Back to Journals » Journal of Inflammation Research » Volume 17
Prediction of the Short-Term Effectiveness of Ustekinumab in Patients with Moderate to Severe Crohn’s Disease
Authors Su T , Liu L, Meng F, Wu H , Liu T, Deng J, Peng X, Zhi M, Yao J
Received 17 July 2024
Accepted for publication 12 November 2024
Published 20 November 2024 Volume 2024:17 Pages 9181—9191
DOI https://doi.org/10.2147/JIR.S479618
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Tao Su,1,2,* Ling Liu,3,* Fan Meng,4,* Hongzhen Wu,1,2 Tao Liu,1,2 Jun Deng,1,2 Xiang Peng,1,2 Min Zhi,1,2 Jiayin Yao1,2
1Department of Gastroenterology, Guangdong Provincial Key Laboratory of Colorectal and Pelvic Floor Disease, The Sixth Affiliated Hospital, Sun Yat-Sen University, Guangzhou, Guangdong Province, People’s Republic of China; 2Biomedical Innovation Center, The Sixth Affiliated Hospital, Sun Yat-Sen University, Guangzhou, Guangdong Province, People’s Republic of China; 3Department of Anesthesiology, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong Province, People’s Republic of China; 4Digestive System Department, The First Affiliated Hospital of Gannan Medical University, Ganzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Min Zhi; Jiayin Yao, Department of Gastroenterology, The Sixth Affiliated Hospital, Sun Yat-Sen University, 26th Yuancun the Second Road, Guangzhou, Guangdong Province, 510655, People’s Republic of China, Email [email protected]; [email protected]
Background: Ustekinumab (UST) is recommended as the first-line treatment for patients with moderate to severe Crohn’s disease (CD). However, the efficacy of certain patients may be suboptimal and necessitate intensive treatment or modification of the treatment regimen. We sought to establish a nomogram model to predict the short-term effectiveness of UST in moderate to severe CD patients.
Methods: We established a derivation cohort comprising patients diagnosed with CD and treated with UST at the Sixth Affiliated Hospital of Sun Yat-sen University from May 2020 to July 2023. The patient data, including demographic and clinical characteristics as well as treatment details, were systematically collected. The achievement of clinical remission (defined as Crohn’s Disease Activity Index, CDAI < 150, without corticosteroid usage) after induction therapy was the endpoint observed during follow-up. Potential predictors were identified through the Least Absolute Shrinkage and Selection Operator (LASSO) regression analysis. Subsequently, a multivariate logistic regression analysis was conducted to construct a nomogram model. The predictive accuracy and discriminative power of the model were assessed by Receiver Operating Characteristics (ROC) curves and calibration curves. Decision curve analysis (DCA) was employed to assess the clinical application value of the model.
Results: 162 patients were included in the derivation cohort. The predictor’s selection was according to the minimum criteria. Prognostic factors, including duration, body mass index (BMI), smoking, extraintestinal manifestations (EIMs), perianal lesions (P), history of Vedolizumab therapy, and albumin levels (ALB), were identified and included in the nomogram. The model showed good discrimination and calibration on internal validation based on the bootstrap method (C-index: 0.843, 95% confidence interval: 0.768– 0.903). Moreover, DCA demonstrated that the nomogram was clinically beneficial.
Conclusion: We constructed a practical tool to assist clinicians in identifying moderate to severe CD patients who are expected to have a good clinical response to UST, promoting personalized treatment and the development of precision medicine.
Keywords: Ustekinumab, Crohn’s disease, clinical remission, nomogram
A Letter to the Editor has been published for this article.
Introduction
Crohn’s disease (CD) is a chronic inflammatory disease that primarily affects the gastrointestinal tract. Common clinical manifestations include frequent episodes of diarrhea, abdominal cramping, and significant weight loss.1 The treatment modalities primarily encompass pharmacotherapy and surgical intervention.2 Regarding pharmacotherapy, commonly employed medications comprise non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, biological agents such as tumor necrosis factor-alpha (TNF-α) inhibitors and immunosuppressants.3 For an extended period, TNF-α inhibitors like infliximab (IFX), and adalimumab (ADA) constituted the exclusive class of biological agents employed for managing CD in China.
Ustekinumab (UST), a monoclonal antibody that specifically targets the p40 subunit of interleukin-12 and interleukin-23, has emerged as a novel therapeutic agent approved for the management of CD in recent years.4 Specifically, UST has been recommended as induction therapy for achieving remission in adults diagnosed with moderate to severe CD.5 The study indicates that UST is not inferior to IFX in terms of short-term efficacy and onset of action.6 Additionally, UST is characterized by low immunogenicity, a low incidence of anti-drug antibodies, and high safety. Even among patients who have failed anti–TNF-α therapy, UST demonstrated significant efficacy.7,8 However, similar to the TNF-α inhibitors class, some patients did not respond to UST.9 The efficacy of UST varies among individuals and its high cost necessitates selective treatment for patients with the highest likelihood of response.10
The mechanism of UST anti-response or failure response is multi-factor, including disease characteristics, drugs, and treatment strategies. Based on genomics, protein groups, and pharmacology, the cost of research is high, and it is difficult to enter clinical practice in the short term. The scientific ECCO workshop also emphasized the need to re-understand and analyze the existing clinical prognostic markers for better generalization performance.10 The objective of our study is to develop and validate prediction models utilizing baseline variables (eg, demographics, clinical characteristics, biochemical markers, etc). To predict the probability of achieving clinical remission following induction therapy in patients before initiating UST treatment, so as to guide the development of individualized treatment plan to promote precision medicine.
Materials and Methods
Study Design and Patients
This was a single-center retrospective observational cohort study. We established a derivation cohort comprising patients diagnosed with CD and treated with UST at the Sixth Affiliated Hospital of Sun Yat-sen University from May 2020 to July 2023. The study was approved by the Ethics Committee of Sun Yat-Sen University (2024ZSLYEC-243) and, therefore, adheres to the ethical standards outlined in the Declaration of Helsinki. Given the retrospective nature of this study and the utilization of anonymous data, our Institutional Review Board waived the requirement for written informed consent.
In this study, patients who met the following inclusion criteria were included: First, the diagnosis of CD was established based on internationally accepted criteria in combination with clinical presentation, endoscopic examination, radiology, histopathology, and serology.11,12 Second, the patient was in the moderate to severe disease activity stage, that is, Crohn’s disease Activity Index (CDAI) > 220.13 Third, patients received UST and were followed regularly through 16/20 weeks. Finally, pre-treatment clinical data were available, including baseline biologic measures, and demographic and clinical characteristics, among others. Patients with ambiguous diagnoses or discontinuation of UST therapy or modification in treatment regimen within a 16-week period were excluded. The patients received an initial intravenous infusion of UST, with a dosage of 260 mg for individuals weighing < 55 kg, 520 mg for those weighing > 85 kg, and 390 mg for those weighing between 55–85 kg. This was followed by subsequent subcutaneous injections of UST at a dose of 90 mg every 8 or 12 weeks.14 The visual representation of the study design can be observed in Figure 1.
 |
Figure 1 The study flowchart. The flowchart illustrates the patient screening process and the model construction process. |
Definition of Outcome
The outcome of the present study was clinical remission after induction therapy. Clinical remission was defined as CDAI < 150, without the use of corticosteroids.13 We selected this outcome measure because a large number of patients lacked baseline endoscopic data and fecal calprotectin data. Although CDAI is influenced by the subjective feelings of patients, considering the actual situation in China, the improvement of clinical symptoms is an important factor in ensuring patient treatment compliance.15,16 Induction therapy refers to the first two treatments of UST, and based on the interval time (8 or 12 weeks) until the third UST treatment, the assessment time for clinical remission is approximately between weeks 16–20.
Data Collection
Potential predictors were identified through a comprehensive review of clinical expertise and existing literature. The specific variables collected were as follows: gender; age; disease classification (Montreal classification);17 disease duration; smoking habit; body mass index (BMI); previous medical and surgical treatment history; extraintestinal manifestations (EIMs); C-reactive protein (CRP); albumin (Alb); platelet count (PLT) and other laboratory indicators; CDAI. Response to induction therapy including symptoms and laboratory indicators. The CDAI was assessed by two or more senior gastroenterologists based on hospitalization records and follow-up documentation.
Statistical Analysis
Multiple imputation was performed for a variable if less than 20% of data were missing. Predictive mean matching was employed for imputing numeric features, logistic regression was utilized for imputing binary variables, and Bayesian polytomous regression was applied for imputing factor features.18 We conducted 100 imputations and selected the final imputed dataset based on the Akaike information criterion (AIC). The continuous data was presented as mean ± standard deviation (SD), while the categorical data was reported as the count (proportion). The comparison between clinical remission and nonclinical remission groups was conducted by unpaired t-tests or chi-square tests. For model development, the least absolute shrinkage and selection operator (LASSO) regression technique was employed to identify predictors for multivariable analysis. LASSO regression is a kind of compressed estimation, which can avoid over-fitting and solve the problem of severe collinearity by constructing a penalty function to get a more refined model. The final model was established by multivariate logistic regression analysis based on the AIC. The discriminative power was evaluated by calculating the area under the receiver operating characteristic curve (AUROC). The calibration was evaluated by plotting the calibration curve and employing the Hosmer-Lemeshow test.19 The clinical application value of the model was assessed by decision curve analysis (DCA).20 The bootstrap method was employed to conduct internal validation.21 The performance of the models was compared by calculating Net Reclassification Improvement (NRI) and Integrated Discrimination Improvement (IDI). All statistical analysis and nomogram construction were conducted in R software (version 4.2.3).
Results
Patient Characteristics
The derivation cohort consisted of 162 patients. Among the collected variables, only 3 had missing values, with the highest percentage of missingness being 9.7%. A total of 125 (77.2%) patients achieved clinical remission after induction therapy. The lesion location of L4 was excluded from the predictive factors because of its low proportion in the total study population (2 cases, 1.2%). Table 1 showcased the clinical and demographic traits of the study cohort by the outcome metric.
 |
Table 1 Comparison of Demographic and Clinical Characteristics Between Patients with Different Observed Outcomes |
Predictor Selection
The LASSO regression analysis incorporated a total of 26 variables. (Figure 2). Based on the 1-standard error (SE) criteria, disease duration, and Alb remained significant predictors. Based on the minimum criteria, 9 variables remained potential predictors of clinical remission, including disease duration, BMI, smoking habit, EIMs, perianal lesions (P), disease behavior, history of TNF-α inhibitors therapy, history of Vedolizumab (VDZ) therapy, and Alb.
To develop the prediction models, we included the 2 and 9 variables selected after LASSO regression analysis into the multivariate logistic regression analysis, resulting in the construction of Model A and Model B, respectively. Table 2 shows the results of the multivariate analysis.
 |
Table 2 Multivariable Logistic Analysis to Screen the Potential Prognostic Factors |
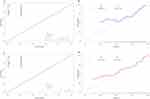
The Performance of the Prediction Models
The AUROC of Model A was 0.763 (95% confidence interval [CI], 0.682–0.843), and the internal validation by the bootstrap method with resampling set at 1000 iterations yielded a consistent AUROC value of 0.763 (95% CI, 0.684–0.844). Model B exhibited an AUROC of 0.843 (95% CI, 0.778–0.908), and internal validation using the bootstrap method with resampling set at 1000 iterations also resulted in an AUROC value of 0.843 (95% CI, 0.768–0.903). DeLong’s test for two correlated ROC curves demonstrated statistically significant differences between the models (P=0.027). (Figure 3) Both models showed good calibration. (Figure 4) The P values of the Hosmer–Lemeshow test were 0.619 and 0.196, respectively, suggesting that the models had a strong goodness of fit.
DCA was employed and visualized to evaluate the two models’ clinical application value. (Figure 5) The decision curves demonstrated that employing two models to predict the probability of clinical remission yields greater benefits compared to either implementing treat-all or treat-none strategies, provided that the threshold probability for achieving clinical remission exceeds 22%. Moreover, the benefits of Model B outweigh those of Model A. Compared with Model A, Model B revealed a positive NRI (0.207, 95% CI, 0.011–0.403, P=0.039) and IDI (0.119, 95% CI, 0.051–0.187, P<0.001). Based on the aforementioned analysis, Model B had been determined as the ultimate prediction model for predicting the short-term efficacy of UST. To visually illustrate the prediction model, we have constructed a nomogram and demonstrated its application through an example to provide a clinically practical tool. (Figure 6)
Discussion
In this study, we established a nomogram model to predict the short-term efficacy of UST in moderate to severe CD patients. The model incorporated 7 variables, including disease duration, BMI, smoking habit, EIMs, P, history of VDZ therapy, and Alb. The AUROC of the model was 0.843. The nomogram showed good calibration and clinical application value.
CD, a subtype of inflammatory bowel disease (IBD), can affect the entire digestive tract, and there is currently no cure, which means that patients need lifelong treatment and sustained economic costs.22 According to statistics, the point prevalence of CD in the United States exhibited a significant increase, rising from 56 per 100,000 individuals in 2010 to 165 per 100,000 individuals in 2019.23 The estimated direct annual costs incurred by patients with IBD varied from $7,824 to $41,829. CD was linked to higher expenditures than ulcerative colitis.24 In China, the average annual cost of CD treatment amounted to approximately 54,000 yuan, with hospitalization expenses accounting for 57.4% and individuals bearing 55.6% of the financial burden.25
Limited research has been conducted to explore the association between clinical, biological, or pharmacological parameters and UST responsiveness. Previously reported predictors, including demographic characteristics such as age and sex, did not appear to be associated with primary response to UST.26 One study suggested that prior anti-TNF-α therapy was a risk factor for UST treatment failure, but this was not supported by another study.27,28 The presence of ileocolonic disease, absence of prior surgery, and uncomplicated phenotype were found to be associated with better response to UST in CD patients.29 Conversely, perianal disease and smoking may be negative predictors of the short-term efficacy of UST.28,30 Unlike anti-TNF-α therapy, UST did not show an association between high CRP levels at baseline and a positive response in CD patients.4 However, the albumin-to-CRP ratio at week 6 was a good predictor of long-term efficacy to UST.31 And lower albumin levels at baseline may be a risk factor for dose escalation of UST.32
Overall, the clinical remission rate after the induction therapy is approximately 50% to 70%, with a significant proportion of patients exhibiting suboptimal response to UST. In our study, a longer disease duration, higher BMI, and perianal involvement were identified as negative predictors of clinical remission following induction therapy through multivariate logistic regression analysis. Conversely, a higher baseline Alb level was found to be associated with the opposite outcome. Except for BMI, the overall findings were in line with clinical observations and previous research studies. The study by Wong et al revealed an inverse correlation between higher BMI and UST drug levels, while no significant impact of BMI on clinical efficacy was observed.33 However, another study showed that low baseline BMI was a negative predictor of clinical remission.34 Further research is needed to clarify the relationship. Smoking was not found to influence clinical remission in our cohort, but this may be attributed to the limited number of cases included in our study. We have not yet found any studies reporting the effect of VDZ failure on the efficacy of UST. However, UST as a second-line biotherapy after VDZ failure was effective for more than 60% of CD patients.35
The advantage of our model is that access to the indicators is simple, without invasive means or complex indicators such as omics. This can improve patient acceptability and reduce costs. The predicted results can guide clinicians to develop individualized treatment plans. For example, a concurrent immunomodulator may be administered as an induction therapy in patients with a low expected probability of clinical remission.36 Our study is in line with the ECCO initiative and promotes the development of precision medicine.10
Our study has certain limitations. Firstly, in this study, the sample size was limited, and some indicators such as L4 had fewer cases. Secondly, clinical remission is not the optimal treatment endpoint recommended by the guidelines. Mucosal healing and transmural healing should be deeper treatment goals. However, we believe that clinical remission should be the initial goal of treatment. Finally, we did not conduct external validation, which limited the generalization performance of the model.
Conclusion
In conclusion, using data from 162 patients with moderate-to-severe CD, we successfully developed a nomogram model to predict the short-term efficacy of UST. This tool will assist clinicians in identifying patients who are expected to have a favorable clinical response to UST, aiding in the formulation of personalized treatment plans and advancing the development of precision medicine. Furthermore, by predicting patients’ drug responses before medication, especially when drug options are limited or due to economic burdens, identifying those with low benefits and altering treatment plans accordingly can prevent treatment delays and improve patient outcomes.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Disclosure of Ethical Statements
This study adheres to the ethical standards outlined in the Declaration of Helsinki and was approved by the Ethics Committee of Sun Yat-Sen University (2024ZSLYEC-243).
Patient Consent Statement
Due to the retrospective study design, which utilized de-identified data, written informed consent from the patients was exempted.
Acknowledgment
Supported by the program of Guangdong Provincial Clinical Research Center for Digestive Diseases (2020B1111170004). The abstract of this paper was presented at the 12th annual meeting of the Asian Organization for Crohn’s and Colitis (AOCC) as a poster presentation with interim findings.
Funding
This study was supported by the National Natural Science Foundation of China [81900490] and Project 1010 of the Sixth Affiliated Hospital of Sun Yat-Sen University [1010PY(2020)-55].
Disclosure
All authors declare no conflict of interest.
References
1. Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn’s disease. Lancet. 2017;389(10080):1741–1755. doi:10.1016/s0140-6736(16)31711-1
2. Adamina M, Bonovas S, Raine T, et al. ECCO Guidelines on Therapeutics in Crohn’s Disease: surgical Treatment. J Crohns Colitis. 2020;14(2):155–168. doi:10.1093/ecco-jcc/jjz187
3. Torres J, Bonovas S, Doherty G, et al. ECCO Guidelines on Therapeutics in Crohn’s Disease: medical Treatment. J Crohns Colitis. 2020;14(1):4–22. doi:10.1093/ecco-jcc/jjz180
4. Feagan BG, Sandborn WJ, Gasink C, et al. Ustekinumab as Induction and Maintenance Therapy for Crohn’s Disease. N Engl J Med. 2016;375(20):1946–1960. doi:10.1056/NEJMoa1602773
5. Macaluso FS, Papi C, Orlando A, et al. Use of biologics for the management of Crohn’s disease: IG-IBD clinical guidelines based on the GRADE methodology. Dig Liver Dis. 2023;55(4):442–453. doi:10.1016/j.dld.2023.01.155
6. Narula N, Wong ECL, Dulai PS, et al. Comparative Efficacy and Rapidity of Action for Infliximab vs Ustekinumab in Biologic Naïve Crohn’s Disease. Clin Gastroenterol Hepatol. 2022;20(7):1579–1587.e2. doi:10.1016/j.cgh.2021.04.006
7. Bressler B. Is there an optimal sequence of biologic therapies for inflammatory bowel disease? Therap Adv Gastroenterol. 2023;16:17562848231159452. doi:10.1177/17562848231159452
8. Chang S, Hudesman D. First-Line Biologics or Small Molecules in Inflammatory Bowel Disease: a Practical Guide for the Clinician. Curr Gastroenterol Rep. 2020;22(2):7. doi:10.1007/s11894-020-0745-y
9. Sandborn WJ, Rebuck R, Wang Y, et al. Five-Year Efficacy and Safety of Ustekinumab Treatment in Crohn’s Disease: the IM-UNITI Trial. Clin Gastroenterol Hepatol. 2022;20(3):578–590.e4. doi:10.1016/j.cgh.2021.02.025
10. Verstockt B, Noor NM, Marigorta UM, Pavlidis P, Deepak P, Ungaro RC. Results of the Seventh Scientific Workshop of ECCO: precision Medicine in IBD-Disease Outcome and Response to Therapy. J Crohns Colitis. 2021;15(9):1431–1442. doi:10.1093/ecco-jcc/jjab050
11. Gomollón F, Dignass A, Annese V, et al. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: part 1: diagnosis and Medical Management. J Crohns Colitis. 2017;11(1):3–25. doi:10.1093/ecco-jcc/jjw168
12. K Wu, J Liang, ZH Ran, JM Qian, H Yang, MH Chen. Chinese consensus on diagnosis and treatment in inflammatory bowel disease (2018, Beijing). J Dig Dis. 2021;22(6):298–317. doi:10.1111/1751-2980.12994
13. Best WR, Becktel JM, Singleton JW, Kern
14. Kotze PG, Ma C, Almutairdi A, Panaccione R. Clinical utility of ustekinumab in Crohn’s disease. J Inflamm Res. 2018;11:35–47. doi:10.2147/jir.S157358
15. Chan W, Chen A, Tiao D, Selinger C, Leong R. Medication adherence in inflammatory bowel disease. Intest Res. 2017;15(4):434–445. doi:10.5217/ir.2017.15.4.434
16. Cohen NA, Micic DM, Sakuraba A. Factors associated with poor compliance amongst hospitalized, predominantly adolescent pediatric Crohn’s disease patients. Ann Med. 2022;54(1):886–892. doi:10.1080/07853890.2022.2057582
17. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55(6):749–753. doi:10.1136/gut.2005.082909
18. Rubin DB, Schenker N. Multiple imputation in health-care databases: an overview and some applications. Stat Med. 1991;10(4):585–598. doi:10.1002/sim.4780100410
19. Steyerberg EW, Vickers AJ, Cook NR, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology. 2010;21(1):128–138. doi:10.1097/EDE.0b013e3181c30fb2
20. Van Calster B, Wynants L, Verbeek JFM, et al. Reporting and Interpreting Decision Curve Analysis: a Guide for Investigators. Eur Urol. 2018;74(6):796–804. doi:10.1016/j.eururo.2018.08.038
21. Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): the TRIPOD statement. Ann Intern Med. 2015;162(1):55–63. doi:10.7326/m14-0697
22. Nakase H, Uchino M, Shinzaki S, et al. Evidence-based clinical practice guidelines for inflammatory bowel disease 2020. J Gastroenterol. 2021;56(6):489–526. doi:10.1007/s00535-021-01784-1
23. Hutfless S, Jasper RA, Chen PH, Joseph S, Miller S, Brant SR. Burden of Crohn’s Disease in the United States Medicaid Population, 2010–2019. Clin Gastroenterol Hepatol. 2023. doi:10.1016/j.cgh.2023.05.002
24. Kahn-Boesel O, Cautha S, Ufere NN, Ananthakrishnan AN, Kochar B. A Narrative Review of Financial Burden, Distress, and Toxicity of Inflammatory Bowel Diseases in the United States. Am J Gastroenterol. 2023;118(9):1545–1553. doi:10.14309/ajg.0000000000002345
25. Zhou WP, Mu N, Jian WY, Wang HH. Economic burden and factors associated with Crohn’s disease. Beijing Da Xue Xue Bao Yi Xue Ban. 2021;53(3):555–559. doi:10.19723/j.issn.1671-167X.2021.03.019
26. Gisbert JP, Chaparro M. Predictors of Primary Response to Biologic Treatment [Anti-TNF, Vedolizumab, and Ustekinumab] in Patients With Inflammatory Bowel Disease: from Basic Science to Clinical Practice. J Crohns Colitis. 2020;14(5):694–709. doi:10.1093/ecco-jcc/jjz195
27. Johnson AM, Barsky M, Ahmed W, et al. The Real-World Effectiveness and Safety of Ustekinumab in the Treatment of Crohn’s Disease: results From the SUCCESS Consortium. Am J Gastroenterol. 2023;118(2):317–328. doi:10.14309/ajg.0000000000002047
28. Parra RS, Chebli JMF, Queiroz NSF, et al. Long-term effectiveness and safety of ustekinumab in bio-naïve and bio-experienced anti-tumor necrosis factor patients with Crohn’s disease: a real-world multicenter Brazilian study. BMC Gastroenterol. 2022;22(1):199. doi:10.1186/s12876-022-02280-3
29. Barré A, Colombel JF, Ungaro R. Review article: predictors of response to vedolizumab and ustekinumab in inflammatory bowel disease. Aliment Pharmacol Ther. 2018;47(7):896–905. doi:10.1111/apt.14550
30. Dalal RS, Njie C, Marcus J, Gupta S, Allegretti JR. Predictors of Ustekinumab Failure in Crohn’s Disease After Dose Intensification. Inflamm Bowel Dis. 2021;27(8):1294–1301. doi:10.1093/ibd/izaa282
31. Waljee AK, Wallace BI, Cohen-Mekelburg S, et al. Development and Validation of Machine Learning Models in Prediction of Remission in Patients With Moderate to Severe Crohn Disease. JAMA Netw Open. 2019;2(5):e193721. doi:10.1001/jamanetworkopen.2019.3721
32. Petrov JC, Al-Bawardy B, Alzahrani R, Mohamed G, Fine S. Rates, Predictors, and Outcomes of Ustekinumab Dose Escalation in Inflammatory Bowel Disease. J Clin Gastroenterol. 2024. doi:10.1097/mcg.0000000000002003
33. Wong ECL, Marshall JK, Reinisch W, Narula N. Body Mass Index Does Not Impact Clinical Efficacy of Ustekinumab in Crohn’s Disease: a Post Hoc Analysis of the IM-UNITI Trial. Inflamm Bowel Dis. 2021;27(6):848–854. doi:10.1093/ibd/izaa214
34. Liefferinckx C, Verstockt B, Gils A, et al. Long-term Clinical Effectiveness of Ustekinumab in Patients with Crohn’s Disease Who Failed Biologic Therapies: a National Cohort Study. J Crohns Colitis. 2019;13(11):1401–1409. doi:10.1093/ecco-jcc/jjz080
35. Albshesh A, Bannon L, Sharar Fischler T, et al. Comparison of Short- and Long-Term Effectiveness between Anti-TNF and Ustekinumab after Vedolizumab Failure as First-Line Therapy in Crohn’s Disease: a Multi-Center Retrospective Cohort Study. J Clin Med. 2023;12(7):2503. doi:10.3390/jcm12072503
36. Yoshihara T, Shinzaki S, Amano T, et al. Concomitant use of an immunomodulator with ustekinumab as an induction therapy for Crohn’s disease: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2021;36(7):1744–1753. doi:10.1111/jgh.15401
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Predicting Mucosal Healing in Crohn’s Disease: A Nomogram Model Developed from a Retrospective Cohort
Tang N, Chen H, Chen R, Tang W, Zhang H
Journal of Inflammation Research 2022, 15:5515-5525
Published Date: 23 September 2022