Back to Journals » Journal of Inflammation Research » Volume 17
Predictive Factors and Nomogram for Spontaneous Bacterial Peritonitis in Decompensated Cirrhosis Among the Elderly
Authors Yan F , Peng X, Yang X, Yuan L, Zheng X, Yang Y
Received 1 August 2024
Accepted for publication 28 November 2024
Published 12 December 2024 Volume 2024:17 Pages 10901—10911
DOI https://doi.org/10.2147/JIR.S484629
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tara Strutt
Fang Yan,1,2,* Xiaoxia Peng,1,* Xingyao Yang,3,* Li Yuan,4,* Xiaomei Zheng,1 Yongxue Yang1
1Geriatric Diseases Institute of Chengdu, Department of Geriatrics, Chengdu Fifth People’s Hospital (The Second Clinical Medical College, Affiliated Fifth People’s Hospital of Chengdu University of Traditional Chinese Medicine), Chengdu, People’s Republic of China; 2Center for Medicine Research and Translation, Chengdu Fifth People’s Hospital (The Second Clinical Medical College, Affiliated Fifth People’s Hospital of Chengdu University of Traditional Chinese Medicine), Chengdu, People’s Republic of China; 3Geriatric Diseases Institute of Chengdu, Department of Orthopedics, Chengdu Fifth People’s Hospital (The Second Clinical Medical College, Affiliated Fifth People’s Hospital of Chengdu University of Traditional Chinese Medicine), Chengdu, People’s Republic of China; 4Department of Clinical Laboratory, Chengdu Fifth People’s Hospital (The Second Clinical Medical College, Affiliated Fifth People’s Hospital of Chengdu University of Traditional Chinese Medicine), Chengdu, Sichuan Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yongxue Yang; Xiaomei Zheng, Email [email protected]; [email protected]
Background and Aims: Spontaneous bacterial peritonitis (SBP) represents a significant complication in the decompensated phase of cirrhosis. The challenges in treating SBP and the associated mortality rates are markedly elevated in elderly individuals. Timely detection and intervention for SBP are imperative. We aimed to develop a predictive tool for the occurrence of SBP in elderly individuals with decompensated cirrhosis (DC).
Methods: Elderly patients diagnosed with DC were enrolled from Chengdu Fifth People’s Hospital in China, spanning from January 1, 2015, to September 31, 2023. Among the patients, 337 were assigned to the training cohort, while 145 were designated to the validation cohort. A multivariate logistic regression analysis was performed to identify significant predictors and to develop a nomogram for predicting the occurrence of SBP. To evaluate the model’s discrimination and calibration, a bootstrap method with 1000 resamples was utilized.
Results: Findings from the multivariate logistic regression analysis indicated that constipation (odds ratio [OR] 2.09, 95% confidence interval [CI] 1.25− 3.49, P=0.005), ascites (OR 2.84, 95% CI 1.64− 4.92, P< 0.001), Child-Pugh-Turcotte (CPT) score (OR 4.80, 95% CI 1.69− 13.60, P=0.003), and high sensitivity C-reactive protein (hs-CRP) (OR 2.96, 95% CI 1.54− 5.45, P=0.001) were significant independent predictors for the occurrence of SBP in elderly individuals with DC. The generated nomogram showed an area under the curve of 0.779 for the training cohort and 0.817 for the validation cohort. The nomogram’s calibration curve nearly matched the perfect diagonal line, and decision curve analysis showed an improved net benefit for the model. Subsequent validation further corroborated the reliability of the predictive nomogram.
Conclusion: In conclusion, the nomogram, incorporating variables such as constipation, ascites, CPT score, and hs-CRP, effectively predicted the occurrence of SBP in elderly patients with DC, underscoring its substantial clinical applicability.
Keywords: spontaneous bacterial peritonitis, decompensated cirrhosis, elderly, nomogram
Introduction
Spontaneous bacterial peritonitis (SBP) frequently occurs in individuals suffering from severe liver conditions, especially liver cirrhosis (LC), and greatly impacts mortality and morbidity.1 SBP usually occurs without an identifiable source of infection, so it was once called primary peritonitis. And it is also a sign of serious or worsening underlying diseases.2 As the population ages, there is a growing proportion of elderly individuals with cirrhosis who are at increased risk for infections. Studies indicate that infections are the primary cause of death among elderly cirrhosis patients, with a fatality rate of 12% to 15% in those with SBP complications, compared to under 10% in younger adults.3
The prevalence of symptoms in individuals with SBP commonly includes fever, chills, and abdominal pain, with some cases presenting confusion or exhibiting no symptoms.1 SBP can manifest in an atypical manner in elderly individuals due to physiological decline and compromised immune responses. Despite numerous studies addressing the morbidity, diagnosis, and treatment of SBP, early detection remains challenging. SBP is diagnosed according to the protocols set by the European Association for the Study of the Liver and the American Association for the Study of Liver Diseases, which recommend that high levels of polymorphonuclear leukocytes in ascitic fluid, in the absence of an intra-abdominal infection source, signify SBP.4,5 However, ascites puncture, a necessary invasive procedure to confirm SBP, is hindered by poor patient compliance and time-consuming nature, resulting in a low positive rate ranging from 35% to 65%.6 Moreover, elderly patients with compromised physical health may not be suitable candidates for ascites puncture. Therefore, early diagnosis of SBP is impeded either due to atypical symptom presentation or limited patient compliance leading to a low positivity rate during ascites puncture testing.
Based on existing diagnostic methods, numerous cases of SBP may be inaccurately diagnosed, resulting in treatment delays or inappropriate antibiotic usage. The principal issue with SBP lies in the potential progression to sepsis, a severe systemic infection with life-threatening consequences. The likelihood of mortality is heightened by delays in both diagnosing and treating SBP.7 Timely identification of SBP is imperative for improving diagnostic precision, lowering clinical mortality rates, and maximizing patient outcomes. Earlier research verified that the Child-Pugh-Turcotte (CPT) score and the model for end-stage liver disease (MELD) score could predict mortality in patients with DC.8,9 Nevertheless, later studies have shown that these scores perform poorly in prediction when compared to alternative scoring systems.10,11
The chronic liver failure-sequential organ failure assessment score (CLIF-SOFA), CLIF consortium acute on chronic liver failure score (CLIF-C ACLF), and CLIF consortium acute decompensation (CLIF-C AD) scores are well-recognized prognostic tools for patients with cirrhosis.12–14 And these scores might provide further depth in assessing the risk and outcomes of SBP. Lately, new markers have been discovered as potential indicators of SBP in DC. For instance, various standard lab test markers such as ascites calprotectin and lactoferrin,15 serum procalcitonin and CRP16, as well as the platelet and neutrophil-to-lymphocyte ratio (NLR)17,18 have been documented in the diagnosis of SBP in DC. Furthermore, other indicators like ascites19, IL-1720 and CD20621 have been identified as possible biomarkers for diagnosing SBP in DC. Nevertheless, these findings still need confirmation because of constraints like limited sample sizes and interfering variables. Therefore, it remains necessary to identify reliable biomarkers for SBP.
A nomogram serves as a valuable tool that integrates multiple risk indicators to predict the comprehensive likelihood of a specific outcome. It enables the quantification of disease risk among patients and holds significant relevance in the prognosis and assessment of various diseases.22–25 While numerous studies have explored the morbidity, diagnosis, and management of SBP, only a handful have pinpointed the independent risk factors of SBP in cirrhotic patients and utilized them to develop a nomogram, especially focusing on adults instead of the elderly. As a result, there is a lack of relevant studies focused on developing a nomogram for predicting SBP in elderly cirrhosis patients.
This study aimed to construct a predictive nomogram that integrates various risk factors to facilitate early prediction of SBP in elderly patients with DC. The nomogram model is expected to perform early risk assessment for patients, followed by risk stratification and early intervention for high-risk individuals to decrease hospitalization duration. For low-risk patients, it may help reduce antibiotic misuse, excessive invasive abdominal punctures, bacterial resistance, and adverse events related to invasive procedures. Consequently, this model can serve as a foundation for the creation of personalized clinical diagnosis and treatment plans, ultimately enhancing healthcare quality.
Methods
Study Design and Population
This study was designed as a retrospective investigation of the data from enrolled elderly SBP patients with cirrhosis managed at Chengdu Fifth People’s Hospital. The study protocol was in accordance with the Declaration of Helsinki and received approval from the Ethics Committee of Chengdu Fifth People’s Hospital (2024–014-01). This retrospective study utilized only pre-existing medical records, ensuring that all data remained anonymous, thereby the requirement for informed consent was waived.
This retrospective analysis included 482 patients admitted to Chengdu Fifth People’s Hospital in Chengdu, China, from January 1, 2015, to September 31, 2023. They were subsequently split into the training cohort and the internal validation cohort at a 7:3 ratio by R language software for further examination.
The inclusion criteria were: a diagnosis of DC and ≥60 years old. The exclusion criteria included individuals with acquired immunodeficiency syndrome, those with tumors, patients experiencing secondary peritonitis or tuberculous peritonitis, those who had received antibiotics within a week before admission, and cases with incomplete clinical records. Every participant in this research belonged to the Han ethnicity.
Data Collection
Both clinical assessments and lab results were gathered upon admission. Clinical data from enrolled patients included the following: demographic information; medical history; clinical symptoms; laboratory data; complications: gastrointestinal bleeding, dominant hepatic encephalopathy, hypersplenism, hepatorenal syndrome, portal vein thrombosis, liver cancer and others.
Definitions
Diagnosing DC relies on LC, accompanied by issues like portal hypertension and/or liver impairment. The identification of liver cirrhosis aligns with the “Chinese guidelines for managing liver cirrhosis”.26 According to the guidelines from the European Association for the Study of the Liver and the American Association for the Study of Liver Diseases, SBP is diagnosed when ascitic fluid shows elevated polymorphonuclear leukocyte counts and there is no other intra-abdominal infection source.4,5
Determination of Training Cohort and Validation Cohort and Screening Variables
The R programming language was employed to split 482 patients into a training group and an internal validation group in a 7:3 proportion, ensuring that outcome events were randomly allocated between the two groups. The training cohort is used to filter variables and build the model, and the internal validation cohort is used to validate the model. Multiple factors were chosen from the dataset, such as albumin activated partial thromboplastin time (APTT), constipation, CPT score, creatinine, high sensitivity C-reactive protein (hs-CRP), gastrointestinal hemorrhage, hepatorenal syndrome, ascites volume, hypersplenism, etiology of cirrhosis (alcoholic and others) and smoking.
Development and Assessment of the Nomogram
Logistic regression analyses, both univariate and multivariate, were performed on the training group to determine the odds ratio (OR) and its 95% confidence interval (CI).Factors identified by univariate logistic regression were subsequently incorporated into a multivariate analysis, where independent predictors (P<0.05) were used to develop a nomogram model for forecasting SBP occurrence.
Guideline lines were subsequently extended upward to determine the scores assigned on the nomogram, with the cumulative points found on the “Total Points” scale. Following this, a vertical line was extended downward to intersect with the lower scales, thereby establishing the likelihood of SBP. The risk score of the nomogram was computed utilizing the designated risk score formula. The ability of the nomogram to discriminate was evaluated by determining the area under the curve (AUC).The effectiveness and calibration precision of the nomogram model were evaluated using the calibration curve. Validation of both discrimination and calibration was performed using bootstrapping with 1000 samples. The overall clinical advantage of the nomogram was assessed using decision curve analysis (DCA).
Statistical Analysis
R software was used for statistical analysis. Logistic regression analyses, both univariate and multivariate, were applied to the training cohort, and the respective OR along with 95% CI were determined. The variables identified through univariate logistic regression analysis were incorporated into the multivariate logistic regression analysis, and the independent risk factors were used to create nomogram. The risk score of the nomogram was calculated with the risk score formula. The nomogram’s predictive power was assessed using the AUC. The efficiency and Calibration degree of the nomogram model was evaluated with the calibration curve. DCA evaluated the nomogram’s net clinical benefit. The variation was statistically meaningful with P<0.05.
Results
General Characteristics
A total of 494 patients were initially recruited from Chengdu Fifth People’s Hospital. However, 12 cases were excluded due to insufficient clinical data, resulting in 482 eligible DC patients being enrolled in the study. These patients were subsequently randomized into a training cohort and an internal validation cohort in a 7:3 ratio (Figure S1). The training cohort comprised 337 patients with an average age of 71.43±7.63 years, including 183 males. The validation cohort consisted of 145 individuals, averaging 71.24±7.00 years old, including 70 males. There were no differences in terms of age or gender ratio between the two cohorts. Additional baseline information and risk factors were presented in Table 1.
 |
Table 1 Development and Validation of Nomogram of SBP Risk Factors for Elderly Patients Hospitalized with Decompensated Cirrhosis |
Screening for Predictive Factors
Univariate and multivariate logistic regression analyses were employed to identify independent predictive factors for the occurrence of SBP in elderly patients with DC.
The variables included in the nomogram were clinical commonly used indicators including albumin, APTT, creatinine, cirrhosis etiology and CPT scores, CLIF-SOFA scores, CLIF-C ACLF scores and CLIF-C AD scores and others were selected in our analysis. Then, a multivariate logistic regression analysis revealed that four factors were independent predictors of SBP in this patient population. The results indicated that constipation (OR 2.09, 95% CI 1.25−3.49), ascites (OR 2.84, 95% CI 1.64−4.92), CPT score (OR 4.80, 95% CI 1.69−13.6), and hs-CRP levels (OR 2.96, 95% CI 1.54−5.45) were significantly associated with the development of SBP in elderly patients with DC (Table 2).
 |
Table 2 Univariate and multivariate Logistic Regression Analyses for Screening Predictors in the training Cohort |
Risk Prediction Nomogram Development
The logistic regression model was developed utilizing the aforementioned four factors within the training cohort. Subsequently, these factors were incorporated into a nomogram (Figure 1). For each patient, a higher total score on the nomogram indicated an elevated risk of SBP. The length of the line corresponding to each variable in the nomogram reflects the magnitude of the predictor’s contribution to the occurrence of SBP.
Verification of the Nomogram
The nomogram was developed using the training cohort, and we validated it with a separate dataset. The AUC for the training and validation cohorts was determined using the ROC curve. As shown in Figure 2, the AUC values for the training and validation cohorts were 0.779 and 0.817, respectively, both approximating 0.8. This suggests that the nomogram exhibits a robust predictive capability for the occurrence of SBP in elderly patients with DC.
 |
Figure 2 ROC curves. (A) Training cohort. (B) Validation cohort. Abbreviation: ROC, receiver operating characteristic; AUC, area under the ROC curve. |
Calibration Curve of the Nomogram
A calibration graph was utilized to compare the nomogram’s calibration curve with the ideal reference line. In this graph, the black dotted line denotes the ideal reference line, while the blue solid line represents the apparent prediction lines, and the red dotted line represent the bias-corrected lines of the nomogram, respectively (Figure 3). The proximity of the predicted line to the ideal line indicates a better fit and a more accurate prediction of the SBP occurrence rate by the nomogram. The calibration curve of the nomogram demonstrated a high consistency between the predicted results and the actual outcomes in this study.
 |
Figure 3 Calibration curves of nomogram of elderly patients with decompensated cirrhosis. (A) Training cohort. (B) Validation cohort. |
Clinical Usefulness of the Nomogram
DCA analysis was conducted to assess the net benefit in two cohorts. For elderly patients, when the threshold probabilities were between 6% and 74% in the training cohort and between 11% and 89% in the validation cohort, the incidence of SBP offered a higher net benefit than the “All” or “None” approaches, demonstrating its value in clinical decision-making (Figure 4).
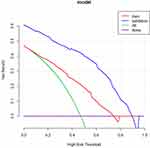 |
Figure 4 Decision curve analysis in prediction of SBP. Abbreviations: SBP, spontaneous bacterial peritonitis. |
Discussion
The present study developed a nomogram that integrated clinically accessible indicators such as constipation, ascites, CPT score, and hs-CRP to predict the likelihood of SBP in elderly patients diagnosed with DC upon hospital admission. The nomogram demonstrated favorable discriminatory and calibration abilities. DCA indicated its potential for practical clinical utility. Consequently, the nomogram provides a user-friendly and personalized tool for healthcare providers to enhance their treatment strategies for elderly DC patients at risk of developing SBP complications.
This research explored the risk elements linked to SBP incidence and discovered four new metrics to develop a tailored nomogram for senior patients with DC. Consistent with our findings, other studies have reported that a nomogram comprising seven variables, including mean red blood cell hemoglobin concentration, prothrombin time, lymphocyte percentage, prealbumin, total bilirubin, CRP and PCT levels served as an effective tool for identifying SBP in adult patients with DC.27 Additionally, a separate study revealed that older age independently influenced predictive models for assessing the prognosis of DC in adults, in contrast to younger individuals.28 Unlike previous studies, our research focuses on establishing a nomogram specifically tailored for elderly DC patients, thereby providing a more specialized tool for this demographic.
Constipation is a common health issue among the elderly, presenting a substantial challenge to achieving healthy longevity in an increasingly aging society.29 A meta-analysis revealed a 10.1% prevalence of chronic constipation according to the Rome IV criteria, with incidence rates increasing with advancing age.30,31 Projections indicate a rise in the number of individuals affected by chronic constipation in the future, with reports suggesting a poor prognosis.32
Our study identified constipation as an independent predictor of SBP in elderly patients with DC. It is hypothesized that constipation may promote bacterial overgrowth within the intestinal tract, resulting in increased intraluminal pressure and subsequent weakening of the intestinal wall. This condition can facilitate the translocation of commensal intestinal bacteria into the peritoneal cavity, potentially leading to peritonitis. The occurrence of HE in cirrhosis is closely associated with constipation, which serves as a risk factor for HE. This is because the large intestine reabsorbs metabolic waste containing ammonia into the bloodstream, causing elevated blood ammonia levels.33 Therefore, it is crucial to assess elderly patients with cirrhosis for symptoms indicative of constipation, such as difficult defecation, dry stool, and a history of constipation, and provide timely interventions when necessary.
Ascites formation is the most prevalent manifestation of DC.34 Approximately 40% of individuals with cirrhosis receive their diagnosis upon presenting with complications such as HE or ascites.35 Long-term survival is diminished in patients with cirrhosis who develop ascites, compared to those with ascites-free cirrhosis, with those developing refractory ascites exhibiting particularly poor prognoses.36 Zhang et al37 reported that ascites was one of the six factors used to construct a nomogram for predicting the risk of first variceal hemorrhage, another complication observed in DC patients. Our study identified ascites as a significant factor in the model for forecasting the occurrence of SBP in older individuals with DC. The likelihood of SBP increased with greater ascites volume.
The CPT score has been recognized as an independent predictor of SBP, with a score of ≥7 associated with a nearly 5.6-fold increase in the odds of SBP occurrence in our study. The CPT score is widely acknowledged as a convenient and reliable method for assessing the prognosis of DC patients.38 This score incorporates five parameters, including three laboratory values and two subjective categories, assigning scores ranging from 5 to 15 and categorizing patients into CTP class A, B, or C.39 Previous research has established that the CPT classification is a significant predictor of concurrent infections in individuals with liver disease.40 The CPT score has been recognized as an important factor associated with the severity of hepatic encephalopathy and may serve as an effective prognostic indicator in patients with DC.41 Specifically, in this study, a higher CPT score is correlated with an increased likelihood of SBP in elderly patients with DC, thereby providing clinicians with a useful method for evaluating the risk of this related complication.
The CLIF-SOFA, CLIF-C ACLF, and CLIF-C AD scores are well-established prognostic tools for patients with cirrhosis. Accordingly, we evaluated these scores, integrated them in our study. However, contrary to our expectations, these scores were not selected as predictors in the nomogram based on the univariate and multivariate logistic regression analyses. It is important to note that our data were collected from a single center, and thus, future studies should include a larger, multi-center cohort to more accurately assess the prognostic value of these scores.
Hs-CRP is a serum protein produced mainly by the liver during the acute phase in reaction to tissue injury.42 Its assay allows for the detection of much lower levels than traditional CRP assays are commonly conducted in various labs to identify infections and assess how patients respond to antibiotic treatments. Nonetheless, the generation of hs-CRP due to infection might be reduced in individuals with liver impairment, making it challenging to interpret hs-CRP levels in those with LC.43,44 Our study found a 4.6-fold increased risk of SBP in elderly patients with DC when hs-CRP levels were ≥4 mg/L compared to those with levels <4 mg/L. These findings are consistent with previous studies reporting that hs-CRP level independently predicted poor outcomes in cirrhotic patients with SBP.45
One notable advantage of this study lied in its integration of comprehensive and clinically accessible data to develop a tool for SBP in elderly inpatients. Additionally, the nomogram formulated in this research demonstrated robust performance in terms of identification, calibration, and clinical application. In addition, the nomogram developed in this study incorporated commonly used clinical indicators, including a single laboratory index (hs-CRP), which was both cost-effective and practical for rapid application relative to other benchmarks. This tool demonstrated ease of use and enhanced predictive accuracy specifically for elderly patients with DC. Its straightforward application offers clinicians an intuitive method for effectively implementing SBP monitoring in hospitalized elderly patients, thereby facilitating the timely identification of high-risk individual. Therefore, it has significant clinical implications for elderly patient management.
However, our study is subject to several limitations. Firstly, it was a retrospective study conducted with internal validation at a single center, which may introduce bias and affect the negative primary outcome. Consequently, prospective and multicenter studies with larger sample sizes and other confounding variables require greater attention and external validations of the nomogram in varied groups are essential for future research. Secondly, the sample size was relatively small. Thirdly, our study primarily relied on data collected within the first 24 hours of admission, whereas dynamic data and the rate of variation in indicators may offer significant clinical insights.
Conclusions
In conclusion, we have developed a nomogram that incorporates clinically accessible indicators, including constipation, ascites, CPT score, and hs-CRP to predict the likelihood of SBP in elderly patients diagnosed with DC upon hospital admission. The nomogram exhibited favorable predictive accuracy and clinical utility following validation. This proposed nomogram represents an easy-to-use tool with significant potential for clinical application.
Data Sharing Statement
The data underlying this article will be shared on reasonable request to the corresponding author.
Acknowledgments
This study was supported by the Chengdu University of Traditional Chinese Medicine Joint Innovation Fund Project (No.LH202402002) and Chengdu Medical Research Project (No.2023459).
Author Contributions
Fang Yan, Xiaoxia Peng, Xingyao Yang and Li Yuan contributed equally to this work and share first authorship. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
None of the authors have conflicts of interest to disclose. None of the authors have financial relationships relevant to this article to disclose.
References
1. Zhang G, Jazwinski FA. Spontaneous Bacterial Peritonitis. JAMA. 2021;325:1118. doi:10.1001/jama.2020.10292
2. Long B, Gottlieb M. Emergency medicine updates: spontaneous bacterial peritonitis. Am J Emerg Med. 2023;70:84. doi:10.1016/j.ajem.2023.05.015
3. Mancinella A, Mancinella M, Marigliano B, et al. [Cirrhotic spontaneous bacterial peritonitis in the elderly]. Recenti Prog Med. 2011;102:28–32.
4. AA DM, AM C, LC L, et al. Multi-resistant bacteria in spontaneous bacterial peritonitis: a new step in management? World J Gastroenterol. 2014;20:14079. doi:10.3748/wjg.v20.i39.14079
5. Wiest R, Lawson M, Geuking M. Pathological bacterial translocation in liver cirrhosis. J Hepatol. 2014;60:197–209. doi:10.1016/j.jhep.2013.07.044
6. Shizuma T. Spontaneous bacterial and fungal peritonitis in patients with liver cirrhosis: a literature review. World J Hepatol. 2018;10:254–266. doi:10.4254/wjh.v10.i2.254
7. Abdu B, Akolkar S, Picking C, et al. Factors Associated with Delayed Paracentesis in Patients with Spontaneous Bacterial Peritonitis. Dig Dis Sci. 2021;66:4035–4045. doi:10.1007/s10620-020-06750-0
8. RN P, IM M-L, JL D, et al. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–649. doi:10.1002/bjs.1800600817
9. PS K, RH W, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464–470. doi:10.1053/jhep.2001.22172
10. FC L, YC F, YK L, et al. Plasma diamine oxidase level predicts 6-month readmission for patients with hepatitis B virus-related decompensated cirrhosis. Virol J. 2019;16:115. doi:10.1186/s12985-019-1219-4
11. Yao Y, Yang D, Huang Y, et al. Predictive value of insulin-like growth factor 1-Child-Turcotte-Pugh score for mortality in patients with decompensated cirrhosis. Clin Chim Acta. 2020;505:141–147. doi:10.1016/j.cca.2020.02.031
12. IMHGCdS B, RiGUFdSCF B, IMHGCdS B, et al. Liver‐specific scores as predictors of mortality in spontaneous bacterial peritonitis. GastroHep. 2020;2:224–231. doi:10.1002/ygh2.419
13. Moreau R, Jalan R, Gines P, et al. Acute-on-Chronic Liver Failure Is a Distinct Syndrome That Develops in Patients With Acute Decompensation of Cirrhosis. Gastroenterology. 2013;144:1426–1437. doi:10.1053/j.gastro.2013.02.042
14. JRdO C, MLd S, WM S, et al. Acute-on-chronic liver failure is independently associated with lower survival in patients with spontaneous bacterial peritonitis. Arquivos de gastroenterologia. 2021;58:344–352. doi:10.1590/s0004-2803.202100000-58
15. KP P, PM K, JP G, et al. Ascitic calprotectin and lactoferrin for detection of spontaneous bacterial peritonitis: a systematic review and meta-analysis. Transl Gastroenterol Hepatol. 2022;7:37. doi:10.21037/tgh-20-323
16. Verma R, Satapathy SK, Bilal M. Procalcitonin and C-reactive protein in the diagnosis of spontaneous bacterial peritonitis. translat Gastroent Hepat. 2022;7:36. doi:10.21037/tgh-19-297
17. Abdel HMR, HA E-A, MN A, et al. Can platelets indices and blood neutrophil to lymphocyte ratio be used as predictors for diagnosis of spontaneous bacterial peritonitis in decompensated post hepatitis liver cirrhosis? Egypt J Immunol. 2022;29:12–24. doi:10.55133/eji.290402
18. Mousa N, Besheer T, Abdel-Razik A, et al. Can combined blood neutrophil to lymphocyte ratio and C-reactive protein be used for diagnosis of spontaneous bacterial peritonitis? Br J Biomed Sci. 2018;75:71–75. doi:10.1080/09674845.2017.1396706
19. Wu X, Luo J, Huang W, et al. Role of ascitic endocan levels in the diagnosis of spontaneous bacterial peritonitis in decompensated cirrhosis. Biomarkers. 2020;25:360–366. doi:10.1080/1354750X.2020.1764107
20. HKH K, AA M, AM H, et al. Serum and ascitic fluid interleukin-17 in spontaneous bacterial peritonitis in Egyptian patients with HCV-related liver cirrhosis. Curr Res Transl Med. 2020;68:237–243. doi:10.1016/j.retram.2020.03.001
21. Stengel S, Quickert S, Lutz P, et al. Peritoneal Level of CD206 Associates With Mortality and an Inflammatory Macrophage Phenotype in Patients With Decompensated Cirrhosis and Spontaneous Bacterial Peritonitis. Gastroenterology. 2020;158:1745–1761. doi:10.1053/j.gastro.2020.01.029
22. Mu X, Li Y, He L, et al. Prognostic nomogram for adenoid cystic carcinoma in different anatomic sites. Head Neck. 2021;43:48–59. doi:10.1002/hed.26443
23. Chen H, CT L, CQ H, et al. Nomogram based on nutritional and inflammatory indicators for survival prediction of small cell carcinoma of the esophagus. Nutrition. 2021;84:111086. doi:10.1016/j.nut.2020.111086
24. Zhang W, Fang M, Dong D, et al. Development and validation of a CT-based radiomic nomogram for preoperative prediction of early recurrence in advanced gastric cancer. Radiother Oncol. 2020;145:13–20. doi:10.1016/j.radonc.2019.11.023
25. VP B, Gonen M, JJ S, et al. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16:e173–80. doi:10.1016/S1470-2045(14)71116-7
26. XY X, HG D, WG L, et al. Chinese guidelines on management of hepatic encephalopathy in cirrhosis. World J Gastroenterol. 2019;25:5403. doi:10.3748/wjg.v25.i36.5403
27. Xiang S, Tan J, Tan C, et al. Establishment and Validation of a Non-Invasive Diagnostic Nomogram to Identify Spontaneous Bacterial Peritonitis in Patients With Decompensated Cirrhosis. Front Med Lausanne. 2021;8:797363. doi:10.3389/fmed.2021.797363
28. RR W, HQ G, YY W, et al. Development and Validation of a Prognostic Model for One-year Survival of Cirrhosis Patients with First-ever Spontaneous Bacterial Peritonitis. J Clin Transl Hepatol. 2021;9:647–654. doi:10.14218/JCTH.2021.00031
29. Lafcı D, Kaşikçi M. The effect of aroma massage on constipation in elderly individuals. Exp Gerontol. 2023;171:112023. doi:10.1016/j.exger.2022.112023
30. Barberio B, Judge C, EV S, et al. Global prevalence of functional constipation according to the Rome criteria: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:638–648. doi:10.1016/S2468-1253(21)00111-4
31. NC S, AC F. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. Am J Gastroenterol. 2011;106:1582. doi:10.1038/ajg.2011.164
32. Sumida K, MZ M, PK P, et al. Constipation and risk of death and cardiovascular events. Atherosclerosis. 2019;281:114–120. doi:10.1016/j.atherosclerosis.2018.12.021
33. Xu J, Ma R, LF C, et al. Effects of probiotic therapy on hepatic encephalopathy in patients with liver cirrhosis: an updated meta-analysis of six randomized controlled trials. Hepatobiliary Pancreat Dis Int. 2014;13:354–360. doi:10.1016/S1499-3872(14)60280-0
34. Gantzel RH, Aagaard NK, Vilstrup H, et al. Development and validation of the Cirrhotic Ascites Severity model-A patient-reported outcome-based model to predict 1-year mortality. Hepatol Commun. 2022;6:3175–3185. doi:10.1002/hep4.2065
35. EB T, ND P. Diagnosis and Management of Cirrhosis and Its Complications: a Review. JAMA. 2023;329:1589–1602. doi:10.1001/jama.2023.5997
36. Tonon M, Piano S, CG G, et al. Outcomes and Mortality of Grade 1 Ascites and Recurrent Ascites in Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2021;19:358–66.e8. doi:10.1016/j.cgh.2020.03.065
37. Zhang Q, Niu S, Yang L, et al. A novel prognostic model for predicting the risk of first variceal hemorrhage in patients with HBV-related cirrhosis. Front Cell Infect Microbiol. 2023;13:1062172. doi:10.3389/fcimb.2023.1062172
38. Jamil Z, Perveen S, Khalid S, et al. Child-Pugh Score, MELD Score and Glasgow Blatchford Score to Predict the In-Hospital Outcome of Portal Hypertensive Patients Presenting with Upper Gastrointestinal Bleeding: an Experience from Tertiary Healthcare System. J Clin Med. 2022;12:11. doi:10.3390/jcm12010011
39. MG K, Mahmud N. Assessing the risk of surgery in patients with cirrhosis. Hepatol Commun. 2023;7.
40. Tandon P, JG A, Keough A, et al. Risk of Bacterial Infection in Patients With Cirrhosis and Acute Variceal Hemorrhage, Based on Child-Pugh Class, and Effects of Antibiotics. Clin Gastroenterol Hepatol. 2015;13:1189–1196. doi:10.1016/j.cgh.2014.11.019
41. Peng Y, Wei Q, Liu Y, et al. Prediction and Risk Factors for Prognosis of Cirrhotic Patients with Hepatic Encephalopathy. Gastroenterol Res Pract. 2021;2021:5623601. doi:10.1155/2021/5623601
42. Hurlimann J, GJ T, GM H. The liver as the site of C-reactive protein formation. J Exp Med. 1966;123:365–378. doi:10.1084/jem.123.2.365
43. WB P, KD L, CS L, et al. Production of C-reactive protein in Escherichia coli-infected patients with liver dysfunction due to liver cirrhosis. Diagn Microbiol Infect Dis. 2005;51:227–230. doi:10.1016/j.diagmicrobio.2004.11.014
44. Mackenzie I, Woodhouse J. C-reactive protein concentrations during bacteraemia: a comparison between patients with and without liver dysfunction. Intensive Care Med. 2006;32:1344–1351. doi:10.1007/s00134-006-0251-1
45. Cho Y, SY P, JH L, et al. High-sensitivity C-reactive protein level is an independent predictor of poor prognosis in cirrhotic patients with spontaneous bacterial peritonitis. J Clin Gastroenterol. 2014;48:444–449. doi:10.1097/MCG.0b013e3182a6cdef
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
An Easy-to-Use Nomogram Based on SII and SIRI to Predict in-Hospital Mortality Risk in Elderly Patients with Acute Myocardial Infarction
Chen Y, Xie K, Han Y, Xu Q, Zhao X
Journal of Inflammation Research 2023, 16:4061-4071
Published Date: 13 September 2023
Development and Internal Validation of a Nomogram for Predicting Postoperative Cardiac Events in Elderly Hip Fracture Patients
Liu Y, Liu H, Zhang F
Clinical Interventions in Aging 2023, 18:2063-2078
Published Date: 12 December 2023
A Novel Nomogram Developed Based on Preoperative Immune Inflammation-Related Indicators for the Prediction of Postoperative Delirium Risk in Elderly Hip Fracture Cases: A Single-Center Retrospective Cohort Study
Chen X, Fan Y, Tu H, Chen J
Journal of Inflammation Research 2024, 17:7155-7169
Published Date: 9 October 2024


