal transport function failure, including cardiovascular causes of death, ultrafiltration failure-induced PD withdrawal, heart failure. Among these 129 patients, 4 patients died; 9 patients had been withdrawn from PD;7 patients developed heart failure. Multivariate logistic regression analysis showed effluent Masp-1 Ar was an independent predictor of adverse events after adjusting for Age, Sex, Uric acid, Creatinine, Calcium, Phosphate, Albumin, Hemoglobin, PTH, Hypertension, Diabetic mellitus, hs-CRP, 4h ultrafiltration volume, PD vintage, Renal Kt/V urea, Peritoneal Kt/V urea, Total Kt/V urea, History of peritonitis, Glucose exposure (odds ratio [OR]:1.50; 95% CI: 1.11 ~ 2.02; P= 0.009) (Table 5). As depicted in Figure 2, Masp-1 can accurately predict the prognosis of the adverse events related peritoneal transport function failure (AUROC:0.75, 95% CI:0.64–0.86; P<0.05) and which was even slightly better than the predictive ability of D/P Cr (AUROC:0.70, 95% CI:0.55–0.85;P<0.05).
 |
Table 4 Association between effluent complements and increased PSTR assessed by PET |
 |
Table 5 Association between effluent complement Masp-1 Ar and the adverse events related peritoneal transport function failure |
Discussion
In the present study, we aimed to investigate the association between complement components in peritoneal cavity and peritoneal transport solute rate among CAPD patients. To our knowledge, we report for the first time that the lectin pathway, including Masp-1, M-Ficolin, C2, and C4b, were activated in peritoneal cavity in patients with CAPD, and these complement components were significantly correlated with peritoneal membrane transport properties; effluent Masp-1 was an independent predictor factor for increased PSTR.
The peritoneal membrane undergoes structural and functional changes during extended periods of peritoneal dialysis. Structural alterations include the denudation of peritoneal mesothelial cells, thickening of the submesothelial layer, neoangiogenesis, and thickening of the vascular wall with type IV collagen deposition.3,4 The most prevalent functional deterioration observed is an increase in PSTR, leading to compromised ultrafiltration capacity. Elevated PSTR has been identified as an independent predictor of heightened risk for technique failure and mortality in PD patients.5,18 A meta-analysis encompassing 6648 PD patients revealed a statistically significant correlation between an elevated PSTR and increased mortality, along with a trend towards higher rates of technique failure. The analysis involved the pooling of data from 19 studies to calculate a summary relative risk of mortality of 1.15 for each 0.1 unit increase in the D/P Cr ratio.19 A large retrospective study has recently reported a strong inverse relationship between D/P Cr and D/D0 glucose, as well as an intimate link between these parameters and hospitalization rate or all-cause mortality.5 Consequently, our research has been centered on identifying effective indicators capable of predicting the PSTR. Besides, 4h-UF and the complement excretion rate in peritoneal effluent show no significant correlation. The possible explanations are as follows: First, due to differences in residual kidney function, the ultrafiltration volume in peritoneal dialysis is not only affected by the peritoneal transport rate. Second, The ultrafiltration volume measured using the PET method is likely to have some degree of error. This is partly due to the fact that commercially available peritoneal dialysis (PD) bags often contain more dialysate than the stated volume (overfill) for flush-before-fill procedures, and this overfill amount can vary, leading to imprecision in the measurement.20
The complement system is essential for both innate and adaptive immune responses. Previous studies have reported that the complement system can be triggered within the peritoneal cavity. Cell and tissue experiments showed that CD55 on the peritoneal mesothelium regulates local complement system cascade activation. Different complement factors are produced and secreted by mesothelial cells, including C4, C3, and C5b-9.12,21 Daniel Kitterer et al reported that effluent CD55 is expressed less in the H/HA group than in the L/LA group; As well, the level of dialysis glucose exposure is related to C5b-9 deposition in PD patients’ arterioles.22 Thus, complement cascade pathways are notably involved in the peritoneal cavity in PD patients according to previous studies. However, the specific complement pathway activation and the correlation between complement factors and peritoneal membrane transport properties remain unclear. Firstly, we screened complement pathways through a multiplex suspension protein array, C2, C4b, C5, C5a, Factor D, Factor I, and MBL could be detected in the effluents. A correlation could be established between the effluent C2 or C4b levels and D/P Cr according to the PET results. Additionally, the levels of C2 or C4b in the PD effluents did not depend on the serum concentration, revealing that C2 or C4b mainly originated from peritoneal mesothelium. C2 and C4b are the core constituents of the classical or lectin complement system. In the classical pathway, C1q binds to antibodies or immune complexes, leading to the activation of C2 and C4. In the lectin pathway, carbohydrates expressed on the surface of injured cells or pathogens bind to 1 of 6 pattern-recognition molecules: mannan-binding lectin (MBL), collectin-10, collectin-11, L-Ficolin, H-Ficolin, or M-Ficolin. By forming complexes with MBL-associated serine proteases 1 (MASP-1) and 2 (MASP-2), these pattern-recognition molecules activate C2 and C4. Therefore, the complement components belonging to these pathways were further examined by ELISA kits among another 129 patients, including C1q, Masp-1, Masp-2, M-Ficolin, H-Ficolin, L-Ficolin, C2 and C4b. The detection results showed that the Ar levels of Masp-1, M-Ficolin, C2 and C4b in effluents were significantly positively correlated with D/P Cr, and these parameters were expressed higher in H/HA group than the L/LA group. Logistic-regression models were generated after adjusting for Age, Sex, Uric acid, Creatinine, Calcium, Phosphate, Albumin, Hemoglobin, PTH, Hypertension, Diabetic mellitus, hs-CRP, 4h ultrafiltration volume, PD vintage, Renal Kt/V urea, Peritoneal Kt/V urea, Total Kt/V urea, History of peritonitis, Glucose exposure, and effluent Masp-1 in effluents remained to be an independent predictor factor for increased PSTR and the adverse events related peritoneal transport function failure. The above results suggested that lectin pathway may dominate the complement activation in peritoneal cavity in PD patients. The possible causal mechanism of complement activation in PD patients is presented below: PD therapy decreases the expression of complement regulators such as CD55 and CD59 on the peritoneal mesothelium, leading to local complement activation.22 Currently, the mainstream view is that epithelial-mesenchymal transition(EMT) indeed participates in peritoneal fibrosis and the decline of peritoneal function.23 There are also studies indicating a relationship between complement and cellular EMT.24,25 Thus, except for predicting increased PSTR, the activation of the complement cascade may also contribute to mesothelial EMT and peritoneal fibrosis, accelerating the loss of peritoneal membrane function. So far, no animal or cell experiments have clearly established a relationship between complement activation and peritoneal mesothelial cells injury, which warrants further research, and the role of complement inhibitors in alleviating peritoneal functional impairment also merits further investigation. Moreover, Maria Bartosova et al suggests that The amount of glucose exposure in peritoneal dialysis fluid is closely related to the expression of peritoneal complement regulatory proteins. Therefore, we further analyzed the correlation between glucose exposure and complement levels. In our cohort, except for L- Ficolin Ar in effluents, there was no significant correlation between complement levels and the overnight glucose exposure.
Among the patients who were followed up, 67% belonged to the H/HA group based on the PET results, which is consistent with findings from other multicenter studies (ranging from 47.4–83%).8,26,27 While comparing the parameters between the H/HA and L/LA groups, it was found that patients with faster solute-transfer rate had longer PD duration. The H/HA group manifested as lower serum albumin and hemoglobin levels than the L/LA group (Table 3). These findings can be interpreted through several different mechanisms: patients with a faster PSTR often have a higher baseline albumin clearance and a higher prevalence of systemic inflammation, a greater comorbidity burden, or an increased fluid load.7,28–33 Moreover, phosphate clearance is increased in the H/HA group compared with the L/LA group, consistent with a previous report.5
Although the findings from the current study are intriguing and potentially carry significant importance, they should be regarded as preliminary and necessitate further validation through corroborative and mechanistic investigations. First, with the cross-sectional nature of this work, causality cannot be established, and this was a retrospective analysis, which has inherent limitations, the dynamic analysis of effluent complement concentration and PSTR is of greater significance. Second, we did not explore the association between the effluent MASP-1 levels and survival curve or hospitalization rate during PD because of insufficient follow-up duration. Furthermore, the small sample size in this single-center study may lead to selection bias. It is evident that a large-scale study with extended follow-up is necessary to validate our findings.
In summary, complement factors, especially the lectin pathway is activated in peritoneal cavity in PD patients; effluent Masp-1 may potentially be a potentially useful biomarker for identifying increased PSTR.
Acknowledgments
This work was supported by Science Foundation of Jiangsu Province Grant (BK20231199); Science and Technology Project of Suzhou (SKY2022141); Scientific Research Project of Jiangsu Provincial Health Commission (H2017037).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors hereby declare that they have no competing interests.
References
1. Teitelbaum I. Teitelbaum I: peritoneal Dialysis. N Engl J Med. 2021;385:1786–1795. doi:10.1056/NEJMra2100152
2. Li PK, Chow KM, Van de Luijtgaarden MW, et al. Changes in the worldwide epidemiology of peritoneal dialysis. Nat Rev Nephrol. 2017;13:90–103. doi:10.1038/nrneph.2016.181
3. Morelle J, Lambie M, Oberg CM, Davies S. The peritoneal membrane and its role in peritoneal dialysis. Clin J Am Soc Nephrol. 2023;19:244–253. doi:10.2215/CJN.0000000000000282
4. Krediet RT, Struijk DG. Peritoneal changes in patients on long-term peritoneal dialysis. Nat Rev Nephrol. 2013;9:419–429. doi:10.1038/nrneph.2013.99
5. Mehrotra R, Ravel V, Streja E, et al. Peritoneal Equilibration Test and Patient Outcomes. Clin J Am Soc Nephrol. 2015;10:1990–2001. doi:10.2215/CJN.03470315
6. Wu B, Zhao H, Zuo L, et al. Short-term peritoneal rest reduces peritoneal solute transport rate and increases ultrafiltration in high/high average transport peritoneal dialysis patients: a crossover randomized controlled trial. Clin Kidney J. 2024;17:sfae251.
7. Lopes Barreto D, Krediet RT. Current status and practical use of effluent biomarkers in peritoneal dialysis patients. Am J Kidney Dis. 2013;62:823–833. doi:10.1053/j.ajkd.2013.01.031
8. Sezer S, Tutal E, Arat Z, et al. Peritoneal transport status influence on atherosclerosis/inflammation in CAPD patients. J Ren Nutr. 2005;15:427–434. doi:10.1053/j.jrn.2005.07.007
9. Yang X, Tong Y, Yan H, Ni Z, Qian J, Fang W. High intraperitoneal interleukin-6 levels predict peritonitis in peritoneal dialysis patients: a prospective cohort study. Am J Nephrol. 2018;47:317–324. doi:10.1159/000489271
10. McCaughan JA, O’Rourke DM, Courtney AE. The complement cascade in kidney disease: from sideline to center stage. Am J Kidney Dis. 2013;62:604–614. doi:10.1053/j.ajkd.2012.12.033
11. Lo MW, Woodruff TM. Complement: bridging the innate and adaptive immune systems in sterile inflammation. J Leukoc Biol. 2020;108:339–351. doi:10.1002/JLB.3MIR0220-270R
12. Tang S, Leung JC, Chan LY, et al. Regulation of complement C3 and C4 synthesis in human peritoneal mesothelial cells by peritoneal dialysis fluid. Clin Exp Immunol. 2004;136:85–94. doi:10.1111/j.1365-2249.2004.02407.x
13. Young GA, Kendall S, Brownjohn AM. Complement activation during CAPD. Nephrol Dial Transplant. 1993;8:1372–1375.
14. Poppelaars F, Faria B, Gaya da Costa M, et al. The complement system in dialysis: a forgotten story? Front Immunol. 2018;9:71. doi:10.3389/fimmu.2018.00071
15. Reddingius RE, Schroder CH, Daha MR, Willems HL, Koster AM, Monnens LA. Complement in serum and dialysate in children on continuous ambulatory peritoneal dialysis. Perit Dial Int. 1995;15:49–53. doi:10.1177/089686089501500110
16. Sritippayawan S, Chiangjong W, Semangoen T, et al. Proteomic analysis of peritoneal dialysate fluid in patients with different types of peritoneal membranes. J Proteome Res. 2007;6:4356–4362. doi:10.1021/pr0702969
17. Hirahara I, Inoue M, Okuda K, Ando Y, Muto S, Kusano E. The potential of matrix metalloproteinase-2 as a marker of peritoneal injury, increased solute transport, or progression to encapsulating peritoneal sclerosis during peritoneal dialysis--A multicentre study in Japan. Nephrol Dial Transplant. 2007;22:560–567. doi:10.1093/ndt/gfl566
18. Huang G, Wang Y, Shi Y, et al. The prognosis and risk factors of baseline high peritoneal transporters on patients with peritoneal dialysis. J Cell Mol Med. 2021;25:8628–8644. doi:10.1111/jcmm.16819
19. Brimble KS, Walker M, Margetts PJ, Kundhal KK, Rabbat CG. Meta-analysis: peritoneal membrane transport, mortality, and technique failure in peritoneal dialysis. J Am Soc Nephrol. 2006;17:2591–2598. doi:10.1681/ASN.2006030194
20. Davies SJ. Overfill or ultrafiltration? We need to be clear. Perit Dial Int. 2006;26:449–451. doi:10.1177/089686080602600408
21. Barbano G, Cappa F, Prigione I, et al. Peritoneal mesothelial cells produce complement factors and express CD59 that inhibits C5b-9-mediated cell lysis. Adv Perit Dial. 1999;15:253–257.
22. Sei Y, Mizuno M, Suzuki Y, et al. Expression of membrane complement regulators, CD46, CD55 and CD59, in mesothelial cells of patients on peritoneal dialysis therapy. Mol Immunol. 2015;65:302–309. doi:10.1016/j.molimm.2015.02.005
23. Yanez-Mo M, Lara-Pezzi E, Selgas R, et al. Peritoneal dialysis and epithelial-to-mesenchymal transition of mesothelial cells. N Engl J Med. 2003;348:403–413. doi:10.1056/NEJMoa020809
24. Goswami MT, Reka AK, Kurapati H, et al. Regulation of complement-dependent cytotoxicity by TGF-beta-induced epithelial-mesenchymal transition. Oncogene. 2016;35:1888–1898. doi:10.1038/onc.2015.258
25. Otsuki T, Fukuda N, Chen L, Tsunemi A, Abe M. Twist-related protein 1 induces epithelial-mesenchymal transition and renal fibrosis through the upregulation of complement 3. PLoS One. 2022;17:e0272917.
26. Agarwal DK, Sharma AP, Gupta A, et al. Peritoneal equilibration test in Indian patients on continuous ambulatory peritoneal dialysis: does it affect patient outcome? Adv Perit Dial. 2000;16:148–151.
27. Chung SH, Chu WS, Lee HA, et al. Peritoneal transport characteristics, comorbid diseases and survival in CAPD patients. Perit Dial Int. 2000;20:541–547. doi:10.1177/089686080002000509
28. Asano M, Ishii T, Hirayama A, et al. Differences in peritoneal solute transport rates in peritoneal dialysis. Clin Exp Nephrol. 2019;23:122–134. doi:10.1007/s10157-018-1611-1
29. Liu Y, Huang R, Guo Q, et al. Baseline higher peritoneal transport had been associated with worse nutritional status of incident continuous ambulatory peritoneal dialysis patients in Southern China: a 1-year prospective study. Br J Nutr. 2015;114:398–405. doi:10.1017/S0007114515001804
30. Kang DH, Yoon KI, Choi KB, et al. Relationship of peritoneal membrane transport characteristics to the nutritional status in CAPD patients. Nephrol Dial Transplant. 1999;14:1715–1722. doi:10.1093/ndt/14.7.1715
31. Margetts PJ, McMullin JP, Rabbat CG, Churchill DN. Peritoneal membrane transport and hypoalbuminemia: cause or effect? Perit Dial Int. 2000;20:14–18. doi:10.1177/089686080002000104
32. John B, Tan BK, Dainty S, Spanel P, Smith D, Davies SJ. Plasma volume, albumin, and fluid status in peritoneal dialysis patients. Clin J Am Soc Nephrol. 2010;5:1463–1470. doi:10.2215/CJN.09411209
33. Lim PS, Chen HP, Chen CH, Wu MY, Wu CY, Wu TK. Association between redox status of serum albumin and peritoneal membrane transport properties in patients on peritoneal dialysis. Blood Purif. 2015;40:243–249. doi:10.1159/000439240
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Lectin Complement Pathway Activation is Associated with Massive Proteinuria in PLA2R-Positive Membranous Nephropathy: A Retrospective Study
Li J, Zhang J, Wang X, Zheng X, Gao H, Jiang S, Li W
International Journal of General Medicine 2023, 16:1879-1889
Published Date: 17 May 2023