Back to Journals » Clinical Ophthalmology » Volume 18
Outcomes of Ahmed Glaucoma Valve Implantation with Subsequent Trans-Scleral Diode Cyclophotocoagulation as the Main Intervention if IOP Remained Medically Uncontrolled
Authors Radhakrishnan S , Kots-Gotlib N, Pickering TD, McCurdy J, Siu J, Pham D, Iwach AG
Received 30 October 2024
Accepted for publication 10 December 2024
Published 17 December 2024 Volume 2024:18 Pages 3825—3836
DOI https://doi.org/10.2147/OPTH.S498973
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sunita Radhakrishnan,1,2 Nadiya Kots-Gotlib,2 Terri-Diann Pickering,1 Jordan McCurdy,3 Joshua Siu,4 Don Pham,5 Andrew G Iwach1,2
1Glaucoma Center of San Francisco, San Francisco, CA, USA; 2Glaucoma Research & Education Group, San Francisco, CA, USA; 3David Geffen School of Medicine @ UCLA, Los Angeles, CA, USA; 4Valley Hospital Medical Center, Las Vegas, NV, USA; 5Beaumont/Corewell Health, Taylor, MI, USA
Correspondence: Sunita Radhakrishnan, Glaucoma Center of San Francisco, 55 Stevenson Street, San Francisco, CA, 94105, USA, Tel +1 415 981 2020, Fax +1 415 981 2019, Email [email protected]
Purpose: To evaluate the efficacy and safety of Ahmed glaucoma valve (AGV) implantation with subsequent trans-scleral diode cyclophotocoagulation (CPC) as the main intervention if IOP remained medically uncontrolled.
Patients and Methods: Charts of 108 consecutive eyes (90 patients) that underwent AGV implantation from 2003 to 2018 at a single clinical practice were retrospectively reviewed. The procedure was considered a failure if any of the following occurred: additional incisional glaucoma surgery, IOP > 21 mmHg or < 20% reduction from baseline on 2 consecutive study visits after 3 months, IOP ≤ 5 mmHg on 2 consecutive study visits after 3 months, loss of light perception, or AGV removal.
Results: The mean follow-up time was 5.4 ± 3.1 years. Diode CPC was performed in 32%. The mean IOP was 24.8 ± 8.2 mmHg before intervention, and 12.5 ± 5.6 mmHg at last follow-up (p< 0.0001). The mean logMAR VA decreased by 0.24 (p=0.002). The success rate was 68%. The reasons for failure were additional incisional glaucoma surgery in 7%, AGV removal in 4%, loss of light perception in 4%, inadequate IOP reduction in 13%, and IOP ≤ 5 mm HG in 6%. The probability of survival by Kaplan Meier analysis was 88%, 76% and 69% at 1, 3, and 5 years after the procedure, respectively. Complications of AGV and CPC were comparable to those previously reported in the literature.
Conclusion: The treatment approach of AGV implantation with subsequent trans-scleral diode CPC, as needed, was successful in over 2/3rd of subjects. This study adds to the literature supporting the use of CPC when IOP is medically uncontrolled after AGV.
Keywords: surgery, laser, valved glaucoma implant, cyclodestruction
Introduction
Glaucoma drainage devices are an important option for intraocular pressure (IOP) management when other therapies have failed. However, even after placement of these devices, the IOP may not be well controlled. In the pooled data analysis of the Ahmed Baerveldt Comparison (ABC) and the Ahmed Versus Baerveldt (AVB) studies, the cumulative failure rate at 5 years was 49% in the Ahmed group and 37% in the Baerveldt group, and high IOP was the most common reason for failure in both groups.1 Most patients continue to require medical therapy after glaucoma drainage device (GDD) placement and for those who need further intervention, the commonly used options are cyclophotocoagulation (CPC) or a second GDD.
In patients with glaucoma who have already been treated with non-incisional measures, and who are not candidates for minimally invasive glaucoma surgery (MIGS) or have already undergone MIGS, it has been our preference to perform the Ahmed Glaucoma Valve (AGV) implant and then treat with trans-scleral diode CPC if IOP remains uncontrolled despite restarting medical therapy. Although a GDD is considered to have “failed” if any type of additional IOP lowering intervention is required, we propose that a diode CPC in this setting merits a different consideration than incisional surgery. Diode CPC is a non-incisional procedure with inherently lower risk than an incisional procedure. Also, when diode CPC is performed for additional IOP control after GDD placement, the extent of treatment required is typically lower than if diode CPC were the primary IOP lowering treatment.2–4 Thus side effects can be minimized while maintaining efficacy. Furthermore, use of the “slow-coagulation” technique of CPC is associated with less inflammation when compared to the traditional CPC settings.5
We know that glaucoma is a chronically progressive disease and the currently available treatment modalities are all frequently associated with a gradual loss of IOP control over time. Since patients with glaucoma are living longer, we need ways to extend the duration of IOP control so that functional vision can be maintained lifelong. In our opinion, the treatment approach of AGV implant supplemented by slow-coagulation diode CPC, when needed, takes advantage of the favorable safety profiles of both procedures while maximizing IOP lowering efficacy.
To the best of our knowledge there is no previous data published on this treatment strategy since the studies on aqueous drainage devices consider CPC as a criterion for failure and censor these patients from further IOP analysis. This prevailing perspective of analyzing GDDs as a “one and done” procedure where any additional intervention is deemed a failure, is restrictive and rather unrealistic. It is more practical to anticipate the need for additional treatment and consider how to achieve long term IOP control after a GDD while minimizing complications.
The treatment strategy described in this study also differs from published studies regarding CPC for medically uncontrolled IOP following an aqueous drainage device. The latter include only that subset of patients who required additional intervention after a GDD and do not reflect the entire group that received the drainage device. Thus, there is a lack of practically useful data on the longer-term course after drainage device placement, especially in those patients who require further intervention. In this study, our aim is to address this gap and present our experience with AGV implantation and subsequent diode CPC as the main intervention if IOP remained medically uncontrolled.
Materials and Methods
Patients
This was a single center retrospective study of consecutive patients who underwent AGV implantation during a 15-year period from 2003 to 2018. The study was approved by an independent institutional review board (Advarra) and complied with the tenets of the Declaration of Helsinki. Since the study was retrospective in nature, the subjects whose charts were reviewed were not available to provide informed consent, and therefore a waiver of informed consent was approved by the institutional review board. Patient data confidentiality was maintained by following the standards for handling protected health information.
Patient charts were reviewed and the following baseline parameters were collected: age, gender, race, glaucoma type, lens status, previous glaucoma procedures, vertical cup to disc ratio (VCDR), Humphrey visual field mean deviation (HVF MD), and central corneal thickness (CCT). Visual acuity, IOP, and number of glaucoma medications were recorded at baseline and at each of the following post-operative timepoints – 1 day, 1 week, 1 month, 3 months, 6 months, 12 months, and yearly thereafter until the last follow-up visit. Surgery details that were recorded included surgeon, location of AGV plate and tube, type of patch graft, and complications.
Surgical Technique
All cases were performed by one of 3 glaucoma fellowship-trained surgeons and the AGV model used most often was the FP7. A few eyes were implanted with the FP8 and S2 models. A fornix-based conjunctival flap was dissected in the superotemporal quadrant; if there was extensive scarring superotemporally, then the inferonasal quadrant was used. The implant was primed with balanced salt solution, placed in the subTenon space, and the anterior edge was sutured to the sclera 8–9 mm posterior to the limbus using two 8–0 nylon sutures. The tube tip was then trimmed bevel up to extend about 2 mm if placed in the AC and 3.5 to 4 mm if placed into the anterior vitreous cavity. For insertion into the AC, a 22 G needle was used to create a tract starting 2–3 mm posterior to the limbus. For insertion via the pars plana, if there was concurrent vitrectomy, then the superotemporal (or inferonasal) vitrectomy port was used as the tube entry site and if the eye had been already vitrectomized in a separate prior surgery, then a 22 G needle was used to create a tract into the anterior vitreous cavity starting 3.5 mm posterior to the limbus. In cases with concurrent vitrectomy, the AGV plate was first sutured to the sclera. The retina specialist then placed three 25G vitrectomy ports and the port in the implant quadrant was inserted without tunneling. After the vitrectomy and any concurrent retinal procedure was completed, the vitreous base in the AGV quadrant was carefully inspected and further shaved if necessary. The port in this quadrant was then removed and the trimmed tube was inserted through the scleral opening into the anterior vitreous. After tube insertion, a patch graft was placed over the tube’s entry site and sutured to the sclera with 8–0 vicryl sutures. Commercially available preserved pericardium was the most commonly used graft; the other materials used were preserved sclera or preserved split thickness cornea. A few cases were performed using a scleral tunneling technique without the use of a patch graft. In most cases, the tube was not separately anchored to sclera. The conjunctiva was then closed using 8–0 vicryl sutures. Post-operatively, steroid (prednisolone acetate or difluprednate) and moxifloxacin drops were initiated at 3–4 times a day. Antibiotic drops were used for 2 weeks and steroid was tapered over 4–6 weeks based on the surgeon’s discretion. Pre-operative IOP lowering medications were restarted if IOP was not well controlled. At around 2011 or so, the authors’ modified this part of the post-operative management and began to routinely restart aqueous suppressants when IOP was over 10 mm Hg. Other pre-operative IOP lowering medications were also resumed if IOP was not well controlled. If IOP remained uncontrolled despite restarting medical therapy, then additional intervention with trans-scleral diode CPC was performed in all cases except those where CPC was contraindicated, or a different IOP lowering procedure was deemed more appropriate by the treating surgeon. Diode CPC was performed using the Iridex G-Probe with power of 1.25 to 2 W and duration of 2 to 4 seconds. The number of laser applications was usually 15 or less. Post-operatively prednisolone eyedrops were initiated at 4 times a day and then tapered over 2–4 weeks based on the degree of inflammation. If further IOP lowering intervention was required after one diode CPC, the decision to perform additional CPC versus another IOP lowering intervention was based on the treating surgeon’s discretion.
Data Analysis
The AGV implant was considered a failure if any of the following occurred: additional IOP lowering incisional surgery (trans-scleral CPC was allowed since the goal of the study was to evaluate outcomes of AGV with subsequent CPC, as needed), IOP >21 mmHg or less than 20% reduction from baseline on 2 consecutive study visits after 3 months, IOP ≤ 5 mmHg on 2 consecutive study visits after 3 months, loss of light perception, or removal of the implant for any reason.
The time to failure was defined as the time from AGV implantation to additional IOP lowering incisional surgery, loss of acuity to NLP, removal of the AGV implant, or the first of 2 consecutive study visits after 3 months in which the patient had persistent hypotony (IOP ≤5 mmHg) or inadequately controlled IOP (IOP >21 mmHg or not reduced by 20%). Data on IOP and numbers of glaucoma medications were censored once a patient had additional IOP lowering incisional surgery, AGV implant removal, or loss of light perception, but not after trans-scleral CPC, surgical intervention for a complication, or failure due to high IOP or hypotony. Last follow-up was defined as the date of last available follow-up or the last follow-up until failure due to additional IOP lowering incisional surgery, loss of acuity to NLP, or AGV implant removal.
Statistical analysis was performed using SAS® v9.4. A p-value of less than 0.05 was considered significant. Due to a minority of patients who contributed two eyes to the analyses, all eyes were considered and analyzed as independent observations. Continuous parameters were compared using a t-test and the Chi-squared test was used for categorical parameters. Cox proportional hazards model was used to evaluate factors associated with survival time of AGV implant. The variables included in the analysis were age, gender, race, type of glaucoma, VCDR, HVF MD, lens status, CCT, baseline IOP, number of IOP lowering medications, use of oral IOP lowering agents, baseline VA, prior glaucoma surgery, prior CPC, surgeon, tube tip location, primary AGV (versus AGV after prior glaucoma surgery), and duration between surgery and post-operative IOP elevation above 10mm Hg.
Results
A total of 108 eyes of 90 patients were enrolled in the study. Table 1 shows their baseline characteristics. The mean age was 66 years, 52% of patients were male, and 57% were Caucasian. The most common type of glaucoma was POAG (48%, 52/108), and 64% (69/108) were pseudophakic. Forty four percent (47/108) had undergone prior incisional glaucoma surgery and the mean number of incisional procedures prior to AGV implantation was 1.7 ± 0.9 (range 1 to 4). Eleven percent (12/108) had undergone prior trans-scleral CPC, including micropulse CPC (10/12) and diode CPC (2/12). Humphrey visual field data were available for 102 eyes (94% of the total sample). The mean defect was −12.60 ± 7.82 dB (range −0.78 to −32.62 dB); 22% (22/102) had a mild defect (−6.00 dB or better), 32% (32/102) had a moderate defect (−6.01 dB to −12.00 dB), and 48% (48/102) had a severe defect (worse than −12.00 dB). The mean VCDR was 0.8 ± 0.2. The tube tip was placed in the anterior chamber in 81% (87/108), the pars plana in 19% (20/108), and the sulcus in 1% (1/108). Of the 20 eyes that had pars plana placement of the tube, 65% (13/20) had pars plana vitrectomy concurrent to AGV placement. The patch graft material used was pericardium in 78% (84/108), cornea in 13% (14/108), sclera in 8% (9/108), and dura substitute in 1% (1/108).
 |
Table 1 Baseline Characteristics |
Trans-scleral CPC was performed in 32% (35/108 eyes) and included diode CPC in 94% (33/35 eyes) and micropulse CPC in 6% (2/35 eyes). Among the 35 eyes that underwent trans-scleral CPC, 66% (23/35 eyes) had 1 CPC, 17% (6/35 eyes) had 2 CPCs, and the remaining (17%, 6/35 eyes) had 3 to 6 CPCs. The average number of spots for the first diode CPC was 13 ± 2 (range 9–18, median 14). The average number of spots for the second diode CPC was 13 ± 3 (range 10–18, median 12). The mean interval between AGV and first CPC was 24.4 ± 29.2 months (range 1 month to 9.3 years).
The mean follow-up time was 5.4 ± 3.1 years, with a range of 5 months to 18.75 years. Post-operative data were available for 99%, 92%, 88%, 78%, 65%, and 35% of eyes at 1 day, 6 months, 1 year, 2 years, 4 years, and 6 years, respectively.
Intraocular Pressure and Efficacy Outcomes
Mean IOP decreased from 24.8 ± 8.2 mmHg pre-operatively to 12.5 ± 5.6mm Hg at last follow-up, a 46% reduction (p < 0.0001). [Figure 1 and Table 2]. There was also a decrease in the average number of medications from 3.5 ± 1.1, before intervention, to 2.1 ± 1.4 at last follow-up.
 |
Table 2 IOP & Medications Before and After Ahmed Glaucoma Valve Supplemented with Diode Cyclophotocoagulation |
 |
Figure 1 Intraocular pressure (IOP) after Ahmed Glaucoma Valve (AGV). |
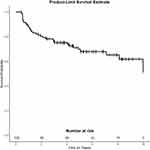
The AGV implant with subsequent CPC, as needed, was successful in 68% (73/108 eyes). The probability of survival by Kaplan Meier analysis was 88%, 80%, 76% and 69% at 1, 2, 3, and 5 years after the procedure, respectively (Figure 2). The reasons for failure (Table 3) were additional incisional glaucoma surgery in 7% (7/108 eyes), AGV removal in 4% (4/108 eyes), loss of light perception in 4% (4/108 eyes), inadequate IOP lowering in 13% (14/108 eyes) and IOP ≤ 5 mm HG in 6% (6/108 eyes). The additional incisional surgeries included Kahook dual blade goniotomy (combined with cataract surgery) in 3 eyes, second AGV in 2 eyes, AGV replacement with supraTenon Baerveldt implant in 1 eye, and endocyclophotocoagulation in 1 eye. Among the 7 eyes that had further incisional surgery after AGV, CPC was not considered appropriate in 5 eyes due to active uveitis, or the surgeon’s judgement that a different procedure was more appropriate; the remaining 2 eyes underwent 2 diode CPCs but IOP remained uncontrolled and therefore further incisional surgery was performed. Of those who failed due to the inadequate IOP lowering criterion, 64% (9/14) did not have any further intervention, and 36% (5/14) underwent diode CPC. Of the 6 eyes that failed due to IOP being 5 mm HG or lower, three underwent surgical revision, 1 eye had low IOP due to traumatic retinal detachment, and 2 eyes of the same patient had numerical hypotony which did not affect vision or require treatment. If CPC was included as a criterion for failure, then the probability of survival of the AGV implant was 72%, 62%, 57% and 47% at 1, 2, 3, and 5 years after the procedure, respectively (Figure 3). Kaplan Meier analysis was also performed for the subset of 35 eyes that underwent diode CPC. The probability of survival in this subgroup was 86%, 74%, 71%, and 71% at 1, 2, 3 and 5 years respectively.
 |
Table 3 Reasons for Failure After Ahmed Glaucoma Valve with Subsequent Cyclophotocoagulation, as Needed |
Using multivariable Cox proportional hazards models, none of the factors analyzed were found to be associated with survival of the AGV implant.
Safety Outcomes
Visual Acuity
Loss of light perception occurred in 4% (4/108 eyes); 3 of these 4 eyes had neovascular glaucoma with pre-operative visual acuity at counting fingers or worse, 1 eye with pre-operative visual acuity of 20/100 had glaucoma progression in the setting of non-adherence with topical therapy, and long gaps in follow-up.
In eyes that retained vision at last follow-up, Snellen visual acuity was within 1 line of baseline in 51% (55/108), worse by ≥4 lines in 12% (13/108), and better by ≥ 4 lines in 6% (7/108). Of the 13 eyes with reduced vision from baseline, 4 eyes had reduced vision due to corneal edema, 2 eyes due to cataract, and 1 eye each due to endophthalmitis, epiretinal membrane, macular degeneration, and corneal graft failure. In 2 eyes, there was no obvious cause for reduced vision. In the 7 eyes that had improved vision from baseline, 3 eyes had poor vision pre-operatively due to high intraocular pressure and cornea edema, and the vision improved after post-surgical IOP reduction. The remaining 4 eyes had improved vision following cataract surgery, corneal transplantation, and repositioning of a subluxed intraocular lens.
The change in logMAR visual acuity from before surgery to last follow-up was significant with a mean decrease of 0.24 (approximately 2 Snellen lines, p = 0.002, t test).
Complications
There were no complications after AGV implantation in 52% (56/108 eyes, Table 4). Corneal edema occurred in 10% (11/108 eyes) and of these 11 eyes, 8 had new and persistent corneal edema after AGV, and 3 eyes had worsening of pre-existing corneal edema. Of the 8 eyes that had new onset corneal edema, 5 had pre-existing or concurrent factors that increased the risk of developing corneal edema, such as, flat anterior chamber with previous glaucoma filtering surgery, cataract surgery complicated by vitreous loss, iridocorneoendothelial syndrome, ocular ischemic syndrome with recurrent hyphema, and chronic hypotony. There were 12 eyes (11% of 108) with corneal transplants, and corneal graft failure after AGV implantation occurred in 6 of these eyes (50% of 12). All six eyes with corneal transplant failure had undergone AGV implantation in the AC, and 4 of these 6 eyes had the corneal transplant following AGV implantation. Of the 6 eyes in which the corneal transplant was stable, the corneal surgery preceded the AGV implant in 4 eyes, and the AGV was placed in the pars plana in 4 eyes. Binocular diplopia occurred in 7% (8/108 eyes); in 5 of these 8 eyes diplopia resolved within 3 months of the AGV implant and 3 of the 8 eyes had persistent diplopia requiring treatment. Hyphema lasting over a month occurred in 2% (2/108 eyes) and vitreous hemorrhage occurred in 3% (3/108 eyes, one eye required vitrectomy). Complications related to exposure of the AGV implant occurred in 12% (13/108 eyes) and included tube exposure (9 eyes, 8%), plate exposure (2 eyes), plate suture exposure with leak (1 eye), and patch graft exposure requiring surgical revision (1 eye). All of these eyes had either tube revision or AGV removal, except for one eye with early post-operative tube erosion that was noted to have spontaneously closed when the patient was brought to the operating room for revision. Of the 9 eyes that had tube erosion, all had tube placement in the AC, 8 were placed in the superotemporal quadrant and 1 in the inferotemporal quadrant, and all had placement of patch graft (6 eyes with pericardium, and 1 each with cornea, sclera, and Dura substitute). Endophthalmitis occurred in 2% (2/108 eyes); 1 of these eyes had tube exposure and the other had plate exposure. Tube obstruction requiring surgical revision occurred in 2% (2/108 eyes). One eye had sulcus tube placement and had elevated IOP at the first post-operative day and the tube was repositioned to the pars plana. The other eye had prior complete vitrectomy and underwent pars plana AGV implantation. On the third post-operative day, there was symptomatic IOP elevation; the patient then underwent pars plana vitrectomy to remove residual vitreous that was obstructing the tube. The AGV implant was removed in 4% (4/108 eyes) due to recurrent tube erosion (3 eyes), and plate exposure with endophthalmitis (1 eye). Two eyes (2% of 108) had rapid progression of cataract within 10 days of AGV implantation, one underwent cataract surgery and regained pre-AGV visual acuity, the other eye had pre-existing poor visual potential due to retinal pathology and therefore no further intervention was performed.
 |
Table 4 Complications After Ahmed Glaucoma Valve (AGV) Implantation |
Additional non-IOP lowering interventions that occurred during the follow-up period included cataract surgery in 8% (9/108), partial or full-thickness corneal transplant in 6% (6/108), Yag capsulotomy or surgical capsulectomy in 5% (5/108), IOL repositioning in 2% (2/108), and multiple interventions (retinal detachment repair followed by corneal transplant and cataract surgery) in 1% (1/108).
Thirty-five eyes (32% of 108) underwent CPC after AGV implantation. There were no complications after CPC in 80% (28/35 eyes, Table 5). Macular edema occurred in 6% (2/35 eyes) – both eyes required long-term topical anti-inflammatory agents and retained good visual acuity. Prolonged and recurrent iritis occurred in 6% (2/35 – both eyes of the same patient). This patient required maintenance treatment with topical steroid and retained good visual acuity in both eyes. Corneal complications included worsening of corneal edema in 6% (2/35 eyes), and corneal graft failure in 3% (1/35 eyes).
 |
Table 5 Complications After Trans-Scleral Diode Cyclophotocoagulation (CPC) |
Discussion
In this retrospective study, the treatment approach of AGV with subsequent slow-coagulation trans-scleral diode CPC, if IOP remained medically controlled, was successful in over 2/3 of subjects. Complications noted in this study were comparable to those reported in previous studies.
The main goal of glaucoma treatment is to maintain functional vision throughout the patient’s lifetime. This is achieved through controlling intraocular pressure by various means, all of which tend to lose efficacy with time. Aqueous drainage devices are typically utilized when a patient has uncontrolled IOP despite the use of non-incisional glaucoma therapy, and these devices may be used either as the primary incisional glaucoma therapy or following other surgical treatments such as angle-based surgery and filtering bleb surgery. Even after GDD implantation, most patients still require medical therapy, and some may need additional intervention.
When IOP is not medically controlled after AGV implantation, the commonly used treatment options include a second GDD or trans-scleral CPC. The available data indicates that CPC has an advantage over a second drainage device in this setting. The Second Aqueous Shunt Implant versus Transscleral Cyclophotocoagulation Treatment Study (ASSISTS) was a randomized controlled trial that compared a second drainage device (n = 22) and CPC (n=20) in eyes that had inadequately controlled IOP despite placement of one GDD and medications.4 The study had a follow-up of 18 months and showed that both approaches had high short-term success rates, but a second GDD was associated with a higher risk of additional glaucoma surgery. In a retrospective study by Levinson et al, sequential GDD implantation (n=32) was compared to CPC (n=21) following failure of a primary drainage device.6 The review period was 10 years and the authors reported that both procedures reduced IOP, but CPC led to a greater IOP reduction and the likelihood of corneal decompensation in eyes without pre-existing corneal edema was much lower for CPC.
In patients with glaucoma who require additional intervention besides medications, laser trabeculoplasty, and angle-based MIGS, our preferred surgical approach is the AGV implant. If IOP remains uncontrolled after AGV implantation and restarting medical therapy, our preferred treatment modality is a limited trans-scleral diode CPC using the “slow-coagulation technique”. In this retrospective study, we reviewed patients who underwent AGV implantation over a 15-year period. The definition of failure included multiple outcomes and based on these criteria 68% of eyes were successful. Diode CPC was performed in 32%, and 2/3rd of these required only 1 CPC treatment. Most of the failures were due to inadequate IOP lowering which was defined based on previously described and commonly used criteria. However, the clinical decision of whether IOP control is adequate or not is based on multiple factors and not solely on IOP reduction. This is illustrated by the fact that nearly two-third of eyes that “failed” by the IOP lowering criteria did not undergo any further intervention; the rest underwent diode CPC, and none had further incisional glaucoma surgery.
For direct comparison of our study with previous studies on the AGV implant, we also analyzed our data using the same failure criteria as the Ahmed Baerveldt Comparison (ABC) study.7 The ABC study was a randomized controlled trial which compared the AGV to the Baerveldt implant, and it considered CPC as a criterion for failure. The 5-year probability of survival in the current study decreased from 69% (when diode CPC was not considered a failure) to 47% when using the ABC study criteria for failure. This was comparable to the 5- year survival probability of 45% reported in the AGV arm of the ABC study. Although the probability of survival was similar in the two studies, the total number of subjects who needed any IOP lowering intervention after AGV was higher in this study than in the ABC study. This could be due to several factors including the lower mean pre-op IOP in this study (24.8 ± 8.2 mm Hg versus 31.2 ± 10.9 in ABC) and the longer duration of follow-up in this study. In addition, the ABC study had a much higher proportion of subjects with NVG (29% versus 4% in this study) and these subjects typically do not require as low a target IOP as patients with primary open angle glaucoma (POAG). The proportion of subjects with POAG was higher in this study (52% versus 41% in the ABC study) and although target IOP was not available for every subject, 23 of 108 eyes (21%) had a documented target IOP of less than 13 mm HG (range 8–12 mm HG).
The Ahmed Versus Baerveldt (AVB) study was another randomized controlled trial that compared the Ahmed and Baerveldt implants and, like the ABC study, it defined diode CPC as a criterion for device failure.8 The number of subjects needing any glaucoma intervention after AGV was again higher in our study when compared to the AGV arm of the AVB study, and this was likely for the same reasons that have been noted above. The mean baseline IOP and proportion of subjects with NVG were both higher in the AVB study than in this study.
Post-operative complications after AGV in the current study were comparable to those reported in the AGV arms of the ABC and AVB studies.8,9 Corneal edema occurred in 10% in this study with most having new onset edema. However, many of these eyes had pre-existing factors that are associated with an increased likelihood of developing corneal edema. In comparison, the AVB study reported corneal edema in 11% and the ABC study reported persistent corneal edema in 20% with edema attributable to the tube shunt in 11%. Consistent with previous data,10 this study also showed a high rate of corneal transplant failure in eyes with AGV. Pars plana placement of the tube was associated with a lower incidence of failure in this study. Sulcus placement has been reported to have lower endothelial loss than placement in the AC but could not be evaluated in this study.11 Tube erosion occurred in 8% over a mean follow-up period of slightly over 5 years (range 5 months to 18.75 years). In comparison, the ABC and AVB studies reported tube erosion in 3% and 4% respectively, over 5 years. Binocular diplopia occurred in 7% with only 3% having persistent diplopia that required treatment. In comparison, binocular diplopia occurred in 13% and 5% respectively in the ABC and AVB studies. Loss of light perception occurred in 4% in this study compared to 12% and 6% respectively in the ABC and AVB studies both of which had a higher proportion of eyes with neovascular glaucoma than the current study. Removal of the AGV implant occurred in 4% in this study compared to 5% and 0.8% respectively in the ABC and AVB studies. Hypotony requiring tube revision occurred in 3% in this study compared to 0.6% and 1% respectively in the ABC and AVB studies.
Complications after diode CPC in this study were comparable to those previously reported, and none of the eyes developed hypotony after CPC.12 Nearly 95% of the eyes that underwent CPC in this study had diode CPC. Although micropulse CPC is an alternative to diode CPC, we have previously reported that nearly 50% of eyes that underwent micropulse CPC required further IOP lowering intervention and 11% had persistent complications.13 Therefore, we prefer diode CPC over micropulse CPC.
The limitations of our study include its retrospective nature which has inherent drawbacks compared to a prospective study. Treatment decisions were based on each surgeon’s discretion and the treatment protocol was not standardized. There was also no comparator group in the study. In addition, the specific treatment approach we describe is associated with a good safety and efficacy profile in our hands and in our patient population but may not be generalizable to other settings.
In conclusion, we present a cohort of patients treated with AGV implant followed by trans-scleral diode CPC as the main intervention if IOP remained medically uncontrolled. The efficacy and safety of this treatment approach was comparable to previously published reports on these two procedures. The proportion of subjects requiring diode CPC after AGV was higher than in previous reports on the AGV implant, likely due to differences in subject characteristics as well as the longer duration of follow-up in this study.
Acknowledgments
- Funding/Support: Glaucoma Research Foundation, San Francisco, CA.
- Statistician: Srichand Jasti ME, MStat, PhD – Hillsborough, NJ
Disclosure
SR: Netra Systems Inc. (Consultant); AI: Belkin Lasers, Alcon, Ophthalmic Mutual Insurance Company (Consultant), and Eyenovia (Stock Owner). The authors report no other conflicts of interest this work.
References
1. Christakis PG, Zhang D, Budenz DL, et al. ABC-AVB study groups. five-year pooled data analysis of the Ahmed Baerveldt comparison study and the Ahmed versus Baerveldt study. Am J Ophthalmol. 2017;176:118–126. doi:10.1016/j.ajo.2017.01.003
2. Egbert PR, Fiadoyor S, Budenz DL, Dadzie P, Byrd S. Diode laser transscleral cyclophotocoagulation as a primary surgical treatment for primary open-angle glaucoma. Arch Ophthalmol. 2001;119:345–350. doi:10.1001/archopht.119.3.345
3. Lai JS, Tham CC, Chan JC, Lam DS. Diode laser transscleral cyclophotocoagulation as primary surgical treatment for medically uncontrolled chronic angle closure glaucoma: long-term clinical outcomes. J Glaucoma. 2005;14:114–119. doi:10.1097/01.ijg.0000151890.41239.c5
4. Feldman RM, Chuang AZ, Mansberger SL, et al.; Assists GroupOutcomes of the second aqueous shunt implant versus transscleral cyclophotocoagulation treatment study: a randomized comparative trial. J Glaucoma. 2022;31(9):701–709. doi:10.1097/IJG.0000000000002079
5. Duerr ERH, Sayed MS, Moster SJ, et al. Transscleral diode laser cyclophotocoagulation: a comparison of slow coagulation and standard coagulation techniques. Ophthalmol Glaucoma. 2018;1(2):115–122. doi:10.1016/j.ogla.2018.08.007
6. Levinson JD, Giangiacomo AL, Beck AD, et al. A comparison of sequential glaucoma drainage device implantation versus cyclophotocoagulation following failure of a primary drainage device. J Glaucoma. 2017;26(4):311–314. doi:10.1097/IJG.0000000000000370
7. Budenz DL, Barton K, Gedde SJ, et al.; Ahmed Baerveldt Comparison Study Group. Five-year treatment outcomes in the Ahmed Baerveldt comparison study. Ophthalmology. 2015;122(2):308–316. doi:10.1016/j.ophtha.2014.08.043
8. Christakis PG, Kalenak JW, Tsai JC, et al. Ahmed versus Baerveldt study: five-year treatment outcomes. Ophthalmology. 2016;123(10):2093–2102. doi:10.1016/j.ophtha.2016.06.035
9. Budenz DL, Feuer WJ, Barton K, et al. Ahmed Baerveldt comparison study group. postoperative complications in the Ahmed Baerveldt comparison study during five years of follow-up. Am J Ophthalmol. 2016;163:75–82. doi:10.1016/j.ajo.2015.11.023
10. Ayyala RS. Penetrating keratoplasty and glaucoma. Surv Ophthalmol. 2000;45(2):91–105. doi:10.1016/S0039-6257(00)00141-7
11. Zhang Q, Liu Y, Thanapaisal S, et al. The effect of tube location on corneal endothelial cells in patients with Ahmed glaucoma valve. Ophthalmology. 2021;128(2):218–226. doi:10.1016/j.ophtha.2020.06.050
12. Anand N, Klug E, Nirappel A, Solá-Del Valle D. A review of cyclodestructive procedures for the treatment of glaucoma. Semin Ophthalmol. 2020;35(5–6):261–275. doi:10.1080/08820538.2020.1810711
13. Radhakrishnan S, Wan J, Tran B, et al. Micropulse cyclophotocoagulation: a multicenter study of efficacy, safety, and factors associated with increased risk of complications. J Glaucoma. 2020;29(12):1126–1131. doi:10.1097/IJG.0000000000001644
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.