Back to Journals » International Medical Case Reports Journal » Volume 18
Metastatic Adamantinoma of Fibula to the Lungs: A Rare Case Report
Authors Knaj D, Ahmad G, Alshehabi Z, Ahmad IY
Received 29 April 2025
Accepted for publication 15 July 2025
Published 18 July 2025 Volume 2025:18 Pages 909—914
DOI https://doi.org/10.2147/IMCRJ.S535403
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Thomas E Hutson
Duaa Knaj,1 Ghanem Ahmad,2 Zuheir Alshehabi,3 Issa Yusuof Ahmad3
1Department of Oncology, Tishreen University, Latakia, Syrian Arab Republic; 2Department of Vascular Surgery, Tishreen University, Latakia, Syrian Arab Republic; 3Department of Pathology, Tishreen University, Latakia, Syrian Arab Republic
Correspondence: Duaa Knaj, Tishreen University, Latakia, Syrian Arab Republic, Email [email protected]
Background: Adamantinoma is a low-grade, primary malignant bone tumor commonly found in the tibia with or without fibular involvement.
Case Presentation: A 21-year-old female patient was admitted to the hospital with a mass on the upper lateral aspect of the left leg. She reported the onset of a small swelling in the left leg eight months prior to admission. It has gradually increased in size to involve the upper leg and part of the knee. The patient had limited range of motion in the knee joint and difficulty leaning on the affected limb. Radiographs showed a cortical-destroying osteolytic lesion at the head of the fibula extending into the surrounding soft tissue. Ultrasound imaging showed a mixed echo formation with indistinct borders and multiple chambers separated by trabeculae demonstrating blood flow. MRI revealed the absence of the fibular head as evidenced by cortical destruction and extension into adjacent soft tissue. CT scan showed a 12× 13 cm mass in the left popliteal region extending to the knee margin. Enlarged lymph nodes were noted in the left groin. Multiple small metastases were observed in the lungs. Histologically, atypical epithelial cells and stromal spindle cells were observed. CK and CK19 staining was positive. The patient was treated with Sunitinib 50 mg orally, once daily for 4 weeks, followed by 2 weeks off for 2 cycles. During treatment (after 2 cycles) the tumor showed progressive growth, resulting in decreased function of the affected limb. She was referred to the surgical department where the appropriate surgical amputation was performed. After surgery, the patient’s general condition improved. A further CT scan revealed a slight progression of metastatic lesions in the lungs, which prompted the decision to administer chemotherapy, but she refused to continue the treatment and did not receive chemotherapy. Two months later, she presented to the hospital in poor general condition. CT scan revealed extensive and progressive lesions in both lungs, leading to chest pain, hemoptysis, and hypoxia. Despite supportive care, the patient eventually died.
Conclusion: This case report presents a rare case of metastatic adamantinoma that did not respond to treatment with Sunitinib.
Keywords: adamantinoma, fibula, cytokeratin, sunitinib
Introduction
Adamantinoma is a low-grade, slowly growing, primary malignant bone tumor composed of epithelial cells in a fibrous or osteo-fibrous stroma.1 The most common location of this tumor is in the tibia, with or without involvement of the fibula.2 In some cases, adamantinoma is found in other locations, including the humerus, ulna, femur, radius, ribs, and spine as primary sites.3 This tumor can also manifest in the fibula without involving the tibia, as seen in this case. In both classic and differentiated adamantinoma, genetic studies showed the presence of trisomy of one or more chromosomes 7, 8, 12 and 19.4
Case Presentation
A 21-year-old Syrian female patient was admitted to our hospital with a mass on the left leg. On clinical examination, the patient was in good general condition. A solitary mass measuring approximately 12×13 cm was observed on the upper lateral aspect of the leg. On palpation, the mass was tender with a localized increase in temperature, without redness coloration. The patient reported the onset of a small, slightly painful swelling in the left leg eight months prior to presentation. Over time, the swelling has increased in size to involve the top of the leg and part of the knee. The patient had limited range of motion in the knee joint and difficulty leaning on the affected limb. She reported numbness in her left foot, which was otherwise fully mobile.
Palpation of the pulse showed it to be present in both the dorsal foot and posterior tibial arteries. The patient had a nine-year history of smoking but no family history of cancer. At the time of presentation, laboratory tests showed white blood cell (WBC) 9.6/mm³, red blood cell (RBC) 5.29×106/mm³, hemoglobin (Hgb) 11.2 g/dL, platelet (Plt) 272 10³/mL, C-reactive protein (CRP) 31.3 mg/L, urea 37 mg/dL, creatinine 0.69 mg/dL. Lateral and posteroanterior radiographs of the left leg showed a cortical-destroying osteolytic lesion at the head of the left fibula extending into the surrounding soft tissues (Figure 1). Ultrasound (US) imaging revealed a mixed echo formation with poorly defined borders, containing numerous chambers separated by trabeculae with evidence of blood flow.
 |
Figure 1 Radiograph of the left leg. Lateral (A) and PA (B) images show an osteolytic lesion destroying the head of the fibula and extending into the surrounding soft tissues. |
Magnetic resonance imaging (MRI) of the affected area revealed the absence of the left fibular head, as evidenced by cortical destruction and extension into the adjacent soft tissue (Figure 2). A CT scan of the chest, abdomen, and pelvis revealed a mass in the left popliteal region measuring 12×13 cm extending into the border of the knee. The mass showed calcifications, extensive infiltration of muscle and soft tissue, and destruction of adjacent bone. In addition, lymph nodes in the left inguinal region were found to be enlarged with a maximum diameter of 17 mm. Multiple small metastases up to 10 mm in diameter were also found in the lungs. The differential diagnosis of adamantinoma included osteofibrous dysplasia (OFD) and fibrous dysplasia which could be difficultly distinguished from adamantinoma. However, OFD is specifically located in the cortex without involvement of the medullary canal. Osteosarcoma, Ewing sarcoma, chondrosarcoma, soft tissue tumors, and metastatic carcinoma also should be differential diagnosis of adamantinoma.
 |
Figure 2 MRI imaging showing the left tibia with the absence of the fibular head, with a clear extension into the adjacent soft tissue. |
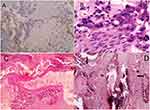
A tissue biopsy was obtained from the mass, and subsequent histological examination using hematoxylin and eosin staining revealed the presence of epithelial components and stromal elements, as well as evidence of osteoid formation. The tissue sample showed the presence of atypical epithelial cells and stromal spindle cells. Immunohistochemical staining was performed, and the results showed positive reactivity for cytokeratin and CK19, thereby supporting the diagnosis of adamantinoma. The positivity for EMA and P63, and negativity for CD34 distinguish adamantinoma from other tumors, thereby indicating its epithelial origin (Figure 3). In addition, positive staining for vimentin has been documented.5 This case presented metastatic adamantinoma Stage III according to Enneking staging.6
Given the rarity of the tumor and the lack of established treatment standards, a review of the reported cases in the medical literature was undertaken and a multidisciplinary team was convened to discuss the case. The results showed that metastatic adamantinoma responded to tyrosine kinase inhibitors such as Sunitinib and Pazopanib, whereas conventional chemotherapy had a less pronounced response, as evidenced by published cases. Dudek et al7 reported a case of tibial adamantinoma that was unresponsive to initial treatment with chemotherapy; however, lung metastases occurred after 4 months of chemotherapy. The patient received Sunitinib for metastatic adamantinoma. Significant improvement in pulmonary symptoms and sustained disease control over 11 months was achieved. Liman et al5 reported another case of tibial adamantinoma to lungs which was treated with chemotherapy for 7 months and achieved a partial response for 4 months. PET scan showed disease progression, so the patient received Sunitinib, which achieved a good partial response for 3 years. However, many studies have suggested that metastatic adamantinoma may be resistant to chemotherapy. We decided to treat the patient with Sunitinib 50 mg orally, once daily for 4 weeks, followed by 2 weeks off for 6 cycles. During treatment (after 2 cycles), the tumor showed progressive growth and became locally aggressive, leading to deterioration in the functional status of the affected limb (Figure 4). We decided to refer the patient to the surgical department, where the appropriate surgical amputation was performed. After surgery, the patient’s general condition improved. A further CT scan of the chest was performed one month later and showed a slight progression of the metastatic lesions in the lungs. The decision was made to treat the patient with chemotherapy (Gemcitabine 900 mg/m2 IV days 1, 8 + Docetaxel 75 mg/m2 IV day 8) every 21 days for 6 cycles. However, this chemotherapy regimen is less toxic than other protocols that are used for bone sarcoma). The patient was informed of the decision, but unfortunately she refused to continue the treatment and did not receive chemotherapy. Two months later, the patient returned to the hospital with hemoptysis and a poor general condition. A CT scan revealed extensive and progressive lesions in both lungs, resulting in chest pain, hemoptysis, and hypoxia. Despite supportive care, the patient eventually died.
 |
Figure 4 A photograph of a massive necrotic mass in the left leg was obtained prior to trans-femoral amputation (above the knee). |
Discussion
Adamantinoma is a rare neoplasm accounting for 0.3% to 1% of all primary bone tumors.8 It typically presents in adults, predominantly in the second and third decades of life,9 although some cases have been documented in older and younger age groups.10 There is a slight predominance of this tumor in males compared to females.11 This neoplasm originates from epithelial cells and is typically positive for keratin by IHC staining. The initial symptoms of adamantinoma are typically non-specific and depend on the location and extent of the tumor. The majority of patients present with a palpable swelling, which may or may not be accompanied by pain, and which typically evolves gradually. The onset is gradual and insidious, but progressive in nature. In more than half of the cases, previous trauma or pathological fractures have been reported as a cause of the onset of symptoms. In addition, bowing deformities of the affected tibia have been observed.12 However, our patient did not have any previous traumas or pathological fractures prior to the onset of symptoms. Sometimes symptoms related to tumor metastases may be present, such as paraneoplastic hypercalcemia with pulmonary metastases and neurological symptoms in the context of spinal lesions.13 Classic and differentiated adamantinomas are the two distinct forms have been recognized. Classic adamantinoma typically manifests after the second decade of life, with an average age of onset at approximately 40 years. It is characterized by an aggressive clinical course. In contrast, differentiated adamantinoma predominantly affects younger patients, with a mean age of onset of 20 years.14 In our case, the characteristic radiological features of the tumor were not seen due to the extensive growth into the fibula, which occupied the head at diagnosis, and the extensive infiltration of adjacent tissues. These tumors have the potential for both local recurrence and metastasis, and the most common sites of metastasis are the lungs and regional lymph nodes. Localized primary tumors are usually treated by wide surgical resection with limb salvage and limb reconstruction.15 Although there is no evidence that amputation improves survival compared with other surgical modalities, it may be considered as a treatment option in cases of local recurrence or when other options are not available.16 We made the decision to perform the amputation when the tumor showed a worsening trend and the patient’s functional status also showed a decline, indicating that she had not achieved a response to targeted therapy.
Conclusion
Adamantinoma is a rare tumor and there is no standard treatment for all cases. It is imperative to make an accurate diagnosis and differentiate it from other tumors in order to make an appropriate management decision.
Ethical Approval
As we prepared the case for publication after the patient’s death, written informed consent to publish this case and any accompanying images was obtained from the patient’s parents. The institutional approval for the study of the case was not required to publish the case details.
Disclosure
The authors declare that there is no conflict of interest regarding the publication of this article.
References
1. Moon NF, Mori H. Adamantinoma of the appendicular skeleton–updated. Clin Orthop Relat Res. 1986;204:215–237. doi:10.1097/00003086-198603000-00025
2. Holden DM, Joyce MJ, Sundaram M. Adamantinoma. Orthopedics. 2014;37(6):362,420–362,422. doi:10.3928/01477447-20140528-01
3. Ulmar B, Delling G, Werner M, Huch K, Reichel H. Classical and atypical location of adamantinomas_presentation of two cases. Onkologie. 2006;29(6):276–278. doi:10.1159/000093049
4. Kanamori M, Antonescu CR, Scott M, et al. Extra copies of chromosomes 7, 8, 12, 19, and 21 are recurrent in adamantinoma. J MolDiagn. 2001;3(1):16–21.
5. Liman AD, Liman AK, Shields J, Englert B, Shah R. A case of metastatic adamantinoma that responded well to sunitinib. Case Reports Oncol Med. 2016;2016:5982313. doi:10.1155/2016/5982313
6. Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 1980;153(153):106–120. doi:10.1097/00003086-198011000-00013
7. Dudek AZ, Murthaiah PK, Franklin M, Truskinovsky AM. Metastatic adamantinoma responds to treatment with receptor tyrosine kinase inhibitor. Acta Oncologica. 2010;49(1):102–104. doi:10.3109/02841860902913579
8. Unni KK, Dahlin DC, Beabout JW, Ivins JC. Adamantinomas of long bones. Cancer. 1974;34(5):1796–1805. doi:10.1002/1097-0142(197411)34:5<1796::AID-CNCR2820340530>3.0.CO;2-Z
9. Unni KK. Dahlin’s Bone Tumors: General Aspects and Data on 11,087 Cases.
10. Van Rijn R, Bras J, Schaap G, van den Berg H, Maas M. Adamantinoma in childhood: report of six cases and review of the literature. Pediatr Radiol. 2006;36(10):1068–1074. doi:10.1007/s00247-006-0272-5
11. Gulia A, Panda PK. Adamantinoma; an update. J Bone Soft Tissue Tumors. 2017;3(2):16–19.Jo. doi:10.13107/jbst.2454–5473.221
12. Filippou DK, Papadopoulos V, Kiparidou E, Demertzis NT. Adamantinoma of tibia: a case of late local recurrence along with lung metastases. J Postgrad Med. 2003;49(1):75–77. doi:10.4103/0022-3859.923
13. Dini LI, Mendonca R, Adamy CA, Saraiva GA. Adamantinoma of the spine: case report. Neurosurgery. 2006;59(2):E426. doi:10.1227/01.NEU.0000223497.06588.4A
14. Kumar A, Sharma R, Verma AK, Tiwari A, Mishra J. An unusual case of adamantinoma of long bone. Autops Case Rep. 2021;11:e2021276. doi:10.4322/acr.2021.276
15. Houdek MT, Sherman CE, Inwards CY, Wenger DE, Rose PS, Sim FH. Adamantinoma of bone: long-term follow-up of 46 consecutive patients. J Surg Oncol. 2018;118(7):1150–1154. doi:10.1002/jso.25269
16. Khan MH, Darji R, Rao U, McGough R. Leg pain and swelling in a 22-year-old man. Clin Orthop Relat Res. 2006;448:259–266.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.