Back to Journals » Clinical Ophthalmology » Volume 18
Long Term Visual Outcomes of an Extended Macular Vision IOL in Eyes with Macular Disease and Visually Insignificant Cataract
Authors Badalà F, Bona E, Devincenzi G, Nouri-Mahdavi K
Received 5 June 2024
Accepted for publication 30 September 2024
Published 4 October 2024 Volume 2024:18 Pages 2765—2775
DOI https://doi.org/10.2147/OPTH.S481570
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Federico Badalà,1 Elena Bona,1 Giulia Devincenzi,1 Kouros Nouri-Mahdavi2
1Micro Chirurgia Oculare, Eye Clinic, Milan, Italy; 2Glaucoma Division, Stein Eye Institute, David Geffen School of Medicine, University of California Los Angeles, Los Angeles, CA, USA
Correspondence: Federico Badalà, Email [email protected]
Purpose: To determine long-term efficacy and safety of an extended macular vision intraocular lens (IOL) implanted in patients with dry age-related macular degeneration (AMD) and visually insignificant cataracts.
Design: Retrospective observational case series.
Setting: MicroChirurgia Oculare, Italy.
Methods: A retrospective case series of patients with dry AMD and visually insignificant cataracts undergoing phacoemulsification and implantation of an extended macular vision IOL designed to optimize image quality up to 10° from the foveal center (EyeMax Mono, Sharpview Ophthalmology, London, UK). Criteria for implantation were visually insignificant cataract (NC1 according to LOCS III classification) with dry age-related macular degeneration. Hypermetropia was targeted in most eyes to provide magnification when corrected with spectacles. Primary outcome measures were changes in corrected distant and secondary outcome measures included near visual acuity (CDVA and CNVA, respectively) between baseline and latest follow-up and safety outcomes.
Results: 113 eyes of 86 patients (mean age 70.3± 7.9 years) were included (mean follow-up: 48.3± 25.1 months). Mean CDVA improved by 0.22 logMAR (11 ETDRS letters), from 0.53± 0.4 to 0.31± 0.3 (n=113, p< 0.001). Similarly, mean CNVA improved by 0.08 logMAR (4 ETDRS letters), from 0.45± 0.2 to 0.37± 0.2 (n=77, p< 0.001). Eleven eyes had AMD with extensive atrophy, and their mean CDVA improved by 0.32 logMAR (16 ETDRS letters). Three eyes (2.7%) experienced loss of more than one line in logMAR CDVA and four eyes (5.2%) experienced loss of more than one line in logMAR CNVA. No complications or instances of IOL exchange were reported.
Conclusion: Visual improvement in eyes with visually insignificant cataract and AMD who underwent phacoemulsification and were implanted with EyeMax Mono IOL appears to be influenced by the IOL optical design. Vision enhancement in eyes with visually insignificant cataracts underscores the IOL’s ability to optimize use of healthy retinal areas. Prospective studies with control groups are needed to confirm these findings.
Keywords: AMD, Age macular degeneration, extended macular vision IOL, IOL, preferred retinal locus, PRL
Introduction
Central vision loss refers to the impairment or loss of the central portion of the visual field, which is responsible for sharp vision and the ability to perceive fine details, recognize faces, and read text.1 Loss of central vision occurs due to macular diseases such as age-related macular degeneration (AMD), Stargardt disease, and diabetic retinopathy.2 Blindness due to AMD alone affects 2–3% of the US population aged >50 years.3 It is estimated that by 2040, 288 million people will suffer from AMD worldwide.4 Loss of central vision can significantly impact an individual’s quality of life.
Patients with macular diseases such as AMD usually develop an adaptive mechanism to overcome central vision loss by selecting a preferred retinal locus (PRL). PRL allows a patient with a damaged macula to use a different part of the macula other than the fovea. In other words, the brain locates a healthy region of the macula and uses it as an alternative to the fovea. Unfortunately, when this occurs, vision is less crisp because the PRL outside the fovea does not naturally provide the same quality of vision as that of the fovea. However, the brain automatically selects a PRL that provides the sharpest vision that can be achieved in patients with macular pathology.5,6 PRLs can be evaluated using microperimetry to assess fixation stability through indices, such as bivariate contour ellipse areas (BCEA 63% and BCEA 95%). Microperimetry also determines the PRL’s location relative to the fovea, providing valuable insights into the patient’s visual function.7 Corresponding PRLs in both eyes need to be developed for achieving useful binocular vision.8
Different solutions have been proposed to help patients with central vision loss, including low-vision aids and intraocular telescopes. Low vision aids such as hand/stand magnifiers and closed-circuit televisions, though effective, have several limitations because they are cumbersome to use and cosmetically unappealing.9 Implantable devices such as implantable miniature telescopes (IMT), and the intraocular lens for visually impaired people (IOL-VIP) system surpass the limitations of low vision aids by creating a magnified retinal image. However, drawbacks include a limited field of view, potential complications such as endothelial cell loss, and the need for post-surgical PRL training making careful patient selection crucial.10 Furthermore, the use of intraocular telescopes requires a larger corneal incision and advanced surgical skills.10,11
Patients with macular disorders who require cataract surgery are usually implanted with standard IOLs, often monofocal models, and vision is subsequently optimized with glasses. Unfortunately, monofocal IOLs tightly focus light on the fovea (up to 4 degrees of retinal eccentricity),12 an area that may already be affected by the pathology.13,14
To the best of our knowledge, the EyeMax Mono (Sharpview Ophthalmology, London, UK) is currently the only extended macular vision (EMV) IOL, reported in the scientific literature and commercially available to surgeons in Europe. It was specifically designed to enhance the image quality at the PRL located within 10° of eccentricity. It aims to help the patient to develop a single or multiple PRLs in potentially unaffected areas of the retina.15 It is a single-piece, soft, hydrophobic acrylic IOL similar to standard monofocal IOLs in implantation technique and safety profile but it features wavefront-optimized optics designed to broaden the focus and minimize image blurring in a large area of the retina.12,15
Previous studies have primarily focused on the short-term efficacy and safety of the EyeMax Mono IOL, predominantly in cases of age-related macular degeneration (AMD) in a variety of patients.12,15,16 This study investigated the visual outcomes of this EMV IOL in patients who preoperatively had visually insignificant cataracts and were diagnosed with AMD to isolate the effectiveness of the IOL alone.
At the time of this study (2024), the EyeMax Mono IOL is not yet FDA-approved, but it is CE-marked, so licensed for use in the European Union.
Methods
Study Design
This retrospective observational study investigated the visual outcomes of EyeMax Mono IOL in patients with dry AMD (intermediate grade or more severe). Local ethics approval (Micro Chirurgia Oculare, Milan, Italy) was obtained for this retrospective consecutive case series, which adhered to the tenets of the Declaration of Helsinki. Each patient provided written informed consent after the nature of the procedure and options had been discussed. All surgeries were performed by a single surgeon (FB) between June 2016 and June 2023.
Patients
The study recruited a cohort of individuals who preoperatively had center-involving maculopathy (intermediate AMD or worse) and visually insignificant cataracts (NC1 according to the LOCS III classification),17,18 and underwent cataract extraction with EyeMax Mono IOL implantation to optimize visual acuity between June 2016 and June 2023. AMD was graded according to AREDS study,19 where intermediate AMD is defined as having one or more large (≥125 μm) drusen and/or extensive intermediate (≥63 μm but < 125 μm) drusen.
Included eyes must have healthy retina within 2 disc-diameters from the fovea. Visual results of eyes with AMD with extensive atrophy were discussed separately as they were not expected to improve by cataract removal.20 These eyes exhibited fovea-involving geographic atrophy or had geographic atrophy measuring at least one disc area (AREDS grade 6 or 7).21
Eyes with a non-functional retina located approximately within 2-disc diameters (equivalent to 10 degrees) from the foveal center were excluded. Other exclusion criteria were the presence of wet AMD or any other visual condition that might interfere with visual outcomes such as glaucoma, and corneal diseases.
Patient consent was obtained in line with standard practice relating to cataract surgery in the context of macular disease, specifically with regard to the limited benefits where there was extensive central macular involvement and the potential advantages of image optimization where there was an existing preferred retinal locus or the potential for becoming dependent on one in the future. Patients were informed of the limitations of optical approaches in the context of progressive disease and expected progressive loss of vision due to the underlying retinal disease; patients were also informed that IOL implantation would have no effect on the progression of the retinal pathology, and the only intention of the surgery was the optimization of their existing vision quality.
All subjects underwent baseline and postoperative assessment of corrected distance (decimal converted to logMAR) and near visual acuity (Jaeger chart converted to logMAR22), manifest refraction, intraocular pressure measurement (Goldmann applanation tonometry), macular optical coherence tomography (Spectralis, Heidelberg Engineering, Germany) and examination of the anterior segment and dilated fundus.
Cataract subtype and density were graded by one surgeon (FB) and one optometrist, according to the LOCS III scale;17 only eyes with visually insignificant cataract18 and no posterior subcapsular cataract were included in this analysis to isolate the effect of the EyeMax Mono IOL from the visual improvement achieved by removing the cataract.
The primary outcome measure was the change in corrected distance visual acuity (CDVA) from the baseline to the last follow-up. Secondary outcome measures included the change in corrected near visual acuity (CNVA) from baseline to the last follow-up, as well as safety, which was assessed in accordance with the American Academy of Ophthalmology Cataract in the Adult Eye Preferred Practice Pattern.23
The EyeMax Mono IOL
The EyeMax Mono IOL is a CE-marked single piece that is currently available in Europe. It is an injectable, hydrophobic, acrylic extended macular vision intraocular lens designed for placement in the capsular bag.
Laboratory simulations demonstrate that the IOL produces high-quality images at 4° and 7.5° from the fovea indicating its optimization for extended macular vision.15
The intraocular lens (IOL) incorporates a hyperaspheric design, which builds upon the concept of aspheric lenses to minimize optical distortions near the lens periphery. The lens optics are wavefront-optimised to minimise image blur across all areas of the macula extending 10 degrees from the foveal centre;15,24 this is opposed to standard monofocal IOLs, where image quality is poor outside the central 4 degrees from the foveal centre (Figure 1).12 For the EMV IOL, as the dioptric power of the IOL increases, the posterior surface of the lens becomes more curved while the anterior surface changes the sign of the curvature, running from positive curvature to a flatter curvature and then negative curvature; details of the extended macular vision IOL have been described in the literature.12
 |
Figure 1 EyeMax Mono field of optimization. |
Surgical Intervention
A modest hypermetropic postoperative refraction was targeted, depending on the severity of the macular disease and refraction in the unoperated eye at the surgeon’s discretion. For example, +2 D of hypermetropia after surgery creates approximately 1.2x spectacle-corrected magnification with a reading addition. Such patients were counselled that they would be more dependent on single-vision distance and near glasses postoperatively.
The intraocular lens power was estimated using the Haigis formula and an A-constant of 119.2. Implantation was performed via standard phacoemulsification cataract surgery (CENTURION® Vision System, Alcon, Fort Worth, Texas, USA) under topical and intracameral anesthesia. The extended macular vision IOL was injected into the capsular bag via a 2.7 mm clear corneal incision. Subjects were managed with a standard postoperative regimen of dexamethasone 0.1% eye drops, four times daily, tapered over a month, and a topical antibiotic for two weeks.
Statistical Analyses
Statistical analysis was performed using the SPSS software version 23 (IBM, Armonk, USA). Descriptive statistics, in the form of mean±standard deviation, were used to summarize the changes in CDVA and CNVA. A paired nonparametric test (Wilcoxon signed-rank test) was used to compare CDVA and CNVA preoperatively versus the last follow-up. Comparisons of different groups at the same time points were performed using Welch’s t-test. The Shapiro–Wilk test was used to determine normality. Pearson’s correlation coefficient was used to estimate the correlation between the numerical data. A p<0.05 was considered statistically significant.
Results
Data from 113 eyes of 86 patients were analyzed. All surgeries were performed between March 2016 and July 2023. The mean age was 70.3±7.9 years (range: 46–87; median: 72). Males accounted for 51.2% of the study cohort. All the eyes had dry AMD (intermediate AMD or worse). One patient had dry AMD at a relatively young age (46 years) due to occupational sun exposure25 and was followed up for 76 months. Eleven eyes (9.7%) had extensive atrophy (geographic atrophy with a size of ≥ 2-disc diameter involving the fovea). We have created this subgroup since they have the worst prognosis and are not likely to improve by cataract removal.20 The mean follow-up duration for all eyes was 48.3±25.1 months (range: 1–85; median: 56). Table 1 presents demographic data.
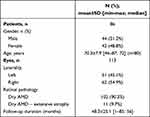 |
Table 1 Demographics |
Efficacy
Table 2 shows the mean improvement in the visual and refractive outcomes following IOL implantation. CDVA (logMAR) significantly improved from 0.53±0.4 to 0.31±0.3 (n=113; p<0.001), which is equivalent to a mean improvement of 11 ETDRS letters. CNVA (logMAR) significantly improved from 0.45±0.2 to 0.37±0.2 (4 ETDRS letters) (n=77; p<0.001). Mean preoperative spherical equivalent (SE) was −0.35±2.6 D (range: −9.9 to +3.4; median: 0.3; n=109); mean postoperative SE was +2.13±1.0 D (range: −1.5 to +4.3; median: +2.1; n=108).
CDVA (logMAR) changes: 107 eyes (94.7%) gained one line or more, 3 eyes (2.65%) had no change, and 3 eyes (2.65%) lost one or more lines. CNVA (logMAR) changes: 39 eyes (50.6%) gained one or more lines, 30 eyes (39.0%) had no change, and 8 eyes (10.4%) lost one or more lines. Thirty-nine eyes (34.5%) gained three or more lines of CDVA and 12 eyes (15.6%) gained three or more lines of CNVA (Figure 2A). Baseline OCT images of certain eyes that demonstrated notable improvements in CDVA are displayed in Figure 3.
 |
Figure 2 (A) Gain/loss of CDVA and CNVA lines. (B) Gain/loss of CDVA and CNVA lines grouped by severity. |
Nine eyes were rendered emmetropic (SE<1D) postoperatively, excluding the effect of magnification obtained by correcting postoperative hypermetropia. Their mean postoperative SE was −0.10±0.8 D (n=9) while their baseline SE was −5.35±3.0 D (n=9). Their CDVA (logMAR) significantly improved from 0.42±0.3 to 0.19±0.2 (n=9) (p=0.004) and their CNVA (logMAR) was 0.32±0.1 at baseline and 0.28±0.1 (n=7) at the latest follow-up (p=0.269).
Correlations
There was a trend towards greater changes in CDVA in patients with poorer baseline CDVA (Pearson’s r=0.412; p<0.001); similarly, a greater CNVA change (improvement) was noticed in eyes with worse preoperative CNVA (Pearson’s r=0.453; p<0.001). Additionally, both postoperative CDVA and CNVA were strongly correlated with their respective preoperative values (Pearson’s r=0.852, p<0.001 and Pearson’s r=0.657, p<0.001, respectively).
The following correlations were also observed between preoperative and postoperative measurements: preoperative CDVA is strongly correlated to both preoperative and postoperative CNVA (Pearson’s r=0.575; p<0.001 and Pearson’s r=0.646; p<0.001, respectively); postoperative CDVA is strongly correlated to both preoperative and postoperative CNVA (Pearson’s r=0.543; p<0.001 and Pearson’s r=0.714; p<0.001, respectively). Notably, follow-up duration were not correlated with postoperative CDVA or CNVA.
When classified in the groups based on severity, in the dry AMD group, postoperative CDVA was again strongly correlated to preoperative CDVA (Pearson’s r=0.744; p<0.001), preoperative CNVA (Pearson’s r=0.450; p<0.001), and postoperative CNVA (Pearson’s r=0.647; p<0.001). Similarly, postoperative CNVA strongly correlated with preoperative CDVA (Pearson’s r=0.532; p<0.001) and preoperative CNVA (Pearson’s r=0.571; p<0.001). In contrast, due to the small sample size and missing data in the AMD with extended atrophy group, the postoperative CDVA was only strongly correlated with the preoperative CDVA (Pearson’s r = 0.949; p < 0.001).
In Table 3 and Figure 2B, eyes are categorized based on AMD severity, with a distinct group for those exhibiting extensive atrophy due to their poor prognosis. Both groups showed significant improvement in CDVA (0.21 logMAR for Dry AMD group and 0.32 logMAR for Dry AMD with extensive atrophy group), whereas the dry AMD group showed significant improvement in CNVA. The group “Dry AMD – extensive atrophy” (n=2) was not sufficiently powered to return a statistically significant result for CNVA. Overall, CDVA improved better than CNVA (Figure 2b).
As shown in Table 4, the improvement in CDVA in eyes that had visually insignificant cataract was maintained up to 96 months (p<0.001).
Safety
No intra- or postoperative complications were identified, and there were no issues with IOL implantation. None of the eyes required IOL exchange and there were no reported cases of diplopia or dysphotopsia. Mean intraocular pressure (IOP) was stable: 13.9±1.7 mmHg preoperatively and 13.8±1.9 mmHg postoperatively (p=0.54, n=112).
Discussion
Central vision loss caused by AMD impacts individuals’ daily activities, leading to emotional, social, and economic consequences such as decreased independence, reduced quality of life, and increased depression.24 Managing central vision loss is crucial to alleviate its burden on affected individuals and society.
The primary objective of the current study was to evaluate the improvement in CDVA achieved by the EyeMax Mono EMV IOL in patients with moderate AMD or worse over an extended period of time. Eyes with NC1 cataract were selected to provide a clearer understanding of the lens’s effectiveness in improving vision for AMD patients, in isolation from the removal of the cataract. According to Chew et al, cortical cataract less than grade 3 does not affect the vision.18 Early cases of AMD were also not included in the study because far visual acuity under photopic conditions is barely affected at this stage.26
One hundred and thirteen eyes were included in this study. The primary outcome of the current study was the change in CDVA between baseline and the last follow-up. After a mean of 48.3 months, mean CDVA improved by 0.22 logMAR (p<0.001), which is less than the mean improvement achieved in a study by Qureshi et al on 244 eyes (0.35 logMAR after 3 months).15 This can be justified by fact that Qureshi et al recruited patient with cataracts and with a lower mean baseline CDVA in their study (1.06 logMAR in their study vs 0.53 logMAR in the current study); indeed, in the current study we observed that a lower baseline visual acuity was correlated with a greater gain in visual acuity (Pearson’s r=0.412; p<0.001). In addition, the current study excluded the effect of cataract removal by selecting eyes with visually insignificant cataract, whereas the cataract degree was not specified in the study by Qureshi et al.
The main finding of this study is the visual improvement of eyes with visually insignificant cataract, and the visual outcome in these eyes isolates the optical effect of the IOL from the effect of cataract removal. Both CDVA and CNVA significantly improved by a mean of 0.22 logMAR and 0.07 logMAR, respectively. In 2018, Hengerer et al assessed the effect of the sulcal implantation of a lens of the same optical design of the EyeMax Mono in 22 pseudophakic eyes, with moderate to severe dry AMD, stable wet AMD, or disciform scar, and reported an improvement in CDVA of 0.39 logMAR.27 Similarly, in the current study, 11 eyes of the NC1 group had dry AMD with extensive maculopathy, and those eyes achieved an improvement of 0.32 logMAR.
The CDVA improvement in dry AMD with extensive atrophy cases is particularly meaningful since it was not expected to improve visual acuity in cases with extensive geographic atrophy.20 Baseline OCT images of patients with extensive AMD-related atrophy who experienced notable improvements in CDVA are displayed in Figure 3b–d.
Previous studies on the EyeMax Mono IOL had relatively short follow-up periods, with the longest postoperative follow-up period of 6 months. Since new PRLs can take up to 6 months to fully develop in old age,28,29 a longer follow-up might reveal better visual improvement. In the current study, eyes were followed up for 48.3±25.1 months (range: 1–85 months; median: 56 months). This study also aimed to determine whether visual acuity gains in the eyes were eroded by the progressive nature of retinal diseases (Table 4). Interestingly, eyes that were followed up the longest (61–96 months) still showed a significant improvement in CDVA of 0.23±0.2 logMAR (n=50, p<0.001) as compared to preoperative values. We hypothesized that the large area of focus provided by the EMV IOL design allows the brain to find new PRLs despite the progression of retinal pathology. This can provide hope to those who lose their central vision at a young age. Indeed, one of our patients was diagnosed with AMD at a relatively young age due to occupational sun exposure,25 was followed for 76 months, and had CDVA improved from logMAR 0.3 to logMAR 0.12 at the last follow-up.
Interestingly, according to Table 4, the mean postoperative CDVA was better in eyes with follow-up at 31–96 months than in eyes with 1–30 months although the difference was not statistically significant (p=0.193).
Despite no significant difference between the different follow-up groups at baseline, it seems that preoperative CDVA was worst in the earliest cases (Table 4); speculatively, the reason is that we began by implanting the IOL in the most severe maculopathy cases, and as we observed positive outcomes in these patients, we started including less severe cases as well. Nevertheless, this observation is consistent with our finding that patients with poorer preoperative CDVA experienced greater improvement after surgery.
It could be argued that the improvement in visual acuity in extended macular vision IOL implantation is due to magnification achieved by spectacle correction of postoperative hypermetropia. Indeed, the refractive target in most cases was +2D to +3.5D, which is expected to give up to 1.2x magnification. However, 9 eyes had postoperative SE <1D. Their CDVA significantly improved by 0.23 logMAR (p=0.004) indicating that in addition to the magnification, the design of the EMV IOL that optimizes vision in the whole macula contributes to the improvement of vision in eyes with spectacle-corrected hypermetropia postoperatively.
Patients with a lower baseline CDVA showed a trend toward greater postoperative gains (Pearson’s r=0.412; p<0.001). Similarly, worse preoperative CNVA was associated with greater postoperative improvement (Pearson’s r=0.453; P <0.001). Notably, follow-up duration were not correlated to both CDVA and CNVA at the last follow-up, suggesting that the progressive nature of the disease did not compromise the CDVA and CNVA gains achieved by the EMV IOL.
The safety of the EyeMax Mono IOL has been established in previous research.12,15,27 In this cohort, only three eyes (2.7%) lost one or more lines of CDVA, and four eyes (5.2%) lost one or more lines of CNVA. This may be attributed to the progression of the retinal pathology. No significant changes were noted in the IOP.
Compared with other IOLs for AMD patients such as the IOL-AMD system, which provides similar magnification (1.3x),30,31 EyeMax Mono requires a smaller capsulorrhexis (2.7 mm vs 6 mm for IOL-VIP)31 because the latter is thicker, consisting of two IOLs. Moreover, a preoperative iridotomy is required with IOL-VIP system to avoid the risk of pupillary block.31 Additionally, the outcomes of the IOL-VIP system depend on a rehabilitation program for PRL training, which is not necessary for the EyeMax Mono IOL.30,31 In one study on IOL-VIP system, 40 eyes with central scotoma due to a macular disease showed a mean improvement in logMAR CDVA from 1.28 to 0.77,31 which is greater than the CDVA gain in the current study (from 0.53±0.4 to 0.31±0.3), perhaps because the baseline CDVA was worse. It is expected that eyes with worse CDVA will experience greater postoperative CDVA gains, as evidenced by the group with extensive atrophy that improved from 1.11±0.5 to 0.79±0.5.
One limitation of this study is its retrospective design, which did not allow for the collection of additional objective data, such as OCT angiography, contrast sensitivity, and microperimetry, nor did it permit the assessment of the impact of the IOL on the quality of life. Other limitations are the lack of CNVA data in several eyes and that binocular visual acuity was not reported in the cohort who had the IOL implanted in both eyes – which could have given additional indications of functional vision. In the study by Hengerer et al, binocular visual acuity was found to improve over time due to neuroadaptation.27
In this study, we examined the effect of EyeMax Mono IOL implantation in individuals who preoperatively had visually insignificant cataracts and center-involving maculopathy - intermediate AMD or worse. The observed improvement suggests the effectiveness of the IOL’s ability to utilize unaffected retinal areas for better vision. These enhancements emphasize the role of the IOL’s optical design in optimizing visual outcomes, independent of cataract removal or magnification adjustments through spectacles.
Future research and prospective studies with a control group are needed to verify these findings and shed light on the contribution of the EyeMax Mono IOL optical design to visual improvements, including contrast sensitivity, in addition to distant and near visual acuity, and to refine treatment options for those with central vision loss due to various macular lesions. Additionally, future research should include an evaluation of the effect of EMV IOL implantation on patients’ quality of life as well as the change in microperimetry after implanting an EMV IOL, which was not recorded in our study.
Summary
An extended macular vision IOL designed to optimize image quality across a wider macular area was found to be safe and effective, delivering superior long-term visual outcomes in patients with central vision loss.
Acknowledgments
Editorial assistance was provided by GP Communications and was funded by Sharpview Ophthalmology (London, UK). The funder was not involved with the data collection, analysis, or interpretation, and did not influence the results of the study.
Disclosure
Dr Kouros Nouri-Mahdavi reports grants from Heidelberg Engineering, honoraria from Topcon Healthcare, outside the submitted work. The authors have no financial or proprietary interest in any of the materials or methods mentioned. No financial support was received for this study.
References
1. Sverdlichenko I, Mandelcorn MS, Issashar Leibovitzh G, Mandelcorn ED, Markowitz SN, Tarita‐Nistor L. Binocular visual function and fixational control in patients with macular disease: a review. Ophthalmic Physiol Opt. 2022;42(2):258–271. doi:10.1111/opo.12925
2. CHEUNG SH, LEGGE GE. Functional and cortical adaptations to central vision loss. Vis Neurosci. 2005;22(2):187–201. doi:10.1017/S0952523805222071
3. Jager RD, Mieler WF, Miller JW. Age-Related Macular Degeneration. N Engl J Med. 2008;358(24):2606–2617. doi:10.1056/NEJMra0801537
4. Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(2). doi:10.1016/S2214-109X(13)70145-1
5. Crossland MD, Engel SA, Legge GE. THE PREFERRED RETINAL LOCUS IN MACULAR DISEASE. Retina. 2011;31(10):2109–2114. doi:10.1097/IAE.0b013e31820d3fba
6. Van der Stigchel S, Bethlehem RAI, Klein BP, TTJM B, Nijboer TCW, Dumoulin SO. Macular degeneration affects eye movement behavior during visual search. Front Psychol. 2013;4. doi:10.3389/fpsyg.2013.00579
7. Tarita-Nistor L, González EG, Markowitz SN, Steinbach MJ. Fixation Characteristics Of Patients With Macular Degeneration Recorded With The Mp-1 Microperimeter. Retina. 2008;28(1):125–133. doi:10.1097/IAE.0b013e3180ed4571
8. GREENSTEIN VC, V. SANTOSRA, TSANG SH, SMITH RT, BARILE GR, SEIPLE W. Preferred Retinal Locus In Macular Disease. Retina. 2008;28(9):1234–1240. doi:10.1097/IAE.0b013e31817c1b47
9. Altpeter EK, Nguyen NX. Bedarf an vergrößernden Sehhilfen bei altersbedingter Makuladegeneration. Der Ophthalmologe. 2015;112(11):923–928. doi:10.1007/s00347-015-0062-2
10. Grzybowski A, Wasinska-Borowiec W, Alio JL, Amat-Peral P, Tabernero J. Intraocular lenses in age-related macular degeneration. Graefes Arch Clin Exp Ophthal. 2017;255(9):1687–1696. doi:10.1007/s00417-017-3740-8
11. Dunbar HMP, Dhawahir-Scala FE. A Discussion of Commercially Available Intra-ocular Telescopic Implants for Patients with Age-Related Macular Degeneration. Ophthalmol Ther. 2018;7(1):33–48. doi:10.1007/s40123-018-0129-7
12. Robbie SJ, Tabernero J, Artal P, Qureshi MA. Initial Clinical Results With a Novel Monofocal-Type Intraocular Lens for Extended Macular Vision in Patients With Macular Degeneration. J Refract Surg. 2018;34(11):718–725. doi:10.3928/1081597X-20180831-01
13. Kessel L, Erngaard D, Flesner P, Andresen J, Tendal B, Hjortdal J. Cataract surgery and age‐related macular degeneration. An evidence‐based update. Acta Ophthalmol. 2015;93(7):593–600. doi:10.1111/aos.12665
14. Casparis H, Lindsley K, Kuo IC, Sikder S, Bressler NM. Surgery for cataracts in people with age-related macular degeneration. Cochrane Database Syst Rev. 2017;2017(2). doi:10.1002/14651858.CD006757.pub4
15. Qureshi MA, Robbie SJ, Hengerer FH, Auffarth GU, Conrad-Hengerer I, Artal P. Consecutive case series of 244 age-related macular degeneration patients undergoing implantation with an extended macular vision IOL. Eur J Ophthalmol. 2018;28(2):198–203. doi:10.5301/ejo.5001052
16. Borkenstein AF, Borkenstein EM. A case report detailing use of a new intraocular lens with advanced technology, designed specifically for patients with center-involving macular disorders. Medicine. 2019;98(30):e16583. doi:10.1097/MD.0000000000016583
17. Chylack LT. The Lens Opacities Classification System III. Archives of Ophthal. 1993;111(6):831. doi:10.1001/archopht.1993.01090060119035
18. Chew M, Chiang PPC, Zheng Y, et al. The Impact of Cataract, Cataract Types, and Cataract Grades on Vision-Specific Functioning Using Rasch Analysis. Am J Ophthalmol. 2012;154(1):29–38.e2. doi:10.1016/j.ajo.2012.01.033
19. Forooghian F, Agrón E, Clemons TE, Ferris FL, Chew EY. Visual Acuity Outcomes after Cataract Surgery in Patients with Age-Related Macular Degeneration: age-Related Eye Disease Study Report No. 27. Ophthalmology. 2009;116(11):2093–2100. doi:10.1016/j.ophtha.2009.04.033
20. Chen AX, Haueisen A, Rasendran C, et al. Visual outcomes following cataract surgery in age-related macular degeneration patients. Can J Ophthalmol. 2021;56(6):348–354. doi:10.1016/j.jcjo.2021.01.018
21. Davis MD, Gangnon RE, Lee LY, et al. The Age-Related Eye Disease Study severity scale for age-related macular degeneration: AREDS Report No. 17. Arch Ophthalmol. 2005;123(11):1484–1498. doi:10.1001/archopht.123.11.1484
22. Runge PE. Eduard Jaeger’s Test-Types (Schrift-Scalen) and the historical development of vision tests. Trans Am Ophthalmol Soc. 2000;98:375.
23. Olson RJ, Braga-Mele R, Chen SH, et al. Cataract in the Adult Eye Preferred Practice Pattern®. Ophthalmology. 2017;124(2):P1–P119. doi:10.1016/j.ophtha.2016.09.027
24. Borkenstein AF, Borkenstein EM, Persson S, Muus G, Nielsen NV. Improving Outcomes for Patients with Age-Related Macular Degeneration and Cataracts: the Importance of Including an Assessment of Activities of Daily Life (ADL). Clin Ophthalmol. 2021;15:3333–3339. doi:10.2147/OPTH.S327274
25. Sui GY, Liu GC, Liu GY, et al. Is sunlight exposure a risk factor for age-related macular degeneration? A systematic review and meta-analysis. Br J Ophthalmol. 2013;97(4):389–394. doi:10.1136/bjophthalmol-2012-302281
26. Scilley K, Jackson GR, Cideciyan AV, Maguire MG, Jacobson SG, Owsley C. Early age-related maculopathy and self-reported visual difficulty in daily life. Ophthalmology. 2002;109(7):1235–1242. doi:10.1016/S0161-6420(02)01060-6
27. Hengerer FH, Auffarth GU, Robbie SJ, Yildirim TM, Conrad-Hengerer I. First Results of a New Hyperaspheric Add-on Intraocular Lens Approach Implanted in Pseudophakic Patients with Age-Related Macular Degeneration. Ophthalmol Retina. 2018;2(9):900–905. doi:10.1016/j.oret.2018.02.003
28. Crossland MD, Culham LE, Kabanarou SA, Rubin GS. Preferred Retinal Locus Development in Patients with Macular Disease. Ophthalmology. 2005;112(9):1579–1585. doi:10.1016/j.ophtha.2005.03.027
29. Costela FM, Reeves SM, Woods RL. Orientation of the preferred retinal locus (PRL) is maintained following changes in simulated scotoma size. J Vis. 2020;20(7):25. doi:10.1167/jov.20.7.25
30. Singer M, Herro A, Probandarwalla SS, et al. Improving quality of life in patients with end-stage age-related macular degeneration: focus on miniature ocular implants. Clin Ophthalmol. 2011:33. doi:10.2147/OPTH.S15028
31. Orzalesi N, Pierrottet CO, Zenoni S, Savaresi C. The IOL-Vip System. Ophthalmology. 2007;114(5):860–865.e1. doi:10.1016/j.ophtha.2007.01.005
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





