Back to Journals » Patient Preference and Adherence » Volume 19
Preferences for First-Line Chronic Lymphocytic Leukemia Treatments: Results From a Multinational Study on the Perspectives of Patients and Physicians
Authors Sile B, Patel D, Horchi D, Rault B , Mulvihill E, Beusterien K, Stewart K, Miranda P , Guillaume X
Received 4 December 2024
Accepted for publication 12 March 2025
Published 29 March 2025 Volume 2025:19 Pages 823—837
DOI https://doi.org/10.2147/PPA.S510401
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Bersabeh Sile,1 Dipen Patel,2 Dahbia Horchi,3 Bleuenn Rault,3 Emily Mulvihill,4 Kathleen Beusterien,4 Katherine Stewart,2 Paulo Miranda,2 Xavier Guillaume3
1AstraZeneca, Cambridge, UK; 2AstraZeneca, Gaithersburg, MD, USA; 3Oracle Life Sciences, Paris, France; 4Oracle Life Sciences, North Kansas City, MO, USA
Correspondence: Xavier Guillaume, Oracle Life Sciences, 198 Avenue de France, Paris, 75013, France, Tel + 33 6 14 57 45 95, Email [email protected]
Background: Few studies have explored physician and patient preferences for the treatment of chronic lymphocytic leukemia (CLL) related to treatment efficacy, adverse events (AEs), and treatment duration. Thus, this observational, mixed-methods study investigated patients’ and physicians’ preferences for CLL first-line treatments.
Materials and Methods: An online discrete choice experiment in five countries among 192 patients and 259 physicians in the US, the UK, Germany, France, and Australia examined the importance of outcomes and treatment attributes.
Results: Increasing 5-year progression-free survival (5-year PFS) was most important to patients and physicians, with a relative importance (RI) of 30.3% among patients and 37.8% among physicians, followed by reducing the risks of common side effects (RI 21.6% among patients, 22.9% among physicians) and adverse events (AEs) leading to treatment discontinuation (RI 22.1% among patients, 20.6% among physicians). Patients strongly preferred time limited treatment regimen over treatment to progression (TTP). Specifically, patients and physicians would require a 6.4% vs 2.3% increase in 5-year PFS, a 19.4% vs 8.9% decrease in the risk of common all grades side effects, and a 7.5% vs 3.7% decrease in the risk of treatment discontinuation due to AEs, respectively, to compensate for a daily oral medication taken indefinitely vs daily oral medication taken for 24 months.
Conclusion: Overall, patients and physicians favor time-limited treatment regimens over TTP and value treatments with greater PFS benefits followed by lower side effects. Patients and physicians were both willing to trade-off switching from time-limited treatment to TTP for a better 5-year PFS, decrease side effects, and risk of treatment discontinuation due to AEs.
Keywords: chronic lymphocytic leukemia, first-line treatment, discrete choice experiment, fixed-duration treatment, patient and physician preferences
Introduction
Chronic lymphocytic leukemia (CLL) is the most common leukemia in adults in developed countries.1 Its incidence is 4.6/100,000 population per year in the US2 rising to over 32/100,000 population per year in people > 75 years of age globally.2 CLL is characterized by a relatively low mortality, with a 5-year relative survival rate of 88%.2 However, the 5-year survival rate is approximately 20% among very high-risk patients.3 CLL is usually diagnosed in older adults, with a median age at diagnosis of approximately 70 years.2 With the rapidly ageing population, the incidence and prevalence of CLL is expected to continue to increase.
Numerous advances in the treatment of CLL have been made, including the introduction of novel classes of targeted small molecules (eg, Bruton’s tyrosine kinase inhibitor (BTKi), B cell lymphoma-2 inhibitor (BCL2i) and phosphoinositide 3-kinase inhibitor (PI3Ki)).4,5 These small-molecule therapies, which have shown to be very effective against the disease and in patients with high-risk cytogenetics,6 are aimed at replacing the classic cytostatic agents fludarabine, cyclophosphamide and rituximab (FCR) as standard first-line treatment for younger, fit patients, and bendamustine and rituximab (BR) for treatment naive (TN) patients > 65 years of age.7–11 Based on published randomized clinical trials comparing chemoimmunotherapy (Chemotherapy-induced thrombocytopenia [CIT]) regimens with BTKi, namely, ibrutinib or acalabrutinib, BTKis are now considered a feasible option for all patients in the first-line setting.12–16
Today, with growing experience related to the use of continuous single BTKi-based treatments, such as ibrutinib, zanubrutinib and acalabrutinib, several potential drawbacks have emerged. Long-term follow-up from first-line BTKi trials show that responses are maintained in more than 70% of patients at five years, but discontinuations due to toxicities can be up to 40%.17–19 Intolerance, particularly due to cardiac dysrhythmias and increased bleeding risk, is a major reason for discontinuation in about 30% of patients. Although acalabrutinib may present lower toxicity in some cases, resistance and cost issues are not significantly different from ibrutinib.20–22 For patients with chronic toxicities, the cumulative effect significantly impairs the quality of life. Additionally, the development of BTKi resistant clones occurs in about 20% of patients,23 and the cost of these therapies over time remains substantial, due to their continuous and indefinite use.
Toxicities, resistance, and the growing cost of treatment to progression (TTP) treatment with BTKi have provided a robust argument to investigate time-limited combination therapy with targeted agents.24 Trials have already shown that such time-limited combinations can achieve deep remissions for the majority of patients.25 In particular, time-limited BCL2i-based regimens are now approved in both first-line and relapsed/refractory CLL. In addition, ongoing clinical trials are investigating novel drug combinations with different durations of therapy to provide additional treatment options for CLL patients, including BCL2i +BTKi combinations: BCL2i +ibrutinib (GLOW/CLL3011; NCT03462719), zanubrutinib± BCL2i (SEQUOIA; NCT03336333), and acalabrutinib+ BCL2i ±obinutuzumab (ACE-CL-311; NCT03836361).26,27
Few studies have explored physician and patient preferences for the treatment of CLL related to treatment efficacy, adverse events (AEs), and duration of treatment regimen, particularly among currently available treatment regimens in first-line CLL treatment. A recent study on CLL treatment preferences conducted with 220 patients and 151 physicians in the US sought to understand how variations in attributes impact treatment choice among patients and physicians through a discrete choice experiment (DCE) methodology.28 However, this study combined the administration form (intravenous vs oral) and the therapy duration/frequency (treat to progression vs treat for 24 months) into one attribute which may have obscured the individual contribution of treatment duration to overall treatment preference attributes.
Therefore, existing literature has yet to analyze the role of treatment duration associated with therapies for first-line CLL therapy in determining treatment selection preference as well as the importance of patient characteristics as a possible decision bias. Understanding the similarities and differences in preferences between physicians and patients with CLL is key to supporting decision-making; therefore, there is also a need to explore the potential gap between the preferences of physicians and patients in the first-line treatment setting.
This study aimed to address these knowledge gaps by utilizing a discrete choice experiment (DCE) to determine preferences among patients and physicians in the United States (US), Western Europe (United Kingdom (UK), France, Germany), and Australia regarding key CLL first-line treatment attributes including TTP vs time-limited combination therapy.
Materials and Methods
Study Design
This was an observational, mixed-methods study that was conducted according to best practice guidelines for Conjoint Analyses published by the International Society of Pharmacoeconomics and Outcomes Research (ISPOR) Good Research Practices for Conjoint Analysis Task Force.29 Prior to a quantitative survey, in Phase 1, qualitative in-depth interviews were conducted via telephone with patients (N=28) and oncologists, hemato-oncologists or hematologists (N=12) in Australia, France, Germany and the UK, using a semi-structured interview guide to establish which attributes were the most important to patients and oncologists and survey content.30 Then, pretest interviews were conducted in Phase 2 to confirm that the DCE experiment and survey questions are appropriate and sufficiently clear to respondents. The study received exemption determination from Pearl Institutional Review Board (IRB) on March 10th, 2022. The survey was administered online in the US, UK, Germany, France, and Australia. Additionally, survey reminders were sent to non-responders to help reduce non-response bias.
Population
All study participants in the study were recruited through a convenience sampling method. Patients were recruited by Global Perspectives and Focus People (Australia) via referrals by physicians treating these patients, supported by social media targeting, outreach from patient databases, patient organizations, and support groups. Inclusion criteria consisted of patients aged ≥18 years, diagnosed with CLL by a healthcare provider and who were not currently employed by a market research, advertising, or pharmaceutical company. Physicians were recruited from the Kantar Profiles Panel and its panel partners. The physicians were medical oncologists, hemato-oncologists, and hematologists, had practiced between 5 and 30 years in current specialty, were Board certified (US only), had managed at least 20 patients (US, France, Germany) or 8 patients (UK, Australia) with CLL in the past 12 months prior to study enrollment, had prescribed novel agents (eg, BTKi, PI3Ki, BCL2i) for patients with CLL, and at least 50% of their time was spent in direct patient care (vs teaching, research, administrative work, etc.). All study participants provided informed consent.
Data Collection
The survey captured sociodemographic data, medical history, assessment of individual treatment attributes and attribute levels and preferences for first-line CLL treatment using a DCE. In a series of 12 DCE tasks, participants considered two hypothetical treatment options shown side-by-side and were asked to choose the one that was preferable to them. Each hypothetical treatment consisted of combinations of characteristics (“attributes”; eg, PFS) and how each hypothetical treatment satisfies the attributes (“attribute levels”; eg, 3 months, 5 months, etc.). The full set of attributes and attribute levels (referred to as ‘levels’) that respondents evaluated in the DCE is known as the experimental design, which approximates a balanced design with minimal overlap.31 As such, all respondents were presented with different combinations of levels in the DCE tasks. The operational definitions of survey attributes and levels used in the DCE for both patients and physicians are summarized in Table 1. The attribute and levels were consistent across the groups except for minor variations in wording to account for differences in health literacy levels in the patient group. The experiment included 5 attributes with 3–4 levels per attribute for each stakeholder group. To help stakeholders familiarize themselves with the different treatment attributes in the DCE, participants first rated each attribute level on its own on a scale of 1 (Very bad) to 5 (Very good). While the study is focused on novel agents that can be used in first-line, idelalisib or duvelisib (PKI3i) was not included in the experiment as these therapies were not approved in first-line settings and are not often used in routine clinical practice in the US. Other variables were collected and analyzed descriptively. Variables for patients included age, sociodemographic and clinical characteristics, such as sex, race/ethnicity (US only), education, employment status, treatment experience (watchful waiting versus treated patients, experience with time-limited and time-to-progression treatments), self-reported Eastern Cooperative Oncology Group (ECOG) status, and time since diagnosis. Other variables for physicians included clinical specialty, number of patients managed in the past 12 months (with cancer/with CLL), treatment settings of the CLL patients managed, number of years of practice, percentage of time spent in direct patient care, sociodemographic such as sex, year of born, state/region of residence, location of practice (major metropolitan area, urban area, suburb of a large city, small city, rural or small town), proportion of professional time spent treating patients according to the practice settings.
 |
Table 1 Attributes and Levels Included in the DCE |
Sample Size
The DCE experiment comprised 12 choice tasks with two treatment profiles per task. The combinations of levels shown for each profile was based on a balanced design with minimal overlap. The formula used to determine minimum sample sizes for aggregate attribute level full-profile DCE modelling is nta/c >500, where n is the number of respondents, t is the number of choice tasks, a is the number of alternatives per task, and c is equal to the largest number of attribute levels for any one attribute.31 With a sample size of 192 patients and 259 physicians, 12 DCE tasks showing 2 alternatives per task and up to 3 levels per attribute, the formula result is 1536 for patients and 2072 for physicians, which is far above 500, indicating that we have sufficient sample size in each group to obtain relatively precise utility estimates for the main effects.
Statistical Analysis
Analyses were conducted using R, version 4.2.2 and SPSS Statistics version 28.0.1.0, while Lighthouse studio from Sawtooth Software version 9.14.2 was used for DCE design and analysis. Descriptive analyses were performed on the full data sets using counts and percentages for categorical variables and means, standard deviations, median and range for continuous variables. A hierarchical Bayesian (HB) logistic regression was used to estimate preference weights for each attribute level and relative attribute importance (RI). The parameter estimates (utilities) from the HB analysis enable the calculation of the conditional relative importance of each attribute. The underlying choice-probability model in HB was conditional logit, using effects coding for the attribute levels. The model assumed that the preferences are normally distributed. The relative importance was calculated at the respondent attribute level by dividing the range of each attribute (utility of the most preferred level minus utility of the least preferred level) by the sum of ranges of all attributes and multiplying by 100. For each respondent, the relative importance estimates across attributes add to 100%. The estimates indicate how much the difference between the most preferred versus least preferred levels of each attribute affects the decision to choose a treatment.
The study team also assessed levels of respondent quality to identify and remove/replace those whose response patterns suggested a lack of attention in completing the DCE, indicating a lack of validity.
Results
Sample Characteristics of Patients and Physicians
A total of 195 patients and 302 physicians were recruited to participate in the survey. Three patients across the US (n=2) and UK (n=1) and 43 physicians across the US (n=30), UK (n=3), Australia (n=3), France (n=4), and Germany (n=3) were excluded from the final analysis due to low-quality data (ie, provided random or illogical responses and sped through the survey). The final sample included 192 patients and 259 physicians (US [n=100; n=97], UK [n=30; n=52], Germany [n=30; n=51], France [n=30; n=34], and Australia [n=2; n=25]) respectively.
Table 2 details the patient sociodemographic characteristics. Patients were fairly split across different regions of geography and population (ie, rural, suburb, major urban area). Most physicians were practicing in the major metropolitan (43.6%) and urban areas (31.7%). The average age of the patients was 63.5 (SD=10.6) years, with over half of patients indicating they were female (57.8%). In the US, the vast majority of the participants identified as White (94.0%). The majority were married or in a committed relationship (72.4%) and completed at least a university or college degree (74.5%). At the time of the study, only 21.4% of patients were employed full time, 48.4% were retired, and 13.5% were either employed part-time or employed but on a temporary leave of absence.
 |
Table 2 Patient Sociodemographic Characteristics (N=192) |
Patients reported that they had been diagnosed for an average of 7.7 (SD=6.5) years prior to completion of questionnaire. When asked about their current health status, about one-third (34.9%) indicated that their health was fair or poor, 38.0% indicated good health, and more than one-quarter (27.1%) indicated very good or excellent health. When asked about chromosomal and genetic mutations, over half (52.6%) of patients did not know or did not have any listed mutation. Of the remaining half, the most prominent mutation was a deletion at chromosome 13q (21.4%), followed by a deletion at chromosome 17p (16.1%), and an immunoglobulin heavy-chain gene mutation (13.5%). A chromosome deletion at 11q and trisomy 12 was least reported at 9.4% and 7.3%, respectively.
When asked about treatment history, almost one-third of patients (30.7%) had never undergone treatment with prescription medication, whereas 43.2% reported they were currently on treatment and 26.0% reported having undergone treatment in the past. Of those patients with experience taking prescription medications (n=133), almost half of patients (48.2%) reported being currently on or completed first-line treatment; 28.6% were currently on or completed second-line treatment, and 23.3% were currently on or completed third-line treatment. Patient experience with treatment varied with 22.6% using oral pills only, 12.8% using intravenous medication only, and most patients using both oral and intravenous medications at 63.2%. Three-quarters of patients (75.9%) reported using finite treatment at some point in their treatment journey compared to 54.9% using continuous treatment. Among patients who were currently being treated (n=83), 24.1% reported their treatment as finite whereas 65.1% reported their treatment as continuous. Among patients who have previously received or are currently receiving treatment (n=133), 83.5% reported experiencing a side effect related to their CLL treatment. Among those reporting side effects (n=111), those most experienced were muscle, joint, or bone pain (64.0%), headaches (58.6%), and diarrhea (54.1%). Severe side effects were also experienced, such as problems with heart rhythm (15.3%), infection (18.0%), and bleeding (hemorrhage) (14.4%). When asked about the impact of these side effects, over half of patients (55.9%) reported an impact on quality of life and felt they were difficult to manage; 29.7% reported hospitalization associated with side effects; and 25.2% of patients reported treatment discontinuation due to sides effects (Table 3).
 |
Table 3 Patient Clinical Characteristics and Treatment History (N=192) |
The mean age of the physician sample was 50.2 (SD=8.2) years old, with 73.7% identifying as male. The sociodemographic characteristics of the physicians are summarized in Table 4. Physicians had an average of 17.3 (SD=5.9) years of experience. Most physicians (n=167; 64.5%) specialized in both hematology and oncology, while 19.7% specialized in medical oncology and 15.8% in hematology. On average, physicians reported treating approximately 600 patients with cancer in the past 12 months, with most patients having breast cancer (mean: 72.4 patients) followed by chronic lymphocytic leukemia (mean: 66.6 patients). Physicians on average spent 87.9% of their time in direct patient care compared to other activities, such as research or administration and practiced in various settings including private practice and teaching and non-teaching hospitals.
 |
Table 4 Physician Sociodemographic Characteristics (N=259) |
Approximately, three-quarters of physicians would “often” or “always” discuss impacts of side effects on quality of life (79.2%), treatment options when initiating a new line of therapy (77.6%), the advantages/disadvantages of time-limited versus time-to-progression therapies (73.8%), and efficacy associated with different treatments (84.6%). For each topic, about one-third of physicians answered to have “always” discuss it with patients. Almost three-quarters of physicians also agreed that patients’ eligibility is the most important factor in selecting between time limited and TTP therapy (72.6%). Physicians were also asked about their preferences and practices when it came to treatment planning. Physicians agreed that they prefer to prescribe more aggressive treatments in first-line if patients are willing to accept the side effects and can tolerate the treatment (78.0%). Further, 71.0% of physicians agreed that targeted time-limited therapy is best suited for patients who are young, fit, and willing to accept aggressive first-line treatment. Almost half of physicians also agreed that time-limited treatments are generally more aggressive than TTP regimens (48.2%). When it came to patients’ preferences, 63.7% agreed that they would tailor the strategy to their patients’ preference and similarly, 66.0% agreed that they prefer to listen to their patients’ wishes when it comes to treatment duration (time-limited vs TTP treatment). Most physicians (86.1%) felt it was important to provide patients with all the information they need to understand the recommendation.
DCE Findings for Patients and Physicians
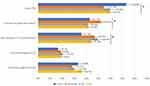
Figure 1 presents the mean preference weights for each attribute level in the DCE. For the quantitative attributes (PFS, common all grade side-effects, and risk of AE leading to treatment discontinuation), the preference weights generally increased linearly as the levels improved (proportional relationship between the best outcomes and the highest preference weights within each attribute). The relative importance of each attribute for patients and physicians is shown in Figure 2. Increasing 5-year PFS from 63% to 84% had the most influence on treatment choice among both patients and physicians (relative importances = 30.3% vs 37.8%, respectively), followed by decreasing common all grade side-effects from 58% to 12% (21.6% vs 22.9%, respectively) and decreasing AEs leading to treatment discontinuation from 22% to 5% (22.1% vs 20.6%, respectively). Treatment regimen for both oral (16.6% vs 11.6%) and IV (9.5% vs 7.2%) treatments were least important to patients and physicians, respectively; however, they were still influential in decision-making.
 |
Figure 1 DCE – Mean attribute level preference weights for physicians and patients. Abbreviations: AEs, Adverse events; IV, Intravenous; PFS, Progression-Free Survival; TT, Treatment. |
Patients valued switching from an indefinite oral regimen to a time-limited regimen more so than physicians. Specifically, patients and physicians would require a 6.4% vs 2.3% increase in 5-year PFS, a 19.4% vs 8.9% decrease in the risk of common all grades side effects, and a 7.5% vs 3.7% decrease in the risk of treatment discontinuation due to AEs, respectively, to compensate for a daily oral medication taken indefinitely vs daily oral medication taken for 24 months (Table 5).
 |
Table 5 DCE – Trade-Offs Required to Compensate for a Daily Oral Medication Taken Indefinitely Vs Daily Oral Medication Taken for 24 months (Everything Else Being Equal) |
Figure 3 presents the mean attribute importance estimates by country for patients. Attribute importances differed significantly among countries (p < 0.05), with the exception of the oral regimens and the IV regimens. Patients in France valued increases in 5-year PFS more highly, and they least valued reducing the risk of AEs leading to treatment discontinuation, compared to patients in Germany, UK, and US (p < 0.05). Patients in Germany valued reducing the risk of common all grade side effects more highly than patients in the other countries (p < 0.05). Within the oral regimens, patients in all countries least preferred ‘daily oral medication taken until disease progression’. No significant differences were observed in attribute importance among physicians across countries.
Discussion
This study provides insights on patients and physicians perspectives of key attributes of first-line CLL treatments across five countries. In our study, 5-year PFS was the most important attribute for both patients and physicians with treatment regimen ranking as least important for both. Treatment regimen, whether oral or IV and whether time-limited or indefinite, was least important to both patients and physicians. It is not surprising that physicians and patients are in many ways aligned in their priorities and acceptable trade-offs. Patients prioritized adverse events leading to treatment discontinuation as second, while physicians rated all grade side effects as second. Our findings show that, although time-limited treatment is generally more preferred than treating until progression, particularly among patients, this criterion is not as important as efficacy or side effects. This study found that physicians and patients would be willing to accept increased risk of side effects within the ranges evaluated in exchange for improvements in efficacy. Thus, in the real-world, where PFS is similar, physician and patient preferences would be driven by side effects, then by mode of administration. The relative importance of 5-year PFS was more important to patients than physicians, whereas it was similar between the two groups for side-effect attributes. Thus, it can be inferred that compared with physicians, patients required significantly higher increases in the chance of 5-year PFS to accept an increased risk of side effects. Notably, when considering treatment-related side effects, patients and physicians differed in how they prioritized these with respect to how bothersome they are.
Advances in understanding leukemogenesis mechanisms have enabled better stratification of CLL patients in terms of survival. It is well known to clinicians that TP53 lesions and del(17p) adversely impact prognosis.6 In our study, 47.4% of patients were aware of their cytogenetic mutation, 14.6% were aware that they had no cytogenetic mutation, and 38.0% did not know their cytogenetic status, suggesting that cytogenetic status may be an element of shared treatment decision-making for some but not all patients. Further research is needed to understand the relationship between prognosis and treatment preferences in CLL.
The current study addressed key gaps in the limited prior literature on stakeholder preferences in CLL. More specifically, instead of combining the administration form and the therapy duration/frequency into one attribute,28 this study was undertaken to address this issue by examining administration form and therapy duration/frequency as separate attributes, allowing for a clearer analysis of their individual contributions to treatment preferences. Given the growing number of treatment options in CLL, it is fundamental to understand these preferences in greater detail to guide clinical decision and enhance patient outcomes. Moreover, the current study uses more recent clinical data to inform its attribute levels. Previous data collection was completed in May 2019,28 and significant developments have since occurred, such as acalabrutinib achieving its primary efficacy endpoint against ibrutinib in CLL.32 Therefore, this study provides a more detailed and up-to-date analysis of treatment preferences. Similarly, other prior studies, which were published in 2016–2017,33,34 did not include attributes and levels representing a broader array of novel therapies, as only ibrutinib was approved at that time. Instead, these earlier studies included choice tasks with chemotherapy. The present study makes important contributions to the understanding of physician and patient preferences in the global context of the most current standards of care in CLL treatment.
Strengths
The attractiveness of a treatment to individuals depends on patients’ relative preferences for these attributes expressed by patients’ willingness to accept trade-offs among them. Although there are alternatives to eliciting patient preferences (eg, revealed preferences, direct ratings/rankings, etc.), DCE is one of the most common approaches for assessing preferences in a healthcare context, it has been increasingly applied in healthcare decisions, it has a strong foundation in psychology and economics,35,36 and it has become of increasing interest to health authorities and clinicians to facilitate shared decision-making.
Strengths of the study are the use of robust preference elicitation methods and the adherence to best practices for DCE/Conjoint studies outlined in the ISPOR DCE/Conjoint Task Force Report.31 Additionally, potential hypothetical bias was limited by constructing choice questions that mimicked realistic treatment options as closely as possible and were based on the published clinical evidence available at the time the study was conducted. The attributes and levels included in the study were also informed by prior qualitative research with patients with CLL and physicians, and the final survey instrument was pilot tested to ensure the DCE choice tasks were clear, appropriate, and interpreted as intended.
Limitations
An online survey likely under-represents people without access to or familiarity with online survey administration as well as individuals who are elderly, institutionalized or with the most severe comorbidities and disabilities. This may also underrepresent physicians who do not have the capacity or familiarity of online research.
Furthermore, the self-reported nature of the survey is associated with potential corresponding biases such as inaccurate recall and false reporting (whether intentional or unintentional). That said, measures were taken to minimize intentionally false reporting, such as excluding respondents with implausible responses.
As is inherent with any research relying on convenience sampling methods, it is possible that certain subgroups of patients and physicians may be over-represented, such as white participants in our patient sample in the US (the only country where ethnicity was collected), and that the results may not be generalizable to the entire population.
Additionally, the DCE methodology involves respondents choosing between hypothetical treatment profiles with a set of attributes that may not reflect all the aspects of a treatment that can influence patient preference. These choices are intended to simulate possible clinical decisions but obviously do not have the same clinical, financial, or emotional consequences of actual decisions. As such, results from this study may not reflect real-world treatment decisions, which could be influenced by other factors not captured in the survey, such as physician recommendation, etc. Thus, differences can arise between stated and actual choices. Potential hypothetical bias has been limited by constructing choice questions that mimic realistic clinical choices as closely as possible and map clearly into clinical evidence. Finally, as the study was conducted in 2022, some new time-limited therapeutic approaches, such as BTKi-BCL2i combinations, were not yet available for CLL and not included in the DCE design.
Conclusion
This study provides key insights into the treatment preferences of physicians and patients with CLL as well as the trade-offs they are willing to make between efficacy, side effects, and duration/administration when selecting a targeted agent for first-line CLL treatment. Collectively, these results revealed that physicians and patients both value PFS benefits most, followed by risk of AEs. Patients and physicians were both willing to trade-off switching from time-limited treatment to treat to progression for a better 5-year PFS, decrease side effects, and risk of treatment discontinuation due to AEs. The type of regimen, whether it is TTP or time-limited, is less important to patients and physicians; however, on average, they favor a time-limited treatment over treating until progression. Thus, patients may perceive the risks and benefits associated with novel targeted agents differently than physicians, and these results can provide guidance to physicians when counselling patients about selecting a novel targeted agent for CLL and underscore the need for patient-physician discussions about the realistic benefits and risks of treatment.
Abbreviations
AE, Adverse event; BCL2i, B cell lymphoma-2 inhibitor; BR, Bendamustine and rituximab; BTKi, Bruton’s tyrosine kinase inhibitor; CIT, Chemotherapy-induced thrombocytopenia; CLL, Chronic lymphocytic leukemia; DCE, Discrete choice experiment; ECOG, Eastern Cooperative Oncology Group; FCR, Fludarabine, cyclophosphamide and rituximab; HB, hierarchical Bayesian; IRB, Institutional Review Board; ISPOR, International Society of Pharmacoeconomics and Outcomes Research; PFS, Progression-free survival; PI3Ki, Phosphoinositide 3-kinase inhibitor; RI, Relative importance; SD, Standard deviation; TN, treatment naïve; TTP, Treatment to progression.
Data Sharing Statement
Datasets are available upon reasonable request to the corresponding author.
Ethical Disclosure
This study was conducted according to best practice guidelines for Conjoint Analyses published by the International Society of Pharmacoeconomics and Outcomes Research (ISPOR) Good Research Practices for Conjoint Analysis Task Force. Prior to data collection, institutional review board (IRB) exemption was granted, according to FDA 21 CFR 56.104 and 45CFR46.104(b)(2): (2) Tests, Surveys, Interviews on 03/10/2022. This study complies with the ethical principles of the Declaration of Helsinki.
Acknowledgments
The authors thank Dr. Nadine Saleh and Uwe Walschus for their assistance in the manuscript writing. We are grateful to all participants of our study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by AstraZeneca.
Disclosure
BS is a former employee of AstraZeneca at the time the study was conducted. DP, KS and PM are employees of AstraZeneca and have stock ownership in AstraZeneca. BR, EM, KB and XG are employees of Oracle Life Sciences, who were contracted by AstraZeneca to conduct this research. DH was an employee of Oracle Life Sciences at the time the study was conducted. The authors report no other competing interests in this work.
References
1. Hallek M, Al-Sawaf O. Chronic lymphocytic leukemia: 2022 update on diagnostic and therapeutic procedures. Am J Hematol.; 96 12: 1679–1705 doi: 10.1002/ajh.26367.
2. Chronic Lymphocytic Leukemia-Cancer Stat Facts. Surveillance, epidemiology, and end results program. 2023. Available from: https://seer.cancer.gov/statfacts/html/clyl.html.
3. International CLL-IPI working group. An international prognostic index for patients with chronic lymphocytic leukaemia (CLL-IPI): a meta-analysis of individual patient data. Lancet Oncol. 2016;17(6):779–790. doi:10.1016/S1470-2045(16)30029-8
4. Munir T, Brown JR, O’Brien S, et al. Final analysis from RESONATE: up to six years of follow-up on ibrutinib in patients with previously treated chronic lymphocytic leukemia or small lymphocytic lymphoma. Am J Hematol. 2019;94(12):1353–1363. doi:10.1002/ajh.25638
5. Sharman JP, Coutre SE, Furman RR, et al. Final results of a randomized, Phase III study of rituximab with or without idelalisib followed by open-label idelalisib in patients with relapsed chronic lymphocytic leukemia. J Clin Oncol. 2019;37(16):1391–1402. doi:10.1200/JCO.18.01460
6. Martino EA, Bruzzese A, Vigna E, et al. Acalabrutinib in chronic lymphocytic leukemia. Expert Opin Pharmacother. 2023;24(5):545–549. doi:10.1080/14656566.2023.2194486
7. Keating MJ, O’Brien S, Albitar M, et al. Early results of a chemoimmunotherapy regimen of fludarabine, cyclophosphamide, and rituximab as initial therapy for chronic lymphocytic leukemia. J Clin Oncol. 2005;23(18):4079–4088. doi:10.1200/JCO.2005.12.051
8. Eichhorst B, Fink AM, Bahlo J, et al. First-line chemoimmunotherapy with bendamustine and rituximab versus fludarabine, cyclophosphamide, and rituximab in patients with advanced chronic lymphocytic leukaemia (CLL10): an international, open-label, randomised, Phase 3, non-inferiority trial. Lancet Oncol. 2016;17(7):928–942. doi:10.1016/S1470-2045(16)30051-1
9. Tam CS, O’Brien S, Wierda W, et al. Long-term results of the fludarabine, cyclophosphamide, and rituximab regimen as initial therapy of chronic lymphocytic leukemia. Blood. 2008;112(4):975–980. doi:10.1182/blood-2008-02-140582
10. Hallek M, Fingerle-Rowson G, Fink AM, et al. First-line treatment with Fludarabine (F), Cyclophosphamide (C), and Rituximab (R) (FCR) Improves Overall Survival (OS) in Previously Untreated Patients (pts) with Advanced Chronic Lymphocytic Leukemia (CLL): results of a randomized phase III trial on behalf of an international group of investigators and the German CLL study group. Blood. 2009;114(22):535. doi:10.1182/blood-2009-03-211714
11. Fischer K, Bahlo J, Fink AM, et al. Long-term remissions after FCR chemoimmunotherapy in previously untreated patients with CLL: updated results of the CLL8 trial. Blood. 2016;127(2):208–215. doi:10.1182/blood-2015-06-651125
12. FDA. Project Orbis: FDA approves acalabrutinib for CLL and SLL (2019). Available from: https://www.fda.gov/drugs/resources-information-approved-drugs/project-orbis-fda-approves-acalabrutinib-cll-and-sll.
13. Byrd JC, Furman RR, Coutre SE, et al. Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N Engl J Med. 2013;369(1):32–42. doi:10.1056/NEJMoa1215637
14. FDA. IMBRUVICA® (ibrutinib) Approved by U.S. FDA for the first-line treatment of chronic lymphocytic leukemia (2016). Available from: https://www.prnewswire.com/news-releases/imbruvica-ibrutinib-approved-by-us-fda-for-the-first-line-treatment-of-chronic-lymphocytic-leukemia-300231107.html.
15. Byrd JC, Brown JR, O’Brien S, et al. Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med. 2014;371(3):213–223. doi:10.1056/NEJMoa1400376
16. Burger JA, Tedeschi A, Barr PM, et al. Ibrutinib as initial therapy for patients with chronic lymphocytic leukemia. N Engl J Med. 2015;373(25):2425–2437. doi:10.1056/NEJMoa1509388
17. Hardy-Abeloos C, Pinotti R, Gabrilove J. Ibrutinib dose modifications in the management of CLL. J Hematol Oncol. 2020;13(1):66. doi:10.1186/s13045-020-00870-w
18. Mato AR, Nabhan C, Thompson MC, et al. Toxicities and outcomes of 616 ibrutinib-treated patients in the United States: a real-world analysis. Haematologica. 2018;103(5):874–879. doi:10.3324/haematol.2017.182907
19. Nuttall E, Tung J, Trounce E, Johnston R, Chevassut T. Real-world experience of ibrutinib therapy in relapsed chronic lymphocytic leukemia: results of a single-center retrospective analysis. J Blood Med. 2019;10:199–208. doi:10.2147/JBM.S202286
20. Byrd JC, Hillmen P, O’Brien S, et al. Long-term follow-up of the RESONATE phase 3 trial of ibrutinib vs ofatumumab. Blood. 2019;133(19):2031–2042. doi:10.1182/blood-2018-08-870238
21. Moreno C, Greil R, Demirkan F, et al. Ibrutinib plus obinutuzumab versus chlorambucil plus obinutuzumab in first-line treatment of chronic lymphocytic leukaemia (iLLUMINATE): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20(1):43–56. doi:10.1016/S1470-2045(18)30788-5
22. Mato AR, Thompson M, Allan JN, et al. Real-world outcomes and management strategies for venetoclax-treated chronic lymphocytic leukemia patients in the United States. Haematologica. 2018;103(9):1511–1517. doi:10.3324/haematol.2018.193615
23. Molica S, Gianfelici V, Levato L. Emerging Bruton tyrosine kinase inhibitors for chronic lymphocytic leukaemia: one step ahead ibrutinib. Expert Opin Emerg Drugs. 2020;25(1):25–35. doi:10.1080/14728214.2020.1724282
24. Farooqui AA, Ashraf A, Bin FT, et al. Novel targeted therapies for chronic lymphocytic leukemia in elderly patients: a systematic review. Clin Lymphoma Myeloma Leuk. 2020;20(7):e414–e426. doi:10.1016/j.clml.2020.02.013
25. Al-Sawaf O, Zhang C, Lu T, et al. Minimal residual disease dynamics after venetoclax-obinutuzumab treatment: extended off-treatment follow-up from the randomized CLL14 study. J Clin Oncol. 2021;39(36):4049–4060. doi:10.1200/JCO.21.01181
26. FDA. FDA approves venetoclax for CLL and SLL (2019). Available from: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-venetoclax-cll-and-sll.
27. AbbVie. AbbVie Receives European Commission Approval of VENCLYXTO® Combination Regimen for Patients with Previously-Untreated Chronic Lymphocytic Leukemia (2020). Available from: https://www.prnewswire.com/news-releases/abbvie-receives-european-commission-approval-of-venclyxto-combination-regimen-for-patients-with-previously-untreated-chronic-lymphocytic-leukemia-301021997.html.
28. Le H, Ryan K, Wahlstrom SK, et al. Oncologist and patient preferences for novel agents in first-line treatment for chronic lymphocytic leukemia: commonalities and disconnects. Patient Prefer Adherence. 2021;15:99–110. doi:10.2147/PPA.S289139
29. Bridges JFP, Hauber AB, Marshall D, et al. Conjoint analysis applications in health--a checklist: a report of the ISPOR good research practices for conjoint analysis task force. Value Health. 2011;14(4):403–413. doi:10.1016/j.jval.2010.11.013
30. Wallington M, Guillaume X, Mulvihill E, et al. Clinician and patient factors influencing treatment decisions in front-line chronic lymphocytic leukemia: a qualitative research study. Blood. 2022;140(S1):10810–10811. doi:10.1182/blood-2022-165766
31. Johnson R, Orme B. Getting the Most from CBC (2003). Available from: https://sawtoothsoftware.com/resources/technical-papers/getting-the-most-from-cbc.
32. Byrd JC, Hillmen P, Ghia P, et al. Acalabrutinib versus ibrutinib in previously treated chronic lymphocytic leukemia: results of the first randomized phase III trial. J Clin Oncol. 2021;39(31):3441–3452. doi:10.1200/JCO.21.01210
33. Mansfield C, Masaquel A, Sutphin J, et al. Patients’ priorities in selecting chronic lymphocytic leukemia treatments. Blood Adv. 2017;1(24):2176–2185. doi:10.1182/bloodadvances.2017007294
34. Landfeldt E, Eriksson J, Ireland S, et al. Patient, physician, and general population preferences for treatment characteristics in relapsed or refractory chronic lymphocytic leukemia: a conjoint analysis. Leuk Res. 2016;40:17–23. doi:10.1016/j.leukres.2015.11.006
35. Thurstone L. A law of comparative judgment. Psychol Rev. 1927;37(4):273–286. doi:10.1037/h0070288
36. Fadden D. Conditional logit analysis of qualitative choice behavior. Front Econometrics. 1974;105–142.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.