Back to Journals » Vascular Health and Risk Management » Volume 21
Predictors of Patency Following Infrainguinal Arterial Interventions Under Intravascular Ultrasound Guidance: Analysis from the iDissection Studies
Authors Shammas NW , Shammas GA, Sharis W , Arvanitis Z , Jones-Miller S
Received 6 February 2025
Accepted for publication 17 June 2025
Published 30 June 2025 Volume 2025:21 Pages 505—518
DOI https://doi.org/10.2147/VHRM.S518392
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Daniel Duprez
Nicolas W Shammas, Gail A Shammas, William Sharis, Zoe Arvanitis, Sue Jones-Miller
Cardiology Division, Midwest Cardiovascular Research Foundation, Davenport, IA, USA
Correspondence: Nicolas W Shammas, Cardiology Division, Midwest Cardiovascular Research Foundation, 630 E 4th Street, Davenport, IA, 52801, USA, Email [email protected]
Background: Intravascular Ultrasound (IVUS) has been shown in smaller studies to improve outcomes when used to guide infrainguinal peripheral arterial interventions. The iDissection series of studies were conducted to determine the presence of dissections with various prepping devices in femoropopliteal and infrapopliteal arteries. The impact of IVUS-directed treatment on the long-term outcomes in these patients remains unclear.
Methods: All patients were enrolled at a single center with the exception of the Auryon BTK study (at 4 US centers). Seven prospective iDissection studies had been previously conducted with IVUS and the data was core lab adjudicated. We retrospectively analyzed major adverse limb events, freedom from target lesion revascularization (freedom from TLR) and patency at 1 year in these patients using medical records. The study was approved by a central ethics committee. Proportional and Kaplan–Meier survival analysis were performed. Logistic regression analysis to determine independent predictors of patency was performed.
Results: A total of 102 patients (n=135 encounters) were included. The median age was 72 years. 49.0% were diabetics and 50.0% had chronic limb-threatening ischemia (CLTI). 69.6% of lesions are de novo, 32.6% chronic total occlusion, 60.7% with moderate or severe calcium, and 72.6% femoropopliteal. Stent use was 38.5% (of which 53.8% drug eluting and 73.1% primary stenting), and drug-coated balloons 55.6%. Vessel prepping included atherectomy (66.7%), angioplasty (14.8%) and Flex VP (18.5%). Proportional Freedom from TLR at 1 year was 89.4%, and patency 89.4%. There was one major amputation. Mortality was 7.8% (95% CI; 3.49, 14.87). Logistic regression analysis showed that post balloon stenosis (odds ratio (OR) 1.07, p=0.015), tobacco use (OR 0.20, p=− 0.007), presence of CTO (OR 3.59, p=0.019), and male sex (OR 3.85, p=0.035) were predictors of patency loss.
Conclusion: Infrainguinal arteries treated with IVUS guidance appears to have good patency and freedom from TLR. The presence of adventitial dissections does not appear to be predictive of patency likely confounded with the high use of drug-coated balloons and drug-eluting stents.
Keywords: dissection, intravascular ultrasound, patency, target lesion revascularization, vessel prepping, drug coated balloons, drug eluting stents
Background
The use of precision imaging with intravascular ultrasound (IVUS) was shown to improve outcomes of patients undergoing coronary interventions.1–5 In peripheral arterial interventions, IVUS has been shown to be more accurate than angiography in defining plaque morphology, the presence of calcium and its severity, the number and extent of dissections, vessel size and lesion severity.6–9 Smaller studies also indicated the positive role of IVUS in peripheral arterial interventions in reducing target lesion revascularization (TLR), improving patency and resulting in fewer complications.10–16 Furthermore, operators quite often change their intraprocedural strategy of treatment based on IVUS findings. In the ADAPT-DES study IVUS changed PCI strategy in 74% of the time with operators using larger stents, higher balloon inflation and the need for additional post dilation.17
The core lab adjudicated iDissection series of prospective studies (n=7) were performed to determine the presence and extent of dissections and vessel sizing with IVUS when compared with angiography and using various atherectomy and vessel prepping devices. In this study we evaluate the long-term outcome of patients treated in the iDissection studies.
Methods
All patients in the seven prospective iDissection studies were included in this analysis.7–9,18–20 Angiographic analysis in these patients was conducted by the QVA and IVUS Core Laboratory at the Midwest Cardiovascular Research Foundation (MCRF), Davenport, IA, USA. IVUS analysis was also done by the core laboratory at MCRF and St John Providence Health System, Detroit, MI, USA. All inclusion and exclusion criteria, procedural details and 30-day outcomes in each study have also been published. The 1-year data was retrospectively collected from medical records. The study was approved by WCG, a central Ethics Committee, Princeton, NJ. A waiver of informed consent was granted by the Ethics Committee given the retrospective nature of the data collection and no risks to subjects. The study complies with the Declaration of Helsinki. Demographics, clinical, angiographic and procedural outcomes were pooled from all the studies. The primary endpoints were target lesion revascularization (TLR) (defined as the retreatment of the index lesion) and clinical patency (defined as PSVR ≤2.4 and no TLR) at 30 days, 6 months and 12 months. During the follow-up analysis, the TLR, target vessel revascularization (TVR), mortality and patency rates were cumulative, and the denominator (N) was based on the follow-up visit, not the actual days from the index procedure.
Statistical Analysis
Descriptive analysis on all variables was done. Analysis was performed per patient and per encounter treated for each study arm. Continuous data was presented as mean ± standard deviation [median]; Categorical data was given as count/sample (percentage). Pearson’s Chi-Square Exact Test, Fisher’s Exact Test, Sign test and Student’s t-test were used where appropriate. Normality and outlier tests were done with Anderson–Darling test and Grubbs test, respectively. Median confidence intervals were used when data was not normally distributed. The proportion confidence interval was calculated using the Adjusted Blaker’s exact method.
Logistic regression analysis for patency was done. In addition, TLR and patency rates were analyzed for significance with drug-coated balloon or drug-coated stent. Logistic regression analysis was evaluated for significance with the Wald Test, area under ROC curve and Goodness of Fit tests, Pearson and Hosmer-Lemeshow. Predicted probability was evaluated for various hypothetical post-balloon stenosis (Core Lab verified), presence of chronic total occlusion, and tobacco use. Several multiple logistic regression analysis models were conducted to determine if drug elution had an impact on the overall outcome of TLR in the overall cohort. These models included below versus above the knee treatment, presence of C dissections on IVUS (adventitial dissections), and the use of DCB and DES. Survival analysis for freedom from TLR, patency and freedom from TLR for femoropopliteal versus infrapopliteal interventions were plotted. Procedures with patients who died, lost to follow-up or had missing information were censored. Statistical significance was determined by a p-value < 0.05. Software used was Minitab 21 (State College Pennsylvania, USA) and Cytel Studio 12 (Cambridge, Massachusetts, USA).
Results
A total of 102 patients (n=135 encounters) were included. The median age was 72 years. 49.0% were diabetics and 50.0% had chronic limb-threatening ischemia (CLTI). 69.6% of lesions are de novo, 32.6% chronic total occlusion, 60.7% with moderate or severe calcium, and 72.6% femoropopliteal. Stent use was 38.5% (of which 53.8% drug eluting and 73.1% primary stenting), and drug-coated balloons 55.6%. Vessel prepping included atherectomy (66.7%), angioplasty (14.8%) and Flex VP (18.5%) (Tables 1 and 2). NHLBI and IVUS dissections are listed in Table 3. There was one in-hospital mortality secondary to a retroperitoneal bleed and deemed to be procedure- but not device-related (Table 4). Individual outcomes are listed in Table 5.
 |
Table 1 Demographics and Clinical Variables |
 |
Table 2 Procedural and Angiographic Variables |
 |
Table 3 Angiographic and IVUS Dissections |
 |
Table 4 In-Hospital Complications |
 |
Table 5 Outcomes |
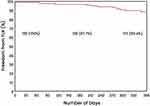
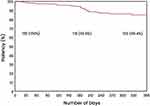
On follow-up 7 patients died, 8 lost to follow-up and 3 had missing information. Proportional Freedom from TLR at 1 year was 89.4% (Figure 1) and patency 89.4% (Figure 2). There was one major amputation. Mortality was 7.8%. The probability of patency was higher in the femoropopliteal arteries versus infrapopliteal arteries (88.1% vs 71.9% respectively, p=0.023) (Figure 3) but probability of freedom from TLR was statistically similar (88.1% vs 93.6%, p=0.424). The Rutherford Becker category at 30-day remained unchanged at 1-year follow-up (Table 6).
 |
Table 6 Rutherford Becker Category |
Logistic regression analysis showed that post-balloon stenosis (odds ratio (OR) 1.07, p=0.015), tobacco use (OR 0.2, p=−0.007), presence of CTO (OR 3.6, p=0.019), and male sex (OR 3.85, p=0.035) were predictors of patency loss. Multiple regression models that included the presence of deep dissections on IVUS (p=0.597), above versus below the knee treatment (p=0.289), and use of drug-coated balloons (p=0.209) or drug-eluting stents (p=0.141) did not appear to predict target lesion revascularization.
Discussion
IVUS is a precision imaging modality that offers significantly more accurate information to vessel wall morphology and size, lesion extent and severity, and degree of calcification. IVUS guidance quite often alters the intraprocedural strategy of the operator in treating peripheral arterial disease (see typical cases 1 to 3 below; Figure 4–6). In this study, we have observed a high rate of freedom from TLR and patency in a cohort of patients with complex disease with 49.0% of patients being diabetics and just half the patients have chronic threatening limb ischemia. CKD was present in 45.1% of patients, CTO in 32.6% and severe calcium in 40.7% of patients.
A recent metanalysis evaluating the risk of restenosis post lower extremity arterial interventions showed Trans-Atlantic Inter-Society Consensus II classification, age, hypertension, diabetes, high-sensitivity C-reactive protein, and surgical approach were independent predictors of restenosis.21 In our cohort and under IVUS guidance predictors of loss of patency were residual narrowing, CTO and male sex. This is consistent with data published by Horie et al22 that reported a primary patency rate of 80.0% at 1-year after drug-coated balloon treatment of femoropopliteal lesions. In their study, predictors of restenosis were CTO (p < 0.001), circumferential calcification (p = 0.023), and smaller post-procedural minimum lumen area (p=0.036). Similarly, in a cohort of patients where 73.4% of patients had femoropopliteal arteries treated with DCB under IVUS guidance, predictors of restenosis were history of revascularization, CTO, residual stenosis, smaller distal reference vessel diameter, severe calcification and low‐dose DCB.23 CTO and residual narrowing appear to be consistent predictors of restenosis among published studies of femoropopliteal interventions performed with IVUS guidance.
Deeper dissections into the adventitia by IVUS did not appear to predict a higher rate of restenosis, likely related to the higher use of drug-eluting balloons and stents in the femoropopliteal arteries. Deeper dissections with adventitial injuries have been reported to predict loss of patency24 but the use of drug elution has also been shown to mitigate the risk of deeper dissections.25 Despite the use of drug elution, a recent randomized trial has shown that the addition of IVUS significantly improves outcome when compared with angiography-guided drug-coated balloon use in femoropopliteal arteries, particularly in complex lesions.26
Adventitial injury is more likely to impact long-term outcome when no drug elution is used. In the infrapopliteal arteries, the rate of deep dissections was very small with vessel prepping. Despite no drug elution use, the overall freedom from TLR appears to be superior to historic controls in the infrapopliteal arteries where no IVUS was used routinely.27,28 This suggests that IVUS guidance in the infrapopliteal arteries is likely to improve outcomes despite no use of drug elution. This needs to be confirmed in randomized trials in infrapopliteal interventions.
The rate of patency was higher at 1 year following treatment of femoropopliteal arteries when compared to infrapopliteal ones despite the use of IVUS. Despite this difference, patency rate in the infrapopliteal arteries was high at 71.9% with very low rate of amputation, mortality and overall procedural complications. This is in contrast to the overall 1-year historic primary patency of 63.1%, repeat revascularization 18.2%, major amputation 14.9% and all-cause mortality 15.1%.27,28 Multiple logistic regression analysis including above versus below the knee interventions, and use of drug elution vs no drug elution has shown no differences in TLR in this IVUS-treated cohort.
Example of Cases of Intravascular Ultrasound Applications
Case 1 (Figure 4). Patient presents with claudication Rutherford Becker category III after failed home exercise program. Ankle Brachial Index on the left was 0.6. Angiography revealed a total occlusion (CTO) of the left mid and distal superficial artery with collaterals to the left popliteal and left tibial arteries. CTO was crossed successfully using a crossing catheter and a 0.014″ 25 gm-tip wire. IVUS was then done and confirmed the intraluminal crossing of the wire and a vessel diameter of 5 to 5.5 mm. Laser atherectomy was then performed with the 2.35 mm of the 355-nm laser catheter followed by a 5 mm angioplasty balloon at 6 atmospheres. Angiographically, there was good flow in the vessel. One area of the vessel (arrow pointing on mark 24 of the ruler on the angiographic panel) appeared to have some haziness and had about 30–35% narrowing. Repeat IVUS showed a small intimal dissection of no clinical significance. There was residual plaque noted but good flow. No stenting was needed. IVUS in this case determined the intraluminal crossing of a CTO allowing us to use atherectomy safely. Also it guided the size of the balloon post atherectomy. In addition, it identified an insignificant dissection that did not need to be stented despite the appearance of haziness on the angiogram.
Case 2 (Figure 5). Patient presents with claudication Rutherford Becker category III and Ankle Brachial Index of 0.5. Angiography showed a severe 90% lesion in the mid to distal right superficial femoral artery. IVUS was performed. Fibrocalcific plaque was noted. Rotational atherectomy was performed followed by drug-coated balloon with size guided by the IVUS. Angiography showed the possibility of a type D spiral dissection (see 15 and 18 on the ruler marker). IVUS was then performed and showed a dissection (less than 180-degree arc and involving the intima and media. No injury to the adventitia is seen). The flow was good. We decided given the IVUS findings not to stent this vessel. IVUS did guide the extent of dissection, the size of the vessel and the nature of the plaque; none were adequately visualized by angiography.
Case 3 (Figure 6). Patient presents with chronic-threatening limb ischemia and an ulcer on the dorsal aspect of the first big toe. Angiography revealed severe disease in the tibial arteries with total occlusion of the anterior tibial artery (AT) and the tibioperoneal (TP) trunk. The peroneal, dorsalis pedis (DP) and distal AT were faintly filling with collaterals. Angiographically, the vessel was estimated to be 3.5 mm. An intravascular ultrasound (IVUS) showed the vessel size to be approximately 4.5 mm. This changed our original plan to use a 1.5 mm laser to 2 mm laser catheter. Post laser treatment, followed by a 4 mm low pressure balloon angioplasty (5 atmospheres), less than 10% residual narrowing is noted with no dissections. IVUS in this case was critical to provide the appropriate size of the vessel that led to the choice of the appropriate laser catheter size and balloon size. Also it verified the optimal final results with no dissections and good minimal luminal area gain.
Limitation of the Study
The study is limited by its smaller size and no control group (all patients had IVUS). The data however was acquired prospectively up to 1-month follow-up and was adjudicated by core lab. IVUS based multicenter and randomized studies are needed to determine the impact of IVUS on long-term outcomes of infrainguinal arterial endovascular intervention with prespecified subgroup analysis of patients with adventitial injury and drug elution. A basic knowledge of IVUS image interpretation is needed. Several aspects to IVUS need to be learned including vessel sizing, different plaque morphology, presence and severity of calcium, presence and extent of dissection, and assessment of lesion severity before and after treatments. Operators with less experience in IVUS may not be able to adequately utilize IVUS to its full potential in guiding peripheral arterial interventions. We believe IVUS training is critical for endovascular operators.
Acknowledgments
The abstract of this paper was presented at the CRT 2024 Conference as an oral presentation with interim findings. The abstract was published in J Am Coll Cardiol Intv. 2025 Feb, 18 (4_Supplement) S40. https://www.jacc.org/doi/10.1016/j.jcin.2025.01.136
Disclosure
Dr Shammas receives educational and research grants from Angiodynamics, Boston Scientific, Bard/BD, Phillips and Abbott. He is also on the speaker bureau of Janssen, Lilly, Boehringer Ingelheim, Amgen and Bayer. The authors report no other conflicts of interest in this work.
References
1. Xu A, Wang D, Chen B, et al. Efficacy of IVUS-guided stent implantation in patients with complex CAD: a meta-analysis based on RCTs. Front Cardiovasc Med. 2024;28(11):1446014. doi:10.3389/fcvm.2024.1446014
2. Darmoch F, Alraies MC, Al-Khadra Y, Moussa Pacha H, Pinto DS, Osborn EA. Intravascular ultrasound imaging–guided versus coronary angiography–guided percutaneous coronary intervention: a systematic review and meta-analysis. J Am Heart Assoc. 2020;9(5):e013678. doi:10.1161/JAHA.119.013678
3. Zhang J, Gao X, Kan J, et al. Intravascular Ultrasound Versus Angiography-Guided Drug-Eluting Stent Implantation: the ULTIMATE Trial. JACC. 2018;72(24):3126–3137. doi:10.1016/j.jacc.2018.09.013
4. Ahn JM, Kang SJ, Yoon SH, et al. Meta-analysis of outcomes after intravascular ultrasound-guided versus angiography-guided drug-eluting stent implantation in 26,503 patients enrolled in three randomized trials and 14 observational studies. Am J Cardiol. 2014;113(8):1338–1347. doi:10.1016/j.amjcard.2013.12.043
5. Hong S-J, Mintz GS, Ahn CM, et al. Effect of Intravascular Ultrasound-Guided Drug-Eluting Stent Implantation: 5-Year Follow-Up of the IVUS-XPL Randomized Trial. JACC: Cardiovasc Interv. 2020;13(1):62–71. doi:10.1016/j.jcin.2019.09.033
6. Shammas N, Radaideh Q, Daher GE, Rachwan RJ, Radaideh Y, Radaideh Y. The role of precise imaging with intravascular ultrasound in coronary and peripheral interventions. Vasc Health Risk Manag. 2019;15:283–290. doi:10.2147/VHRM.S210928
7. Shammas NW, Torey JT, Shammas WJ, Jones-Miller S, Shammas GA. Intravascular Ultrasound Assessment and Correlation With Angiographic Findings of Arterial Dissections Following Auryon Laser Atherectomy and Adjunctive Balloon Angioplasty: results of the iDissection Auryon Laser Study. J Endovasc Ther. 2022;29(1):23–31. Epub 2021 Jun 28. doi:10.1177/15266028211028200.
8. Shammas NW, Shammas WJ, Jones-Miller S, et al. Optimal Vessel Sizing and Understanding Dissections in Infrapopliteal Interventions: data From the iDissection Below the Knee Study. J Endovasc Ther. 2020;27(4):575–580. Epub 2020 May 18. doi:10.1177/1526602820924815.
9. Shammas NW, Torey JT, Shammas WJ, Jones-Miller S, Shammas GA. Intravascular Ultrasound Assessment and Correlation With Angiographic Findings Demonstrating Femoropopliteal Arterial Dissections Post Atherectomy: results From the iDissection Study. J Invasive Cardiol. 2018;30(7):240–244.
10. IVUS-ACS Investigators, Gao X, Kan J, Wu Z, et al. IVUS-Guided vs Angiography-Guided PCI in Patients With Diabetes With Acute Coronary Syndromes: the IVUS-ACS Trial. JACC: Cardiovasc Interv. 2024;18:283–293. Online ahead of print. doi:10.1016/j.jcin.2024.09.061
11. Gee A, Tarricone A, Lavery L, et al. The Role of Intravascular Ultrasound in Limb Salvage: a Systematic Review and Meta-Analysis. Vasc Endovascular Surg. 2024;2024:15385744241292861. Online ahead of print. doi:10.1177/15385744241292861
12. Fujihara M, Yazu Y, Takahara M. Intravascular Ultrasound-Guided Interventions for Below-the-Knee Disease in Patients with Chronic Limb-Threatening Ischemia. J Endovasc Ther. 2020;27(4):565–574. Epub 2020 Jun 26. doi:10.1177/1526602820935606.
13. Soga Y, Takahara M, Ito N, et al. Clinical impact of intravascular ultrasound-guided balloon angioplasty in patients with chronic limb threatening ischemia for isolated infrapopliteal lesion. Catheter Cardiovasc Interv. 2021;97(3):E376–E384. Epub 2020 Oct 21. doi:10.1002/ccd.29347.
14. Hartung V, Augustin AM, Gruschwitz P, Grunz JP, Knarr J, Kickuth R. Endovascular therapy in intermittent claudication: impact of IVUS guidance on treatment decisions. Rofo. 2024;2024:1. Online ahead of print. doi:10.1055/a-2379-8857
15. Ko YG, Lee SJ, Ahn CM, et al. IVUS-DCB investigators. Intravascular ultrasound-guided drug-coated balloon angioplasty for femoropopliteal artery disease: a clinical trial. Eur Heart J. 2024;45(31):2839–2847. doi:10.1093/eurheartj/ehae372
16. Allan RB, Puckridge PJ, Spark JI, Delaney CL. The Impact of Intravascular Ultrasound on Femoropopliteal Artery Endovascular Interventions: a Randomized Controlled Trial. JACC: Cardiovasc Interv. 2022;15(5):536–546. doi:10.1016/j.jcin.2022.01.001
17. Witzenbichler B, Maehara A, Weisz G, et al. Relationship between intravascular ultrasound guidance and clinical outcomes after drug-eluting stents: the assessment of dual antiplatelet therapy with drug-eluting stents (ADAPT-DES) study. Circulation. 2014;129(4):463–470. doi:10.1161/CIRCULATIONAHA.113.003942
18. Shammas NW, Shammas WJ, Shammas GA, Jones-Miller S. Intravascular Ultrasound Assessment of Arterial Dissections Following Rotarex Atherectomy: results of the iDissection Rotarex Study. J Soc Cardiovasc Angiogr Interv. 2024;3(9):102155. eCollection 2024 Sep. doi:10.1016/j.jscai.2024.102155.
19. Shammas NW, Shammas WJ, Shammas GA, Jones-Miller S. Femoropopliteal Arterial Dissections Following FLEX VP and Balloon Angioplasty Versus Balloon Angioplasty Alone: intravascular Ultrasound Assessment and Correlation With Angiographic Findings. Cardiovasc Revasc Med. 2022;44:62–66. Epub 2022 Jul 5. doi:10.1016/j.carrev.2022.06.262
20. Shammas NW, Shammas WJ, Jones-Miller S, Radaideh Q, Shammas GA. Femoropopliteal Arterial Dissections Post Flex Vessel Prep and Adjunctive Angioplasty: results of the Flex iDissection Study. J Invasive Cardiol. 2019;31(5):121–126. doi:10.25270/jic/19.00079
21. Quan X, Liu Y, Xiong H, et al. Risk-Prediction Model of Restenosis after Endovascular Treatment for Peripheral Arterial Disease: a Systematic Review and Meta-analysis. J Endovasc Ther. 2024;8:15266028241289083. Online ahead of print. doi:10.1177/15266028241289083
22. Horie K, Tanaka A, Taguri M, Inoue N. Impact of Baseline and Postprocedural Intravascular Ultrasound Findings on 1-Year Primary Patency After Drug-Coated Balloon Treatment of Femoropopliteal Lesions. J Endovasc Ther. 2022;29(1):66–75. Epub 2021 Nov 15. doi:10.1177/15266028211058683.
23. Soga Y, Takahara M, Iida O, et al. The POPCORN. Vessel Patency and Associated Factors of Drug‐Coated Balloon for Femoropopliteal Lesion. J Am Heart Assoc. 2022;12(1):e025677. doi:10.1161/JAHA.122.025677
24. Tarricone A, Ali Z, Rajamanickam A, et al. Histopathological evidence of adventitial or medial injury is a strong predictor of restenosis during directional atherectomy for peripheral artery disease. J Endovasc Ther. 2015;22(5):712–715. doi:10.1177/1526602815597683
25. Tepe G, Zeller T, Schnorr B, et al. High-grade, non-flow-limiting dissections do not negatively impact long-term outcome after paclitaxel-coated balloon angioplasty: an additional analysis from the THUNDER study. J Endovasc Ther. 2013;20(6):792–800. doi:10.1583/13-4392R.1
26. Lee SJ, Kim TH, Lee JH, et al. IVUS-DCB Investigators. Intravascular Ultrasound-Guided vs Angiography-Guided Drug-Coated Balloon Angioplasty in Patients With Complex Femoropopliteal Artery Disease. JACC: Cardiovasc Interv. 2025;18(5):558–569. doi:10.1016/j.jcin.2024.10.052
27. Snyder D, Zilinyi RS, Pruthi S, et al. Percutaneous Transluminal Angioplasty for Infrapopliteal Chronic Limb-Threatening Ischemia: a Systematic Review and Meta-analysis of Primary Patency and Binary Restenosis Rates. J Endovasc Ther. 2023;26:15266028231212133. Online ahead of print. doi:10.1177/15266028231212133
28. Mustapha JA, Finton SM, Diaz-Sandoval LJ, et al. Percutaneous transluminal angioplasty in patients with infrapopliteal arterial disease. Circ Cardiovasc Interv. 2016;9(5):e003468. doi:10.1161/CIRCINTERVENTIONS.115.003468
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Jetstream Atherectomy Followed by Paclitaxel-Coated Balloons versus Balloon Angioplasty Followed by Paclitaxel-Coated Balloons: Twelve-Month Exploratory Results of the Prospective Randomized JET-RANGER Study
Shammas NW, Purushottam B, Shammas WJ, Christensen L, Shammas G, Weakley D, Jones-Miller S
Vascular Health and Risk Management 2022, 18:603-615
Published Date: 2 August 2022
Jetstream Atherectomy with Paclitaxel-Coated Balloons: Two-Year Outcome of the Prospective Randomized JET-RANGER Study
Shammas NW, Shammas G, Christensen L, Jones-Miller S
Vascular Health and Risk Management 2023, 19:133-137
Published Date: 11 March 2023