Back to Journals » Clinical Ophthalmology » Volume 18
Pattern of Spheroidal Degeneration of Cornea and Its Association with Other Eye Diseases at Anterior Segment Clinic in Menelik II Tertiary Referral Hospital
Authors Tesfay K , Shibeshi MA
Received 20 August 2024
Accepted for publication 14 November 2024
Published 23 November 2024 Volume 2024:18 Pages 3417—3423
DOI https://doi.org/10.2147/OPTH.S492306
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Kiros Tesfay, Menen Ayalew Shibeshi
Department of Ophthalmology, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Kiros Tesfay, Email [email protected]
Purpose: The purpose of the study was to assess the pattern of spheroidal degeneration of cornea (SDC) and its association with other eye diseases at the anterior segment clinic (ASC) in Menelik II Tertiary Referral Hospital.
Methods: A hospital-based prospective descriptive study was conducted at ASC, in Menelik II Tertiary Referral Hospital, from May 2021 to September 2022. All enrolled patients meeting the inclusion criteria were selected and assessed with a structured questionnaire. Descriptive analysis was used to describe the study variables in terms of frequency and percentage. The results were presented using tables and figures.
Results: Out of 62 cases of SDC, 48 (77.4%) were male and 14 (22.6%) were female. It was more prevalent in the age groups of 60– 69 and 70– 79. Most respondents had outdoor activity (91.9%). A total of 24.2% of patients were found to have Stage I; 35.5% were found to have Stage II; and 40.3% were in Stage III. Posterior subcapsular cataract (PSC) was found in 10 (16.1%) SDC cases, post-trachomatous corneal opacity (CO) in 10 (16.1%) SDC cases, and non-trachomatous CO in 8 (12.9%) SDC cases, but none of them had an association with SDC.
Conclusion: Between May 2021 and September 2022, sixty-two cases of SDC were found at the ASC in Menelik II Tertiary Referral Hospital. The data showed a preponderance of SDC in males and older subjects. Stage III and primary types are the leading presentations. It was observed predominantly in individuals who spent most of their time outdoors. Pterygium, corneal opacity, pseudoexfoliation (PXF), PSC, and glaucoma were noted; however, none of these had a significant association with SDC.
Keywords: corneal opacity, pseudoexfoliation, pterygium, outdoor, spheroidal degeneration of cornea, stage
Introduction
Spheroidal degeneration of cornea (SDC) is an acquired degeneration of the cornea or conjunctivae that is characterized by the deposition of translucent golden-yellow globules and amber-colored oily spherules in the superficial layers of the cornea. These spherules accumulate typically near the limbus in the early stages and progressing toward the center of the cornea in a band-shaped pattern. Histochemical stains confirm that the droplets contain protein. It has been postulated that the protein material may result from the actions of ultraviolet (UV) light on serum proteins that diffuse into the cornea from limbal vessels. There are more than ten synonyms for SDC. This diversity is related to the variation in the geographic distribution of this entity and the descriptions given by various authors under different names. It was first described by Bietti in 1955 in the southwest region of Saudi Arabia.1–6 For convenience, the term SDC was used in this study.
Fraunfelder et al categorized SDC into three forms: primary, secondary, and conjunctival types. The primary form is associated with aging in a normal eye, while the secondary form occurs in eyes with existing pathologies. The conjunctival type is marked by deposits on the conjunctiva with or without corneal involvement.7 SDC progresses through three stages based on tissue involvement: Stage 1 is peripheral, and vision is unaffected; Stage 2 involves the interpalpebral fissure, leading to visual reduction to 6/60; Stage 3 shows clusters of large golden droplets, severely impacting vision to the point of counting fingers or hand movements.8,9 Increasing age and exposure to UV light are the most common associated factors. Other proposed risk factors include dry eyes, malnutrition, corneal trauma or microtrauma, extremes of temperature, genetic factors, keratitis, lattice corneal dystrophy, and glaucoma. SDC presents symptoms such as intense foreign body sensations, pain, redness, photophobia, and deteriorating vision, significantly affecting patients’ quality of life.10–13
This study aims to assess the pattern of spheroidal degeneration of the cornea (SDC) and its association with other eye diseases among patients visiting Menelik II Tertiary Referral Hospital.
Methods and Materials
Study Area and Period
A hospital-based prospective descriptive study was conducted at the anterior segment clinic (ASC) in Menelik II Tertiary Referral Hospital, located in Addis Ababa, from May 2021 to September 2022. This hospital is the leading and pioneering ophthalmology teaching center in the country. It serves as a teaching, research, and patient care service.
Source Population
All consecutive patients with eye diseases in Menelik II tertiary referral hospital who visited the hospital during the study period.
Study Population
All patients with SDC who visited Menelik II tertiary referral hospital at the ASC during the study period.
Sample Size Determination and Sampling Technique
All patients who visited the hospital with a diagnosis of SDC during the study period were included.
Inclusion Criteria
All patients evaluated by authors with a diagnosis of SDC.
Data Collection Procedure
Primary data was collected using a standardized data collection tool that incorporated all relevant study variables. The measured variables included age, sex, indoor or outdoor job, visual acuity (VA), pseudoexfoliation (PXF), pterygium, arcus senile, cataract, stage, and type of SDC. All enrolled patients meeting the inclusion criteria were selected and assessed using a structured questionnaire. After taking demographic details and history, all patients underwent a complete ocular examination. All examinations were carried out by the authors. VA was measured using a standard tumbling-E Snellen chart, and intraocular pressure was measured with an I-Care tonometer before pupillary dilation. All subjects were examined with a Haag-Streit slit lamp biomicroscope (SLB) in a suitable room. The SLB is specifically an instrument used to examine both anterior and posterior segments of the eye.14–17
The diagnosis of SDC was established based on several key observations: the presence of amber granules in the superficial cornea at the periphery of the interpalpebral area, progressively increasing opacification with the granules coalescing and spreading towards the center, and the appearance of nodules accompanied by surrounding stromal haze. Additionally, SDC was divided into three stages and three types. Only one eye was taken into consideration for bilateral involvement. The figures presented refer only to eyes with SDC of lesser grade. This is done to avoid overestimation. During the same inspection, the presence of pterygium and other ocular surface diseases were confirmed.2,7,9
The pupils were dilated with one drop of tropicamide 0.8% and phenylephrine hydrochloride 5% to allow examination of PXF, cataract, and optic disc. Moreover, the pupils were fully dilated, and no subjects in this study exhibited miotic or undilated pupils. All subjects’ eyes were examined using a SLB before and after pupillary dilatation for signs of PXF in the anterior segment. PXF was diagnosed on SLB by the presence of white or gray flakes resembling dandruff on the pupil border or the characteristic light gray membrane of exfoliation material on the lens anterior capsule surface, often with curled anterior edges. Glaucoma was diagnosed on the basis of cupped disc, characteristic visual field defect (Humphrey field analyzer), and IOP above 21 mm Hg as well.2,9,16
Data Analysis
The data analysis was done using statistical software, statistical product and service solutions (SPSS), Version 26.0. Figures and tables were created using Microsoft Word and Excel. Descriptive analysis was used to describe the study variables by frequency and percentage. Statistical analyses were performed using chi-square tests for categorical variables, with P <0.05 taken as statistically significant. The results were presented using tables and figures.
Ethical Approval
Prior to the commencement of the study, ethical approval was obtained from the Research and Ethical Committee of the Ophthalmology Department at Addis Ababa University (Prof. Yilkal Adamu, Dr. Sadik Taju, and Dr. Tiliksew Teshome), under reference number OREC/007/21. Informed written consent was secured from all subjects, and the study was conducted in accordance with the principles outlined in the Declaration of Helsinki.
Result
Sociodemographic
From May 2021 to September 2022, a total of 24,068 patients were seen at ASC, in Menelik II tertiary referral hospital. Among those visitors, 62 cases of SDC were found. Based on this data, the magnitude of SDC was 0.258%, or one SDC per 388 cases. The sociodemographic details were categorized into age, sex, and out-door or in-door job. The age of the subjects was categorized into the ages of <39, 40–49, 50–59, 60–69, 70–79, and >80 years, with 11%, 9.7%, 12.9%, 27.4%, 29%, and 9.7% in each of the categories, respectively. SDC was more prevalent in males than females; forty-eight (77.4%) with SDC were males, and fourteen (22.6%) were females (Table 1).
 |
Table 1 Sociodemographic Characteristics in Cases of Spheroidal Degeneration of Cornea |
Outdoor and indoor activities
Regarding the number of hours spent indoor or outdoor, most respondents (91.9%) were involved in outdoor activities, while only 8.1% participated in indoor activities (Table 2).
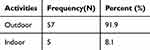 |
Table 2 Frequency of Outdoor or Indoor Activities of Spheroidal Degeneration of Cornea Cases |
Stage of SDC Cases
A total of 15 (24.2%) patients were found to have Stage I, 22 (35.5%) were found to have Stage II, and 25 (40.3%) were in Stage III. Out of 62, 31 (50%) are primary types, 26 (40.9%) are secondary, and 5 (8.1%) are conjunctival types (Table 3).
 |
Table 3 Stage of Spheroidal Degeneration of Cornea Cases |
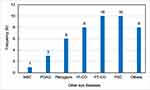
Other Eye Diseases
A frequency analysis had shown that PSC was found in 10 (16.1%) SDC cases, post-trachomatous CO in 10 (16.1%) SDC cases, non-trachomatous CO in 8 (12.9%) SDC cases, pterygium in 6 (9.7%) SDC cases, and primary open-angle glaucoma in 3 (4.8%) SDC cases. Sixteen (25.8%) cases of SDC had no other eye disease (Figure 1).
Discussion
In this study, a total of 62 SDC cases were found. The magnitude of SDC in this study was quite lower than the studies done by Amit Mohan (10.7%) and H Mohan Kumar (68.7%).2,4 This could be due to the short study period, and cases in their early stages might not visit a tertiary hospital.
Ethiopian researchers had not yet published any work on this study topic. However, Rodger visited the Dahlak Islands in the former province of Ethiopia, Eritrea, in 1973 and showed that SDC accounted for 57% of all cases of blindness there.15 Similarly, a recent study done in the Islands of the Northern Red Sea Zone, Eritrea, showed that the prevalence of SDC was 19.6%.18 Another countrywide survey in the Republic of Djibouti found the overall prevalence for both sexes of all ages to be 2.8% for the rural population and 0.5% for urban dwellers.14 A study done by Johnson showed SCD was the third most common cause of blindness in Somalia, after cataract and glaucoma.16 Taylor et al studied 838 male watermen over the age of 30 from Chesapeake Bay in Maryland (USA) and found the prevalence of SCD was 19%. Comparably, Garner et al found a prevalence of 6% in England.1
In our study, the prevalence of the condition was higher in the age groups of 60–69 and 70–79, while it was notably lower in individuals aged above 80 years. This finding contrasts with a study conducted in Jizan, Saudi Arabia, where the highest prevalence was observed in the younger age groups of 21–31 and 32–41 years. Consistent with our findings, a study conducted among Greenlandic and Caucasian populations in Copenhagen reported an increase in prevalence with age, with higher rates observed in men compared to women. This trend is also noted despite the differences seen in studies from the Dahlak Islands and South West Africa.14,15 The higher prevalence among older adults and men can be attributed to prolonged and more frequent exposure to risk factors, particularly for those who spend a significant amount of time outdoors.9
The prevalence in males was higher than in females in most age groups. The greatest difference was seen in the age groups of 60–69 years and 70–79 years. The primary type is more prevalent in older age groups. Generally, all types of SDC were more prevalent in males and older age groups (Table 4 and Figure 2). Johnson discovered that among Labrador residents over 40 years old, the frequency was generally 60.1% for men and 13.5% for women.1
 |
Table 4 Distribution Types of Spheroidal Degeneration of Cornea Cases by Age Categories |
 |
Figure 2 Distribution of types of spheroidal degeneration of cornea cases by sex. Legends in the figure (color). Blue = Female. Red = Male. Green = Total. |
Nearly 92% of the study participants had outdoor activities for more than 8 hours a day, which is in agreement with a study done by Ahmed Alibrahim, where 78% of cases of SDC had outdoor work. It has been claimed that outdoor workers, such as fishermen, are highly susceptible to UV radiation exposure.17
Around 40.3% of the total of 62 cases examined were found to have Stage III, followed by Stage II (35.5%) and Stage I (24.2%). In the study done by Amit Mohan, 55% were stage I, stage II (32%), and stage III (13%).2 H Mohan Kumar showed in his study that 43.75% of patients had stage 1, 10.93% had stage 2, 7.81% had stage 3, and 6.25% had stage 4 SDC.4
In this study, PSC was observed in 10 cases, pterygium in 6 cases, and post-inflammatory conditions, including trachomatous CO, in 18 cases. No statistically significant associations were found between the observed other eye disease and the stage or type of SDC. In contrast, Resnikoff et al reported a link between SDC and conditions such as cataract, PXF, and pterygium, noting that UV irradiation plays a significant role in all these conditions.1
Limitation of the Study
- Short study period.
- Hospital-based rather than cross-sectional community study.
- Mild cases and those with no visually significant complaints might not visit a tertiary hospital. So, they might be missed.
Conclusion
Our study highlights key demographic pattern, potential risk factors, and other eye disease co-presented with SDC, offering valuable insights as the first investigation of its kind in Ethiopia. We recommend conducting further community-based studies with larger sample sizes to better understand the public health significance of SDC and to guide potential preventive measures within the Ethiopia context.
Abbreviations
ASC, Anterior Segment Clinic; CO, Corneal Opacity; PSC, Posterior Subcapsular Cataract; PXF, Pseudoexfoliation; SDC, Spheroidal Degeneration of Cornea; SLB, Slit Lamp Biomicroscope; SPSS, statistical product and service solutions; UV, ultraviolet.
Acknowledgments
We are grateful to Prof. Abebe Bejiga and Dr. Alemayehu Weldeyesus for their valuable input on this research. We also thank all participants for their valuable voluntarism in taking part in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study did not receive any external funding. The department has issued a claim letter for the APC (Article Processing Charge) waiver, referenced as MF/OPH/243/24.
Disclosure
The authors report no other conflicts of interest in this work.
References
1. Gray RH, Johnson GJ, Freedman A. Climatic droplet keratopathy. Surv Ophthal. 1992;36(4):241–253. doi:10.1016/0039-6257(92)90093-9
2. Mohan A, Jamil Z, Bhatanagar VC, Gajraj M. Prevalence of spheroidal degeneration of cornea and its association with other eye diseases in tribes of Western Rajasthan. Ind j ophthal. 2017;65(10):1010–1014. doi:10.4103/ijo.IJO_84_17
3. Elhusseiny AM, El Sheikh RH, Jamerson EC, et al. Advanced spheroidal degeneration. Digital J Ophthal. 2019;25(4):68–71. doi:10.5693/djo.02.2019.11.001
4. Kumar HM, Madhumita M. Association of spheroidal degeneration in pseudoexfoliation cases. Indian J Clin Exp Ophth. 2019;5(2):186–189. doi:10.18231/j.ijceo.2019.044
5. Johnson GJ, Overall MA. Histology of spheroidal degeneration of the cornea in Labrador. Br J Ophthalmol. 1978;62(1):53–61. doi:10.1136/bjo.62.1.53
6. Garner A, Fraunfelder FT, Barras TC, Hinzpeter EN. Spheroidal degeneration of cornea and conjunctiva. Br J Ophthalmol. 1976;60(6):473–478. doi:10.1136/bjo.60.6.473
7. Fraunfelder FT, Hanna C, Parker JM. Spheroid degeneration of the cornea and conjunctiva: 1. Clinical course and characteristics. Am J Ophthalmol. 1972;74(5):821–823. doi:10.1016/0002-9394(72)91202-0
8. Serra HM, Holopainen JM, Beuerman R, Kaarniranta K, Suárez MF, Urrets‐Zavalía JA. Climatic droplet keratopathy: an old disease in new clothes. Acta Ophthalmologica. 2015;93(6):496–504. doi:10.1111/aos.12628
9. Bartholomew RS. Spheroidal degeneration of the cornea. Prevalence and association with other eye diseases. Doc Ophthalmol. 1977;43(2):325–340. doi:10.1007/BF01569202
10. Sood T, Sharma RL, Mandeep T, Sood S, Sharma A. Climatic Keratopathy in Snow Laden Hilly Areas. Int J Ophthalmol Eye Res. 2016;4(5):212–214.
11. Johnson GJ. Aetiology of spheroidal degeneration of the cornea in Labrador. Br J Ophthalmol. 1981;65(4):270–283. doi:10.1136/bjo.65.4.270
12. Santo RM, Yamaguchi T, Kanai A. Spheroidal keratopathy associated with subepithelial corneal amyloidosis: a clinicopathologic case report and a proposed new classification for spheroidal keratopathy. Ophthalmology. 1993;100(10):1455–1461. doi:10.1016/S0161-6420(93)31456-9
13. Viswamithra P, Murthy SR. Spheroidal degeneration–An epidemiological study. J Dent Med Sci. 2014;8:48–53.
14. NORN M. Spheroid degeneration, keratopathy, pinguecula, and pterygium in Japan. Acta ophthalmologica. 1984;62(1):54–60. doi:10.1111/j.1755-3768.1984.tb06756.x
15. Anderson J, Fuglsang H. Droplet degeneration of the cornea in North Cameroon. Prevalence and clinical appearances. Br J Ophthalmol. 1976;60(4):256–262. doi:10.1136/bjo.60.4.256
16. Johnson G, Minassian D, Franken S. Alterations of the anterior lens capsule associated with climatic keratopathy. Br J Ophthalmol. 1989;73(3):229–234. doi:10.1136/bjo.73.3.229
17. Alibrahim A, Tamrin M, Bahri S, et al. Prevalence of cataract, climatic droplet keratopathy and eyelid diseases among fishermen in Jazan in Saudi Arabia, and the association of risk factors. Malaysian. J Hum Fact Ergon J. 2017;1(2):58–63.
18. Tesfai B, Kebede S, Kibreab F, Fessehatsion K, Asmelash S, Guelay Y. Prevalence of Solar Keratopathy, Pterygium and Cataract in the Islands of Northern Red Sea Zone, Eritrea: cross-Sectional Study. Clin Ophthalmol. 2021;15:2983–2991. doi:10.2147/OPTH.S321413
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.