Back to Journals » International Journal of General Medicine » Volume 18
Prediction of First-Onset Cerebral Infarction Risk in Patients with Acute Myocardial Infarction: A Retrospective Cohort Study
Authors Zeng Z, Luo R, Xu W, Yao H, Lan X
Received 2 March 2025
Accepted for publication 18 June 2025
Published 27 June 2025 Volume 2025:18 Pages 3501—3513
DOI https://doi.org/10.2147/IJGM.S523100
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Yuriy Sirenko
Zifeng Zeng,1,2 Rongtai Luo,1,2 Weiyong Xu,1,2 Huaqing Yao,1,2 Xinping Lan1,2
1Center for Cardiovascular Diseases, Meizhou People’s Hospital, Meizhou, People’s Republic of China; 2Guangdong Provincial Engineering and Technology Research Center for Molecular Diagnostics of Cardiovascular Diseases, Meizhou People’s Hospital, Meizhou, People’s Republic of China
Correspondence: Xinping Lan, Center for Cardiovascular Diseases, Meizhou People’s Hospital, Meizhou Academy of Medical Sciences, Meizhou, People’s Republic of China, Email [email protected]
Background: The occurrence of cerebral infarction significantly increases the risk of major adverse cardiovascular events in patients with acute myocardial infarction (AMI), highlighting the importance of early identification and intervention. Currently, no validated tools exist for individualized risk stratification of cerebral infarction (CI) in patients with AMI.
Objective: This study aimed to identify the most valuable predictors (MVPs) of in-hospital first-onset CI in AMI patients and construct a nomogram for risk stratification.
Methods: This retrospective cohort study enrolled 1,350 AMI patients admitted to the Cardiovascular Center of Meizhou People’s Hospital between January and December 2022. Clinical characteristics and laboratory parameters were analyzed. Least Absolute Shrinkage and Selection Operator regression (LASSO) was used to select MVPs. The nomogram was developed by integrating coefficients of MVPs from logistic regression, and its discrimination, calibration, and clinical utility were validated in the cohort. The optimal cutoff value of the nomogram probability was determined.
Results: CI occurred in 60 patients (4.44%). MVPs included Killip classification (OR = 1.42, 95% CI 1.05– 1.93), PCI therapy (OR = 0.29, 95% CI 0.16– 0.51), C-reactive protein (CRP: OR = 1.01, 95% CI 1.00– 1.01), blood urea nitrogen (BUN: OR = 1.03, 95% CI 0.99– 1.07), and neutrophil-to-lymphocyte ratio (NLR: OR = 1.02, 95% CI 0.99– 1.05). The discriminatory ability of the nomogram was up to 0.804( 95% CI 0.749– 0.859). Additionally, the nomogram showed good calibration and clinical utility in the cohort. Furthermore, the optimal cutoff value of the nomogram probability for distinguishing those who will experience in-hospital first-onset CI was 0.035 (sensitivity 78.3%, specificity 71.1%).
Conclusion: The first nomogram integrating multimodal predictors for discerning AMI patients who will experience in-hospital first-onset CI was developed and validated, which will aid clinicians in clinical decision-making.
Keywords: acute myocardial infarction, cerebral infarction, nomogram, model, first-onset
Introduction
Acute Myocardial Infarction (AMI), the most catastrophic manifestation of coronary artery disease, typically results from acute plaque rupture or sustained coronary occlusion.1 Despite advances in reperfusion therapies2,3 such as the establishment of chest pain centers in China, which have significantly streamlined AMI care pathways,4 emerging data from the 2023 China Cardiovascular Health and Disease Report indicate a growing epidemiological burden, with national incidence reaching 79.7 per 100,000 person-years and mortality rates maintaining an ascending trend.5 Globally, AMI continues to dominate as the principal cause of mortality and disability-adjusted life years worldwide.6
Cerebral infarction (CI), the second-leading global cause of mortality and third-leading contributor to disability,7 constitutes a devastating yet underappreciated complication in AMI management. The novel clinical entity of cardio-cerebral infarction (CCI), defined by the co-occurrence of AMI and CI within 48 hours,8 presents unique therapeutic challenges. Although its incidence remains modest (3.2–4.7% of AMI admissions),9 meta-analyses reveal catastrophic outcomes: 2.3-fold elevated in-hospital mortality (95% CI 1.8–3.0) and 4.1-fold increased risk of major adverse cardiovascular events compared to isolated AMI.10,11 Furthermore, survivors face substantially reduced functional capacity and quality of life.12–14 These findings highlight the urgent need for early identification of AMI patients at high CI risk to implement preventive strategies.
Current research has identified several CI-associated risk factors in AMI populations, including cardiac dysfunction and systemic inflammation.15,16 However, existing risk stratification paradigms remain fragmented, relying predominantly on isolated biomarkers rather than integrative prognostic modeling. Notably, no validated predictive tools currently enable individualized CI risk stratification in AMI patients. To address this gap, we aimed to construct a predict nomogram to discern who will experience in-hospital first-onset CI to help clinical decision-making.
Methods
Study Population
Data from patients diagnosed with AMI at the Cardiovascular Center of Meizhou People’s Hospital (Meizhou, China) between January and December 2022 were retrospectively collected. The diagnosis was confirmed according to the Fourth Universal Definition of Myocardial Infarction.17
The inclusion criteria were:(1) primary diagnosis of AMI; (2) complete baseline clinical documentation. The exclusion criteria were (1) pre-existing cerebrovascular diseases, such as prior cerebral infarction or intracranial hemorrhage; (2) active malignancy or terminal illness; (3) missing critical admission data (>20% of variables incomplete). This study was performed in accordance with the ethical standards of the Declaration of Helsinki and approved by the Human Ethics Committee of Meizhou People’s Hospital.
Data Collection
Demographic and Clinical Variables
We collected potential predictive factors from all patients, including age, sex, BMI, underlying diseases, clinical presentation, therapeutic intervention, left ventricular ejection fraction by echocardiography, and AMI subtype classification (ST-segment/non-ST-segment Elevation Myocardial Infarction). Standardized laboratory tests performed within 24 hours of admission, which included hematology, biochemistry, cardiac biomarkers, and inflammatory markers were collected. Derived indices, calculated as follows: Triglyceride-Glucose (TyG) index = ln [fasting triglycerides (mg/dL) × glucose (mg/dL)/2]; Neutrophil-to-lymphocyte ratio (NLR) = absolute neutrophils/absolute lymphocytes; Platelet-to-lymphocyte ratio (PLR) = platelet count/absolute lymphocytes, were collected.
Outcome Definition
The World Health Organization (WHO) has established a standardized coding and classification framework for CI in the International Classification of Diseases, 10th Revision (ICD-10).18 According to the WHO definition, the diagnosis of CI requires the integration of clinical manifestations, imaging examinations, and other auxiliary tests, while excluding other potential etiologies. In this study, we applied the WHO diagnostic principles for CI and the ICD-10 coding system to confirm cases of CI.
Statistical Analysis
The normal distribution of the continuous variables was assessed using the Kolmogorov–Smirnov test. Variables that followed a normal distribution were expressed as mean ± standard deviation (SD) and compared using the independent samples t-test. Variables that did not follow a normal distribution were expressed as median (interquartile range) and compared using the Mann–Whitney U-test. Categorical variables were expressed as frequency (percentage). Between-group comparisons for categorical data were performed using the chi-square (χ2) test.
The Least Absolute Shrinkage and Selection Operator (LASSO) regression analysis with 10-fold cross-validation was employed to reduce data dimensionality and identify the most valuable predictors (MVPs).19 The nomogram was developed by integrating all MVPs based on their regression coefficients in the binary logistic regression model. Subsequently, the calibration of the nomogram was evaluated using the calibration curve, accompanied by the Hosmer–Lemeshow test. The discrimination ability of the nomogram was assessed using the area under the receiver operating characteristic curve (AUC) and concordance index (C-index). Decision curve analysis (DCA) was performed to assess the net benefit of the nomogram for clinical decisions-making.20 The optimal risk cutoff was determined by maximizing Youden’s index (sensitivity + specificity − 1).
A two-tailed P-value less than 0.05 was considered significant. The Statistical Package for R 4.3.3 software (R Foundation for Statistical Computing) was used for the complete statistical analyses.
Results
Baseline Characteristics
The study cohort consisted of 1,350 AMI patients, including 60 cases (4.44%) who developed first-onset CI during hospitalization (CI group) and 1,290 controls (non-CI group). The overall population showed a male predominance (76%, n = 1,031) with a median age of 68 years (interquartile range [IQR] 59–76). The demographic and clinical characteristics of the two cohorts are summarized in Table 1.
 |
Table 1 General characteristics |
Identification of Optimal Predictive Factors for First-Onset CI
Using LASSO regression with 10-fold cross-validation, the optimal hyperparameter λ was identified based on the minimum binomial deviance. Based on the optimal λ, five non-zero coefficients of preoperative features were selected as MVPs, including Killip classification, PCI therapy, C-reactive protein (CRP), blood urea nitrogen (BUN), and NLR (Figure 1).
The odds ratios (95% CI) of the five MVPs were 1.4238(1.0513–1.9319), 0.2894(0.1638–0.5099), 1.0063(1.0021–1.0103), 1.0317(0.9941–1.0671), and 1.0219 (0.99–1.0525), as shown in Table 2. The list of candidate variables and their standardized coefficients were documented in Table 3.
 |
Table 2 Details of Logistic Regression Analysis based on LASSO Screening Variables |
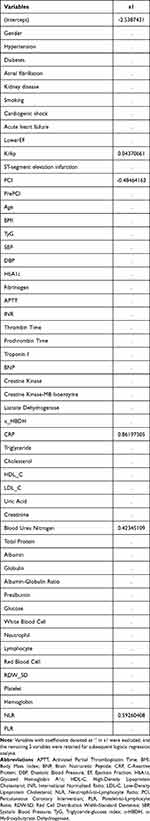 |
Table 3 Variables Selected by LASSO Regression with Coefficient |
Development of the Nomogram
Based on the coefficients of the five predictors, the nomogram was constructed using the “rms” package in R software (Figure 2).
 |
Figure 2 Nomogram for predicting the risk of first-onset CI in patients with AMI. |
To predict the risk of in-hospital first-onset CI in AMI patients using the nomogram, the total score is calculated by summing the individual scores of the five predictors. The risk of CI is then determined by projecting a vertical line downward from the total score.
Multiple Validations of the Nomogram
In the internal validation, the nomogram demonstrated a high accuracy in predicting CI in AMI patients, with an AUC of 0.804 (95% CI: 0.749–0.859; Figure 3A). Using the bootstrap internal resampling method, the C-index was 0.7917 (95% CI: 0.7134–0.870). The C-index obtained through ten-fold cross-validation was 0.7959. The Hosmer–Lemeshow test result (χ² = 4.6377, P = 0.7955) and a close-to-ideal calibration curve indicated good calibration of the nomogram (Figure 3B). DCA demonstrated clinically meaningful net benefits across a threshold probability range of 10% to 80%, suggesting robust utility of the nomogram for risk-stratification in real-world practice (Figure 3C).
Determination of the Optimal Cutoff Value for the Nomogram
Based on data from all 1,350 patients enrolled in this study, as per the rule of the most balance between sensitivity and specificity, the optimal cutoff value of the nomogram was identified as 0.035 (sensitivity 0.783 and specificity 0.711). In other words, under the conditions of this study, patients with a nomogram probability of ≥0.035 were classified as high-risk patients with CI and should receive focused attention and targeted interventions, such as timely PCI treatment, to effectively prevent disease progression and improve patient outcomes.
Discussion
This study developed the first predictive tool to identify patients with AMI at risk of CI. The primary advantage of our model is its ability to enable physicians in resource-limited settings to predict the risk of in-hospital first-onset CI in AMI patients using physical examinations and readily available laboratory indices. Based on the nomogram results, we established an optimal cutoff value to assist clinicians in determining additional treatment strategies.
The co-occurrence of AMI and CI represents a critical clinical scenario with profound implications for patient outcomes. The reported incidence rates of this complication vary widely across studies, ranging from 0.4% to 12.7%. This variation may be attributed to differences in study populations, diagnostic criteria, and methodological approaches. Notably, Chin et al reported the highest incidence at 12.7% in their comprehensive analysis,21 while the GRACE trial reported a more conservative figure of 0.9% for in-hospital stroke among acute coronary syndrome patients.12 Intermediate values were reported by Kajermo et al (2.1% within 30 days post-AMI)16 and Hachet et al (1.25% during hospitalization).22 In our study of 1,350 AMI patients, we identified 60 cases of concurrent CI during hospitalization, resulting in an incidence rate of 4.44%. This higher incidence may be attributed to our stringent inclusion criteria, which excluded patients with prior CI, cerebral hemorrhage, or malignant tumors to minimize confounding factors and improve study rigor. As a result, our study population was more homogeneous, which may have contributed to the higher observed incidence rate.
Previous studies have identified various risk factors for CI in AMI patients, with a predominant focus on non-laboratory indicators. Hachet et al identified female sex, history of transient ischemic attack or stroke, new-onset atrial fibrillation, left ventricular ejection fraction, and CRP as independent predictors.22 Mohammed et al identified hypertension as the most prevalent risk factor, followed by diabetes and atrial fibrillation.11 Hurskainen et al emphasized the significance of paroxysmal atrial fibrillation/flutter, stroke history, left main coronary artery occlusion, coronary artery disease severity, and high Killip classification.23 Our findings are consistent with these studies, showing significant differences in diabetes mellitus, atrial fibrillation, cardiogenic shock, acute heart failure, Killip classification, and reduced ejection fraction between patients with and without concurrent CI.
In addition to these established factors, our study identified several laboratory indices with statistically significant differences, including B-type natriuretic peptide (BNP), cardiac enzymes, uric acid, creatinine, BUN, total protein, albumin, prealbumin, fasting glucose, complete blood count parameters, TyG index, NLR, and PLR. Although these indices have been individually linked to AMI or CI, their combined analysis in our study provides a more comprehensive risk assessment. The inclusion of these laboratory parameters represents a significant advancement in risk stratification, as they offer objective and measurable indicators that are easily accessible in clinical practice.
Using LASSO regression analysis, we identified five optimal predictors for AMI-associated CI: Killip classification, PCI treatment, CRP, BUN, and NLR. These predictors were integrated into a nomogram, which demonstrated excellent predictive performance.
The association between higher Killip classification (III–IV) and increased stroke risk has been well-documented,23,24 likely due to severe myocardial damage causing systemic circulation disturbances and cerebral hypoperfusion. Our findings that PCI treatment as a protective factor highlights the importance of timely coronary reperfusion in stroke prevention. Early revascularization has been demonstrated to reduce stroke risk in AMI patients,25 potentially by improving myocardial function, reducing arrhythmias, and stabilizing of cerebral hemodynamics.The inclusion of CRP in our model is supported by its established role as a biomarker for stroke risk26,27 and its identification as an independent predictor of in-hospital CI in AMI patients.22
Elevated BUN levels have been consistently linked to an increased risk of stroke and ischemic stroke.28 Moreover, elevated BUN levels have been associated with to correlate with poor prognosis in CI.29 The underlying mechanism may involve the disruption of glucose homeostasis,30 which can subsequently lead to the development of diabetes,31 thereby increasing the risk of CI. In addition, BUN levels are influenced by various factors, including protein intake, corticosteroid use, gastrointestinal bleeding, and dehydration,32 all of which reflect the body’s metabolic status. Notably, conditions such as dehydration or impaired renal function are also associated with an increased risk of stroke.33 In our study, BUN levels were significantly higher in patients with CI compared to those without, consistent with previous findings. This consistency supports the validity of including BUN as a predictive factor in our model.
Emerging clinical studies have consistently identified elevated NLR levels in acute ischemic stroke patients compared to healthy controls.34–37 This hematological phenomenon is mechanistically rooted in the robust inflammatory cascade triggered by CI.38 Within hours post-infarction, ischemic brain tissue releases chemokines that recruit peripheral neutrophils to the lesion site, followed by lymphocyte infiltration.39 Neutrophils dominate early pro-inflammatory responses through reactive oxygen species production and protease release,40 while lymphocytes exert delayed immunoregulatory effects.41 The clinical elevation of NLR precisely mirrors the temporal dynamics of post-infarction inflammation, characterized by an acute neutrophilic surge peaking at 1–3 days42 followed by progressive lymphopenia stemming from glucocorticoid-induced apoptotic depletion.43 Beyond its predictive value for infarction risk44,45 and clinical prognosis,37,46,47 NLR quantifies neuroinflammation-mediated secondary injury intensity, demonstrating superior sensitivity to traditional biomarkers in CT-negative minor stroke cases.48 This ratio thus provides a clinically actionable, pathophysiologically grounded monitoring window for early detection and risk stratification in ischemic cerebrovascular events. In the present study, NLR was significantly higher in the concurrent CI group and identified as a significant predictor of in-hospital first-onset CI, corroborating previous findings and reinforcing the rationale for its inclusion in the predictive model.
Extensive evidence underscores the prognostic significance of carotid plaque characteristics in cardiovascular risk stratification. Jérôme Fichet et al demonstrated 52% of acute coronary syndrome patients exhibit concurrent carotid atherosclerosis,49 with ultrasound-derived plaque hardness independently predicting adverse outcomes at 19-month follow-up reported by R Komorovsky.50 Systematic reviews further highlight that biomechanical stress parameters, including wall shear stress and plaque wall stress, demonstrate moderate-to-high sensitivity in forecasting plaque-related cerebrovascular events.51 Longitudinal studies corroborate the superiority of plaque characteristics—such as Total Plaque Risk Score (12-month prognosis52) and carotid intima-media thickness (6.4-year stroke risk53)—in long-term risk prediction. While these plaque-centric biomarkers provide invaluable insights into chronic atherosclerotic progression, their temporal resolution aligns poorly with acute-phase clinical decision-making. Our study strategically focuses on identifying imminent in-hospital CI during AMI management, a critical window where traditional plaque metrics exhibit limited discriminative capacity. Our biomarker panel (CRP, NLR, Killip classification, BUN) detects imminent in-hospital events through distinct pathophysiological pathways - particularly systemic inflammation (CRP/NLR) and acute hemodynamic stress (Killip/BUN). This acute-temporal specificity positions our panel not as a replacement for plaque-based prognostication, but as its necessary counterpart—enabling precision monitoring when anatomical biomarkers lose clinical immediacy.
Limitations
Although this study provides valuable insights into the prediction of CI in AMI patients, several limitations must be acknowledged. First, the study design was a single-center retrospective analysis, which may introduce selection bias and information bias due to the inherent limitations of retrospective data collection. The relatively small sample size further limits the generalizability of our findings. Second, the prediction model was developed and validated using data from a single center, which may limit its external validity. Future multicenter studies with larger, more diverse populations are needed to confirm the predictive efficacy of the model and to develop a more accurate and generalizable tool for clinical application in China. Additionally, the inclusion of only in-hospital CI events may underestimate the true incidence of this complication, as some cases may occur after discharge. Further research should also investigate the potential impact of unmeasured confounders, such as medication adherence and lifestyle factors, on the model’s performance.
Conclusion
This study successfully developed and internally validated the first prediction model for the first onset of CI during hospitalization in AMI patients, using five routinely available clinical indicators: Killip classification, PCI treatment, CRP, BUN, and NLR. The model demonstrated robust predictive performance, with an optimal cutoff value of 0.035 determined by ROC curve analysis (sensitivity: 0.783, specificity: 0.711), providing clinicians with a clear intervention threshold. By integrating key domains of cardiac function assessment (Killip classification), hemodynamic intervention (PCI treatment), inflammatory markers (CRP and NLR), and metabolic status (BUN), the model enables accurate quantification of individualized risk probabilities. This facilitates early identification and stratified management of high-risk populations, providing an evidence-based foundation for prophylactic antithrombotic therapy and multidisciplinary care. Future research should focus on external validation through multicenter prospective cohort studies and further optimization using advanced machine learning algorithms to improve dynamic prediction capabilities. Such efforts will facilitate the integration of this model into clinical decision support systems, ultimately improving patient outcomes in this high-risk population.
Data Sharing Statement
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
This retrospective study was approved by the Institutional Review Board of the Ethics Committee of Medicine, Meizhou People’s Hospital (Approval Number: 2022-C-94). Given the retrospective nature of the study and the use of de-identified patient data, the requirement for informed consent was waived by the Institutional Review Board. The study was conducted in accordance with the ethical standards of the Declaration of Helsinki and its subsequent amendments.
Acknowledgments
The authors would like to thank other colleagues who were not listed in the authorship of Center for Cardiovascular Diseases, Meizhou People’s Hospital, for their valuable comments on the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, including conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the manuscript; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Social Development Science and Technology Program of Meizhou (Grant No. 2022C0301146).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Anderson HVS, Masri SC, Abdallah MS, et al. acc/aha key data elements and definitions for chest pain and acute myocardial infarction: a report of the American heart association/American college of cardiology joint committee on clinical data standards. Circul Cardiovasc Quality Outcomes. 2022;15(10). doi:10.1161/HCQ.0000000000000112
2. Byrne RA, Rossello X, Coughlan JJ, et al. 2023 esc guidelines for the management of acute coronary syndromes. Eur Heart J Acute Cardiovasc Care. 2024;13(1):55–161. doi:10.1093/ehjacc/zuad107
3. Ozaki Y, Tobe A, Onuma Y, et al. Cvit expert consensus document on primary percutaneous coronary intervention (pci) for acute coronary syndromes (acs) in 2024. Cardiovasc Interv Ther. 2024;39(4):335–375. doi:10.1007/s12928-024-01036-y
4. Fan F, Li Y, Zhang Y, et al. Chest pain center accreditation is associated with improved in-hospital outcomes of acute myocardial infarction patients in China: findings from the ccc-acs project. J Am Heart Assoc. 2019;8(21):e013384. doi:10.1161/JAHA.119.013384
5. Improvement NCFC. Executive summary of the 2023 national report on the medical care quality of cardiovascular disease in China. Chin Circul J. 2024;39:625–660. doi:10.3969/j.issn.1000-3614.2024.07.001
6. Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics-2020 update: a report from the American heart association. Circulation. 2020;141(9):e139–e596. doi:10.1161/CIR.0000000000000757
7. Feigin VL, Stark BA, Johnson CO. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 2021;20(10):795–820. doi:10.1016/S1474-4422(21)00252-0
8. Omar HR, Fathy A, Rashad R, Helal E. Concomitant acute right ventricular infarction and ischemic cerebrovascular stroke; Possible explanations. Int Arch Med. 2010;3(1):25. doi:10.1186/1755-7682-3-25
9. Maciejewski D, Nowak K, Wawak M, et al. Rare instances of concomitant acute myocardial infarction and stroke. Bratisl Lek Listy. 2024;125(5):289–298. doi:10.4149/BLL_2024_43
10. Brammas A, Jakobsson S, Ulvenstam A, Mooe T. Mortality after ischemic stroke in patients with acute myocardial infarction: predictors and trends over time in Sweden. Stroke. 2013;44(11):3050–3055. doi:10.1161/STROKEAHA.113.001434
11. Mohammed H, Somaya E. Outcomes of intervention treatment for concurrent cardio-cerebral infarction: a case series and meta-analysis. J Cardiol Cardiovasc Med. 2023;8(1):4–11. doi:10.29328/journal.jccm.1001147
12. Budaj A, Flasinska K, Gore JM, et al. Magnitude of and risk factors for in-hospital and postdischarge stroke in patients with acute coronary syndromes. Circulation. 2005;111(24):3242–3247. doi:10.1161/CIRCULATIONAHA.104.512806
13. Alqahtani F, Aljohani S, Tarabishy A, Busu T, Adcock A, Alkhouli M. Incidence and outcomes of myocardial infarction in patients admitted with acute ischemic stroke. Stroke. 2017;48(11):2931–2938. doi:10.1161/STROKEAHA.117.018408
14. Desai R, Mondal A, Prasad A, et al. Concurrent cardio-cerebral infarctions in covid-19: a systematic review of published case reports/series. Curr Probl Cardiol. 2023;48(10):101814. doi:10.1016/j.cpcardiol.2023.101814
15. Nakaoka T, Sada T, Kira Y, et al. Risk factors for the complication of cerebral infarction in Japanese patients with acute myocardial infarction. Jpn Heart J. 1989;30(5):635–643. doi:10.1536/ihj.30.635
16. Kajermo U, Ulvenstam A, Modica A, Jernberg T, Mooe T. Incidence, trends, and predictors of ischemic stroke 30 days after an acute myocardial infarction. Stroke. 2014;45(5):1324–1330. doi:10.1161/STROKEAHA.113.001963
17. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40(3):237–269. doi:10.1093/eurheartj/ehy462
18. Bramer GR. International statistical classification of diseases and related health problems. Tenth revision. World Health Stat Q. 1988;41(1):32–36.
19. Friedman J, Hastie T, Tibshirani R. Regularization paths for generalized linear models via coordinate descent. J Stat Softw. 2010;33(1):1–22. doi:10.18637/jss.v033.i01
20. Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making. 2006;26(6):565–574. doi:10.1177/0272989X06295361
21. Chin PL, Kaminski J, Rout M. Myocardial infarction coincident with cerebrovascular accidents in the elderly. Age Ageing. 1977;6(1):29–37. doi:10.1093/ageing/6.1.29
22. Hachet O, Guenancia C, Stamboul K, et al. Frequency and predictors of stroke after acute myocardial infarction: specific aspects of in-hospital and postdischarge events. Stroke. 2014;45(12):3514–3520. doi:10.1161/STROKEAHA.114.006707
23. Hurskainen M, Tynkkynen J, Eskola M, Lehtimaki T, Hernesniemi J. Risk factors for ischemic stroke after acute coronary syndrome. J Am Heart Assoc. 2023;
24. Szummer KE, Solomon SD, Velazquez EJ, et al. Heart failure on admission and the risk of stroke following acute myocardial infarction: the valiant registry. Eur Heart J. 2005;26(20):2114–2119. doi:10.1093/eurheartj/ehi352
25. Van de Graaff E, Dutta M, Das P, et al. Early coronary revascularization diminishes the risk of ischemic stroke with acute myocardial infarction. Stroke. 2006;37(10):2546–2551. doi:10.1161/01.STR.0000240495.99425.0f
26. Xin F, Fu L, Liu H, Xu Y, Wei T, Chen M. Exploring metabolic and inflammatory abnormalities in rheumatoid arthritis patients developing stroke disease: a case-control study using electronic medical record data in northern China. Clin Rheumatol. 2019;38(5):1401–1411. doi:10.1007/s10067-019-04440-5
27. Hasan N, Mccolgan P, Bentley P, Edwards RJ, Sharma P. Towards the identification of blood biomarkers for acute stroke in humans: a comprehensive systematic review. Br J Clin Pharmacol. 2012;74(2):230–240. doi:10.1111/j.1365-2125.2012.04212.x
28. Peng R, Liu K, Li W, et al. Blood urea nitrogen, blood urea nitrogen to creatinine ratio and incident stroke: the dongfeng-Tongji cohort. Atherosclerosis. 2021;333:1–8. doi:10.1016/j.atherosclerosis.2021.08.011
29. Zhou P, Liu RL, Wang FX, Hu HF, Deng Z. Blood urea nitrogen has a nonlinear association with 3-month outcomes with acute ischemic stroke: a second analysis based on a prospective cohort study. Clin Nutr ESPEN. 2024;59:140–148. doi:10.1016/j.clnesp.2023.12.001
30. Koppe L, Nyam E, Vivot K, et al. Urea impairs beta cell glycolysis and insulin secretion in chronic kidney disease. J Clin Invest. 2016;126(9):3598–3612. doi:10.1172/JCI86181
31. Xie Y, Bowe B, Li T, Xian H, Yan Y, Al-Aly Z. Higher blood urea nitrogen is associated with increased risk of incident diabetes mellitus. Kidney Int. 2018;93(3):741–752. doi:10.1016/j.kint.2017.08.033
32. Dossetor JB. Creatininemia versus uremia. The relative significance of blood urea nitrogen and serum creatinine concentrations in azotemia. Ann Intern Med. 1966;65(6):1287–1299. doi:10.7326/0003-4819-65-6-1287
33. Coull BM, Beamer N, de Garmo P, et al. Chronic blood hyperviscosity in subjects with acute stroke, transient ischemic attack, and risk factors for stroke. Stroke. 1991;22(2):162–168. doi:10.1161/01.str.22.2.162
34. Akil E, Akil MA, Varol S, et al. Echocardiographic epicardial fat thickness and neutrophil to lymphocyte ratio are novel inflammatory predictors of cerebral ischemic stroke. J Stroke Cerebrovasc Dis. 2014;23(9):2328–2334. doi:10.1016/j.jstrokecerebrovasdis.2014.04.028
35. Celikbilek A, Ismailogullari S, Zararsiz G. Neutrophil to lymphocyte ratio predicts poor prognosis in ischemic cerebrovascular disease. J Clin Lab Anal. 2014;28(1):27–31. doi:10.1002/jcla.21639
36. Farah R, Samra N. Mean platelets volume and neutrophil to lymphocyte ratio as predictors of stroke. J Clin Lab Anal. 2018;32(1). doi:10.1002/jcla.22189
37. Qian K, Hu J, Wang C, et al. Dynamic change of neutrophil-to-lymphocyte ratio and its predictive value of prognosis in acute ischemic stroke. Brain Behav. 2024;14(7):e3616. doi:10.1002/brb3.3616
38. Albaqami FF, Abdel-Rahman RF, Althurwi HN, et al. Targeting inflammation and oxidative stress for protection against ischemic brain injury in rats using cupressuflavone. Saudi Pharm J. 2024;32(1):101933. doi:10.1016/j.jsps.2023.101933
39. Bui TA, Jickling GC, Winship IR. Neutrophil dynamics and inflammaging in acute ischemic stroke: a transcriptomic review. Front Aging Neurosci. 2022;14:1041333. doi:10.3389/fnagi.2022.1041333
40. Alsbrook DL, Di Napoli M, Bhatia K, et al. Neuroinflammation in acute ischemic and hemorrhagic stroke. Curr Neurol Neurosci Rep. 2023;23(8):407–431. doi:10.1007/s11910-023-01282-2
41. Matsumoto S, Murozono M, Kanazawa M, Nara T, Ozawa T, Watanabe Y. Edaravone and cyclosporine a as neuroprotective agents for acute ischemic stroke. Acute Med Surg. 2018;5(3):213–221. doi:10.1002/ams2.343
42. Xu X, Jiang Y. The yin and yang of innate immunity in stroke. Biomed Res Int. 2014;2014:807978. doi:10.1155/2014/807978
43. Li W, Ren X, Zhang L. Clinical efficacy of atorvastatin calcium combined with aspirin in patients with acute ischemic stroke and effect on neutrophils, lymphocytes and il-33. Exp Ther Med. 2020;20(2):1277–1284. doi:10.3892/etm.2020.8820
44. Xue J, Huang W, Chen X, et al. Neutrophil-to-lymphocyte ratio is a prognostic marker in acute ischemic stroke. J Stroke Cerebrovasc Dis. 2017;26(3):650–657. doi:10.1016/j.jstrokecerebrovasdis.2016.11.010
45. Chen C, Gu L, Chen L, et al. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio as potential predictors of prognosis in acute ischemic stroke. Front Neurol. 2020;11:525621. doi:10.3389/fneur.2020.525621
46. Zhu F, Ji Y, Song JH, Huang GX, Zhang YF. Correlations between nlr, nhr, and clinicopathological characteristics, and prognosis of acute ischemic stroke. Medicine. 2023;102(24):e33957. doi:10.1097/MD.0000000000033957
47. Zhu F, Wang Z, Song J, Ji Y. Correlation analysis of inflammatory markers with the short-term prognosis of acute ischaemic stroke. Sci Rep. 2024;14(1):17772. doi:10.1038/s41598-024-66279-4
48. Agard TA, Hass R, Cavrak ME, et al. Neutrophil lymphocyte ratio (nlr) and systemic immune inflammatory index (sii) for the differential diagnosis of ct-negative mild acute ischemic stroke and transient ischemic attack. Int J Neurosci. 2024;134(9):943–950. doi:10.1080/00207454.2023.2171877
49. Fichet J, de Labriolle A, Giraudeau B, Arbeille P, Charbonnier B. Reducing risk of stroke in patients with acute coronary syndrome: is screening for asymptomatic carotid disease useful? Heart Vessels. 2008;23(6):397–402. doi:10.1007/s00380-008-1065-6
50. Komorovsky R, Desideri A, Coscarelli S, et al. Prognostic implications of sonographic characteristics of carotid plaques in patients with acute coronary syndromes. Heart. 2005;91(6):819–820. doi:10.1136/hrt.2004.042283
51. Jreij G, Canton G, Hippe DS, et al. Systematic review of biomechanical forces associated with carotid plaque disruption and stroke. J Vasc Surg. 2025. doi:10.1016/j.jvs.2025.05.014
52. Prati P, Tosetto A, Casaroli M, et al. Carotid plaque morphology improves stroke risk prediction: usefulness of a new ultrasonographic score. Cerebrovasc Dis. 2011;31(3):300–304. doi:10.1159/000320852
53. Kawai T, Ohishi M, Takeya Y, et al. Carotid plaque score and intima media thickness as predictors of stroke and mortality in hypertensive patients. Hypertens Res. 2013;36(10):902–909. doi:10.1038/hr.2013.61
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Development of Risk Prediction Model for Muscular Calf Vein Thrombosis with Acute Exacerbation of Chronic Obstructive Pulmonary Disease
Hu X, Li X, Xu H, Zheng W, Wang J, Wang W, Li S, Zhang N, Wang Y, Han K
International Journal of General Medicine 2022, 15:6549-6560
Published Date: 10 August 2022
Development and Validation of a Risk Nomogram Model for Predicting Constipation in Patients with Type 2 Diabetes Mellitus
Yuan HL, Zhang X, Peng DZ, Lin GB, Li HH, Li FX, Lu JJ, Chu WW
Diabetes, Metabolic Syndrome and Obesity 2023, 16:1109-1120
Published Date: 20 April 2023
Development and Validation of Prediction Models for All-Cause Mortality and Cardiovascular Mortality in Patients on Hemodialysis: A Retrospective Cohort Study in China
Yang M, Yang Y, Xu Y, Wu Y, Lin J, Mai J, Fang K, Ma X, Zou C, Lin Q
Clinical Interventions in Aging 2023, 18:1175-1190
Published Date: 28 July 2023
Identification of Immuno-Inflammation-Related Biomarkers for Acute Myocardial Infarction Based on Bioinformatics
You H, Dong M
Journal of Inflammation Research 2023, 16:3283-3302
Published Date: 7 August 2023
An Easy-to-Use Nomogram Based on SII and SIRI to Predict in-Hospital Mortality Risk in Elderly Patients with Acute Myocardial Infarction
Chen Y, Xie K, Han Y, Xu Q, Zhao X
Journal of Inflammation Research 2023, 16:4061-4071
Published Date: 13 September 2023



