Back to Journals » Risk Management and Healthcare Policy » Volume 18
National Healthcare Transformation Program in Saudi Arabia: Awareness of the New Models of Care Among Health Professionals
Authors Althuwaybi MA, Alshammari TM , Tharkar S , Alodhayani AA, Al-Muammar M, Abulmeaty M, Almutari KM
Received 6 December 2024
Accepted for publication 7 April 2025
Published 3 July 2025 Volume 2025:18 Pages 2259—2274
DOI https://doi.org/10.2147/RMHP.S509155
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Gulsum Kubra Kaya
Mohammed A Althuwaybi,1,2 Thamir M Alshammari,3,4 Shabana Tharkar,2 Abdulaziz A Alodhayani,5 May Al-Muammar,2 Mahmoud Abulmeaty,2 Khalid M Almutari2
1Qassim Health Cluster, Qassim, Saudi Arabia; 2Department of Community Health Science, College of Applied Medical Science, King Saud University, Riyadh, Saudi Arabia; 3Department of Clinical Practice, College of Pharmacy, Jazan University, Jazan, Saudi Arabia; 4Pharmacy Practice Research Unit, College of Pharmacy, Jazan University, Jazan, Saudi Arabia; 5Department of Family and Community Medicine, College of Medicine, King Saud University, Riyadh, Saudi Arabia
Correspondence: Khalid M Almutari, Department of Community Health, College of Applied Medical Sciences King Saud University, Riyadh, Saudi Arabia, Email [email protected]
Objective: This study investigated the level of awareness of the new Models of Care (MoC) implemented under Vision 2030’s National Transformation program among healthcare professionals in the Al-Qassim region of Saudi Arabia.
Methods: A cross-sectional approach was employed to collect data from 323 healthcare professionals, including physicians and nurses, through an online survey designed to evaluate their awareness of six distinct models of care and their respective components.
Results: A significant majority (63.5%) of healthcare providers demonstrated a high level of overall awareness of the MoC. Factors such as holding a higher university degree (p = 0.007), being a physician (p = 0.018), possessing greater work experience (p = 0.017), and having undergone training (p < 0.000) were found to be significantly correlated with increased awareness of the overall model of care. Participants exhibited a strong awareness of preventive care (91%), urgent care (84%), chronic disease care (84%), and mother and childcare (70%) models, whereas awareness of elective (54.8%) and palliative care (55.4%) was notably lower. Both overall and specific awareness levels of MoC were significantly linked to the training received on the subject.
Conclusion: The findings indicate a good understanding of the MoC. However, there is substantial potential for improving awareness through structured training programs. Consequently, healthcare policymakers must prioritize the development of structured training programs through training and reinforcement that address all six MoC components.
Keywords: awareness, healthcare transformation, National Transformation Program, model of care, Saudi Arabia, Vision 2030
Introduction
Saudi Arabia ranks among the top twenty nations globally in terms of gross domestic product (GDP).1 The country has initiated a significant transformation aimed at reducing its reliance on oil by diversifying its economy and fostering national development through “Vision 2030” and the National Transformation Program (NTP).2 The health sector transformation program represents the foremost of the eight key themes within the NTP, concentrating on enhancing public health, extending life expectancy, and reducing morbidity and mortality rates by improving access to and the delivery of healthcare services across all levels of care.3 To achieve the goals of healthcare transformation, new Models of Care (MoC) have been created to implement 27 coordinated interventions through six Systems of Care (SoC).3 These MoCs are innovative frameworks designed to enhance healthcare services efficiently and effectively, with a focus on preventive, primary, and tertiary care. The patient-centric approach of MoC encompasses the provision of healthcare services based on principles that promote equitable access and support integrated care through the efficient use of resources.4 This initiative is expected to significantly alleviate the public health challenges posed by the rapidly growing population. Saudi Arabia encounters significant challenges associated with the mass gatherings in the holy city of Makkah, which attracts hundreds of thousands of pilgrims annually. The risks posed by infectious diseases, trauma, and emergency medical care, including life-threatening emergencies from underlying chronic diseases, are substantial and exert a considerable burden on the healthcare system. Moreover, the number of pilgrims is projected to increase to more than three million by 2030, necessitating restructuring of the health systems that envisage and prioritize the health and safety of the pilgrims.5 Hence, the components of the health transformation have been designed to address health needs throughout the lifespan of an individual, accommodating the needs of both the local population as well as the huge influx of pilgrims through these SoCs, as illustrated in Figure 1.
 |
Figure 1 The six Models of care (MoC) and 27 Systems of care (SoC) interventions. |
All MoC activities will be implemented to streamline the Saudi healthcare system to meet the Kingdom’s “Vision 2030” goals. The health care model is a national project that endeavors to rebuild the health system providing a high level of quality and efficiency, achieving the comprehensive concept of prevention, and providing the optimum professional environment for service providers. The healthcare model is based on three main pillars: Improving the quality of health services provided, ensuring fast access to health services, and increasing the efficiency and effectiveness of healthcare. The suggested modifications to the MoC advocate for a uniform strategy in adopting new models, which necessitate learning and organizational processes at the grassroots level among healthcare providers.
The healthcare models have demonstrated significant effectiveness in improving health conditions and patient outcomes globally. Healthcare reforms benefit the country in many ways. Increased healthcare access, improved quality of services, financial sustainability by controlled spending, comprehensive coverage, and equity deserve special mention. The Organization for Economic Co-operation and Development (OECD) documented evidence of the efficacy of healthcare reforms in improving equity, microeconomic efficiency, and macroeconomic cost control.
A systematic review assessing the comprehensive effectiveness of chronic care models for mental health involving 161 analyses demonstrated improved patient outcomes for various mental health disorders.6 Similarly, another systematic review assessing the effectiveness of chronic care models involving 77 international studies demonstrated significant improvements to population health outcomes and improvement in overall healthcare systems.7
With substantial evidence of effectiveness, the adoption of models of care would immensely improve the country’s healthcare transformation. Healthcare professionals are key stakeholders in the country’s healthcare transformation initiatives. The success of newly introduced healthcare models largely depends on healthcare professionals’ awareness and understanding of these models. The transformation strategy for the health sector emphasizes the significance of attributes such as awareness of the changes, motivation, knowledge and skills, capability, and reinforcement as essential components for the effective execution of the transformation program. One of the first studies on MoC in Saudi Arabia, conducted by Alomari et al,8 assessed the awareness of the MoC among healthcare professionals in the Riyadh First Health Cluster. The findings indicated a notable understanding of the transformation occurring within the health sector. A recent study from the Tabuk region demonstrated a high level of awareness but a lack of understanding of the new models of care among healthcare workers.9
On the other hand, there is a significant lack of detailed information from Al-Qassim health cluster. The current study aimed to assess the level of awareness regarding the MoC and its objectives among primary healthcare providers, including physicians and nurses. Additionally, the study explored various factors that may influence awareness. The results of this study could contribute to addressing the gaps in the current literature and offer valuable insights for policymakers involved in the Kingdom’s strategic goals and reform initiatives.
Materials and Methods
Study Design, Setting and Participants
An observational cross-sectional survey was conducted among primary healthcare physicians and nurses using multistage cluster sampling in the Al-Qassim region of Saudi Arabia between June 1st and September 15th, 2022. Data was collected using an online questionnaire circulated among primary healthcare staff. Strobe guidelines were followed (Supplementary material 1) in this study.
Study Questionnaire
The questionnaire was developed based on a review of the new MoC components and by consulting MoC experts in Al-Qassim Health Cluster. The questionnaire was pilot-tested on a sample of 30 participants to check the validity of the questionnaire. This data was excluded from the final analysis. The questionnaire comprised three sections: Section one collected details of the socio-demographic characteristics of the participants (age, gender, specialty, work experience, and academic qualifications), the second section included twelve questions assessing the participants’ awareness of the models of care, and its components through a set of multiple-choice questions, and the third section consisted of seven questions to assess participants’ understanding and acceptance of MoC and readiness for action.
The reliability score, as determined by Cronbach’s coefficient alpha, was found to be satisfactory in a sample of 30 healthcare practitioners, with a value of 0.857.
Data Collection
The study site included primary healthcare centers (PHCs) belonging to 15 public health clusters in the Al-Qassim region. Of the total 156 PHCs, 56 were selected by systematic random sampling techniques as primary sampling units. The questionnaire, accompanied by the informed consent document, was sent to the official Email address of the director of the chosen Primary Health Centers (PHCs). The director was tasked with reaching out to the healthcare personnel of the corresponding sampling unit through email. Repeated reminders were sent to increase the response rate until the sample size was obtained. Data collection was facilitated through the SurveyMonkey platform, and any incomplete responses were omitted from the analysis.
Power Calculation and Sample Size
The sample size was calculated from a population of 1454 primary healthcare providers, including 429 physicians and 1025 nursing staff, working at 156 PHCCs belonging to 15 public health sectors that report to the Al-Qassim Health Cluster. Due to the lack of data, the expected prevalence of awareness levels among healthcare providers was presumed to be approximately 30%, and the acceptable margin of error was decided to be 5% at a 95% confidence interval.
n = estimated sample size
Z  = the value from normal distribution equivalent to 95 confidence intervals.
= the value from normal distribution equivalent to 95 confidence intervals.
p = expected prevalence or proportion of awareness about Health Care Model. Due to the lack of previous prevalence, expected prevalence of good awareness level among health care providers approximately 30% was considered.
d = difference between estimated proportion and true proportion in population (maximum allowable error = 5%).
The final sample size was estimated at 323 participants.
Statistical Analysis
The Statistical Package for Social Sciences (SPSS) software version 24 was used to analyze the data. Descriptive statistics were used to describe the distribution of socio-demographic characteristics of participants presented as frequency, percentage, mean, and standard deviation. The level of awareness was categorized into high and low according to the total score of each respondent. Eighteen items required scoring for analysis: The items with YES/NO question type were given (1) for correct answer and (0) for wrong answer. For assessing MoC’s overall level of awareness: the total score for sections two and three was 37. Both MoC overall and specific levels of awareness were analyzed. Based on the 50th percentile, participants scoring greater than 60% were considered to have a high awareness level while participants who scored less than 40% were considered to have low awareness levels. For assessing each of the MoC systems’ level of awareness, participants who answered items related to each specific system correctly were considered to have a high awareness level, while participants with incorrect answers were considered to have a low awareness level.
A chi-square test was used to determine the association between overall and specific levels of awareness and participant characteristics (age, gender, type of health specialty, academic qualification, work experience duration, and MoC training status).
Study Bias
Due to the nature of the cross-sectional design, bias in data collection is inevitable Self-reporting bias, recall bias, and sampling bias may have affected the study’s results.
Ethics Approval
Ethics clearance for the study was approved by the Ministry of Health, General Directorate of Health Affairs, Al-Qassim region, Reference No: 1442–88.426. The study adhered to the declaration of Helsinki. An informed consent form was attached, explaining the purpose of the research before the first page of the questionnaire, and the willingness to participate or withdraw at any time was well explained. Anonymity was maintained throughout the questionnaire and data collection process.
Results
A total of 323 healthcare professionals were included in the study, of which nurses accounted for 196 (60.7%). Most of the participants had bachelor’s qualifications (69.7%), and many had more than ten years’ experience (56.7%). Of the total participants, 62.5% had undergone training in models of care. The other details of socio-demographic characteristics are displayed in Table 1.
 |
Table 1 Sociodemographic Details of the Study Participants |
Figure 2 illustrates the level of awareness of various models of care. The participants showed the highest level of awareness for preventive care (90.7%), followed by chronic care (83.9%) and urgent care (83.6%). However, elective and palliative models of care showed low awareness.
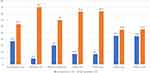 |
Figure 2 Level of awareness of various models of care among the study participants. |
Furthermore, a test of association between independent socio-demographic variables and the level of awareness of the overall MoC is shown in Table 2. Higher university qualification (p = 0.007), longer work experience (p = 0.017), physician as an occupation (p = 0.018), and MoC training (p = 0.000) were associated with higher levels of awareness of overall MoC. The preventive care model and its associated factors with awareness are presented in Table 3. In addition, the association between demographic variables and the preventive care model is demonstrated in Table 4. Increasing age, being a male, work experience, and training status showed positive association.
 |
Table 2 The Association Between Sociodemographic Characteristics and Overall MoC Level of Awareness |
 |
Table 3 Preventive Care Model and Its Associated Factors with Awareness |
 |
Table 4 Association Between Sociodemographic Characteristics and (Mother and Child Care System) Level of Awareness |
The participants presented high awareness of the urgent care model, as shown in Table 5. Increasing age, male graduate physicians with higher work experience and training showed a significant association with higher awareness of the urgent care model. Similar results were obtained for other models of care, like the chronic care model (Table 6), the elective care system (Table 7), and the palliative care model (Table 8).
 |
Table 5 Association Between Sociodemographic Characteristics and Urgent Care System Level of Awareness |
 |
Table 6 Association Between Sociodemographic Characteristics and Chronic Diseases Care System Level of Awareness |
 |
Table 7 Association Between Sociodemographic Characteristics and Elective Care System Level of Awareness |
 |
Table 8 Association Between Sociodemographic Characteristics and Palliative Care System Level of Awareness |
Discussion
“Transform Healthcare” is the first theme of the national transformation program, a part of Saudi Vision 2030 that was introduced to revolutionize healthcare catering to the needs of the ever-increasing demands of the growing population.10 The evolution of the MoC concept serves as the backbone and mainstream of the healthcare system to achieve the healthcare transformation goals. This necessitates better understanding and empowerment of the stakeholders as active players who determine the success of the program. Hence, the present study’s objective was to investigate the awareness of the models of care and its goals among the primary healthcare providers of Al-Qassim region of Saudi Arabia. Although literature exists from the central province, data is specifically sparse from Al-Qassimregion.
Generally, the level of awareness did not seem to reflect being impressive and prodigious since the distribution was disproportionate between the Models of care. The summary of findings suggests that increasing age (up to 40 years), being a physician, higher university qualifications, work experience, and receiving training played a significant role in greater awareness of the models of care. Female gender, nurses, and older healthcare staff showed lower awareness. Evaluating the indicators of higher and lower knowledge levels is imperative since they also assist in recognizing the deficiencies that can be amended to enhance the prospects of improvement.
The overall model of care, elective, and palliative care models deserve special mention due to sub-optimum awareness. The lower awareness of elective and palliative care models could be possibly related to less experience of the healthcare staff at the primary care level since the procedures are mainly performed at secondary and tertiary care centers. Palliative care services are mostly provided in tertiary hospitals, oncology centers, and terminally ill specialized care centers and there is little involvement of the PHC. This reflects on low level of palliative care awareness among participants compared to other systems of care. Contrary to results from Riyadh’s first health cluster study that reported greater awareness of overall models of care, our results showed lower awareness.8 Similarly, a Spanish study that assessed the attitude and knowledge of palliative care among nurses demonstrated low-level knowledge that improved with reinforced training.11 Our findings align well with another regional study from Tabuk province, which revealed that only half of the study participants could accurately understand the fundamental concepts of the healthcare transformation process and the new models of care.9
It is well recognized that knowledge transition is a dynamic process and augments with time. Hence, factors like increasing age and work experience become inter-related. The present study demonstrated a significant association between a high level of awareness and work experience. The physicians and nurses who had more than five to ten years of work experience showed the highest level of awareness of all the healthcare models. However, it was interesting to note that the knowledge levels seem to decline among professionals with increasing experience of eleven years and higher. A similar observation was seen with increasing age. The age category from thirty to forty years showed the highest knowledge levels, while above forty years continued to exhibit a steady decline. Keeping pace with the latest updates using media and technology in the younger age group could be one of the reasons. However, AlOmari et al reported contradictory findings in their study from the Central region that demonstrated high awareness among staff with greater than 20 years’ experience, but on the other hand, they also demonstrated high levels of disagreement, low motivation, and confidence in sharing MoC knowledge in the older age category.8 These findings emanate curiosity to explore the reasons behind the findings. In-depth qualitative studies are warranted to understand this trend. However, education entails a sovereign and independent observation. Being a graduate showed a significant association with higher awareness of the models of care.
Furthermore, the association between the specialty of education and awareness deserves special mention. Physicians generally exhibited a superior comprehension of the care models, as nurses with lower awareness significantly outnumbered the physicians. This disparity contributed to the variation in knowledge levels; nonetheless, nurses demonstrated slightly greater knowledge than physicians within the higher awareness group, particularly regarding specific models such as urgent care (p = 0.035) and the overall model of care (p = 0.018).
Training is a crucial component of continuous professional development and serves as a direct indicator of the success of any particular model. The current study has observed that not receiving training negatively impacted the understanding of the healthcare models. It was surprising to note that around 37.5% of the participants had not received formal training on the MoC. This may negatively influence the knowledge and functioning of the MoC. For instance, the majority of the participants with low awareness have not received formal training. Consistency in the findings was observed in all the models of care that exhibit higher awareness among the trained healthcare providers. Many studies have proven the effectiveness of training in improving the performance of healthcare professionals.12–16
Recommendations
Our research emphasizes the critical need for comprehensive training and reinforcement initiatives aimed at healthcare professionals, with a particular focus on senior professionals and nurses, to effectively implement Models of Care (MoC) across all tiers of healthcare delivery. Given the significant representation of nurses as a large workforce in the healthcare sector and their role in operationalizing the Moc, tailored training programs targeting the specific nurse population are highly recommended. Long-term strategies to maintain MoC awareness, such as establishing a monitoring framework or periodic evaluation of health professionals’ knowledge are also important from a wider perspective to achieve success in healthcare reform implementation.
Furthermore, the healthcare workers include professionals from various nationalities, it is recommended to conduct more in-depth research to analyze the potential effects of cultural and institutional factors on awareness levels. Conducting knowledge assessment studies is recommended to validate existing research and to generate new data from various clusters. Future research should focus on conducting longitudinal studies to evaluate the efficacy of content, delivery and focus of the training programs. Concrete strategies for designing and implementing training programs tailored to specific types of MoCs are recommended. In the broader context of healthcare transformation, qualitative research is recommended to explore the barriers and facilitators of training programs.
Limitations
Online and self-administration methods of data collection are subject to bias stemming from incomplete information and poor responses. A gender imbalance was evident within the specialty, as the majority of nurses were female. Consequently, any correlation between lower awareness levels and the female gender was confounded by the specialty and may not accurately reflect the specific gender. Only physicians and nurses were enrolled in the study; hence, data from other health professionals was not included which limits the generalizability. Other factors like workload and institutional support were not assessed to correlate with study objectives. Moreover, generalizability is limited only to the Al-Qassim cluster.
Conclusion
The participants demonstrated a commendable level of awareness; however, there exists a substantial opportunity to improve the comprehension of the overall model of care and the additional six models. A greater awareness of the MoC was significantly associated with holding advanced university degrees, being a physician, and having undergone specialized training. Nevertheless, senior staff members, particularly those over 40 years of age and with more than 15 years of experience, could benefit from consistent updates concerning the current transformation system. Both general and specific awareness were significantly linked to MoC training. Therefore, as policy implications, healthcare policymakers need to prioritize the establishment of structured training programs that include regular updates for healthcare personnel, and reinforcement training programs should be considered for nursing staff.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available by the authors with the permission of the principal investigator upon reasonable request.
Ethics Statement
Ethics approval was obtained by the Ministry of Health, General Directorate of Health Affairs, Al-Qassim region, Reference No: 1442-88.426
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
We would like to extend our appreciation to King Saud University for funding this work through the Ongoing Research Funding program (ORF-2025-463), King Saud University, Riyadh, Saudi Arabia.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. The Top 20 Largest Economies in the World by GDP. Available from: https://researchfdi.com/resources/articles/world-gdp-largest-economy/.
2. Saudi Vision 2030. Available from: https://www.vision2030.gov.sa/en.
3. Health Sector Transformation Strategy. Saudi Vision 2030. Available from: https://www.moh.gov.sa/en/Ministry/vro/Documents/Healthcare-Transformation-Strategy.pdf.
4. Understanding the process to develop a model of care: an agency for clinical innovation framework. Available from: https://aci.health.nsw.gov.au/data/assets/pdf_file/0009/181935/HS13-034_Framework-DevelopMoC_D7.pdf.
5. Saudi Vision 2030. Pilgrim experience program. Available from: https://www.vision2030.gov.sa/media/bjahzdfw/2021-2025-pilgrim-experience-program-delivery-plan-en.pdf.
6. Woltmann E, Grogan-Kaylor A, Perron B, et al. Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: systematic review and meta-analysis. Am J Psychiatry. 2012;169:790–804. doi:10.1176/appi.ajp.2012.11111616
7. Davy C, Bleasel J, Liu H, Tchan M, Ponniah S, Brown A. Effectiveness of chronic care models: opportunities for improving healthcare practice and health outcomes: a systematic review. BMC Health Serv Res. 2015;15:194. doi:10.1186/s12913-015-0854-8
8. Alomari NA, Alshehry B, Alenazi AH, et al. Model of care knowledge among Riyadh First Health Cluster staff at the Ministry of Health, Saudi Arabia. J Family Med Prim Care. 2021;10(8):3094–3104. doi:10.4103/jfmpc.jfmpc_405_21
9. Ghalibi KM, Ibrahim Omer HM, Al Mamun M. Awareness and readiness of healthcare workers regarding national transformation program in the health sector in Tabuk Region, Saudi Arabia. Saudi J Health syst Res. 2024;4:45–53. doi:10.1159/000534781
10. National Transformation Program. Saudi Arabia: 2030. Saudi Vision. Available from: https://vision2030.gov.sa/sites/default/files/attachments/NTP%20English%20Public%20Document_2810.pdf.
11. Mengual TE, Chover-Sierra E, Ballestar-Tarín ML, et al. Knowledge about palliative care and attitudes toward care of the dying among primary care nurses in Spain. Healthcare. 2023;11:1018. doi:10.3390/healthcare11071018
12. Rowe AK, Rowe SY, Peters DH, et al. The effectiveness of training strategies to improve healthcare provider practices in low-income and middle-income countries. BMJ Global Health. 2021;6:e003229. doi:10.1136/bmjgh-2020-003229
13. Dieleman M, Gerretsen B, van der Wilt GJ. Human resource management interventions to improve health workers’ performance in low and middle income countries: a realist review. Health Res Policy Syst. 2009;7:7. doi:10.1186/1478-4505-7-7
14. O’Brien MA, Rogers S, Jamtvedt G, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2007:4. doi:10.1002/14651858.CD000409
15. Chowdhury S, Mok D, Leenen L. Transformation of health care and the new model of care in Saudi Arabia: kingdom’s vision 2030. J Med Life. 2021;14:347–354. doi:10.25122/jml-2021-0070
16. Oxley H, MacFarlan M. Health care reform controlling spending and increasing efficiency. OECD Economics Department Working Papers, No. 149. Paris: OECD Publishing; 1994. Available from: https://doi.org/10.1787/338757855057.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



