Back to Journals » Clinical Ophthalmology » Volume 19
Optimization of the Ocular Surface Prior to Cataract Surgery Using Cryopreserved Amniotic Membrane
Authors Wongskhaluang J
Received 28 February 2025
Accepted for publication 5 June 2025
Published 25 June 2025 Volume 2025:19 Pages 1975—1983
DOI https://doi.org/10.2147/OPTH.S525438
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Jeff Wongskhaluang
Ophthalmology, Grin Eye Care, Olathe, KS, USA
Correspondence: Jeff Wongskhaluang, Grin Eye Care, 21020 W 151st St, Olathe, KS, 66061, USA, Tel +1 (913) 829-5511, Email [email protected]
Purpose: To assess the benefit of cryopreserved amniotic membrane (cAM) in restoring corneal surface health prior to cataract surgery and enhancing post-operative refractive outcomes in patients with moderate to severe dry eye disease (DED).
Methods: A prospective, repeated-measures, self-controlled study of 64 eyes with moderate to severe DED that were treated with cAM prior to cataract surgery. Biometry, topography, corneal staining (NEI scale), SPEED scores, and best corrected visual acuity (BCVA) were assessed before and after treatment and 1-month post-operatively. Primary outcome was refractive accuracy before and after treatment based on manifest refraction at 1 month post-operatively.
Results: A total of 55 eyes of 37 patients (95% female) completed the study. SPEED scores and NEI scores significantly improved at 1- and 2-weeks post-treatment, with sustained benefit at 1 month post-operatively (P < 0.0001). Spherical equivalent was within ± 0.25 D in 36% of eyes before and 70% of eyes after cAM treatment (P = 0.002); within ± 0.5 D in 66% of eyes before and 94% of eyes after (P < 0.001); within ± 0.75 D in 76% of eyes before and 98% of eyes after (P < 0.001); and within ± 1D in 86% eyes before and 100% of eyes after (P = 0.016). Emmetropia was attained in 84% of eyes, and 93% (51/55) of eyes had 20/20 BCVA post-operatively.
Conclusion: Treatment with cAM prior to cataract surgery can significantly improve both signs and symptoms of moderate to severe DED, with continued improvement post-operatively. Furthermore, CAM may ultimately improve biometry accuracy, mitigating the risk of surgical delay.
Keywords: amniotic membrane, cataract surgery, dry eye, ocular surface optimization
Introduction
Cataract surgery is one of the most commonly performed procedures in the United States, with approximately 3 million cataract surgeries performed annually.1 A high level of refractive accuracy is anticipated by patients undergoing cataract surgery, particularly as the use of premium intraocular lens is increasing.2 Blurred vision is the leading cause of postoperative patient dissatisfaction, which is caused by postoperative refractive error in 57% of cases.3 As a result, thorough pre-operative assessment and precise calculation of the intraocular lens (IOL) power is imperative to obtain accurate post-operative refractive outcomes.
Optical biometry, which is a non-invasive automated method for measuring the anatomical characteristics of the eye, is the current gold standard for calculating IOL power prior to cataract surgery. It measures axial length, keratometry (K) values, lens thickness, and anterior chamber depth. Biometry accuracy is largely dependent on the stability of the ocular surface. An unstable tear film due to ocular surface disease (OSD) often produces inaccurate and fluctuating K measurements4,5 and astigmatism,4,6 which can ultimately result in incorrect IOL selection and impaired post-operative vision. In a study by Epitropoulos et al,4 patients with dry eye demonstrated significantly more variability in average K and anterior corneal astigmatism measurements compared to normal eyes. This is problematic as 30–80%7–10 of patients who are evaluated for cataract surgery have objective signs of dry eye/OSD, but only 3% of diagnosed patients are treated within 12 weeks of cataract surgery.8 Not only can pre-existing OSD impact biometry and post-operative refractive accuracy, it has also been shown to result in persistent or exacerbated signs and symptoms of OSD following cataract surgery.11–13 Thus, it is crucial that high-risk cases with pre-existing OSD receive aggressive management prior to cataract surgery to optimize post-operative visual outcomes and patient satisfaction as well as prevent further deterioration of the ocular surface.
The ASCRS Cornea Clinical Committee recently developed a consensus-based, practical diagnostic algorithm to aid surgeons in efficiently diagnosing and treating visually significant OSD prior to refractive surgery.14 In these guidelines, the use of self-retained cryopreserved amniotic membrane (cAM) in the form of Prokera® is advised to address severe punctate keratitis and restore a smooth ocular surface preoperatively. Prokera is one form of cAM that is commercially available and is a class II medical device that has been cleared by the FDA for the treatment of ocular surface damage and stromal inflammation. Notably, cAM has been recognized by the FDA as having anti-inflammatory, anti-scarring, and wound healing properties.15 Due to these properties as well as its sutureless, self-retained nature, Prokera is a useful treatment modality for a variety of ocular surface diseases and can be placed onto the ocular surface in-office to help promote regenerative wound healing. A number of studies have demonstrated that cAM in the form of Prokera expedites the recovery of a stable ocular surface and improves signs and symptoms of OSD in patients with moderate to severe dry eye.16–19 Nevertheless, its use in optimizing the accuracy of biometry readings prior to cataract surgery has been less reported in the literature. Yeu et al20 previously reported that debridement followed by placement of cAM in 10 patients with epithelial basement membrane dystrophy (EBMD) resulted in a change in keratometry measurements from 43.5 ± 1.2 D at baseline to 44.6 ± 1.2 D at 1 month, and the average change in IOL power was greater than 1D. While this pilot study suggests cAM may help improve IOL calculation accuracy, post-operative data was not collected, and the findings are limited to patients with EBMD. Thus, the purpose of this study is to expand upon these findings by assessing treatment outcomes both before and after cataract surgery and broadening the utility of cAM in ocular surface optimization by assessing its use in patients with moderate to severe keratitis/DED. Such treatment for one week may mitigate the risk of surgical delays.
Materials And Methods
Following approval from Sterling Institutional Review Board (ID: 9132-JWongs), a prospective, single-center, investigator-initiated, repeated-measures study (NCT05148507) was conducted to evaluate the use of self-retained cAM (Prokera Slim®; Biotissue Inc, Miami, FL) in patients presenting with moderate to severe dry eye disease prior to cataract surgery. The study was performed in accordance with the Declaration of Helsinki, and written informed consent was obtained from all subjects prior to enrollment. A total of 64 eyes with moderate to severe dry eye disease, defined as SPEED score ≥10 and total cornea fluorescein staining score ≥4 (NEI scale), were enrolled in the study. All patients were at least 18 years of age, had plans to undergo cataract surgery, failed prior conservative dry eye treatments (artificial tears, ointments, topical steroids, anti-inflammatory drops, warm compresses, etc). within 30 days of screening, and exhibited topographic changes (ie irregularity, dropout, and higher order aberrations) as determined by the investigator. Patients were excluded if they had used contacts lens or scleral lens within 7 days of screening, ocular surgery within 3 months, glaucoma drainage devices or filtering bleb, active infection, significant posterior corneal astigmatism (≥0.75 D), visually significant retinal pathology, clinically significant ocular findings (eg dystrophies, ectasia, etc), short eyes (axial length < 22 mm), or high myopia (axial length ≥ 26 mm). Axial lengths shorter21,22 or longer21,23 than the normal range as well as significant posterior astigmatism24–26 have been shown to be contributing factors to post-operative refractive error after cataract surgery. Thus, these eyes were excluded to eliminate potential variability that could be caused by the inclusion of patients with these conditions. Additional exclusion criteria included history of refractive surgery, ocular trauma, herpetic keratitis, or drug reactions to Ciprofloxacin, Amphotericin B, Glycerol, and/or Dulbecco’s Modified Eagle Medium (DMEM).
Biometry and topography were assessed before and after treatment by the same examiner and devices. Cryopreserved AM (Prokera®; BioTissue, Inc; Miami, FL) was placed on the ocular surface and removed after 5 to 7 days. In brief, CAM was thawed at room temperature for several minutes and rinsed with saline prior to insertion. Following the instillation of topical anesthetic drops (0.5% proparacaine hydrochloride), cAM was placed into the superior fornix while the patient looked down and then slid under the lower eyelid. Patients’ standard of care (ie lubrication, tear supplements, punctal plugs) was continued as necessary and noted in records. Biometry and topography measurements were re-assessed 1 and 2 weeks following cryopreserved AM removal, and patients were scheduled for cataract surgery upon stabilization of the ocular surface within two to four weeks of completing treatment, with the chosen IOL based on the 2-week post-treatment biometry measurements. This is in alignment with the ASCRS Preoperative OSD Algorithm,14 which suggests reassessing the patient approximately 2 to 4 weeks after initiating treatment and waiting at least 7 days between discontinuing amnion-based therapies and proceeding with surgery. Patients that continued to have DED and were not suitable for cataract surgery as determined by the investigator received another treatment of cryopreserved AM.
Assessments
Ocular evaluations, which included signs and symptoms of DED as well as biometry and topography measurements, were assessed at baseline as well as 1- and 2-weeks post-treatment and 1-month post-operatively. Corneal fluorescein staining (CFS) was used to evaluate the cornea using the National Eye Institute (NEI) scale.27 The NEI grading scale divides the corneal area into five sections, each of which is assigned a score between 0 and 3 depending on the amount and distribution of CFS. The scores of the five sections are added to give the total CFS score, ranging from 0 (absence of corneal epitheliopathy) to 15 (severe epitheliopathy). Patients’ subjective symptoms were assessed using the Standard Patient Evaluation of Eye Dryness (SPEED) questionnaire, which is a validated, 8-question dry eye survey that evaluates both the frequency and severity of symptoms. The numeric value for each answer is added to give a total score ranging from 0 to 28, with a score ≥10 indicative of severe dry eye.28 Topography was assessed using the Atlas (Zeiss, Oberkochen, Germany) and VX130+ topographers (Visionix, North Lombard, IL), and biometry was assessed using the IOLMaster® 700 (Carl Zeiss Meditec, Jena, Germany). Parameters assessed included keratometry values, central corneal thickness, anterior chamber depth, lens thickness, and axial length. The Barrett TK Universal II formula was used to calculate the pre- and post-treatment IOL sphere and cylinder power recommendation as well as the predicted post-operative spherical equivalent (SE). Visual acuity was determined using a Snellen chart, and manifest refraction was assessed post-operatively using a standardized phoropter and a “push plus” technique to determine post-operative SE. The accuracy of the predicted SE was compared pre-and post-treatment by calculating the refraction prediction error, which was calculated as the absolute difference between the actual postoperative SE via manifest refraction and the predicted SE using pre-treatment data using standard back-vertex techniques.29 Pre-treatment SE refers to baseline SE and post-treatment SE refers to the SE that was measured at two weeks post-CAM treatment.
Outcomes
Primary outcome measure was the accuracy of the predicted SE pre- and post-treatment. Secondary outcome measures included change in SPEED scores, NEI corneal staining scores, BCVA, and average deviation from refractive target. Additionally, the percentage of eyes that achieved emmetropia (spherical equivalent −0.5 to +0.5 D and <1.0 D astigmatism)30 was also assessed post-operatively.
Sample Size Calculation
The sample size for this study was estimated using a two-sided, McNemars test, with α set to 0.05, 1-β set to 0.80, an odds ratio of 3.2, and a proportion of discordant pairs of 0.525. This resulted in a required sample size of 58 patients. Assuming a dropout rate of 10%,31 a total of 64 eyes were enrolled in this single-site study to ensure the study was adequately powered.
Statistical Analysis
All statistical analyses were carried out using IBM SPSS version 20.0. Categorical variables were described by percentages and frequencies, while continuous variables were described by means and standard deviations. McNemar’s chi-squared for within-subjects designs was used to assess binary dependent variables, such as proportions of eyes achieving target refraction pre- and post-treatment. When assessing continuous dependent variables such as SPEED scores and corneal staining scores, a paired t-test was used. A P value of less than 0.05 was considered statistically significant.
Results
A total of 64 eyes were enrolled in the study. Nine eyes of 6 patients were withdrawn from the study due to cancellation of cataract surgery (n = 4), declined treatment with cAM (n = 3), development of epiretinal membrane (n = 1), and lost to follow-up post-treatment (n = 1). As a result, 55 eyes of 37 patients completed the study and were included for the analysis. The majority of patients were female (94.6%), and the average age was 70.0 ± 6.3 years. All eyes presented with both signs and symptoms of moderate to severe DED despite prior treatment with preservative free artificial tears (100%), anti-inflammatory drops (27.3%), steroid drops (16.4%), gels and ointments (16.4%), warm compresses (9%), and others (12.7%), including punctal plugs, omega-3s, and anti-histamine drops. Upon slit lamp examination, 31% of eyes also presented with blepharitis, and 24% of eyes had meibomian gland dysfunction.
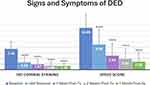
Patients received cAM for 5 to 7 days. One patient complained of discomfort due to the cAM device, which was resolved following tape tarsorrhaphy of the eye. Two patients received a second application of cAM. Upon removal of cAM, both clinical signs and symptoms of DED were significantly improved (Figure 1, p < 0.0001), with further improvement noted at one- and two-weeks post-treatment. The average SPEED score significantly improved from 14.9 ± 4.8 at baseline to 5.0 ± 4.3 at 1 week and 3.9 ± 3.6 at 2 weeks post-treatment (p < 0.0001). Similarly, average NEI corneal staining score significantly improved from 7.4 ± 2.5 at baseline to 1.9 ± 1.8 and 1.5 ± 1.4 at one- and two weeks post-treatment, respectively (p < 0.0001). When assessing visual outcomes pre- and post-treatment, BCVA slightly improved from logMAR 0.29 ± 0.22 to logMAR 0.26 ± 0.16 and 0.24 ± 0.21 at 1 and 2 weeks, respectively; however, this difference was not significant (P = 0.76 and P = 0.15, respectively). Two weeks following cAM treatment, the mean absolute difference from baseline in flat keratometry values (Kmin) and steep keratometry values (Kmax) was 0.35 ± 0.32 D (range: 0–1.22) and 0.30 ± 0.27 D (range: 0–1.38), respectively. Furthermore, mean absolute difference in central corneal thickness was 9.2 ± 9.0 μm (range: 1–38), and axial length changed by an absolute mean of 0.2 ± 0.3 mm (range: 0–0.23). When compared to pre-treatment biometry assessments, median change in recommended IOL SE at two weeks post-treatment was 0.5 D (range: 0–1.5). The majority (52%) of eyes had a change of ±0.5 D, 12% of eyes had ±1.0 D change, 4% of eyes had ±1.5 D change, and 32% of eyes had no change in IOL SE.
At 1 month post cataract surgery, 93% (51/55) of eyes had 20/20 BCVA, with 4 eyes attaining 20/25 BCVA. UCVA was 20/25 or greater in 91% of eyes, with 43 (78.2%) attaining 20/20, 7 eyes (12.7%) attaining 20/25, 2 eyes (3.6%) attaining 20/30, 1 eye (1.8%) attaining 20/40, and 2 eyes (3.6%) attaining 20/50. Of the 51 eyes with a plano refractive target, emmetropia was attained in 84% (43/51) of eyes. Overall, biometry performed after treatment with cAM more accurately predicted the post-operative refractive target compared to pre-treatment values (Figure 2). Spherical equivalent was within ±0.25 D of the refractive target in 36% of eyes before and 70% of eyes after treatment with cAM (P = 0.002); within ±0.5 D in 66% of eyes before and 94% of eyes after (P < 0.001); within ±0.75 D in 76% of eyes before and 98% of eyes after (P < 0.001); and within ±1D in 86% eyes before and 100% of eyes after (P = 0.016). Average deviation from refractive target using post-treatment biometry measurements was 0.22 ± 0.22 D (median: 0.25; range: 0–0.875) following surgery, which was significantly lower than the predicted refractive error using pre-treatment measurements (0.55 ± 0.46 D, P < 0.0001). When compared to baseline, NEI corneal staining scores remained significantly lower at 1 month post-operatively, with an average score of 1.4 ± 1.0 (P < 0.0001, Figure 1). Similarly, dry eye symptoms as measured by the SPEED questionnaire remained significantly improved, with an average score of 2.9 ± 3.0 (P < 0.0001, Figure 1). A representative case example is shown in Figure 3.
Discussion
Our findings demonstrate that pre-operative treatment of dry eye with cAM can quickly restore ocular surface health prior to cataract surgery, improve the accuracy of biometry measurements, and ultimately enhance post-operative refractive outcomes. Following one week of treatment with cAM, both signs and symptoms of DED significantly improved at both 1- and 2-weeks post-treatment. Average NEI corneal staining score improved by 6 points (or 80%) at 2 weeks post-treatment, and average SPEED score improved by more than 10 points, equating to nearly 75% reduction in overall symptoms. While other studies found a significant improvement in Oxford staining scores and SPEED scores after one month of drop therapy prior to cataract surgery, the average SPEED score improved by only 2–3 points, resulting in less than 40% improvement in symptoms.32,33 Overall, biometry performed after treatment with cAM more accurately predicted the post-operative refractive target compared to pre-treatment values, which is likely attributed to a more stable ocular surface as demonstrated by improved corneal signs. Post-operatively, average deviation from refractive target was 0.22 D, which was significantly lower than the predicted refractive error prior to treatment and is relatively lower than what has been previously reported (0.33D) following one month of treatment with cyclosporine 0.9%.33 Additionally, SE was within ±0.25 D of the refractive target in 36% of eyes before and 70% of eyes after treatment with cAM; within ±0.5 D in 66% of eyes before and 94% of eyes after; within ±0.75 D in 76% of eyes before and 98% of eyes after; and within ±1D in 86% eyes before and 100% of eyes after, which is also higher than previous studies that assessed other dry eye therapies.32,33 Ultimately, this resulted in 20/20 BCVA in more than 90% of eyes post-operatively.
The therapeutic benefits of cAM in treating DED have been previously reported and include its ability to reduce the signs, symptoms, and severity of DED as well as promote corneal nerve regeneration.16–19 This may be attributed to AM’s potent anti-inflammatory and wound healing properties.34 Nevertheless, one clear advantage of using cAM as a pre-surgical treatment option is its short treatment duration. While a number of other pharmacological treatments have been shown to improve the signs and symptoms of DED as well as biometry accuracy prior to cataract surgery, many of these drop therapies have a longer treatment duration of four weeks.32,33 Despite this, a subset of patients with more severe forms of DED may show minimal clinical benefit and require more aggressive therapy, further prolonging treatment duration. This notion is supported by the present study sample, which had both signs and symptoms of moderate to severe DED despite prior treatment with anti-inflammatory drops in nearly 30% of patients. Furthermore, it should be noted that non-compliance with other drop therapies prior to cataract surgery has been reported to be as high as 19%.32 While these patients were excluded and their outcomes not reported, it can be inferred that non-compliance may result in a reduced clinical benefit, and additional treatment measures may be required in these patients. Ultimately, this may be problematic as the ASCRS consensus panel recommends delaying cataract surgery until signs and symptoms of OSD are resolved.14 CAM is beneficial as it can resolve signs and symptoms of moderate to severe DED after only one week of treatment, mitigating the risk of surgical delays.
While addressing DED pre-operatively is imperative in obtaining accurate biometry measurements, it is also crucial in preventing worsened signs and symptoms post-operatively. Not only does the incidence of DED increase significantly following cataract surgery, it is also exacerbated in patients with pre-existing symptoms.11–13 Interestingly, in this study, we found that the benefit of cAM in reducing signs and symptoms of DED was still observed one month post-operatively, suggesting that pre-surgical treatment of DED may also help to reduce DED following cataract surgery. While other studies have demonstrated an improvement in signs and symptoms post-treatment, none have reported whether the benefit is maintained post-operatively. While Hovanesian et al32 found a subset of patients retained a beneficial ocular surface effect with lifitegrast at two months post-operatively, these patients received an additional four weeks of lifitegrast that began one month post-operatively. Conversely, patients in this study only received one week of treatment prior to cataract surgery.
There are several limitations in this study. First, there was not a control group in this study to assess whether cAM is superior to other conventional treatments. Nevertheless, this study was self-controlled, using pre-treatment data as the control to ultimately reduce variability that would otherwise be present if using a separate group of subjects as the comparative control group. Additionally, all patients presented with moderate to severe DED despite prior use of preservative free artificial tears in all patients, which is a commonly used vehicle control in randomized controlled trials. This suggests that a control group that received one week of treatment with artificial tears would not have resulted in a clinically significant benefit in our study sample. This is further supplemented by a study which demonstrated that use of artificial tears for two weeks appeared inadequate to significantly affect variability in biometric measurements for patients with dry eye prior to cataract surgery,35 which is a longer treatment duration than the current study (one week). Furthermore, other studied treatment options prior to cataract surgery, including lifitegrast and cyclosporine 0.09%, required four weeks of treatment, making these therapies difficult to use as a control group. Another limitation of this study is that it was conducted at a single-center; thus, this study sample may not be representative of the general population. In particular, 95% of patients in this study were females. This is unsurprising, however, as it is well established that the prevalence of dry eye is significantly higher in females, and females are more likely to undergo cataract surgery.36,37 When compared to males, females also report more severe dry eye symptoms, greater impact on daily activities, more use of dry eye treatments, and a greater amount of time before treatments start working.38,39 This may explain why more females were enrolled into this study, as patients were only included if they had moderate to severe dry eye and were refractory to conventional therapy. Based on the aforementioned information, one may infer that cAM would produce a similar treatment benefit in males, which is a less severe population that tends to respond more quickly to treatment.38,39 Lastly, the examiner assessing biometry and topography was not blinded to treatment status or timepoint. Nevertheless, the risk of bias is largely overcome by the objective nature of the measurements, which were generated by the Atlas and VX130+ topographers and the IOLMaster® 700. Despite the aforementioned limitations, these results suggest that cAM is a valuable therapy that can help optimize the ocular surface prior to cataract surgery.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
Preliminary results were presented at ASCRS 2023 (San Diego, CA) and ASCRS 2024 (Boston, MA).
Disclosure
Dr. Wongskhaluang received a grant from BioTissue, Inc. for this investigator-initiated study.
References
1. Brown GC, Brown MM, Busbee BG, et al. A cost-benefit analysis of 2018 cataract surgery in the United States. Clin Res Ophthalmol. 2019;2:1–13.
2. Kuo IC. Trends in refractive surgery at an academic center: 2007-2009. BMC Ophthalmol. 2011;11:11. doi:10.1186/1471-2415-11-11
3. Gibbons A, Ali TK, Waren DP, et al. Causes and correction of dissatisfaction after implantation of presbyopia-correcting intraocular lenses. Clin Ophthalmol. 2016;10:1965–1970. doi:10.2147/OPTH.S114890
4. Epitropoulos AT, Matossian C, Berdy GJ, et al. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg. 2015;41:1672–1677. doi:10.1016/j.jcrs.2015.01.016
5. Nilsen C, Gundersen M, Graae Jensen P, et al. The significance of dry eye signs on preoperative keratometry measurements in patients scheduled for cataract surgery. Clin Ophthalmol. 2024;18:151–161. doi:10.2147/OPTH.S448168
6. Teshigawara T, Akaishi M, Mizuki Y, et al. Effect of long-acting diquafosol sodium on astigmatism measurement repeatability in preoperative cataract cases with dry eyes: a multicenter prospective study. Ophthalmol Ther. 2024;13:1743–1755.
7. Gupta PK, Drinkwater OJ, VanDusen KW, et al. Prevalence of ocular surface dysfunction in patients presenting for cataract surgery evaluation. J Cataract Refract Surg. 2018;44:1090–1096. doi:10.1016/j.jcrs.2018.06.026
8. Starr CE, Yeh T, Merchea M. Prevalence of preoperative dry eye diagnosis and treatment among cataract surgery patients: an AAO IRIS® registry analysis.
9. Trattler WB, Majmudar PA, Donnenfeld ED, et al. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423–1430. doi:10.2147/OPTH.S120159
10. Graae Jensen P, Gundersen M, Nilsen C, et al. Prevalence of dry eye disease among individuals scheduled for cataract surgery in a Norwegian cataract clinic. Clin Ophthalmol. 2023;Volume 17:1233–1243. doi:10.2147/OPTH.S407805
11. Choi YJ, Park SY, Jun I, et al. Perioperative ocular parameters associated with persistent dry eye symptoms after cataract surgery. Cornea. 2018;37:734–739. doi:10.1097/ICO.0000000000001572
12. Iglesias E, Sajnani R, Levitt RC, et al. Epidemiology of persistent dry eye-like symptoms after cataract surgery. Cornea. 2018;37:893–898. doi:10.1097/ICO.0000000000001491
13. Cetinkaya S, Mestan E, Acir NO, et al. The course of dry eye after phacoemulsification surgery. BMC Ophthalmol. 2015;15:68. doi:10.1186/s12886-015-0058-3
14. Starr CE, Gupta PK, Farid M, et al. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J Cataract Refract Surg. 2019;45:669–684.
15. FDA. Request for designation: amniotic membrane for ocular surface reconstruction. Available from: https://www.fda.gov/downloads/CombinationProducts/JurisdictionalInformation/RFDJurisdictionalDecisions/RedactedDecisionLetters/UCM113701.pdf20012001.
16. McDonald MB, Sheha H, Tighe S, et al. Treatment outcomes in the DRy Eye Amniotic Membrane (DREAM) study. Clin Ophthalmol. 2018;12:677–681.
17. John T, Tighe S, Sheha H, et al. Corneal nerve regeneration after self-retained cryopreserved amniotic membrane in dry eye disease. J Ophthalmol. 2017;2017:6404918.
18. Cheng AM, Zhao D, Chen R, et al. Accelerated restoration of ocular surface health in dry eye disease by self-retained cryopreserved amniotic membrane. Ocul Surf. 2016;14:56–63.
19. Sheppard J, Yeu E, Tseng S. Sutureless cryopreserved amniotic membrane transplantation accelerates ocular surface healing and topographic stabilization for dry eye patients. Scand J Immunol. 2015;81:355–356.
20. Yeu E, Tighe S, Sheha H. Optimizing Ocular Surface Prior to Cataract Surgery. New Orleans, LA: AAO; 2017.
21. Vega Y, Gershoni A, Achiron A, et al. High agreement between Barrett Universal ii calculations with and without utilization of optional biometry parameters. J Clin Med. 2021;11:10. doi:10.3390/jcm11010010
22. Wang Q, Jiang W, Lin T, et al. Meta-analysis of accuracy of intraocular lens power calculation formulas in short eyes. Clin Exp Ophthalmol. 2018;46:356–363. doi:10.1111/ceo.13058
23. Chong EW, Mehta JS. High myopia and cataract surgery. Curr Opin Ophthalmol. 2016;27:45–50. doi:10.1097/ICU.0000000000000217
24. Koch DD, Ali SF, Weikert MP, et al. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38:2080–2087. doi:10.1016/j.jcrs.2012.08.036
25. Lin J, An D, Wu H, et al. Quantifying posterior corneal astigmatism’s contribution to ocular residual astigmatism: implications for personalized refractive surgery. Int Ophthalmol. 2025;45:143.
26. Liu W, Yang L, Liu J. The impact of posterior corneal astigmatism on surgically induced astigmatism in cataract surgery. Int J Gen Med. 2022;15:8417–8425. doi:10.2147/IJGM.S382774
27. Lemp MA. Report of the national eye institute/industry workshop on clinical trials in dry eyes. CLAO J. 1995;21:221–232.
28. Asiedu K, Kyei S, Mensah SN, et al. Ocular Surface Disease Index (OSDI) Versus the Standard Patient Evaluation of Eye Dryness (SPEED): a study of a nonclinical sample. Cornea. 2016;35:175–180. doi:10.1097/ICO.0000000000000712
29. Davison JA, Potvin R. Preoperative measurement vs intraoperative aberrometry for the selection of intraocular lens sphere power in normal eyes. Clin Ophthalmol. 2017;11:923–929. doi:10.2147/OPTH.S135659
30. Abdelghany AA, Alio JL. Surgical options for correction of refractive error following cataract surgery. Eye Vis. 2014;1:2.
31. Baulig C, Knippschild S, Krummenauer F. Meta-analysis of drop out rates in cataract surgery RCTs - an update. Br J Med Med Res. 2016;17:1–17.
32. Hovanesian J, Epitropoulos A, Donnenfeld ED, et al. The effect of lifitegrast on refractive accuracy and symptoms in dry eye patients undergoing cataract surgery. Clin Ophthalmol. 2020;14:2709–2716. doi:10.2147/OPTH.S264520
33. Hovanesian JA, Berdy GJ, Epitropoulos A, et al. Effect of Cyclosporine 0.09% Treatment on Accuracy of Preoperative Biometry and Higher Order aberrations in dry eye patients undergoing cataract surgery. Clin Ophthalmol. 2021;15:3679–3686. doi:10.2147/OPTH.S325659
34. Tseng SC, Espana EM, Kawakita T, et al. How does amniotic membrane work? Ocul Surf. 2004;2:177–187. doi:10.1016/S1542-0124(12)70059-9
35. Nilsen C, Gundersen M, Jensen PG, et al. Effect of artificial tears on preoperative keratometry and refractive precision in cataract surgery. Clin Ophthalmol. 2024;18:1503–1514.
36. Hagström A, Sabazade S, Gill V, et al. Association of female sex with cataract surgery in the general population but not in plaque brachytherapy-treated uveal melanoma patients. Sci Rep. 2024;14:22016.
37. Matossian C, McDonald M, Donaldson KE, et al. Dry eye disease: consideration for women’s health. J Womens Health. 2019;28:502–514. doi:10.1089/jwh.2018.7041
38. Chiang JCB, Wolffsohn JS. Perspectives of dry eye patients in the United Kingdom on risk factors and desired treatment outcomes. Contact Lens Anterior Eye. 2025;48:102340. doi:10.1016/j.clae.2024.102340
39. Schaumberg DA, Uchino M, Christen WG, et al. Patient reported differences in dry eye disease between men and women: impact, management, and patient satisfaction. PLoS One. 2013;8:e76121. doi:10.1371/journal.pone.0076121
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.