Back to Journals » Journal of Inflammation Research » Volume 17
Predictive Value of the Platelet-Lymphocyte Ratio for Intravesical Recurrence After Radical Nephroureterectomy: A Retrospective Study
Authors Zhao Y, Ma Y, Zhang W , Jiao B, Chen Y, Li G, Zhang X
Received 18 June 2024
Accepted for publication 27 November 2024
Published 11 December 2024 Volume 2024:17 Pages 10819—10833
DOI https://doi.org/10.2147/JIR.S483242
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tara Strutt
Yu Zhao,1,* Yina Ma,1,* Wenhui Zhang,2 Binbin Jiao,1 Yuanhao Chen,1 Gao Li,1 Xin Zhang1
1Department of Urology Surgery, Beijing Chao-Yang Hospital Affiliated to Capital Medical University, Beijing, People’s Republic of China; 2Department of Hepatobiliary Surgery, Beijing Chao-Yang Hospital Affiliated to Capital Medical University, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xin Zhang, Email [email protected]
Objective: The aim of this study was to evaluate the impact of preoperative platelet lymphocyte ratio (PLR) on the prognosis of patients after radical nephrectomy (RNU).
Methods: We retrospectively analyzed clinical data from 226 patients without a history of bladder cancer who underwent RNU at Beijing Chaoyang Hospital, Capital Medical University between January 2009 and December 2020. Patients were stratified into two groups (A low PLR group (n = 174) and a high PLR group (PLR ≥ 169.4) based on an optimal PLR threshold (PLR=169.4). The predictive accuracy of inflammatory biomarkers was assessed using receiver operating characteristic curves. Univariate and multivariate Cox proportional risk analyses were used to estimate the effect of PLR on intravesical recurrence-free survival (IVRFS), recurrence-free survival (RFS), and overall survival (OS). The effect of PLR on IVRFS, RFS and OS was further examined using Kaplan-Meier survival curve analysis.
Results: The study cohort comprised 226 individuals with a mean age of 67.2 ± 9.8, 113 (50%) males and 113 (50%) females, 68 (30.1%) low-grade tumors and 158 (69.9%) high-grade tumors. In this study, 81 patients (36.7%) relapsed and 73 patients (32.3%) died. The area under the curve for PLR prediction of IVRFS was 0.603, superior to other inflammatory biomarkers. Multivariate analysis showed that PLR > 169.4 independently increased the risk of IVR after RNU, resulting in lower IVRFS [2.028 (1.014– 4.057), P = 0.046], RFS [1.900 (1.168– 3.090), P = 0.010], and OS [1.866 (1.099– 3.167), P = 0.021]. In addition, survival analysis showed lower IVRFS [8.815 (62.722– 97.278), P = 0.007], RFS [12.084 (44.315– 91.685), P = 0.003] and OS RFS [10.165 (62.077– 101.923), P = 0.005] in the low PLR group.
Conclusion: Elevated preoperative PLR is strongly associated with prognosis in patients with upper urothelial carcinoma (UTUC) after RNU without a history of bladder cancer.
Keywords: platelet-lymphocyte ratio, upper urinary tract uroepithelial carcinoma, intravesical recurrence, radical nephroureterectomy
Introduction
Upper urinary tract uroepithelial carcinoma (UTUC) include renal pelvic and ureteral carcinoma. These tumors fall under the category of urothelial carcinoma together with bladder cancer. UTUC accounts for 5–10% of urothelial carcinomas, which is a rare but highly aggressive malignancy.1,2 Radical nephroureterectomy (RNU) combined with bladder cuff resection is the standard of care for patients with UTUC.3 Once muscular layer infiltration is present, the prognosis of upper urinary tract urothelial carcinoma is usually poor.4 Early-stage tumors often have no clinical symptoms, and about 2/3 of patients have progressive tumors at the time of diagnosis, so the treatment effect and prognosis are poor.3 As it is difficult to accurately determine the presence of muscular infiltration in the imaging assessment of UTUC, UTUC cannot be evaluated for basal infiltration by diagnostic electrocautery as in the case of bladder tumors.5 Therefore, the clinical prognostic assessment of UTUC is a difficulty in its clinical management. The postoperative period after UTUC is prone to recurrence of covered uroepithelial organs and tissues, mainly bladder recurrence, but also contralateral UTUC recurrence.6 Bladder tumor recurrence occurs in 22% to 47% of patients.7,8 Many studies have focused on preoperative, intraoperative, and postoperative prognostic factors in patients with UTUC after RNU.9–12 Preoperative prognostic factors include a variety of variables such as patient age, smoking, tumor lesion, tumor location, grading, hydronephrosis, and inflammation-related markers.11 These markers include neutrophil-to-lymphocyte ratio (NLR), systemic immune-inflammation index (SII), systemic inflammation response index (SIRI), platelet-to-lymphocyte ratio (PLR), lymphocyte-to-monocyte ratio (LMR), neutrophil-to-monocyte ratio (NMR) and etc. In addition, preoperative ureteroscopy combined with endoscopic biopsy has been identified as a risk factor for intravesical recurrence (IVR). If bladder tumor recurrence occurs during the follow-up of UTUC patients, patients will need to undergo one or even more transurethral bladder tumor electrodes, and some patients will even need to be treated with radical cystectomy.3 This seriously affects the quality of survival of patients and can also cause tremendous financial pressure on patients. Therefore, it is particularly important to analyze the factors associated with bladder carcinogenesis after UTUC.13,14
Inflammation plays a contributing role in the initiation and advancement of various cancers.15 Previous studies have shown that inflammation biomarkers, including NLR, SII, SIRI, PLR, MLR, and NMR, are associated with worse urologic outcomes.16–20 They have been identified as an independent prognostic indicator for a number of cancer types, including gastric, colorectal, hepatocellular, and lung cancers.21–24 However, no studies have reported the prognostic value of PLR for IVR after RNU without a history of bladder cancer. These survival-related markers can be explained by the relationship of cancer to platelet, neutrophil, and lymphocyte levels.25 Platelets are reported to be dangerous allies of cancer cells and play a close role in several processes of cancer metastasis.26 Once tumor cells enter the bloodstream, they immediately activate platelets, creating a permissive microenvironment. Platelets protect tumor cells from shear forces and natural killer cells (NK cells) and secrete chemokines to recruit bone marrow cells. This results in tumor cell platelet plugs stopping at the vessel wall. Platelet-derived growth factors then confer a mesenchymal-like phenotype on the tumor cells, opening the capillary endothelium and accelerating extravasation from distant organs. Ultimately, platelet-secreted growth factors stimulate tumor cell proliferation toward micro metastatic foci.27 On the contrary, lymphocytes play an important role in cellular and humoral anti-tumor immune responses. Activated and proliferating lymphocytes play a role in cytotoxic cell death and inhibition of tumor cell proliferation and migration by secreting cytokines such as interferon gamma (IFN-γ) and tumor necrosis factor alpha (TNF-α). Therefore, low lymphocyte counts may reflect impaired host immune surveillance, which is an unfavorable factor in the clinical prognosis of tumor patients.16,28 Considering these mechanisms, higher PLR representing higher platelet and neutrophil counts and lower lymphocytes may predict poorer survival. Therefore, this study was aimed to evaluate the predictive value of PLR for intravesical recurrence-free survival (IVRFS), recurrence-free survival (RFS) and overall survival (OS) in patients without a history of bladder cancer after RNU.
Methods
Patient Selection
This retrospective study was approved by the Institutional Research Ethics Committee of Beijing Chao-Yang Hospital. Informed consent was obtained from all eligible participants in advance. We retrospectively collected the information of patients diagnosed with UTUC who received RNU treatment at our hospital from January 2009 to December 2020, and all patients’ details have been de-identified. We included the patients who meet the following criteria: (1) patients with UTUC confirmed pathologically; (2) patients with primary tumors of uroepithelial origin; (3) patients with unilateral onset, and (4) patients subject to RNU combined with cystic sleeve resection. Patients were excluded according to the following criteria: (1) patients with bilateral UTUC; (2) patients subject to no RNU combined with cystectomy; (3) patients with metastatic uroepithelial carcinoma; (4) patients with a previous history of bladder cancer and other cancers; and (5) patients with any preoperative treatment. Figure 1 shows the flow chart for inclusion and exclusion of patients.
 |
Figure 1 The flow chart for inclusion and exclusion of patients. Abbreviations: UTUC, Upper urothelial carcinoma. RNU, radical nephrectomy. |
Definitions of Inflammatory Indexes
In this study, several inflammatory biomarkers were defined and calculated based on the patients’ routine blood results. NLR was calculated by dividing the neutrophil count by the lymphocyte count. PLR was calculated by dividing the platelet count by the lymphocyte count. LMR was calculated by dividing the lymphocyte count by the monocyte count. NMR was calculated by dividing the neutrophil count by the monocyte count. SII was calculated by multiplying the PLR by the neutrophil count. SIRI is calculated by multiplying NLR by neutrophil count. Venous blood was collected from all patients within 24 hours before surgery for complete blood count analysis.
Follow-Up
Follow-up data on all enrolled patients were collected by various means, including telephone interviews and outpatient or inpatient observation until March 2023 or death. Data including the patient’s preoperative gender, age, height, weight, tumor location, history of hypertension, history of diabetes, uropathology, hydronephrosis, tumor origin, single or multiple, tumor size, and blood counts (including platelets and lymphocytes) were collected. Postoperative data including tumor TNM stage, tumor grade, infiltration, nerve invasion, vascular invasion, and postoperative radiotherapy and chemotherapy were collected. Body mass index (BMI) = weight (kg)/height² (m). Follow-up data included whether the tumor recurred, the site of recurrence, the time from surgery to recurrence, whether the patient died, and the time from surgery to death. Monitoring was done every 3 months in the first postoperative year, every 6 months in the second year, and annually thereafter. Follow-up information included blood tests, cystoscopy, urinary ultrasound, chest and abdominal computed tomography (CT), urine exfoliative cytology, and urography. If clinically indicated, selective bone scan, positron emission tomography/computed tomography (PET/CT) or magnetic resonance imaging (MRI) were performed. IVRFS was defined as the time from the date of RNU to the date of the first IVR according to cystoscopic examination. Tumor staging was defined pathologically according to the American Joint Committee on Cancer (AJCC) Tumor,29 Lymph Node, Metastasis (TNM) Classification (8th edition).30 Tumor grading was recorded according to the patient’s postoperative pathology report, that is, based on the 2004 World Health Organization (WHO) classification.31 When the high-grade component is less than 5%, it is low-grade uroepithelial cancer, and when the high-grade component is greater than or equal to 5%, it is high-grade uroepithelial cancer.31 The location of the tumor was marked according to the location of the dominant tumor. Positive urine cytology was defined as the presence of tumor cells or abnormal cells in the preoperative specimen. Conversely, negative urine cytology was defined as an evaluation that produced a negative result. Evaluation of all histopathologic sections was performed by a senior pathologist. The optimal PLR cutoff value was defined by creating a time-dependent receiver operating characteristic (ROC) curve with IVRFS as the endpoint to yield the highest Youden index value. Patients were stratified into two groups (A low PLR group (PLR < 169.4, n = 174) and a high PLR group (SIRI ≥ 169.4, n = 52) according to the optimal cutoff. RFS was defined as the time between the date of treatment and the date of recurrence. OS was defined as the time between the date of treatment and the date of death or the date of last follow-up.
Statistical Analysis
Given the retrospective nature of the study, the following measures were taken to minimize bias in data collection and analysis: strict inclusion and exclusion criteria were established and data collectors were trained to ensure consistency and accuracy; two researchers collected data and followed up patients to ensure data accuracy; and in this study we included variables that were unstable at baseline (eg, BMI) in the multifactorial analysis, although its univariate analysis p > 0.05.
The overall study population was divided into two separate PLR groups according to the optimal cutoff. We compared baseline differences between groups. Then, using IVRFS, RFS and OS as an outcome indicator, we screened for independent influences on IVRFS, RFS and OS by analyzing univariate and multivariate cox proportional risk regression models (variables with P < 0.05 in the univariate cox regression, PLR, and BMI that were not smooth at baseline were included in the multivariate analysis), and analyzed the influence of PLR on IVRFS, RFS and OS by using the Kaplan-Meier plotting of survival curves. In addition, we divided the included patients into two groups according to gender (male vs female) tumor grade (low-grade vs high grade) for the above analysis.
Depending on their distribution, continuous variables will be expressed as mean and standard deviation or median and interquartile range. Student ‘s t-test or Mann–Whitney U-test will be used for continuous variables and χ2-test or Fisher exact test for categorical variables. Normality of continuous variables will be assessed using the Kolmogorov–Smirnov test. ROC was used to determine the optimal threshold for the prognosis of UTUC patients after RNU. Youden index = sensitivity+specificity-1. The point corresponding to the maximum Youden index is the optimal threshold. We used Cox proportional risk regression model for univariate and multivariate analyses (Variables with P < 0.05 in univariate analysis and unstable baseline were included in multivariate analysis), and Kaplan-Meier (K-M) for plotting survival curves. P < 0.05 was considered a statistically significant difference. GraphPad Prism 8.0, R software (Version 4.2.2) and IBM SPSS Statistics (Version 24) were utilized to complete all statistical analyses and figures.
Results
Characteristics of patients and disease
Monitoring was done every 3 months in the first year after surgery, every 6 months in the second year, and annually thereafter until March 2023 or the patient’s death. A cohort of 226 patients who met the specified inclusion and exclusion criteria were included in the study, including 113 (50%) males and 113 (50%) females, 68 (30.1%) low-grade tumors and 158 (69.9%) high-grade tumors. Ages ranged from 43–88 years with a mean age of (67.2 ±9.8) years. 174 (77.0%) cases in the PLR≤169.4 group, and 52 (23.0%) cases in the PLR>169.4 group. The median survival time was 106 months. By the end of follow-up, a total of 73 (32.3%) patients had died. The clinical characteristics of all patients were summarized in Table 1. There was no significant difference in gender, age, pathologic T stage, pathologic N stage, location, hypertension, diabetes, uropathology, hydronephrosis, tumor origin, multifocality, tumor grade, invasion, nerve invasion, vascular invasion, radiotherapy or chemotherapy and tumor size (P ≥ 0.05), while there was a significant difference in BMI (P = 0.012). The clinical characteristics of males and females were summarized in Table S1. In males, there was no significant difference in gender, age, pathologic T stage, location, hypertension, diabetes, uropathology, hydronephrosis, tumor origin, multifocality, tumor grade, invasion, nerve invasion, vascular invasion, radiotherapy or chemotherapy and tumor size (P ≥ 0.05), while there was a significant difference in pathologic N stage (P = 0.005) and BMI (P = 0.041). In females, there was no significant difference in gender, age, pathologic T stage, pathologic N stage, location, hypertension, diabetes, BMI, uropathology, hydronephrosis, tumor origin, multifocality, tumor grade, invasion, nerve invasion, vascular invasion, radiotherapy or chemotherapy and tumor size (P ≥ 0.05). In addition, we divided the patients into a low-grade tumor group and a high-grade tumor group based on their pathology, and the baseline conditions of the two groups were shown in Table S2. In low-grade group, there was no significant difference in gender, age, pathologic T stage, pathologic N stage, location, hypertension, diabetes, BMI, uropathology, hydronephrosis, tumor origin, multifocality, tumor grade, invasion, nerve invasion, vascular invasion, radiotherapy or chemotherapy and tumor size (P ≥ 0.05). In high-grade group, there was no significant difference in gender, age, pathologic T stage, pathologic N stage, location, hypertension, diabetes, uropathology, hydronephrosis, tumor origin, multifocality, tumor grade, invasion, nerve invasion, vascular invasion, radiotherapy or chemotherapy and tumor size (P ≥ 0.05), while there was a significant difference in BMI (P = 0.004).
 |
Table 1 Clinical and Pathological Characteristics of Patients |
Exploring the Influencing Factors of IVRFS, PFS and OS Using Univariate and Multivariate Cox Regression
ROC curves were used to establish the relationship between preoperative inflammatory biomarkers and prognosis in patients after RNU (Figure 2). PLR corresponded to an area under the curve (AUC) of 0.603 (P = 0.033), LMR corresponded to an AUC of 0.533 (P = 0.499), SIRI corresponded to an AUC of 0.524 (P = 0.624), SII corresponded to an AUC of 0.521 (P = 0.668), NLR corresponded to an AUC of 0.510 (P = 0.837), NMR corresponded to an AUC of 0.506 (P = 0.909). In summary, PLR has the greatest and meaningful diagnostic efficacy.
For All Patients
The results of univariate Cox regression results suggested that pathologic T stage [2.906(1.087–7.771), P = 0.034], pathologic N stage [3.704(1.320–10.396), P = 0.013], tumor origin [7.432(1.011–54.617), P = 0.049] and PLR [2.274(1.233–4.193), P = 0.009] were associated with IVRFS (Table 2); pathologic T stage [3.191(1.536–6.631), P = 0.002; 7.373(3.095–17.569), P<0.001], pathologic N stage [3.385(1.466–7.821), P = 0.004], nerve invasion [3.324(1.792–6.168), P<0.001], vascular invasion[2.138(1.323–3.454), P = 0.002], tumor size [1.677(1.083–2.596), P = 0.020] and PLR [1.926(1.233–3.009), P = 0.004] were associated with RFS (Table 3), and age [2.442(1.529–3.899), P<0.001], pathologic T stage[4.646(1.562–13.815), P = 0.006; 6.373(2.247–18.078), P<0.001; 18.183(5.953–55.539), P<0.001], pathologic N stage[4.281(1.842–9.948), P = 0.001], invasion[2.937(1.461–5.905), P = 0.002], nerve invasion[5.339(2.883–9.886), P<0.001], vascular invasion[2.842(1.736–4.651), P<0.001), tumor size[1.645(1.037–2.610), P = 0.034] and PLR[1.933(1.208–3.094), P = 0.006] were associated with OS (Table 4). Multivariate Cox regression results suggested that tumor origin [3.008(1.535–5.895), P = 0.001] and PLR [2.028(1.014–4.057), P = 0.046] were associated with IVRFS(Table 2), pathologic T stage [2.909(1.348–6.276), P = 0.006; 5.341(1.603–17.791), P = 0.006] and PLR [1.900(1.168–3.090), P = 0.010] were associated with RFS (Table 3), and age [2.037(1.236–3.357), P = 0.005], pathologic T stage[7.1221(701–29.816), P = 0.007; 8.161(2.017–33.014), P = 0.003; 12.913(2.319–71.899), P = 0.003], nerve invasion [2.473(1.134–5.394), P = 0.023] and PLR [1.866(1.099–3.167), P = 0.021] were associated with OS (Table 4).
 |
Table 2 Univariate and Multivariate Cox Regression to Explore the Influence of Intravesical Recurrence-Free Survival for All Patients |
 |
Table 3 Univariate and Multivariate Cox Regression to Explore the Influence of Recurrence-Free Survival for All Patients |
 |
Table 4 Univariate and Multivariate Cox Regression to Explore the Influence of Overall Survival for All Patients |
Grouped by Gender
For males, the results of univariate Cox regression results suggested that pathologic N stage [29.326(3.263–263.590), P = 0.003], tumor origin [2.393(1.074–5.330), P = 0.033], tumor size [2.241(1.063–4.724), P = 0.034] and PLR [2.799(1.289–6.076), P = 0.009] were associated with IVRFS; multivariate Cox regression results suggested that pathologic N stage [19.561(1.861–205.620), P = 0.013], tumor origin[2.565(1.112–5.913), P = 0.027], tumor size [2.573(1.156–5.726), P = 0.021] and PLR [2.546(1.034–6.269), P = 0.042] were associated with IVRFS (Table S3). For females, the results of univariate Cox regression suggested that diabetes [3.188(1.228–8.274), P = 0.017] was associated with IVRFS; multivariate Cox regression results suggested that diabetes [3.372(1.259–8.509), P = 0.015] was associated with IVRFS (Table S4).
Grouped by Tumor Grade
In the low-grade tumor group, the results of univariate Cox regression suggested that pathologic N stage [9.440(1.149–77.582), P = 0.037], tumor origin [3.721(1.288–10.754), P = 0.015], tumor size [3.984(1.437–11.047), P = 0.008] and PLR [3.442(1.295–9.150), P = 0.013] were associated with IVRFS; multivariate Cox regression results suggested that pathologic N stage [21.727(1895–249.077), P = 0.013], tumor origin [4.713(1.445–15.372), P = 0.010], tumor size [6.126(1.860–20.176), P = 0.003] and PLR [3.586(1.172–10.978), P = 0.025] were associated with IVRFS (Table S5). In the high-grade tumor group, the results of univariate Cox regression suggested that pathologic T stage [4.631(1.054–20.353), P = 0.042] and diabetes [2.394(1.140–5.027), P = 0.021] were associated with IVRFS; multivariate Cox regression results suggested that diabetes [2.267(1.066–4.820), P = 0.033] was associated with IVRFS (Table S6).
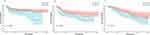
Survival Analysis
We plotted survival curves for the effect of PLR on IVRFS, RFS and OS (Figure 3). In addition, we plotted survival curves for the effect of PLR on IVRFS in males, females, low-grade tumor group and high-grade tumor group, respectively (Figure 4). The K-M survival curves showed that for all patients, IVRFS was significantly higher in patients with PLR ≤169.4 compared to those with PLR >169.4 (P = 0.007), RFS was significantly higher in patients with PLR ≤169.4 compared to those with PLR >169.4 (P = 0.003), and OS was significantly higher in patients with PLR ≤169.4 compared to those with PLR >169.4 (P = 0.005); for male patients, IVRFS was significantly higher in patients with PLR ≤169.4 compared to those with PLR >169.4 (P = 0.006); however, the difference was not statistically significant for female patients (P = 0.229); for the low-grade tumor group, IVRFS was significantly higher in patients with PLR ≤169.4 compared to those with PLR >169.4 (P = 0.008); however, the difference was not statistically significant for female patients (P = 0.260); however, the difference was not statistically significant for female patients (P = 0.153).
Discussion
Our study demonstrated that high PLR was a significant unfavorable prognostic determinant of IVRFS in UTUC patients after RNU, the finding that held true in men and was not statistically significant in women, and held true in the low-grade group and was not statistically significant in the high-grade group. Chronic inflammation caused by smoking and smoke exposure can lead to an excessive increase in neutrophils (neutrophils are the most abundant type of white blood cell in the body and are the body’s rapid response force to fight infections), which, along with an increase in neutrophils, leaves the body susceptible to infections and awakens dormant cancer cells, which can lead to the recurrence of cancer.32 We believe that this difference in the statistical results between men and women may be due mainly to the fact that the variable of smoking was not included in the basic information statistics. Of course, the small sample size is also an important factor in this discrepancy. As we all know, tumor cells of patients with low-grade tumors grow slower, have a low degree of malignancy, and have a low likelihood of recurrence, while those of patients with high-grade tumors grow faster, have a high degree of malignancy, are more invasive, have a high likelihood of recurrence, and are prone to spread to other parts of the body.29,33,34 The differences in our findings between different tumor grades may result from differences in tumor aggressiveness. Low-grade tumors have low invasiveness, and when the PLR is high, it reflects a heavy inflammatory response of the body, and a high inflammatory state promotes the aggressiveness of the tumor. High-grade tumors are inherently highly aggressive and are prone to recurrence and metastasis regardless of the body’s inflammatory state.
Inflammation and immune response are important components of tumorigenesis, proliferation, invasion, and metastasis.35 Inflammation-related indices such as SII, NLR, PLR, LMR, etc., can reflect systemic inflammatory response and have prognostic predictive value in various malignancies.36–39 Inflammation, infection and oncogene activation lead to the activation of transcription factors in the tumor and stroma, which in turn leads to the production of chemokines, cytokines and prostaglandins and induces the recruitment of inflammatory cells.40 Secretion of chemokines and cytokines in the circulation mediates alterations at distal sites, leading to secretion of tumor-derived cytokines and growth factors into the somatic circulation mediating alterations at distal sites.15 Tumor cells and tumor ecological niches regulate the development, maturation, and release of bone marrow neutrophils through the production of growth factors (eg, G-CSF and GM-CSF) and inflammatory cytokines, including IL-6, IL-1β, and IL-17 (Neutrophil Diversity and Plasticity in Tumor Progression and Therapy), which result in peripheral neutrophilia.41,42 Platelets play an important role in tumor progression. Secretion of IL-6 by tumor cells stimulates the production of thrombopoietin (TPO), which leads to megakaryopoiesis and platelet production and results in thrombocytosis and hypercoagulability known as Trousseau syndrome.43,44 Platelets can accelerate tumor progression by interacting directly or indirectly with tumor cells by promoting tumor cell proliferation, resisting cell death, inducing angiogenesis, activating invasion, establishing pre-metastatic microhabitats, and evading immune detection.45 Elevated platelet counts have been reported to be associated with an increased risk of cancer at multiple sites.46 Many studies have reported an association between elevated platelet counts and reduced disease-specific survival in various types of cancer.47 In the context of tumor immune surveillance and resistance, lymphocytes play a crucial role in hindering tumor cell proliferation and growth through cytotoxic cell death. Conversely, the presence of T lymphocytes in the tumor microenvironment has been consistently associated with improved prognosis, highlighting their significant anti-tumor function.48,49 During cancer immune surveillance and resistance, lymphocytes inhibit tumor cell proliferation and growth through cytotoxic cell death. Lymphocytes have important anti-tumor functions, and infiltration of the tumor microenvironment by T lymphocytes is known to correlate with a better prognosis.48,49 CD8+ T cells are directly involved in tumor cell lysis and cytotoxic cytokine production.CD4+ Th1 cells assist cytotoxic T lymphocytes and influence tumor progression through the production of cytokines (eg, IFN-γ), and Th17 cells and Treg cells play a role in the anti-tumor process by activating cytotoxic lymphocytes or suppressing inflammation.50 In conclusion, neutrophils, platelets and lymphocytes are important components of inflammation and immunity associated with cancer. In UTUC, multiple systemic inflammation and immune-related indices have been established based on these factors to predict the prognosis of patients after RNU, including PLR, NLR, LMR, and SII.12,51–53 Elevated platelets and decreased lymphocytes lead to an elevated PLR. Our study demonstrated that high PLR was a significant unfavorable prognostic determinant of IVRFS, RFS and OS in UTUC patients after RNU. This suggests that changes in PLR reflect alterations in the inflammatory state of the body and thus can provide predictive value for patient prognosis.
Although certain factors such as tumor stage, tumor grading, and surgical margins were associated with poorer survival outcomes, these factors are usually assessed postoperatively using pathology specimens. In contrast, blood-based biomarkers of inflammation can be easily obtained before surgery and help urologists make the best clinical decisions for individual patients.25,54,55
For patients with UTUC after RNU, if bladder tumor recurrence is detected, one or even more transurethral bladder tumor electrodes will be required, and some patients may even need to undergo radical cystectomy. This seriously affects the quality of patients’ survival, and also puts tremendous financial pressure on patients, and may even significantly shorten survival time. Therefore, it is essential to predict the likelihood of recurrence in the bladder in advance so as to intervene in advance. Zhenkai Luo et al study shows PLR as an independent risk factor for IVR.56 This study likewise did not take into account the origin of the recurrent bladder tumors. However, in this study, the investigators did not exclude patients with a history of bladder cancer, so it was not possible to determine whether it was a recurrence of the bladder tumor or a recurrence of UTUC in the bladder. In this study, we excluded patients with a history of bladder cancer. A study from Kaohsiung Medical University suggested that the NLR, PLR, and SII were independent predictive factors for both metastasis-free survival (MFS) and cancer-specific survival (CSS) in UTUC patients, but among the factors, only elevated SII can predict bladder recurrence.25 The study excluded patients with a history of bladder cancer, but did not demonstrate the predictive value of PLR for recurrence in the bladder.
This study has several strengths. First, the present study has the innovative finding that high levels of PLR values correlate with intravesical recurrence after RNU only when the primary tumor pathology is low-grade; this correlation does not exist when the primary tumor pathology is high-grade. Second, in this study, patients with a history of bladder cancer were excluded and were able to rule out the effect of bladder tumor recurrence. Finally, compared with other risk factors, PLR could be obtained before surgery, thus rationally guiding further treatment.
PLR, a simple, cost-effective and easily accessible indicator of inflammation, can reflect the risk of recurrence in the bladder in patients with low-grade UTUC. Low-grade UTUC is usually of longer duration and less malignant, but recurrence may still occur. High PLR levels may suggest a higher risk of intravesical recurrence in these patients, and therefore can be used as an adjunctive judgment tool to help clinicians better assess a patient’s risk of recurrence. For patients with low-grade UTUC, a high PLR value may imply that the patient’s immune system is in a higher state of inflammation, suggesting that closer follow-up or targeted adjustments to the treatment regimen may be needed. For example, such patients may require more surveillance, imaging and urine cytology testing, and even consideration of more aggressive adjuvant therapy, such as local immunotherapy, when managing follow-up after RNU. In patients with high-grade bladder cancer, the tumor itself is more malignant, and its risk of recurrence is usually strongly influenced by the aggressiveness and degree of differentiation of the tumor cells themselves, while the relationship with the immune system or inflammatory response may be relatively weak. Therefore, PLR values are of low prognostic significance in such patients, emphasizing that patients with high-grade tumor should pay more attention to the treatment of the tumor itself and the mechanism of recurrence, rather than relying solely on PLR values to assess the risk of recurrence. PLR values in patients with low-grade tumor were associated with intravesical recurrence, suggesting that immune response may play a role in the recurrence process of low-grade tumors. High PLR values may be a reflection of the inflammatory response in the tumor microenvironment, further supporting the potential role of the immune microenvironment in bladder carcinogenesis and recurrence. Therefore, interventions targeting PLR, an indicator of immune inflammation, may become a new research direction in future therapy of UTUC.
However, a little of limitations of this study should be recognized. First, it is important to note that this study is retrospective and was conducted within a single center. This study may suffer from selection bias, information bias and recall bias, which may lead to inaccurate data and an unrepresentative sample. The quality and completeness of the data may be limited by the difficulty in clarifying causality due to the inability to control for confounding factors. Therefore, the findings need to be validated by future multicenter studies with larger samples. Secondly, smoking is known to be a risk factor for uroepithelial carcinoma, and the weakness of this study to include a history of smoking in the data collection could have been a confounding factor. Finally, The cutoff values for this study were determined based on the ROC curves of the data from this study, and other studies have determined their own cutoff values based on the data from their studies. This resulted in different cutoff values being obtained for different study data. Therefore, it is crucial to develop a more universally applicable threshold for PLR.
In conclusion, the findings of this study provide new ideas for recurrence risk assessment in UTUC patients after RNU, especially in patients with low-grade tumors, where the PLR value, as a simple hematological indicator, may become an important tool to assist in diagnosis and prognostic assessment. However, for patients with high-grade tumors, the application value of PLR is low, emphasizing the decisive role of the tumor’s own pathological characteristics in UTUC recurrence. The effect of PLR in association with other immune markers should be further investigated in the future to achieve more precise and individualized treatment.
Conclusion
Our study showed that high preoperative PLR levels were associated with shorter IVRFS, RFS, and OS in UTUC patients after RNU. In particular, high preoperative PLR levels shortened IVRFS in UTUC patients after RNU only in men and patients with low-grade tumors, but not in women and patients with high-grade tumors. This suggests that PLR has some predictive significance for the prognosis of UTUC patients after RNU, which may not be applicable to all populations.
Data Sharing Statement
The data that support the findings of this study are available from the Beijing Chao-Yang hospital. Further information is available from the corresponding author upon request.
Ethics Statement
The study complies with the Declaration of Helsinki and have obtained ethics approval from Beijing Chao-Yang Hospital Affiliated to Capital Medical University.
Acknowledgment
We would like to thank the patients who provided data for our study.
Author Contributions
YZ and YM designed the study and wrote the manuscript. YZ and WZ prepared the figures. BJ collected the data. WZ and YC designed the study. GL revised the manuscript. XZ supervised the study. All authors contributed to the article and approved the submitted version. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Beijing Municipal Natural Science Foundation, Grant/Award Number: 7222073; Beijing Nova Program, Grant/Award Number: 20240484538.
Disclosure
The authors declare no competing interests in this work.
References
1. Zareba P, Rosenzweig B, Winer AG, Coleman JA. Association between lymph node yield and survival among patients undergoing radical nephroureterectomy for urothelial carcinoma of the upper tract. Cancer. 2017;123(10):1741–1750. doi:10.1002/cncr.30516
2. Takemura K, Kawai T, Sato Y, et al. Impact of Initial Computed Tomography Findings on Management of Atypical Urinary Cytology of the Upper Urinary Tract. Urol Int. 2021;105(7–8):619–623. doi:10.1159/000512978
3. Rouprêt M, Seisen T, Birtle AJ, et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2023 Update. Eur Urol. 2023;84(1):49–64. doi:10.1016/j.eururo.2023.03.013
4. Wang X, Yang G, Chai Y, et al. Decreased Preoperative Serum AGR as a Diagnostic Marker of Poor Prognosis after Radical Surgery of Upper Urinary Tract and Bladder Cancers from a Pooled Analysis of 9,002 Patients. Dis Markers. 2022;2022:6575605. doi:10.1155/2022/6575605
5. Tsikitas LA, Hopstone MD, Raman A, Duddalwar V. Imaging in Upper Tract Urothelial Carcinoma: a Review. Cancers (Basel). 2023;16(1):15. doi:10.3390/cancers16010015
6. Xylinas E, Kluth L, Passoni N, et al. Prediction of intravesical recurrence after radical nephroureterectomy: development of a clinical decision-making tool. Eur Urol. 2014;65(3):650–658. doi:10.1016/j.eururo.2013.09.003
7. Xylinas E, Rink M, Margulis V, Karakiewicz P, Novara G, Shariat SF. Multifocal carcinoma in situ of the upper tract is associated with high risk of bladder cancer recurrence. Eur Urol. 2012;61(5):1069–1070. doi:10.1016/j.eururo.2012.02.042
8. Seisen T, Granger B, Colin P, et al. A Systematic Review and Meta-analysis of Clinicopathologic Factors Linked to Intravesical Recurrence After Radical Nephroureterectomy to Treat Upper Tract Urothelial Carcinoma. Eur Urol. 2015;67(6):1122–1133. doi:10.1016/j.eururo.2014.11.035
9. Margulis V, Youssef RF, Karakiewicz PI, et al. Preoperative multivariable prognostic model for prediction of nonorgan confined urothelial carcinoma of the upper urinary tract. J Urol. 2010;184(2):453–458. doi:10.1016/j.juro.2010.03.142
10. Simsir A, Sarsik B, Cureklibatir I, Sen S, Gunaydin G, Cal C. Prognostic factors for upper urinary tract urothelial carcinomas: stage, grade, and smoking status. Int Urol Nephrol. 2011;43(4):1039–1045. doi:10.1007/s11255-011-9915-z
11. Lughezzani G, Burger M, Margulis V, et al. Prognostic factors in upper urinary tract urothelial carcinomas: a comprehensive review of the current literature. Eur Urol. 2012;62(1):100–114. doi:10.1016/j.eururo.2012.02.030
12. Mori K, Janisch F, Mostafaei H, et al. Prognostic value of preoperative blood-based biomarkers in upper tract urothelial carcinoma treated with nephroureterectomy: a systematic review and meta-analysis. Urol Oncol. 2020;38(5):315–333. doi:10.1016/j.urolonc.2020.01.015
13. Hu X, Xue Y, Zhu G. Clinical Characteristics and Current Status of Treatment for Recurrent Bladder Cancer after Surgeries on Upper Tract Urothelial Carcinoma. Diagnostics (Basel). 2023;13:1.
14. Mertens LS, Sharma V, Matin SF, et al. Bladder Recurrence Following Upper Tract Surgery for Urothelial Carcinoma: a Contemporary Review of Risk Factors and Management Strategies. Eur Urol Open Sci. 2023;49:60–66. doi:10.1016/j.euros.2023.01.004
15. Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493–503. doi:10.1016/S1470-2045(14)70263-3
16. Jan HC, Yang WH, Ou CH. Combination of the Preoperative Systemic Immune-Inflammation Index and Monocyte-Lymphocyte Ratio as a Novel Prognostic Factor in Patients with Upper-Tract Urothelial Carcinoma. Ann Surg Oncol. 2019;26(2):669–684. doi:10.1245/s10434-018-6942-3
17. Chen Z, Wang K, Lu H, et al. Systemic inflammation response index predicts prognosis in patients with clear cell renal cell carcinoma: a propensity score-matched analysis. Cancer Manag Res. 2019;11:909–919. doi:10.2147/CMAR.S186976
18. Vartolomei MD, Kimura S, Ferro M, et al. Is neutrophil-to-lymphocytes ratio a clinical relevant preoperative biomarker in upper tract urothelial carcinoma? A meta-analysis of 4385 patients. World J Urol. 2018;36(7):1019–1029. doi:10.1007/s00345-018-2235-5
19. Dalpiaz O, Krieger D, Ehrlich GC, et al. Validation of the Preoperative Platelet-to-Lymphocyte Ratio as a Prognostic Factor in a European Cohort of Patients with Upper Tract Urothelial Carcinoma. Urol Int. 2017;98(3):320–327. doi:10.1159/000452109
20. Luo Z, Yan Y, Jiao B, et al. Prognostic value of the systemic immune-inflammation index in patients with upper tract urothelial carcinoma after radical nephroureterectomy. World J Surg Oncol. 2023;21(1):337. doi:10.1186/s12957-023-03225-0
21. Zhaojun X, Xiaobin C, Juan A, et al. Correlation analysis between preoperative systemic immune inflammation index and prognosis of patients after radical gastric cancer surgery: based on propensity score matching method. World J Surg Oncol. 2022;20(1):1. doi:10.1186/s12957-021-02457-2
22. Shi H, Jiang Y, Cao H, Zhu H, Chen B, Ji W. Nomogram Based on Systemic Immune-Inflammation Index to Predict Overall Survival in Gastric Cancer Patients. Dis Markers. 2018;2018:1787424. doi:10.1155/2018/1787424
23. Chen JH, Zhai ET, Yuan YJ, et al. Systemic immune-inflammation index for predicting prognosis of colorectal cancer. World J Gastroenterol. 2017;23(34):6261–6272. doi:10.3748/wjg.v23.i34.6261
24. Tong YS, Tan J, Zhou XL, Song YQ, Song YJ. Systemic immune-inflammation index predicting chemoradiation resistance and poor outcome in patients with stage III non-small cell lung cancer. J Transl Med. 2017;15(1):221. doi:10.1186/s12967-017-1326-1
25. Chien TM, Li CC, Lu YM, Chou YH, Chang HW, Wu WJ. The Predictive Value of Systemic Immune-Inflammation Index on Bladder Recurrence on Upper Tract Urothelial Carcinoma Outcomes after Radical Nephroureterectomy. J Clin Med. 2021;11(1):10. doi:10.3390/jcm11010010
26. Li N. Platelets in cancer metastasis: to help the “villain” to do evil. Int J Cancer. 2016;138(9):2078–2087. doi:10.1002/ijc.29847
27. Schlesinger M. Role of platelets and platelet receptors in cancer metastasis. J Hematol Oncol. 2018;11(1):125. doi:10.1186/s13045-018-0669-2
28. Zhao J, Huang W, Wu Y, et al. Prognostic role of pretreatment blood lymphocyte count in patients with solid tumors: a systematic review and meta-analysis. Cancer Cell Int. 2020;20(1):15. doi:10.1186/s12935-020-1094-5
29. Almås B, Halvorsen OJ, Gjengstø P, Ulvik Ø, Beisland C. Grading of urothelial carcinoma of the upper urinary tract according to the World Health Organization/International Society of Urological Pathology classification from 2004 is a valuable tool when considering whether a patient is suitable for endoscopic treatment. Scand J Urol. 2016;50(4):298–304. doi:10.3109/21681805.2016.1144220
30. Pedersen CK, Babu AS. Understanding the Lymphatics: an Updated Review of the N Category of the AJCC 8th Edition for Urogenital Cancers. AJR Am J Roentgenol. 2021;217(2):368–377. doi:10.2214/AJR.20.22997
31. Nigwekar P, Amin MB. The many faces of urothelial carcinoma: an update with an emphasis on recently described variants. Adv Anat Pathol. 2008;15(4):218–233. doi:10.1097/PAP.0b013e31817d79b9
32. Albrengues J, Shields MA, Ng D, et al. Neutrophil extracellular traps produced during inflammation awaken dormant cancer cells in mice. Science. 2018;361(6409). doi:10.1126/science.aao4227.
33. Langner C, Hutterer G, Chromecki T, Winkelmayer I, Rehak P, Zigeuner R. pT classification, grade, and vascular invasion as prognostic indicators in urothelial carcinoma of the upper urinary tract. Mod Pathol. 2006;19(2):272–279. doi:10.1038/modpathol.3800529
34. Montironi R, Cheng L, Scarpelli M, Lopez-Beltran A. Pathology and Genetics: tumours of the Urinary System and Male Genital System: clinical Implications of the 4th Edition of the WHO Classification and Beyond. Eur Urol. 2016;70(1):120–123. doi:10.1016/j.eururo.2016.03.011
35. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–867. doi:10.1038/nature01322
36. Cupp MA, Cariolou M, Tzoulaki I, Aune D, Evangelou E, Berlanga-Taylor AJ. Neutrophil to lymphocyte ratio and cancer prognosis: an umbrella review of systematic reviews and meta-analyses of observational studies. BMC Med. 2020;18(1):360. doi:10.1186/s12916-020-01817-1
37. Yamamoto T, Kawada K, Obama K, Romero MP. Inflammation-Related Biomarkers for the Prediction of Prognosis in Colorectal Cancer Patients. Int J Mol Sci. 2021;23(1):22. doi:10.3390/ijms23010022
38. Huang H, Liu Q, Zhu L, et al. Prognostic Value of Preoperative Systemic Immune-Inflammation Index in Patients with Cervical Cancer. Sci Rep. 2019;9(1):3284. doi:10.1038/s41598-019-39150-0
39. Jiang Y, Xu D, Song H, et al. Inflammation and nutrition-based biomarkers in the prognosis of oesophageal cancer: a systematic review and meta-analysis. BMJ Open. 2021;11(9):e048324. doi:10.1136/bmjopen-2020-048324
40. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–444. doi:10.1038/nature07205
41. Ocana A, Nieto-Jiménez C, Pandiella A, Templeton AJ. Neutrophils in cancer: prognostic role and therapeutic strategies. Mol Cancer. 2017;16(1):137. doi:10.1186/s12943-017-0707-7
42. Ruka W, Rutkowski P, Kaminska J, Rysinska A, Steffen J. Alterations of routine blood tests in adult patients with soft tissue sarcomas: relationships to cytokine serum levels and prognostic significance. Ann Oncol. 2001;12(10):1423–1432. doi:10.1023/A:1012527006566
43. Stone RL, Nick AM, McNeish IA, et al. Paraneoplastic thrombocytosis in ovarian cancer. N Engl J Med. 2012;366(7):610–618. doi:10.1056/NEJMoa1110352
44. Haemmerle M, Stone RL, Menter DG, Afshar-Kharghan V, Sood AK. The Platelet Lifeline to Cancer: challenges and Opportunities. Cancer Cell. 2018;33(6):965–983. doi:10.1016/j.ccell.2018.03.002
45. Franco AT, Corken A, Ware J. Platelets at the interface of thrombosis, inflammation, and cancer. Blood. 2015;126(5):582–588. doi:10.1182/blood-2014-08-531582
46. Giannakeas V, Kotsopoulos J, Cheung MC, et al. Analysis of Platelet Count and New Cancer Diagnosis Over a 10-Year Period. JAMA Netw Open. 2022;5(1):e2141633. doi:10.1001/jamanetworkopen.2021.41633
47. Simanek R, Vormittag R, Ay C, et al. High platelet count associated with venous thromboembolism in cancer patients: results from the Vienna Cancer and Thrombosis Study (CATS). J Thromb Haemost. 2010;8(1):114–120. doi:10.1111/j.1538-7836.2009.03680.x
48. van der Leun AM, Thommen DS, Schumacher TN. CD8+ T cell states in human cancer: insights from single-cell analysis. Nat Rev Cancer. 2020;20(4):218–232. doi:10.1038/s41568-019-0235-4
49. Stanton SE, Disis ML. Clinical significance of tumor-infiltrating lymphocytes in breast cancer. J Immunother Cancer. 2016;4(1):59. doi:10.1186/s40425-016-0165-6
50. Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–899. doi:10.1016/j.cell.2010.01.025
51. Stangl-Kremser J, Muto G, Grosso AA, et al. The impact of lymphovascular invasion in patients treated with radical nephroureterectomy for upper tract urothelial carcinoma: an extensive updated systematic review and meta-analysis. Urol Oncol. 2022;40(6):243–261. doi:10.1016/j.urolonc.2022.01.014
52. Kohada Y, Hayashi T, Goto K, et al. Preoperative risk classification using neutrophil-lymphocyte ratio and hydronephrosis for upper tract urothelial carcinoma. Jpn J Clin Oncol. 2018;48(9):841–850. doi:10.1093/jjco/hyy084
53. Vartolomei MD, Mathieu R, Margulis V, et al. Promising role of preoperative neutrophil-to-lymphocyte ratio in patients treated with radical nephroureterectomy. World J Urol. 2017;35(1):121–130. doi:10.1007/s00345-016-1848-9
54. Luo Z, Jiao B, Yan Y, et al. Risk factors for extraurothelial recurrence in upper tract urothelial carcinoma after radical nephroureterectomy: a retrospective study based on a Chinese population. Front Oncol. 2023;13:1164464. doi:10.3389/fonc.2023.1164464
55. Zheng Y, Chen Y, Chen J, et al. Combination of Systemic Inflammation Response Index and Platelet-to-Lymphocyte Ratio as a Novel Prognostic Marker of Upper Tract Urothelial Carcinoma After Radical Nephroureterectomy. Front Oncol. 2019;9:914. doi:10.3389/fonc.2019.00914
56. Luo Z, Jiao B, Huang T, et al. Development and external validation of a novel nomogram to predict intravesical recurrence after radical nephroureterectomy: a multicenter study. J Cancer Res Clin Oncol. 2023;149(13):11223–11231. doi:10.1007/s00432-023-05016-2
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.